Abstract
Objective: To assess the extent to which intensity and timing of televised anti-smoking advertising emphasizing the serious harms of smoking influences quit attempts.
Methods: Using advertising gross rating points (GRPs), we estimated exposure to tobacco control and nicotine replacement therapy (NRT) advertising in the 3, 4–6, 7–9 and 10–12 months prior to follow-up of a replenished cohort of 3037 Australian smokers during 2002–08. Using generalized estimating equations, we related the intensity and timing of advertising exposure from each source to the likelihood of making a quit attempt in the 3 months prior to follow-up.
Results: Tobacco control advertising in the 3-month period prior to follow-up, but not in more distant past periods, was related to a higher likelihood of making a quit attempt. Each 1000 GRP increase per quarter was associated with an 11% increase in making a quit attempt [odds ratio (OR) = 1.11, 95% confidence interval (CI) 1.03–1.19, P = 0.009)]. NRT advertising was unrelated to quit attempts.
Conclusions: Tobacco control advertising emphasizing the serious harms of smoking is associated with short-term increases in the likelihood of smokers making a quit attempt. Repeated cycles of higher intensity tobacco control media campaigns are needed to sustain high levels of quit attempts.
Introduction
Recent reviews of the published literature have concluded that there is strong evidence that televised public health-sponsored mass media campaigns to encourage smoking cessation can increase quitting and contribute to reductions in adult smoking prevalence [1, 2]. Aside from the kind of messages broadcast, the population response of smokers to mass media campaigns is likely to be a function of the extent of population exposure to those messages, as determined by both the intensity and the duration of media campaigns. The extent of advertising that needs to be broadcast to achieve optimum population response is a critical research question for funding agencies because it points to the level and duration of campaign investment that can most efficiently achieve population changes.
Some studies have attempted to use a proxy measure of population quit attempts, such as relating variable campaign advertising investment or advertising rating points (a measure of estimated population exposure) to the volume of calls to a telephone Quitline [3–6]. Given that only a small minority of smokers will ever call a Quitline [7], a broader population-based examination of behavioural outcomes is critical to guide campaign investment decisions.
Some studies point to the possibility that advertising exposure may need to be greater to be able to influence adult smoking than youth smoking. For youth, threshold levels for detecting beneficial effects may exist around 300 advertising gross ratings points (GRPs) per quarter [8] and effects may begin to diminish at levels above 1250 GRPs per quarter [9], with linear increases in between [8–10]. Among adults, Hyland et al. [11] found that an average of 700 GRPs per quarter over a 2-year period in 1999–2000 was only weakly associated with quitting by 2001. A more recent cohort study of Massachusetts adult smokers found that a mean of 2100 GRPs per quarter over a 2-year period prior to baseline was significantly associated with quitting 2 years later [12].
Aside from the intensity of advertising, another important aspect of understanding how campaigns might influence smoking behaviour is the extent to which effects are detectable after the campaign broadcast ends, otherwise known as campaign carry forward, ‘adstock’, or campaign decay [13], hereafter referred to as ‘decay’. Consumer product advertising experience shows that although some advertising may be recalled long after broadcast ends, most media campaigns primarily have their effects on ‘behavioural changes’ while being broadcast and for a short time following [2, 13].
A few studies in tobacco control specifically demonstrate that this may also be the case for media campaigns to change tobacco use. For example, a short-term cohort study in Australia found an increase in adult quitting activity was sustained for at least a month following the onset of a 2-week mass media campaign that promoted the serious health harms of smoking [14]. Youth smoking susceptibility in Minnesota decreased during the broadcasting of a youth smoking prevention media campaign but had increased 6 months after the end of the campaign [15]. A time series analysis of the association between advertising exposure and smoking prevalence pointed to a rapid decay of the beneficial effect of tobacco control advertising on smoking prevalence [16].
In aggregate, these studies suggest that we need to know much more about campaign exposure levels and the rate of campaign decay in driving behaviour change at the population level. The primary aim of the current study was to investigate the effects of exposure intensity and the durability of tobacco control mass media campaigns on increasing the likelihood of quit attempts. Increasing the rate of quit attempts in a population has been demonstrated to be a critical ingredient for reducing overall population smoking prevalence [7, 17].
Methods
Design
We merged estimates of population exposure to televised anti-tobacco advertising and nicotine replacement therapy (NRT) advertising from commercial media monitoring sources for specific media markets to a cohort study of quit attempts among adult smokers, using data collection date and postcode information. Participants’ smoking characteristics taken from the first five waves of data (2002–06) were used to predict quit attempts at the follow-up waves 1 year later (2003–07).
