Abstract
Background
HIV related renal disease is a common occurrence in patients with HIV infection. It is the third leading cause of end stage renal disease among African-American males between the ages of 20 and 64 years in USA. Renal function impairment has been reported at all stages of HIV infection. The aim of this study is to determine the relationship between severity of renal function impairment and CD4 cell count in HIV infected patients.
Method
HIV patients presenting at University of Benin Teaching Hospital Benin, City Nigeria from 1st January to 30th June 2007 were randomly selected and screened for renal functional impairment (RFI). Those with RFI detected by glomerular filtration rate < 60ml/min/1.73m2 or urine protein creatinine ratio 3 200 were stratified into mild, moderate and severe RFI. Forty patients from each stratum and forty HIV infected patients with normal renal functions were recruited as subjects and control respectively. Their clinical and laboratory parameters were evaluated. The data obtained were analysed using SPSS vs 15.0.
Results
Of the HIV patients screened, 53.3% had renal functional impairment. of these, 40.2% had mild, 37.7% had moderate and 22.2% had severe impairment in their renal functions respectively Their mean age was 36.0±8.8 years. The CD4 cell count was found to be 309.75 ± 268.71/ul, 188.45 ± 173.12/ul, and 141.10±126.01/ul among subjects with mild, moderate and severe RFI respectively. The CD4 cell count in control group was 319.05 ± 248.41/ul. The difference was statistically significant. (p = <0.001). CD4 cell count had a significant positive correlation with GFR (r = 0.32, p = 0.042). However, there was a negative correlation between CD4 cell count and proteinuria but this was not statistically significant (r = 0.09, p = 0.173).
Conclusion
Severity of RFI has a positive correlation with degree of immunosuppression in HIV infected patients.
Keywords: Impaired kidney function, Human immunodeficiency virus infection, CD4 cell count
Introduction
Human Immunodeficiency Virus (HIV) was identified in 1983 as a causative agent for Acquired Immunodeficiency Syndrome (AIDS). This virus progressively damages cells of the body's immune system thus predisposing the infected individual to opportunistic infections, cancers, and various organ pathology.1
In 1984 Rao et al reported a renal lesion in patients infected with HIV that was characterized with severe proteinuria, biochemical features of nephrotic syndrome, and RFI that rapidly progresses to end stage renal disease2. Various types and severities of renal disorders have been encountered at all stages of HIV infections, ranging from mild and transient renal impairment to end stage renal disease requiring renal replacement therapy2–5.
The CD4 cell count is used as a surrogate marker of immune statue in HIV infected patients. However infection with HIV leads to destruction and depletion of CD4 cells and this predisposes the individual to various disease conditions6, 7. CD4 cell count has been used to monitor, follow up and determine the severity of HIV infection.7
The RFI has been encountered at various stages of HIV infection, from the stage of seroconversion to advanced AIDS8. The prevalence, severity, morbidity and mortality of renal function impairment in these patients have been associated with the degree of immunosuppression.9, 10, 11 Various studies have reported that CD4 cell count of less than 200/ul is a poor prognostic index in HIV infected patients with renal disease.10, 11,12 13
Early detection and intervention delays progression and in many situations reverses impairment of renal function in HIV infected patients14. The CD4 cell count of HIV infected patients is assessed on presentation in most health facilities. However renal function assessment is sparse in many centres in Nigeria attending to HIV patients. It is necessary to to objectively assess the relationship between renal function and degree of immunosuppression in these patients. This may provide an empirical approach for early diagnosis and management of RFI in HIV infected patients using the CD4 cell count as a guide.
This study aimed to determine the relationship between the severity of renal functional impairment and CD4 cell count among HIV infected patients at the University of Benin Teaching Hospital, Benin City.
Methods
The study population comprised of HIV seropositive patients aged 15 years and above diagnosed by enzyme linked immunosorbent assay and confirmed by immunocomb II presenting at University of Benin Teaching Hospital (out/inpatients) from 1st January 2007 to 30th June 2007, who had RFI. However, patients with conditions that affect renal function not related to HIV (diabetes mellitus, hypertension, heart failure, sickle cell disease, malignancies unrelated to HIV, urinary tract obstruction), past history of kidney disease or features suggestive of kidney disease, urinary tract infection, hepatitis B and C infections, pregnant patients, and patients with conditions that affect CD4 cell count independent of HIV infection (steroid therapy, anti TB therapy), were excluded from the study. Ethical clearance was obtained from the ethical committee of the hospital. The study was explained to the patients and consent obtained from each patient.
