Abstract
Mandibular fractures are relatively less frequent in children when compared to adults, which may be due to the child's protected anatomic features and infrequent exposure of children to alcohol related traffic accidents. Treatment principles of mandibular fractures differ from that of adults due to concerns regarding mandibular growth and development of dentition. A case of a 4.5-year-old boy with fractured body of mandible managed by closed reduction using open occlusal acrylic splint and circum mandibular wiring is presented. This article also provides a review of literature regarding the management of mandibular body fracture in young children.
Keywords: Circum mandibular wiring, mandibular body fractures, open occlusal acrylic splint, pediatric dental trauma
Introduction
The reported incidence of pediatric injuries accounts for 4–6% of the total. Below the age of 5 years, the incidence of pediatric facial fractures is even lower, ranging from 0.6 to 1.2%.[1] The principles of management of mandibular fractures differ in children when compared to adults. While in the adults, absolute reduction and fixation of fractures is indicated, in children minimal manipulation of facial skeleton is mandated. The goal of treatment of these fractures is to restore the underlying bony architecture to pre-injury position, in a stable fashion, as non-invasively as possible, with minimal residual esthetic and functional impairment.
Depending on the type of fracture and the stage of skeletal development the treatment modalities range from conservative non-invasive through closed reduction and immobilization methods to open reduction with internal fixation. Disruption of the periosteal envelope of the mandibular body may have an unpredictable effect on growth. Thus, if reduction is required, closed reduction is favored.
Case Report
A 4.5-year-old boy reported to the dental clinic with bleeding from oral cavity following fall from bicycle. Clinical examination revealed bruise on the chin, open mouth appearance with profuse bleeding from the oral cavity and derangement of occlusion [Figure 1]. Step deformity with tenderness and mobility was elicited along the lower border of the mandible on the left side canine region. Preoperative orthopantamogram (OPG) could not be taken due to the profuse bleeding needing immediate intervention.
Figure 1.

Preoperative photograph following trauma
Under sedation, upper and lower arch alginate impressions were taken and stone casts were poured. An open occlusal acrylic splint was fabricated [Figure 2], and under general anesthesia, the mandibular body fracture was immobilized, fixed with the acrylic splint which was retained by circum mandibular wiring [Figures 3 and 4]. Patient was reviewed every week, and on the third postoperative week, the circum-mandibular wiring and splint was removed under local anesthesia. No mobility was present at the fracture site. Postoperative recovery was uneventful and occlusion achieved was satisfactory, although spacing was seen in incisor–canine region [Figure 5]. Patient was reviewed monthly for 6 months. On 2 months follow-up, the spacing had closed and the child had good alignment of teeth [Figure 6]. Patient had perfect occlusion and good masticatory efficiency.
Figure 2.

Mandibular cast with open occlusal acrylic splint
Figure 3.
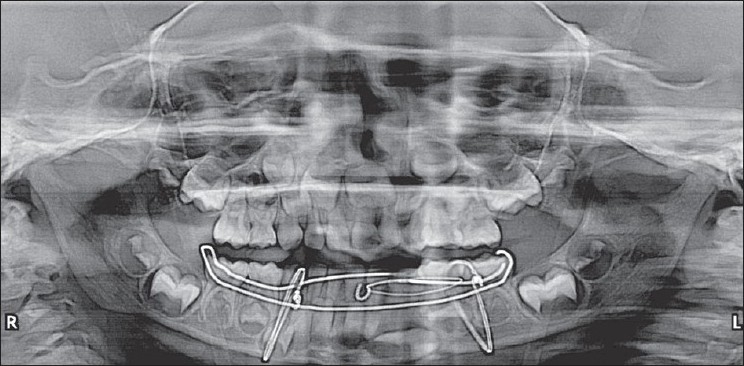
Postoperative photograph after circum mandibular wiring
Figure 4.