Survey participants and measures
Participants were drawn from the first five waves of the Australian arm of the International Tobacco Control Four (ITC-4) Country survey, with follow-up data collected annually from 2003 to 2007. A detailed description of the ITC-4 Country study aims and methods can be found in Thompson et al. [18]. Briefly, participants were first recruited as smokers using stratified random digit dialling methods to try to obtain a representative sample of the smoking population and were surveyed using computer-assisted telephone interview. Smokers were then followed up at approximately 1-year intervals. An incentive of AUD$15 was provided after each survey to promote retention. Additional participants were recruited each year to replace those lost to attrition.
To be categorized as having made a quit attempt at follow-up, smokers needed to respond ‘yes’ to the question as to whether they had made a quit attempt since their last survey interview approximately 1 year beforehand and to have indicated that the time since most recent quit attempt was less than or equal to 90 days. Other smokers were assigned as not making a quit attempt in the 90 days prior to the follow-up survey. Those who had already quit at the commencement of each survey wave were excluded for follow-up analysis. The numbers of smokers and rates of complete follow-up data on quit attempts for each cohort were Wave 1, 2002–03 cohort, 1802 (81%) of 2213 eligible; Wave 2, 2003–04 cohort, 1495 (73%) of 2046 eligible; Wave 3, 2004–05 cohort, 1572 (78%) of 2010 eligible; Wave 4, 2005–06 cohort, 1397 (72%) of 1927 eligible; and Wave 5, 2006–07 cohort, 1528 (74%) of 2052 eligible.
Since intention to quit might conceivably be associated with responsiveness to media messages, we controlled for this potential confounder. We identified whether the participant had an interest in quitting from responses to the following question asked at the commencement of each survey wave: ‘are you planning to quit smoking within the next month, within the next 6 months, sometime in the future, beyond 6 months or are you not planning to quit?’ Responses were dichotomized into yes or no as an indication of their interest in quitting. Responses to the number of cigarettes smoked per day and time to first cigarette of the day were combined from the baseline survey to form the Heaviness of Smoking Index (HSI) [19], resulting in a 7-point scale ranging from 0 (low) to 6 (highly addicted).
We included the following as covariates in the analysis: age at first baseline interview, gender, state of residence, time in the study in months, survey wave (Waves 2 through 6), the number of months between baseline and follow-up survey interviews and quarter of the year. Responses to the number of cigarettes smoked per day and time to first cigarette of the day were combined from the first baseline survey to form the HSI [19], resulting in a 7-point scale ranging from 0 (low) to 6 (highly addicted). We also adjusted for low, middle and high socio-economic status (SES) on the basis of a variable that combined reported income and educational attainment at the first baseline survey. Low SES was defined as having either income below AUD$30 000 per annum or a low/moderate education level. Middle SES was defined as an income between AUD$30 000 and $59 000 and a moderate education level, or as income between $60 000 and $99 000 and low education or as having income below $30 000 and high education. High SES consisted of people with income above $100 000, or else income between $30 000 and $59 000 and high education or income between $60 000 and $99 000 and moderate education. Those with missing income data were classified on the basis of education alone.
Advertising exposure data
Occurrences of all tobacco-related advertisements appearing on television for the major Australian media markets from June 2002 to February 2008 were acquired from OzTAM Pty Ltd (North Sydney, Australia). Estimates of advertising exposure were assessed with television-monitoring devices and self-completion viewing diaries. Advertising exposure data are based on individual ratings of television programs obtained by monitoring household audiences across media markets. Ratings provide an estimate of the percentage of households with televisions watching a program in a media market over a specified period. The advertising exposure measure is based on GRPs for the population aged 18 years and older, with 1000 GRPs per quarter representing an average of 10 potential advertisement exposures for all adults within a media market. GRPs represent average potential exposure: actual exposure for any given individual would vary on the basis of the frequency of actual television viewing and attention to the advertisements within television programs.
GRPs were acquired for the two sole sources of tobacco-relevant television advertising in Australia: tobacco control advertising (from state and national governments or other public health organisations) and direct-to-consumer advertising of NRT by pharmaceutical companies. In Australia, it is important to appreciate that mass media campaigns have been a feature of the tobacco control environment for around 25 years, with states such as Victoria and Western Australia commencing their campaign activity in the 1980’s [20]. Also, unlike some other countries where message themes and target audiences have been variable, the vast majority of advertising messages are aimed at adult smokers and stress the serious health harms of tobacco use. A national mass media campaign was launched in 1997 with broadcast period of around 5 years, which used graphic images of serious smoking-related disease to emphasize the certain effects of smoking to adult smokers and promoted the message that ‘every cigarette is doing you damage’ [21]. During the 2000s, including the period covered by the present study, state-based mass media campaigns aimed at adult smokers have constituted the vast majority of population exposure, with most being messages for adults depicting the serious health consequences of smoking through graphic images, the use of personal stories or simulated demonstrations of health effects. A broadly representative sample of these ads is available at http://www.quit.org.au/browse.asp?ContainerID=1585 [22]. Only a very small minority of state-based advertising featured the health effects of secondhand smoke or was aimed principally at youth. Advertising GRPs from pharmaceutical companies for NRT, which commenced in Australia in 1995, were also aggregated. There has been no television advertising for other pharmaceutical smoking cessation products.