HIV seropositive patients who met the study criteria and presented within the study period were randomly selected and screened for RFI. Patients selected had physical and laboratory (serum creatinine, urea, albumin; spot urine protein and creatinine, using colorimetric method (Randox); and CD4 cell count using fluocytometric method) evaluation. The glomerular filtration rate (GFR) was estimated using 6 variable of Modification of Diet in Renal Disease (MDRD) equation. The urine protein excretion was estimated using protein creatinine ratio (PCR) of spot urine
The RFI was detected using GFR <60ml/min/1.73m2 or PCR 200. Patients with RFI were then stratified into mild (GFR 3 60ml/min/1.73m2 but PCR 3 200), moderate (GFR 30 to 59ml/min/1.73m2) and severe (GFR < 30ml/min/1.73ml/min/1.73m2). Forty patients from each stratum were recruited by simple random sampling for the study. Also forty HIV infected patients with normal renal functions (GFR >60ml/min/1.73m2 and PCR < 200) were also recruited as control.
The data obtained was analysed using SPSS Vs 13.0. The frequency distributions of demographic variables were computed. Chi square and analysis of variance (ANOVA) were used to test the means of CD4 cell count as they vary with severity of RFI. The relationships between CD4 cell count and renal functions were assessed using Spearman's rank correlation coefficient. P value < .05 was considered significant.
Results
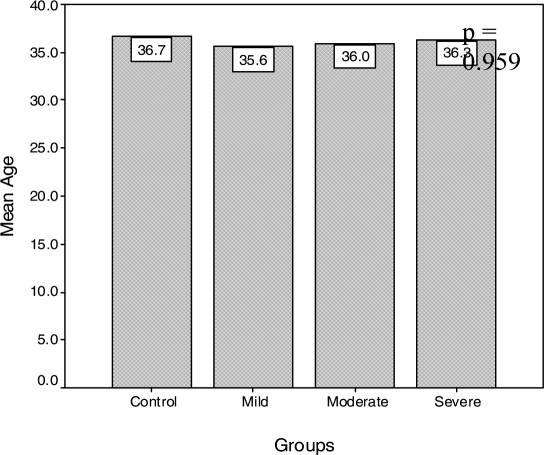
A total of 383 patients were screened, 204(53.3%) patients had RFI, 40.2% of them mild, 37.7% moderate and 22.2% severe. The mean age of subjects was 36.0±8.8 years. However the mean ages for various severities of RFI were 35.6±8, 36.0±9.9 and 36.3±8.3 years for patients with mild, moderate, and severe RFI respectively (fig. 1).
Figure 1.
Mean age of subjects with renal impairment and control groups
The mean systolic blood pressure was 115.33±17.17, 109.64±17.08, 112.11±11.23 and 118.00±17.08mmHg for control, mild, moderate and severe RFI respectively. The difference was not statistically significant (P = 0.605). The mean diastolic blood pressure was 72.33±14.31, 74.19±12.21, 68.15±10.15 and 72.52±21.15mmHg for control, mild, moderate and severe RFI respectively. There was no significant difference (P = 0.345). The mean random blood sugar was 6.81 ±1.20, 7.22±0.97, 8.10±1.55 and 6.25±2.01 mmol/l for control, mild, moderate and severe RFI respectively. The difference was not statistically significant (P = 0.122).
Control - GFR 360ml/min/1.73m2 & PCR < 200mg/g Mild - GFR 360ml/min/1.73m2 and PCR 3200mg/g, Moderate - GFR 30 - 59ml/min/1.73m2, Severe - GFR <30ml/min/1.73m2
The distributions of CD4 cell count were 319.05 ± 248.41/ul, 309.75±268.71/ul, 188.45±173.12/ul, and 141.10±126.01/ul for control, mild RFI, moderate RFI and severe RFI respectively (table 1). These were statistically significant. (p = <0.001).