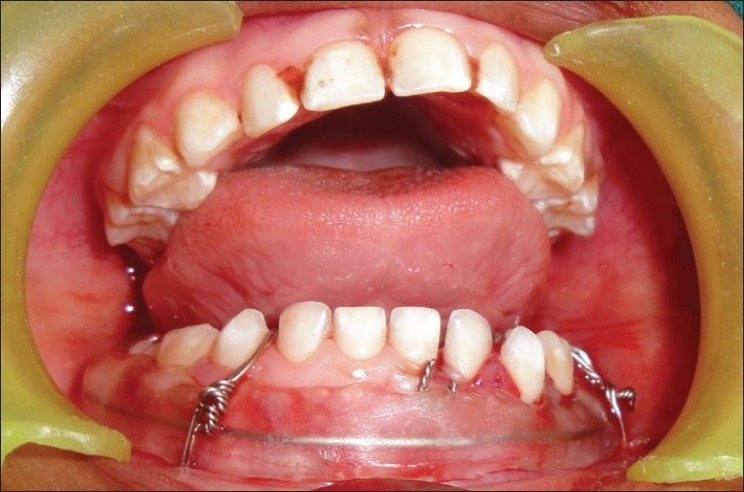
Postoperative orthopantamogram showing circum mandibular wiring
Figure 5.

Spacing evident in incisor–canine region following wire and splint removal
Figure 6.

Follow-up after 2 months showing space closure
Review of literature
Facial fractures in children account for the approximately 5% of all facial fractures.[2] A male predilection is seen in all age groups. The most common fracture in children requiring hospitalization and/or surgery generally involves the mandible and, in particular, the condyle. Fractures in the condylar region are the most common, followed by angle and body fractures. The etiologies of mandibular fractures in children are usually falls and sports injuries.
The protective anatomic feature of a child's face decreases the incidence of facial fractures. In young children (less than 5 years of age), the face is in a more retruded position relative to the “protective” skull, therefore, there is a lower incidence of midface and mandibular fractures and a higher incidence of cranial injuries. With increasing age and facial growth directed in a downward and forward direction, midface and mandible becomes more prominent; thus, the incidence of facial fractures increases, while that of cranial injuries decreases.[3] The high elasticity of young bones, a thick layer of the adipose tissue covering them, a high cancellous-to-cortical bone ratio and flexible suture lines are some of the reasons contributing to the low incidence of facial fractures and minimal displacement of the fracture fragments.[4–5]
The clinical features of a fractured mandible in a child are the same as in an adult, which includes pain, swelling, trismus, derangement of occlusion, sublingual ecchymosis, step deformity, midline deviation, loss of sensation due to nerve damage, bleeding, TMJ problems, tenderness, movement restriction, open bite and crepitus. Thorough clinical examination, however, may be impossible in uncooperative young trauma patients. Lacerations should be evaluated to reveal injuries to underlying structures. General palpation should be applied over all bony surfaces of the mandible. The mandibular range of motion must be examined as patients actively open and close their mouth.
For children, the imaging technique which is of value, especially following trauma, is a computed tomography (CT) scan, since plain radiographs in young children are less helpful than in adults due to unerupted tooth buds obscuring fractures, the increased incidence of greenstick fractures and the fact that the cortex is underdeveloped, leading to difficulty in visualizing fractures.[6]
Treatment of mandibular fracture in children depends on the fracture type and the stage of skeletal and dental development.[7] Mandibular growth and development of dentition are the main concerns while managing pediatric mandibular fractures. In adults, absolute reduction and fixation of fracture is indicated, whereas in children minimal manipulation of the facial skeleton is mandated. The small size of the jaw, existing active bony growth centers and the crowded deciduous teeth with permanent tooth buds located in great proximity to the mandibular and mental nerves, all significantly increase the therapy related risks of pediatric mandibular fractures and their growth related abnormalities.