We constructed variables representing each respondent’s potential exposure to each source of advertising prior to their survey date. These variables were three-monthly (quarterly) summed aggregations of the GRPs occurring in the media market in which they resided for the 3 months leading up to the date of the follow-up survey, 4–6 months prior, 7–9 months prior and 10–12 months prior.
Statistical analysis
The outcome was a binary variable representing the occurrence of a quit attempt in the 3 months prior to completing a follow-up survey. We regressed quit attempts on prior exposure to tobacco control advertising and NRT advertising. The models used generalized estimating equations (GEE) for binary outcomes. This method correctly accounts for the longitudinal study design (multiple observations clustered within individuals). Variance was calculated using cluster robust standard errors.
Our candidate set of predictors consisted of variables measuring interest in quitting and heaviness of smoking (both in the previous wave), baseline measures of age, gender, SES and state, a variable for each individual that represented number of waves in the study, number of months between surveys and the quarter of the year in which the data were collected. Our modelling strategy closely followed that proposed by Hosmer and Lemeshow [23], namely univariate analysis (using GEE), followed by fitting an initial multivariate model with all predictors identified at the univariate stage as having P < 0.25. On the basis of these results, we then modified the model by sequentially refitting the equation to identify all significant predictors as well as any confounders. Our final model consisted of seven covariates, including two confounders (survey year quarter and state), which although non-significant, appeared to modify the values of other estimates in the model.
We undertook additional analyses to examine whether the association between quit attempts and GRPs was non-linear using GRPs2. We also tested whether the effect of GRPs on quitting was modified by interest in quitting from the previous wave by including terms for the product of GRPs and interest in quitting. Finally, we tested the sensitivity of our results by re-estimating the final model using bootstrap estimation with 2000 replications. All analyses were undertaken in Stata 11.1.
Results
Table I shows that, of the 3037 participants, 62.7% had not made a quit attempt in the 90 days prior to any of the follow-up interviews they completed, whereas 27.0% had made one attempt, 7.3% had made two, 2.2% had made three and 0.9% had made four or five. Age group was broadly distributed and just over half of smokers were of low SES. As expected from Australia’s population distribution and the sampling strategy, the majority were residents in New South Wales, Victoria and Queensland.
Table I.
Characteristics of sample, n = 3037
| Variable | Frequency | Sample % |
| Number of quit attempts in the 3 months prior to follow-up survey | ||
| 0 | 1903 | 62.7 |
| 1 | 819 | 27.0 |
| 2 | 221 | 7.3 |
| 3 | 66 | 2.2 |
| 4 or 5 | 28 | 0.9 |
| Age (years) | ||
| 18–24 | 390 | 12.8 |
| 25–39 | 1045 | 34.4 |
| 40–54 | 1102 | 36.3 |
| 55+ | 500 | 16.5 |
| Gender | ||
| Female | 1643 | 54.1 |
| Male | 1394 | 45.9 |
| Socio-economic status | ||
| Low | 1572 | 51.8 |
| Middle | 716 | 23.6 |
| High | 749 | 24.7 |
| State | ||
| Victoria | 773 | 25.5 |
| New South Wales | 1013 | 33.4 |
| Western Australia | 291 | 9.6 |
| South Australia | 215 | 7.1 |
| Tasmania | 103 | 3.4 |
| Queensland | 595 | 19.6 |
| Australian Capital Territory | 47 | 1.6 |
| Wave | ||
| Wave 1: 2002–03 | 1802 | 23.1 |
| Wave 2: 2003–04 | 1495 | 19.2 |
| Wave 3: 2004–05 | 1572 | 20.2 |
| Wave 4: 2005–06 | 1397 | 17.9 |
| Wave 5: 2006–07 | 1528 | 19.6 |
Table II indicates the mean tobacco control advertising exposure over each consecutive 3-month period prior to the follow-up interview. While the mean level of advertising was similar for each period, the standard deviations indicate that there was wide variation between individuals introduced by their residence in different media markets and the date of follow-up survey. Table II also shows the variability in mean tobacco control advertising exposure by media market for the 3-month period prior to follow-up interview. In general, the mean level of GRPs was higher in the metropolitan markets (largely comprising capital cities) than in the regional markets. Finally, Table II displays the mean NRT GRPs for each of the periods examined, indicating variability in exposure of individuals to NRT advertising within each period.