Table 1.
The distributions of CD4 cell count in groups of patients with RFI
| Parameters | Control | Mild | Moderate | Severe | P value |
| n = 40 | n = 40 | n = 40 | n = 40 | ||
| (Mean S±SD) | (Mean S±SD) | (Mean S±SD) | (Mean S±SD) | ||
| CD4 cell | 319.05±248.41 | 309.75±268.71 | 188.45±173.12 | 141.10±126.01 | <0.001 |
| count (/ul) |
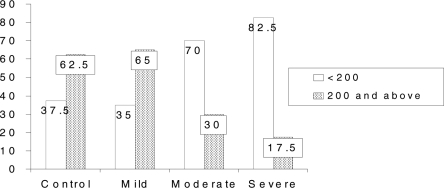
Figure 2 shows that 82.5% of subjects with severe RFI and 70.0% of subjects with moderate RFI had CD4 cell count below 200/ul, but 60.0% of subjects with mild RFI and 62.5% of control had CD4 cell count 200/ul and above. The difference was statistically significant, p = <0.001
Figure 2.
Distribution of groups of RFI in relation to CD4 cell count
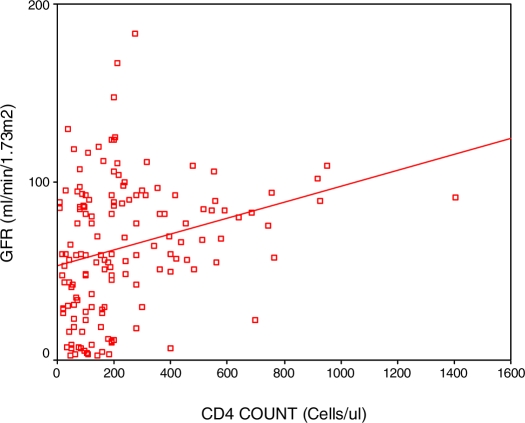
There was a significant positive correlation between CD4 cell count and GFR (r = 0.46 and p = 0.031) (fig. 3)
Figure 3.
Relationship between GFR and CD4 cell count
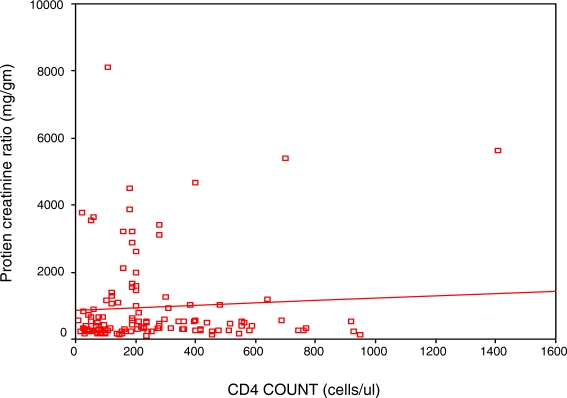
There was no significant correlation between CD4 cell count and proteinuria (r = 0.17, p = 0.148). (Fig. 4)
Figure 4.
