Abstract
An unusual case of fibrous dysplasia involving right craniofacial region in a female is reported. The clinical features, radiological findings, and treatment have been discussed.
Keywords: Craniofacial, fibrous dysplasia
Introduction
Fibrous or fibro-osseous dysplasia (FD) is a developmental disorder of growing bones of unknown etiology. It occurs in two distinct forms polyostotic, which involves several bones and accounts for 30% and the monostotic form, which involves a single bone and constitutes 70% of cases.[1] Craniofacial involvement in FD occurs in nearly 100% of polyostotic and 30% of monostotic forms.[2] The bones commonly involved are mandible (12%) and maxilla (12%), involvement of the ethmoid, sphenoid, frontal, and temporal bones are infrequent.[3] These lesions cause expansion, thickening, and sclerosis of the involved bones with resultant visual complications, hearing disturbances, facial asymmetry and tooth displacement depending on the bone involved. We report a case of craniofacial polyostotic fibrous dysplasia in a 16-year-old female patient.
Case Report
A 16-year-old female presented with a swelling on the right side of the face from past one year. [Figure 1]. There was no history of pain, trauma, epistaxis, loosening of teeth, trismus or diminished vision. Examination of the region revealed a smooth bony-hard swelling involving right maxilla, zygoma, and temporal and mandibular region. The skin over the swelling was normal. The swelling was bulging in the gingivo-buccal sulcus with normal teeth. There was no other swelling in the body and cafe’-au-lait spots were not seen. The throat and nose examination was found to be normal. The routine blood and urine investigation were normal. The CT scan [Figures 2–4] showed a radio-dense mass involving right frontal, temporal, zygomatic, maxilla, and mandible causing facial asymmetry with ground-glass appearance and expansion of involved bones. PA view of skull showed a diffuse radiopacity with faint, linear to irregular central opacities [Figure 5]. An incisional biopsy was subsequently performed, providing a diagnosis of fibrous dysplasia. Microscopic examination showed a cellular connective tissue stroma consisting of fibroblasts arranged in a whorled or storiform pattern, which merged into anastomosing areas of cellular condensation. There was ribbon-like osteoid trabeculae lined by numerous plump osteoblasts that showed a transition into areas of woven bone associated with occasional osteoclasts. Clusters of multinucleated giant cells were noted near areas of cystic change and hemorrhage [Figure 6]. Based on the clinical history, radiographic and histologic features of the lesion, a diagnosis of craniofacial polyostotic fibrous dysplasia was established.
Figure 1.

Clinical appearance of the lesion at the time of evaluation
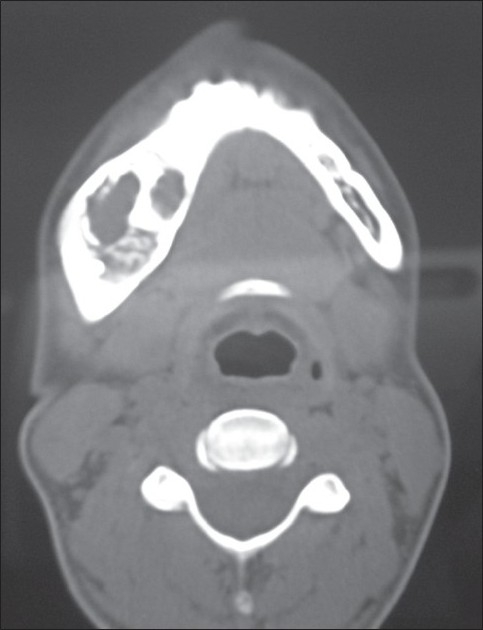
Figure 2.
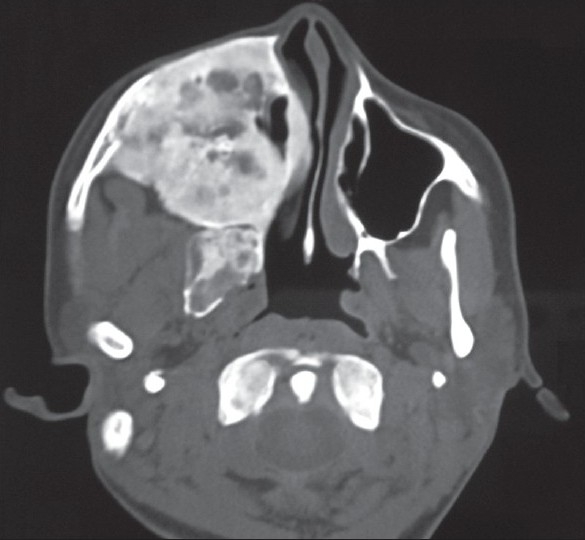
Axial CT image shows a radio opaque lesion occupies most of the facial bones in the mid and upper facial skeleton on the right side, which is signifi cantly expanded. The maxillary sinus and nasal airway on the right is obliterated
Figure 4.