Table II.
Mass media campaign exposure prior to survey follow-up
| Type, location and timing of GRPs | Mean | SD | Minimum | Maximum |
| Tobacco control GRPs for all states | ||||
| 10–12 months prior | 1125 | 870 | 0 | 4100 |
| 7–9 months prior | 1038 | 779 | 0 | 4830 |
| 4–6 months prior | 1245 | 1118 | 0 | 4830 |
| 0–3 months prior | 1296 | 864 | 0 | 3880 |
| Tobacco control GRPs 0–3 months prior by state | ||||
| Victoria | ||||
| Metropolitan | 1128 | 593 | 280 | 2770 |
| Regional | 848 | 505 | 100 | 1910 |
| New South Wales | ||||
| Metropolitan | 1583 | 1063 | 0 | 3880 |
| Regional | 1365 | 877 | 0 | 3560 |
| Western Australia | ||||
| Metropolitan | 1677 | 893 | 0 | 3300 |
| Regional | 1411 | 758 | 40 | 2700 |
| South Australia | ||||
| Metropolitan | 1582 | 753 | 20 | 2840 |
| Tasmania | ||||
| Metropolitan | 1266 | 534 | 220 | 2110 |
| Queensland | ||||
| Metropolitan | 1114 | 814 | 0 | 2710 |
| Regional | 909 | 734 | 0 | 2500 |
| Australian Capital Territory | ||||
| Metropolitan | 258 | 249 | 10 | 680 |
| NRT GRPs for all states | ||||
| 10–12 months prior | 1282 | 594 | 0 | 3060 |
| 7–9 months prior | 1436 | 669 | 0 | 3630 |
| 4–6 months prior | 1570 | 807 | 0 | 4090 |
| 0–3 months prior | 961 | 558 | 0 | 2400 |
| NRT GRPs 0–3 months prior by state | ||||
| Victoria | ||||
| Metropolitan | 1208 | 545 | 370 | 2310 |
| Regional | 581 | 391 | 0 | 1190 |
| New South Wales | ||||
| Metropolitan | 1049 | 493 | 400 | 2060 |
| Regional | 698 | 423 | 0 | 1170 |
| Western Australia | ||||
| Metropolitan | 1062 | 564 | 380 | 2210 |
| Regional | 19 | 53 | 0 | 280 |
| South Australia | ||||
| Metropolitan | 1147 | 593 | 380 | 2400 |
| Tasmania | ||||
| Metropolitan | 295 | 194 | 0 | 590 |
| Queensland | ||||
| Metropolitan | 1093 | 513 | 400 | 2160 |
| Regional | 562 | 380 | 0 | 1180 |
| Australian Capital Territory | ||||
| Metropolitan | 572 | 378 | 0 | 1200 |
Table III shows that at the univariate level, tobacco control GRPs in the 3 months prior to the follow-up survey, but not past periods, were associated with a greater likelihood of making a quit attempt over the same period. NRT GRPs were also unrelated, except for the period 10–12 months past, where they were associated with ‘a reduced’ likelihood of making a quit attempt, although this effect disappeared in the multivariate analyses. Baseline interest in quitting and heaviness of smoking, age and the time-related variables all had strong univariate associations with quit attempts. There was only weak evidence that quit attempts differed between states, while gender and SES were unrelated to quit attempts.
Table III.