Intact active mandibular growth centers are important for preserving mandibular function, which have a significant influence on future facial development. Thus, restoration of the mandibular continuity after fracture is important not only for immediate function but also for future craniofacial development. Accordingly, the goal of treatment is to restore the underlying bony architecture to its pre-injury position in a stable fashion as non-invasively as possible with minimal residual esthetic and functional impairment.
Problems encountered in management of pediatric mandibular fractures
Loose anchorage system due to attrition of deciduous teeth and physiologic resorption of roots.[7]
Precarious dental stability in the mixed dental development period.
Difficulties in securing IMF using arch bars and eyelets as primary teeth are not sufficiently stable and may be avulsed due to the pressure exerted. In addition, the partially erupted secondary teeth are not sufficiently stable in the pediatric soft bone.[2,7]
Shape of the primary teeth: Conical shape with wide cervical margins and tapered occlusal surface makes placement of wires technically challenging.[4]
Restricted normal dietary intake in children on IMF was reported to result in significant weight and protein loss and reduced tidal volume.[7]
Children on IMF are at an increased risk of aspirating gastric contents should they vomit.[7]
The wires cause discomfort and damage periodontal tissues.[2,7]
Despite the fact that the goal of treatment is to establish the bony architecture to pre-injury state as non-invasively as possible, the challenges with closed reduction and IMF are many. However, some authors have indicated that IMF using arch bars is safe in children, especially those older than 9 or 11 years.
Alternative devices for closed reduction
Several studies have recommended the use of pre-fabricated acrylic splints as a treatment for pediatric mandibular fractures. These splints are more reliable than open reduction or IMF techniques with regard to cost effectiveness, ease of application and removal, reduced operating time, maximum stability during healing period, minimal trauma for adjacent anatomical structures and comfort for young patients.[8]
Laster et al,[9] described nickel titanium staples which are inserted in a relatively non-invasive and pain free manner and their eventual removal, if required, is done as quickly as their insertion, facilitated by the fact that the staples are not osseointegrated. Due to their superficial location, there is little risk for inhibiting and deforming facial bone development or having any proximal strategic structures such as nerves and developing dentition. Furthermore, the reduced compression rendered by the staples on the bony fragments result in primary healing with no callus produced.
Modified orthodontic brackets have been used for maxillomandibular fixation (MMF).[10]
Orthodontic resin has been used for fixation of mandibular fractures in children.[2]
Orthodontic rubber elastics in combination with fixed orthodontic brackets were used to create compressive horizontal force marginally over the mandibular fracture site from one side to the other.[2]
A modified orthodontic splint appliance has been applied to fractures where two orthodontic bands are fit on the primary second molars with rounded stainless steel arch wires soldered to them on the buccal and lingual side.[11]
The most common pediatric mandibular fracture: Greenstick fractures
A greenstick fracture is a fracture in which one cortex of the bone is broken and the other cortex is bent. Pediatric patients are more likely than adults to sustain greenstick or incomplete fractures. The relatively high elasticity of the mandibular body's thin cortical bone and a thick surrounding layer of adipose tissue and the relatively larger amount of medullary bone held by a strong periosteal support results in a high incidence of greenstick fractures in children.[5]
A greenstick fracture will ensure stability of the undisplaced segments in children less than 5 years.[5] Furthermore, the osteogenic potential of the periosteum in the developing craniofacial skeleton is very high and will lead to somewhat rapid and easier healing which occurs under the influence of masticatory stress, even when there is imperfect apposition of bone surfaces.[12] Thus, there is a greater degree of tolerance permissible in the alignment of fragments and restoration of occlusion, which will subsequently be corrected by alveolar bone growth at the time of eruption of permanent teeth.[5] Therefore, management of greenstick fractures without displacement and malocclusion would merely be close observation, a liquid-to-soft diet, and avoidance of physical activities (e.g. sports and analgesics).[4] There may be cases in which the fractures can be snapped back into a good reduced position and held by the periosteal sleeve, the fracture surfaces and even by the occlusion.[5] For greenstick/minimally displaced fractures, conservative closed reduction is the most recommended treatment.[9]