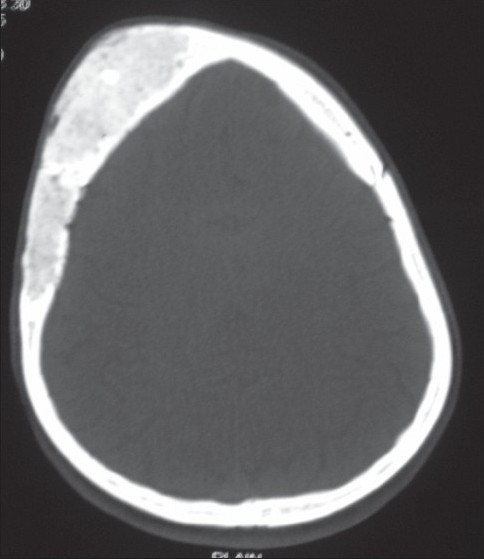
Axial CT image shows expansion of the right frontal and temporal bones
Figure 5.
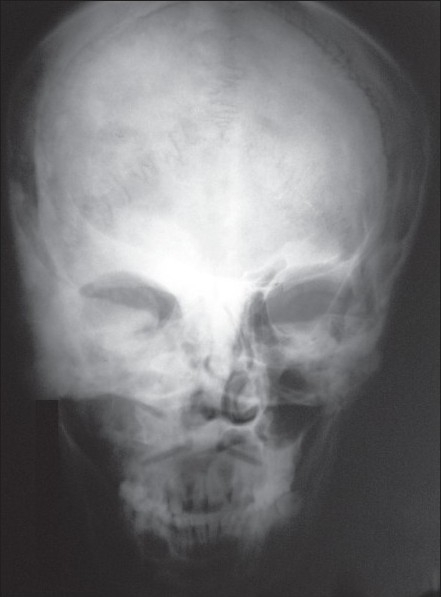
PA view of skull showing diffuse radiopacity with faint, linear to irregular central opacities
Figure 6.
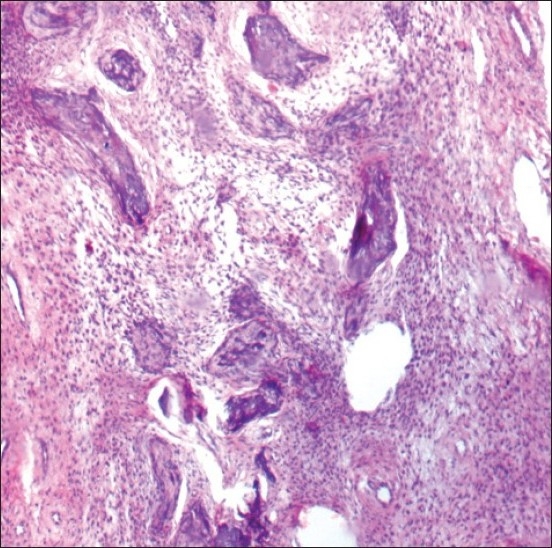
Image using H and E stain (magnifi cation ×4) showing interlacing irregular shaped bone trabeculae set in a well vascularized stroma with dilated vascular channels, consisting with fibrous dysplasia
Figure 3.
Axial CT image shows expansion of the right mandibular with radiopaque and radiolucent changes
Discussion
Fibrous dysplasia is a developmental or growth disorder in which normal bone is replaced by abnormal fibrous tissue that contains small, abnormally arranged bone trabeculae. It is considered by some authors to be a hamartomatous malformation that presumably results from an idiopathic arrest in maturation of bone at the woven bone stage.[3] Craniofacial involvement in fibrous dysplasia is seen in both monostotic and polyostotic forms. Monostotic fibrous dysplasia has a different skeletal distribution from polyostotic disease and occurs most commonly in the femur followed by tibia, craniofacial bones, and ribs.[2] Craniofacial involvement occurs in about 30% of monostotic fibrous dysplasia and typically affects the maxilla, mandible, and rarely the calvarium. Polyostotic form of the disease has nearly 100% involvement of the craniofacial bones.[3] Clinical presentation of fibrous dysplasia varies with the primary bone involved and the extent of disease. Fibrous dysplasia has its onset during early life, usually in late childhood or early adolescence. Patients with polyostotic form of disease are considerably younger. There is an equal sex distribution in monostotic fibrous dysplasia but the polyostotic form has a clear female predilection.[3] Radiographic features of fibrous dysplasia vary depending on the amount of bony and fibrous matrix within the lesion and have been sub-classified into three different patterns: pagetoid type 56%, sclerotic type 23%, and the radiolucent type 21%.[4] Both our patients had sclerotic type of lesions; which is the commonest form of involvement seen in facial bones and bones of the base of skull. The lytic and pagetoid types usually involve the calvarial bones. Radionuclide scanning in fibrous dysplasia shows areas of intensely increased uptake, which is due to diffuse microscopic ossification. Scintigraphy is helpful in determining the activity and potential multicentricity of the lesion; it is specifically helpful in diagnosing when plain radiographs are equivocal.[5] CT accurately establishes the diagnosis and extent of bone involvement. Involvement of optic canals, orbital fissures, frontonasal ducts, and ostiomeatal complex can be best evaluated by CT scanning. CT characteristics of fibrous dysplasia include expansion of the involved bone with heterogenous pattern of CT densities associated with scattered or confluent islands of bone formation. CT attenuation levels have been reported to range from 34 to 513 HU depending on the fibrous tissue and bone content.[6] On magnetic resonance imaging, fibrous dysplasia exhibits homogenous, moderately low signal intensity on T1 weighted images. On T2 weighted images, the tissue usually exhibits very high signal intensity. After intravenous Gd-DTPA, lesions display moderate to significant central contrast enhancement with some rim enhancement. The degree of contrast enhancement on T1 weighted images depends on amount and degree of bone trabeculae and collagen present.[6] Both CT and MRI are excellent imaging modalities in defining the constrictive effect of craniofacial fibrous dysplasia on the orbit, optic canals and adjacent paranasal sinuses.