Odds ratios and 95% CIs from generalized estimating equations of covariates predicting quit attempts
| Univariate analysis |
Initial model |
Final model |
||||
| OR (95% CI) | P | ORa (95% CI) | P | ORa (95% CI) | P | |
| Tobacco control GRPsb | ||||||
| 1–3 months ago | 1.07 (1.01–1.14) | 0.025 | 1.09 (1.01–1.18) | 0.031 | 1.11 (1.03–1.19) | 0.009 |
| 4–6 months ago | 0.96 (0.92–1.01) | 0.153 | 1.05 (0.97–1.13) | 0.212 | ||
| 7–9 months ago | 0.98 (0.92–1.06) | 0.649 | ||||
| 10–12 months ago | 1.00 (0.94–1.06) | 0.938 | ||||
| NRT GRPsb | ||||||
| 1–3 months ago | 0.96 (0.88–1.06) | 0.461 | ||||
| 4–6 months ago | 0.97 (0.90–1.04) | 0.361 | ||||
| 7–9 months ago | 0.96 (0.89–1.05) | 0.406 | ||||
| 10–12 months ago | 0.89 (0.81–0.98) | 0.017 | 0.90 (0.80–1.02) | 0.103 | ||
| Interest in quittingc | <0.001 | <0.001 | <0.001 | |||
| No | 1.00 | 1.00 | 1.00 | |||
| Yes | 2.40 (2.05–2.80) | 2.42 (2.05–2.86) | 2.42 (2.05–2.85) | |||
| Heaviness of smoking indexc | 0.92 (0.89–0.96) | <0.001 | 0.93 (0.89–0.97) | <0.001 | 0.93 (0.90–0.97) | 0.001 |
| Age (years) | <0.001 | <0.001 | <0.001 | |||
| 18–24 | 1.00 | 1.00 | 1.00 | |||
| 25–39 | 0.81 (0.65–1.00) | 0.84 (0.68–1.04) | 0.86 (0.69–1.06) | |||
| 40–54 | 0.63 (0.51–0.77) | 0.73 (0.59–0.92) | 0.77 (0.62–0.95) | |||
| 55+ | 0.88 (0.69–1.11) | 1.18 (0.92–1.51) | 1.20 (0.94–1.55) | |||
| Gender | 0.332 | |||||
| Female | 1.00 | |||||
| Male | 1.07 (0.94–1.22) | |||||
| Socio-economic status | 0.735 | |||||
| Low | 1.00 | |||||
| Middle | 1.00 (0.85–1.18) | |||||
| High | 1.06 (0.91–1.25) | |||||
| State | 0.063 | 0.123 | 0.062 | |||
| Victoria | 1.00 | 1.00 | 1.00 | |||
| New South Wales | 0.99 (0.83–1.18) | 0.93 (0.77–1.12) | 0.98 (0.82–1.17) | |||
| Western Australia | 1.18 (0.94–1.50) | 1.05 (0.80–1.39) | 1.12 (0.88–1.42) | |||
| South Australia | 0.86 (0.65–1.14) | 0.83 (0.62–1.12) | 0.83 (0.62–1.11) | |||
| Tasmania | 1.32 (0.92–1.90) | 1.19 (0.80–1.77) | 1.33 (0.92–1.92) | |||
| Queensland | 0.91 (0.75–1.12) | 0.90 (0.73–1.11) | 0.95 (0.77–1.16) | |||
| Australian Capital Territory | 1.64 (0.99–2.71) | 1.71 (1.03–2.82) | 1.82 (1.11–3.00) | |||
| Time in study | 0.91 (0.87–0.96) | <0.001 | 0.98 (0.92–1.05) | 0.552 | ||
| Wave | 0.90 (0.87–0.94) | <0.001 | 0.87 (0.80–0.95) | 0.002 | 0.87 (0.81–0.93) | <0.001 |
| Months between surveys | 0.97 (0.96–0.99) | 0.001 | 0.99 (0.97–1.02) | 0.520 | ||
| Quarter | <0.001 | 0.645 | 0.569 | |||
| Q1: January to March | 1.00 | 1.00 | 1.00 | |||
| Q2: April to June | 1.44 (0.82–2.53) | 0.88 (0.47–1.66) | 0.94 (0.51–1.72) | |||
| Q3: July to September | 1.40 (0.79–2.49) | 1.02 (0.56–1.87) | 1.09 (0.61–1.98) | |||
| Q4: October to December | 1.13 (0.65–1.98) | 1.02 (0.58–1.79) | 1.06 (0.61–1.86) | |||
Adjusted odds ratio.
In units of 1000 GRPs per quarter.
Response from the previous wave.
Table III also shows that in the final model, tobacco control advertising in the 3 months prior to the follow-up survey was positively associated with quit attempts over the same period, such that each increase of 1000 GRPs over the 3-month period was associated with an 11% increase in the odds of making a quit attempt [odds ratio (OR) = 1.11, 95% confidence interval (CI) 1.03–1.19]. There was no evidence that this relationship was non-linear since refitting the final model with an additional term for GRPs2 did not provide a better fit to the data (P = 0.343). NRT GRPs were unrelated to quit attempts in the initial multivariate model and were dropped from further analysis.
Respondents who had an interest in quitting in the previous year had 2.42 times the odds of making a quit attempt compared with respondents who had no interest in quitting (95% CI 2.05–2.85, P < 0.001). An interaction term between baseline interest in quitting and GRPs in the previous 3 months was non-significant (P = 0.868), indicating that GRPs increased quit attempts to a similar extent among both groups.
Refitting the final model using bootstrap estimation did not result in appreciably different standard errors and CIs (e.g. for tobacco control GRPs, OR = 1.11, 95% CI 1.03–1.19, P = 0.008). This suggests that the conclusions from the final model are fairly robust and not likely to be due to the increased chance of detecting significant effects when several models are fitted on the same set of data.