The closed reduction and immobilization approach can be achieved by means of acrylic splints, circumferential wiring, arch bar or gunning splints.[9] These techniques provide a good reduced position, continuity of periosteal sleeve and maintenance of the soft tissue, thus creating a positive environment for rapid osteogenesis and remodeling processes as well as prevention of any type of non-fibrous union.[12] Furthermore, in the splinted mandible, the fracture segments are tightly fixed and serve in reducing tenderness and pain reactions during a child's daily activity.[12]
Open reduction management of mandibular body fractures in children
Till the mid-seventies, closed reduction by means of IMF was used for all types of pediatric fractures.[12] Today, open reduction and rigid internal fixation (ORIF) has become the standard of care for management of displaced fractures.[4] ORIF includes micro or miniplates or biodegradable devices which significantly increase the therapy related risks previously mentioned. Nonetheless, this technique provides stable three-dimensional reconstruction, promotes primary bone healing and shortens treatment time. Posnick et al,[6] claimed that a decreased dependence in IMF improved postoperative respiratory care, nutritional intake and oral hygiene measures.
The treatment modality for displaced mandibular fractures is debatable between closed reduction and open reduction. While different open reduction techniques have been the standard of care for adults for a long time, its suitability for children remains controversial.[5] The effect of implanted hardware in the mandible of a growing child is not completely understood. Damage to the periosteum and surrounding soft tissues and potential damage to primary teeth and permanent tooth gums is to be considered when choosing internal fixation.[6,7] Rigid internal fixation might create artifacts on CT scans or magnetic resonance imaging (MRI) and may be visible or palpated through the child's thin skin and cause pain and early or late infection.[4]
Therefore, the decision to use ORIF in children should be taken with great caution and only if other means of reduction and fixation are not attainable. Miniplate and screw devices have revolutionized the modern management of facial fractures by enabling precise anatomical reduction and fixation under direct vision.
Problems with ORIF in pediatric trauma
Presence of developing tooth germs, though the inferior border of the mandible can be plated either through an intraoral/extraoral approach. Additionally, the extraoral approach carries the risk of scarring and damage to the marginal mandibular nerve.[5,7]
Interference with growth due to placement of miniplates.[5]
General anesthesia and hospitalization is needed for removal of the hardware after complete healing.[2]
Allergic reactions to the metal resulting in inflammation that needs removal of plate have been reported.[2]
Stress shielding, especially after rigid plate fixation, has been reported and may cause weakening of the bone after removal of the implant.[2]
Corrosion and release of metal ions can lead to removal of the fixation device.[2]
Recent advances in ORIF
Currently, ORIF with resorbable osteosynthesis plates and screws is increasingly being used in children. These biodegradable materials do not interfere with radiodiagnostic techniques due to their radiolucency and they are sufficiently rigid and stable. They eventually degrade, resorb and are eliminated from the body. Although the secondary implant removal operations are avoided and there are no side effects on the growing skeleton, the risk of damaging tooth buds in the pediatric jaw is still present due to drilling for direct application of the resorbable plates and screws.[2] Eppley[2] claims that this risk is minimal since the drill hole and the tapping of the screw penetrate only the outer cortex of the bone. Even if the resorbable screw tip encroaches upon a tooth, its tip is blunt and non-penetrating. Subsequent resorption of the screw removes any potential obstruction to tooth eruption.