Relationship between Protein creatinine ratio and CD4 cell count
Discussion
The prevalence rate of 53.3% of RFI in HIV infected patients as reported in this study is high in contrast to some other studies that reported a prevalence rate of 10 to 30% 5, 10, 14. A study in North Central Nigeria by Agaba et al15 however, reported 52% as a prevalence rate of renal disease in HIV infected patients, which is similiar to our study. The use of urinary protein excretion rate of 200mg/g (PCR) as a measure of RFI must have included patients that hitherto have been excluded by using proteinuria measured by dipstick assessment. Many of the earlier studies mentioned above detected proteinuria with dipstick, which may have contributed to the lower prevalence of RFI as reported in some studies. The socioeconomic state and ethnicity of the studied population could be a predisposing factor to higher risk of RFI. The distribution of the severity of RFI is consistent with the findings in NHANES study in which patients with National Kidney Foundation K - DOQI stages 1, 2 and 3 (mild and moderate) constitute about 80% of the CKD population in USA.16
The CD4 cell count was above 300cells/ul in patients with normal renal function and mild RFI while CD4 cell count in patients with moderate and severe RFI was below 200 cells/ul. This is consistent with earlier studies that reported impaired renal function in HIV infected patients with significant immuno suppression, having CD4 cell count less than 200ul/l8,10 11, 17. There was then an inference that CD4 cell had a protective role in the development of renal diseases except acute tubular ischaemia18. This study also supported by various reports that CD4 cell count less than 200cells/ul is associated with development of opportunistic infections, malignancies and other organ diseases that affects kidney functions. Muloma et al in Kenya and Chaparro et al reported that in addition to CD4 cell count of less than 200cells/ul, high viral load and proteinuria in HIV infected patients were other variables that are associated with progressive renal impairment19, 20. However, RFI including HIV associated nephropathy was recently reported in HIV patients with normal or mildly impaired immune state with CD4 cell count above 200cells/ul and who usually were asymptomatic18, 21, 22.
Proteinuria was found to be higher in this study in patients with lower CD4 cell count. However there was no statistically significant correlation between proteinuria and level of CD4 cell count in this study. Muloma et al19 reported a similar finding in their study in which proteinuria was found to be higher in patients with CD4 cell count less than 200/ul, but had no significant correlation with severity of immunosupression. Some other studies had reported an inverse relationship between proteinuria and CD4 cell count 9, 20. The method of assessing the urine protein excretion (dipstick or PCR) may have influenced the outcome of the studies.
Appropriate renal function assessment in patients with HIV infection is usually not done in many centres attending to these patients; the assessment of renal functions in these centres were mainly on patients with severe HIV/AIDS or those with clinical features suggestive of RFI. This has led to missed or delayed diagnosis of RFI in HIV infected patients in these centres.
Conclusion
This study revealed that RFI especially the mild type, occurs in HIV patients with normal or mildly impaired immune state with CD4 cell count above 300cells/ul. However severity of RFI in HIV infected patients was found to be higher in patients with severe immunosuppression as detected by CD4 cell count less than 200cells/ul.
Thus there is a need for assessment of renal functions in all HIV infected patients at presentation, irrespective of their immune status. This will encourage early detection, prompt intervention and possibly reversal of the RFI.
References
- 1.HIV/AIDS Overview. Emedicine Consumer Health. 2004:1–2. [Google Scholar]
- 2.Rao TKS, Fillipone EJ, Nicastri AD, et al. Associated focal and segmental glomerulosclerosis in Acquired Immunodeficiency Syndrome. N Engl J Med. 1984:1631–1645. doi: 10.1056/NEJM198403153101101. [DOI] [PubMed] [Google Scholar]
- 3.Winston JA, Klotman PE. Are we missing an epidemic of HIVAN? J Am Soc Nephro. 1996;1:1–7. doi: 10.1681/ASN.V711. [DOI] [PubMed] [Google Scholar]
- 4.Seney FD, Jr, Burns DK, Silva FG. Acquired Immunodeficiency Syndrome and the kidney. AM J Kidney Dis. 1990;16:1–1. doi: 10.1016/s0272-6386(12)80779-7. [DOI] [PubMed] [Google Scholar]
- 5.Weiner NJ, Goodman JW, Kimmel PL. The HIV associated renal diseases; current insight into pathogenesis and treatment. Kidney Int. 2002;63:1618–1631. doi: 10.1046/j.1523-1755.2003.00901.x. [DOI] [PubMed] [Google Scholar]
- 6.Onyemelukwe GC, Musa BOP. CD4 / CD8 Lymphocytes / Clinical features of HIV seropositive Nigerians on presentations. Afr J Med Sci. 2002;31:229–233. [PubMed] [Google Scholar]
- 7.Nnorti JP, Butler JC, Gelling L, Kool JL, Reginald AL, Vugis DJ. Invasive pneumococcal disease in HIV/AIDS patients. Ann Int Med. 2000;132(3):182. doi: 10.7326/0003-4819-132-3-200002010-00003. [DOI] [PubMed] [Google Scholar]
- 8.Winston JA, Klotman ME, Klotman PE. HIV associated nephropathy is a late not early manifestations of HIV - 1 infection. Kidney Int. 1999;55:1036–1040. doi: 10.1046/j.1523-1755.1999.0550031036.x. [DOI] [PubMed] [Google Scholar]
- 9.Luke DR, Sarnoski TP, Dennis S. Incidence of microalbuminuria in ambulatory patients with acquired immunodeficiency syndrome. Clin Nephrol. 1992;38:69–74. [PubMed] [Google Scholar]
- 10.Szczech LN, Gupta SK, Habash R, et al. The clinical epidemiology and course of the spectrum of renal diseases associated with HIV infection. Kidney Int. 2004;66:145–152. doi: 10.1111/j.1523-1755.2004.00865.x. [DOI] [PubMed] [Google Scholar]
- 11.Jones R, Scott C, Nelson N, Levey J. Renal complications of HIV. Int J Clin Pract. 2007;61(6):991–998. doi: 10.1111/j.1742-1241.2007.01376.x. [DOI] [PubMed] [Google Scholar]
- 12.Nueremberger E. Concepts in HIVAN. The Hopkins HIV report. 1999. pp. 1–6. http://www.google.com July 2007.