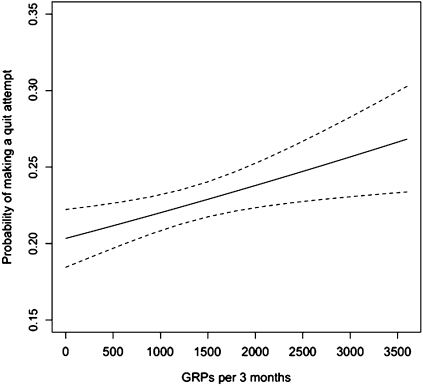
For the purposes of interpretation, Fig. 1 shows the probability of making a quit attempt for different levels of tobacco control GRPs in the 3 months leading up to the date of the follow-up survey. These values are derived from predictions using the final model where GRPs are allowed to vary from their minimum observed value to the maximum, and all other covariates are held constant at their observed values. At zero GRPs (0), the model predicts the probability of making a quit attempt in the 3 months prior to being surveyed is around 20%. At the mean value of approximately 1296 GRPs over 3 months, the predicted probability of making a quit attempt is 22.5% and rises to 27% at the maximum value of 3880 GRPs over a 3-month period, the highest level studied.
Fig. 1.
Predicted probabilities and 95% CI of making a quit attempt in the 3 months prior to the survey date as a function of GRPs over the same period (from final model, all other covariates held constant at their observed values).
Discussion
We found that tobacco control media campaigns are associated with a significant increase in the proportion of smokers who make quit attempts in the months during advertising exposure but not for advertising exposure that is more than 3 months old. This supports past suggestions that there are relatively short-term carry-forward effects of campaigns on quit attempts. In the public health literature, the notion that mass media campaigns might provide a time-limited trigger for prompting behaviour change has not been well appreciated, with some lamenting the absence of long-term effects of only short-run campaigns. Funding authorities often assume that after a period of initial investment, media campaigns might be expected to require very little ongoing support [24]. This suggests a basic misunderstanding of the capability of mass media campaigns to produce durable effects on behaviours like quitting smoking. Our results instead underline the need for repeated cycles of broadcasting of mass media campaigns to achieve sustainable population changes in smoking behaviour.
We found that recent campaign exposure prompted quit attempts even among those not interested in quitting at baseline. This provides support for a recent body of work which indicates that, rather than moving through a series of sequential stages in the quitting process, between 37 and 52% of adult smokers are prompted to quit with little planning and can move from a position where they were not previously thinking about quitting to making a quit attempt [25–27]. Furthermore, spontaneous quit attempts appear to have at least a similar likelihood of success as those that are delayed [28] and unplanned attempts seem at least as successful as those that are planned [26, 27]. In Australia, baseline quit attempt activity is relatively high [14, 29] and anti-smoking mass media campaigns are a frequent reason cited for trying to quit [M. McCarthy, J. Abbott, M. Wakefield, submitted for publication.]. Within the recent 3-month period, the fact that we did not find a diminishing return on quit attempts at higher levels of campaign exposure suggests that even in this population who evidence relatively high quit attempt activity, further increases in tobacco control media campaign investment could be expected to efficiently result in additional population increases in quit attempts.
The fact that NRT advertising was unrelated to quit attempts in this population is worthy of comment. Our findings are consistent with a previous time-series study in Australia which found that while tobacco control advertising accelerated declines in smoking prevalence, NRT advertising did not [16]. Arguably, the main aim of NRT advertising is not to promote quit attempts but to direct those trying to quit to use a particular product as an aid when they do try.
Limitations of the study include the use of GRP data as the measure of media campaign exposure. GRPs represent estimates of exposure at the population level and smokers within media markets may receive more or less exposure depending upon how much television they watch and their television program selection. However, GRPs do correlate well with recall of advertising [8, 30, 31]. A second potential limitation was that our outcome measure was a self-report of making a quit attempt in the past 3 months and our advertising exposures needed to be aggregated accordingly to cover this 3-month period. More fine-grained aggregations at the monthly or weekly level, if sample size permitted, would have furnished more detailed information about the decay of advertising effects. In this respect, future studies might employ weekly or monthly cross-sectional tracking surveys undertaken during and after broadcasting to further investigate campaign decay effects [32]. Thirdly, we did not adjust for the different styles of tobacco control campaigns that were broadcast over the period that may have had different rates of decay. Biener et al. [33] found that recall of hard-hitting ads was greater than for other ads and suggests that decay may be attenuated for these kinds of campaigns. Continuous tracking of graphic ads illustrating health harms of smoking has suggested different effects for different executions [32]. Although the majority of Australian campaign advertising did use this style of message, our aim was to examine the effects in aggregate of tobacco control campaigns. In fact, a strength of our study is that our campaign exposure and outcome measures are not tied to any one specific campaign but are average effects of these styles of campaigns in general. Assessing the effects of individual styles of campaigns on quitting attempts remains a question for further study.