Park BY et al studied the relation between serum alkaline phosphatase and found that post operative serum ALP could be a reliable marker for the predicting the progress of craniofacial FD[7]. Study of 18 cases of FD carried out by Ziadi S et al found that most were monostotic (94%), maxilla and mandible were the most frequent locations (83.3%) and sex ratio was 3.5 in favor of women[8].
Future therapeutic approaches for the treatment of FD will depend on greater understanding of post – natal skeletal stem cell biology and how these cells can be manipulated for efficient bone regeneration[9]. Cyst degeneration may occur spontaneously within FD lesion years after the initial diagnosis and CT scanning remains effective in the diagnosis, monitoring, progression and treatment planning of disease[10].
Surgical treatment of FD consists of either conservative shaving/contouring or radical excision with immediate reconstruction. The choice of surgical option depends on several factors: site of involvement, rate of growth, aesthetic disturbance, functional disruption, patient preference, general health of the patient, surgeon's experience and the availability of a multi-disciplinary team (neurosurgeon, ophthalmologist, maxillofacial surgeon and orthodontist). Medical treatment has a role in the management of craniofacial FD. Some authors have reported their experience with the use of steroids, mainly in the treatment of visual symptoms from optic nerve compression.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Grabias SL, Campbell CJ. Fibrous dysplasia. Orthop Clin North Am. 1997;8:771–83. [PubMed] [Google Scholar]
- 2.Hudson TM, Stiles RG, Monson DK. Fibrous lesions of bone. Radiol Clin North Am. 1993;31:279–97. [PubMed] [Google Scholar]
- 3.Araghi HM, Haery C. Fibro-osseous lesions of craniofacial bones.The role of imaging. Radiol Clin North Am. 1993;31:121–34. [PubMed] [Google Scholar]
- 4.Machida K, Makita K, Nishikawa J, Ohtake T, Olio M. Scintigraphic manifestation of fibrous dysplasia. Clin Nucl Med. 1986;11:426–9. doi: 10.1097/00003072-198606000-00015. [DOI] [PubMed] [Google Scholar]
- 5.Murray DJ, Edwards G, Mainprize JG, Antonyshyn O. Advanced technology in the management of fibrous dysplasia. J Plast Reconstr Aesthet Surg. 2008;61:906–16. doi: 10.1016/j.bjps.2007.08.029. [DOI] [PubMed] [Google Scholar]
- 6.Abdelkarim A, Green R, Startzell J, Preece J. Craniofacial polyostotic fibrous dysplasia: A case report and review of the literature. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008;106:e49–55. doi: 10.1016/j.tripleo.2008.03.023. [DOI] [PubMed] [Google Scholar]
- 7.Park BY, Cheon YW, Kim YO, Pae NS, Lee WJ. Prognosis for craniofacial fibrous dysplasia after incomplete resection: age and serum alkaline phosphatase. Int J Oral Maxillofac Surg. 2010;39(3):221–6. doi: 10.1016/j.ijom.2009.12.008. [DOI] [PubMed] [Google Scholar]
- 8.Zadi S, Trimeche M, Mokni M, Sriha B, et al. Eighteen cases of craniofacial fibrous dysplasia. Rev Stomatol Chir Maxillofac. 2009;110(6):318–22. doi: 10.1016/j.stomax.2008.11.005. [DOI] [PubMed] [Google Scholar]
- 9.Robey PG, Kuznetsov S, Riminucci M, Bianco P. The role of stem cells in fibrous dysplasia of bone and the Mccune-Albright syndrome. Pediatr Endocrinol Rev. 2007;4(Suppl):386–94. [PubMed] [Google Scholar]
- 10.Diah E, Morris DE, Lo LJ, Chen YR. Cyst degeneration in craniofacial fibrous dysplasia: clinical presentation and management. J Neurosurg. 2007;107(3):504–8. doi: 10.3171/JNS-07/09/0504. [DOI] [PubMed] [Google Scholar]