- 13.Ifudu O, Mayers JD, Mathew JJ, et al. Uraemia therapy in patients with end stage renal disease and HIV infection: has the outcome changed in 1990's? Am J kidney Dis. 1997;29(40):549–552. doi: 10.1016/s0272-6386(97)90336-x. [DOI] [PubMed] [Google Scholar]
- 14.Winston JA, Bruggeman LA, Ross MD, et al. Nephropathy and establishment of a renal reservoir of HIV type 1 during primary infection. NEJM. 2001;344(26):1979–1983. doi: 10.1056/NEJM200106283442604. [DOI] [PubMed] [Google Scholar]
- 15.Agaba EI, Agaba PA, Sirisena ND, Antenyi EA, Idoko JA. Renal disease in AIDS patients in North Central Nigeria. Nig J Med. 2003;12(3):120–125. [PubMed] [Google Scholar]
- 16.Nickolas TL, Frisch GD, Opotowsky AR, Arons R, Radhakrishnan J. Awareness of kidney disease in the US population: findings from National Health and Nutritional Examination Survey (NHANES) 1999 to 2000. Am kidney Dis. 2004;44:185–197. doi: 10.1053/j.ajkd.2004.04.023. [DOI] [PubMed] [Google Scholar]
- 17.Krawczyk CS, Holmberg SD, Mooman AC, Gardner LI, McGwin G. Factors associated with chronic renal failure in HIV infected ambulatory patients. AIDS. 2004;18(16):2171–2178. doi: 10.1097/00002030-200411050-00009. [DOI] [PubMed] [Google Scholar]
- 18.Wang Y, Feng X, Bao S, et al. Depletion of CD4 (+) T cells aggravates glomerular and interstitial injury in murine adriamycin nephropathy. Kidney International. 2005;67(S96–S100):1523–1755. doi: 10.1046/j.1523-1755.2001.059003975.x. [DOI] [PubMed] [Google Scholar]
- 19.Muloma E, Owumo Ong'or W, Sidlee J, et al. Renal disease in an ART naïve HIV infected population in western Kenya; IAS conf HIV pathog Treat: Abst MOPE 11.6c23; 2005. [Google Scholar]
- 20.Chaparro WA, Zilleruelo G, Riviera D, et al. HIV nephropathy in children detected by quantitative proteinuria; 11th conf on retrovirus and opportunistic infections. Abst; 752: session 104. [Google Scholar]
- 21.Ham TM, Naicker S, Ramdial PK, Assoung AG. A cross sectional study of HIV seropositive patients with varying degrees of proteinuria in South Africa. Kidney Int. 2006;69:2243–2250. doi: 10.1038/sj.ki.5000339. [DOI] [PubMed] [Google Scholar]
- 22.Bourgoigni J, Rao TKS, Roth D. Renal disease in patients with hepatitis and human immunodeficiency virus [HIV] Atlas of the diseases of the kidney. 2005. On - line edition.