As suggested by Hill and Marks [24], a mass media campaign ought to be considered as akin to holding down a spring in driving behaviour change, restraining the very powerful forces that otherwise promote smoking behaviour. Once campaign broadcasting ends and the factors that promote smoking are allowed to regain dominance, the higher rate of quit attempts declines. Our study results are entirely consistent with this perspective and lend support for ongoing investment in media campaigns to reduce smoking prevalence.
Funding
National Health and Medical Research Council of Australia (NHMRC) (504707). Data collection for the Australian arm of the ITC survey was primarily funded by NHMRC (265903, 450110), with supplementary funding from the Roswell Park Transdisciplinary Tobacco Use Research Center (P50 CA111236); National Cancer Institute of the United States (R01 CA 100362); Robert Wood Johnson Foundation (045734); Canadian Institutes of Health Research (57897, 79551); Cancer Research UK (C312/A3726); Canadian Tobacco Control Research Initiative (014578); the Centre for Behavioural Research and Program Evaluation; the National Cancer Institute of Canada/Canadian Cancer Society. M.was supported by an NHMRC Principal Research Fellowship.
Conflict of interest statement
There is no conflict of interest.
References
- 1.National Cancer Institute. The Role of the Media in Promoting and Reducing Tobacco Use. Bethesda, MD: US Department of Health and Human Services, National Institutes of Health, National Cancer Institute; 2008. (NIH Pub No 07–6242) [Google Scholar]
- 2.Wakefield MA, Loken B, Hornik RC. Use of mass media campaigns to change health behaviour. Lancet. 2010;376:1261–71. doi: 10.1016/S0140-6736(10)60809-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Miller CL, Wakefield M, Roberts L. Uptake and effectiveness of the Australian telephone quitline service in the context of a mass media campaign. Tob Control. 2003;12(Suppl. 2):ii53–8. doi: 10.1136/tc.12.suppl_2.ii53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Erbas B, Bui Q, Huggins R, et al. Investigating the relation between placement of quit antismoking advertisements and number of telephone calls to quitline: a semiparametric modelling approach. J Epidemiol Community Health. 2006;60:180–2. doi: 10.1136/jech.2005.038109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mosbaek CH, Austin DF, Stark MJ, et al. The association between advertising and calls to a tobacco quitline. Tob Control. 2007;16(Suppl. 1):i24–9. doi: 10.1136/tc.2007.020222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Farrelly MC, Hussin A, Bauer UE. Effectiveness and cost effectiveness of television, radio and print advertisements in promoting the New York smokers' quitline. Tob Control. 2007;16(Suppl. 1):i21–3. doi: 10.1136/tc.2007.019984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chapman S. Accelerating smoking cessation and prevention in whole communities. In: Chapman S, editor. Public Health Advocacy and Tobacco Control: Making Smoking History. Malden, MA: Blackwell Publishing; 2007. pp. 127–52. [Google Scholar]
- 8.Emery S, Wakefield MA, Terry-McElrath Y, et al. Televised state-sponsored antitobacco advertising and youth smoking beliefs and behavior in the united states, 1999-2000. Arch Pediatr Adolesc Med. 2005;159:639–45. doi: 10.1001/archpedi.159.7.639. [DOI] [PubMed] [Google Scholar]
- 9.Farrelly MC, Davis KC, Haviland ML, et al. Evidence of a dose-response relationship between “truth” antismoking ads and youth smoking prevalence. Am J Public Health. 2005;95:425–31. doi: 10.2105/AJPH.2004.049692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Terry-McElrath YM, Wakefield MA, Emery S, et al. State anti-tobacco advertising and smoking outcomes by gender and race/ethnicity. Ethn Health. 2007;12:339–62. doi: 10.1080/13557850701300723. [DOI] [PubMed] [Google Scholar]
- 11.Hyland A, Wakefield M, Higbee C, et al. Anti-tobacco television advertising and indicators of smoking cessation in adults: a cohort study. Health Educ Res. 2006;21:296–302. doi: 10.1093/her/cyh068. [DOI] [PubMed] [Google Scholar]
- 12.Durkin S, Biener L, Wakefield M. Effects of different types of antismoking ads on reducing disparities in smoking cessation among socioeconomic subgroups. Am J Public Health. 2009;99:2217–23. doi: 10.2105/AJPH.2009.161638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tellis GJ. Effective Advertising: Understanding When, How, and Why Advertising Works. Thousand Oaks, CA: Sage Publications; 2004. [Google Scholar]
- 14.Borland R, Balmford J. Understanding how mass media campaigns impact on smokers. Tob Control. 2003;12(Suppl. 2):ii45–52. doi: 10.1136/tc.12.suppl_2.ii45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sly DF, Arheart K, Dietz N, et al. The outcome consequences of defunding the Minnesota youth tobacco-use prevention program. Prev Med. 2005;41:503–10. doi: 10.1016/j.ypmed.2004.11.027. [DOI] [PubMed] [Google Scholar]
- 16.Wakefield MA, Durkin S, Spittal MJ, et al. Impact of tobacco control policies and mass media campaigns on monthly adult smoking prevalence. Am J Public Health. 2008;98:1443–50. doi: 10.2105/AJPH.2007.128991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zhu S-H. Presentation to the Oceania Tobacco Control Conference. Differential cessation rates across populations: what explains it and how to reduce it. Auckland, New Zealand, 2007. [Google Scholar]
- 18.Thompson ME, Fong GT, Hammond D, et al. Methods of the international tobacco control (ITC) four country survey. Tob Control. 2006;15(Suppl. 3):iii12–8. doi: 10.1136/tc.2005.013870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kozlowski LT, Porter CQ, Orleans CT, et al. Predicting smoking cessation with self-reported measures of nicotine dependence: FTQ, FTND, and HSI. Drug Alcohol Depend. 1994;34:211–6. doi: 10.1016/0376-8716(94)90158-9. [DOI] [PubMed] [Google Scholar]
- 20.Scollo M, Winstanley M. Social marketing and public education campaigns. In: Scollo M, Winstanley M, editors. Tobacco in Australia: Facts and Issues. 3rd edn. Melbourne, Australia: The Cancer Council Victoria; 2008. [Google Scholar]
- 21.Hill D, Carroll T. Australia's national tobacco campaign. Tob Control. 2003;12(Suppl. 2):ii9–14. doi: 10.1136/tc.12.suppl_2.ii9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Quitline Victoria. Quit Victoria Resource & Media Centre. Available at: http://www.quit.org.au/browse.asp?ContainerID=1585. Accessed: 9 November 2010. [Google Scholar]
- 23.Hosmer DW, Lemeshow S. Applied Logistic Regression Analysis. 2nd edn. New York, NY: Wiley Series in probability and statistics; 2000. [Google Scholar]
- 24.Hill D, Marks R. Health promotion programs for melanoma prevention: screw or spring? Arch Dermatol. 2008;144:538–40. doi: 10.1001/archderm.144.4.538. [DOI] [PubMed] [Google Scholar]
- 25.Larabie LC. To what extent do smokers plan quit attempts? Tob Control. 2005;14:425–8. doi: 10.1136/tc.2005.013615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.West R, Sohal T. Catastrophic pathways to smoking cessation: findings from national survey. BMJ. 2006;332:458–60. doi: 10.1136/bmj.38723.573866.AE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Murray RL, Lewis SA, Coleman T, et al. Unplanned attempts to quit smoking: missed opportunities for health promotion? Addiction. 2009;104:1901–9. doi: 10.1111/j.1360-0443.2009.02647.x. [DOI] [PubMed] [Google Scholar]
- 28.Cooper J, Borland R, Yong HH, et al. To what extent do smokers make spontaneous quit attempts and what are the implications for smoking cessation maintenance? Findings from the international tobacco control four country survey. Nicotine Tob Res. 2010;12(Suppl):S51–7. doi: 10.1093/ntr/ntq052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Borland R, Hyland A, Cummings KM, et al. One size does not fit all when it comes to smoking cessation: observations from the international tobacco control policy evaluation project. Nicotine Tob Res. 2010;12(Suppl):S1–3. doi: 10.1093/ntr/ntq140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Southwell BG, Barmada CH, Hornik RC, et al. Can we measure encoded exposure? Validation evidence from a national campaign. J Health Commun. 2002;7:445–53. doi: 10.1080/10810730290001800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Niederdeppe J. Assessing the validity of confirmed ad recall measures for public health communication campaign evaluation. J Health Commun. 2005;10:635–50. doi: 10.1080/10810730500267662. [DOI] [PubMed] [Google Scholar]
- 32.Donovan RJ, Boulter J, Borland R, et al. Continuous tracking of the Australian national tobacco campaign: advertising effects on recall, recognition, cognitions, and behaviour. Tob Control. 2003;12(Suppl. 2):ii30–9. doi: 10.1136/tc.12.suppl_2.ii30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Biener L, McCallum-Keeler G, Nyman AL. Adults' response to Massachusetts anti-tobacco television advertisements: impact of viewer and advertisement characteristics. Tob Control. 2000;9:401–7. doi: 10.1136/tc.9.4.401. [DOI] [PMC free article] [PubMed] [Google Scholar]