Despite the above reports, the literature advocates conservative management of mandibular body fractures at young ages with the added advantage of decreased immobilization time, decreased muscular atrophy and better oral hygiene.[2]
Complications
Complications per se are very rare in pediatric trauma due to the child's greater osteogenic potential, faster healing rate and less frequent requirement of ORIF. Furthermore, a greater number of fractures are minimal to non-displaced. Late complications such as damage to permanent teeth may occur in 50% of mandibular fractures. TMJ dysfunction (recurrent subluxation, noise and pain, limited condylar translation, deviation on opening, ankylosis) and growth disturbances (e.g. secondary mid face deformity, mandibular hypoplasia and asymmetry) usually occur in pediatric patients with severely comminuted fractures.[2,7]
Malocclusion as a complication of pediatric facial fractures is rare. It has been attributed to short fixation time in alveolar fractures and may be caused by growth abnormalities following condylar fractures.[3] Spontaneous correction of malocclusion is seen as deciduous tooth shed and permanent teeth erupt.[7] Ellis et al,[2] did not find occlusal complication associated with the use of closed treatment and IMF.
Lois et al,[2] found no difference in the complication rates of fractures treated by MMF versus ORIF (4.3% and 5.45%, respectively). They concluded that in fractures with displacement in the range of 2–4 mm, there is no difference between MMF and ORIF.
A recent study of mandibular fracture complications in children[2] noted a lower complication rate (9.1%) with closed treatment of mandibular body, angle and parasymphyseal fractures, while open reduction using miniplate, mandibular plate and mandibular/miniplate fixation revealed a higher rate of complication (30%, 28.6% and 29.2%, respectively). Infection and wound dehiscence occur less frequently with closed versus open.
Nonunion occurs significantly less often in closed reduction than in open treatment. Nonunions of the mandible may develop due to a number of factors, including poor patient compliance with postoperative care, metabolic disturbances and generalized disease states, which can all lead to inadequate bone healing.[2] Other local causes for non union may be related to inadequate immobilization of fracture segments, infections at the fracture site, tissue or foreign body between the segments and the inadequate reduction the fracture segments.[2]
However, Ellis et al,[2] found lower complication rates in patients with comminuted mandibular fracture, who underwent open reduction and fixation (10.3%) than in those who were treated with closed reduction with IMF (17.1%). Yerit et al,[2] found uneventful healing and no complications when using resorbable osteosynthesis plates and screws for ORIF, while others described the same type of complications as mentioned for non-resorbable miniplates infections due to mucosal exposure of the plates, premature occlusal contact and TMJ disorders.[2]
Long-term follow-up on facial and teeth development
A long-term follow-up period is recommended postoperatively in cases of mandibular body fractures in children.[8] Facial growth pattern and mandibular movements should be recorded. Ranta and Ylipaavalniemi[2] pointed out that teeth in which root development has already begun at the time of fracture, appear to erupt normally; however, marked deformation of the crown and roots occur in teeth located on the fracture line when the calcification process is still in progress at the time of fracture.
Developmental disturbances occur in the lower tooth buds at the pre-calcification stages involved in the fracture and internal fixation site, which include damage to the pulp causing pulp obliteration and extensive root resorption as well as impaction. Koenig et al,[2] pointed out that the developing follicle is more elastic than the surrounding bone and better able to survive mechanical injury. Nevertheless, it is difficult to predict the facts of tooth buds and fracture and the implanted hardware fixation.
Suei et al,[2] mentioned that the presence of infection in the fracture site is a crucial factor affecting odontogenic cells in the dental follicle. Surgical procedures as well as fixation and reduction are also potential causes of impaction. Eleonora Schiller et al,[13] report that trauma occurring between 0 and 3 years of age is likely to disturb the formation and mineralization of the permanent teeth.
Nixon and Lowey[2] concluded that mandibular fractures which occur during mixed dentition can be associated with subsequent failed eruption of permanent teeth when the fracture line is reduced using an open surgical approach.
Yocheved Ben Bassat et al,[14] reported discoloration of the crown of permanent tooth in 16% of the children with the incisal one third being the most common site. Hypoplasia was evident in 9% of the permanent teeth.
In our case, the deciduous teeth seem to have aligned well over a period of 2 months, thereby closing the spacing initially seen between the teeth. We opted for the open occlusal acrylic splint because of its ease in lab fabrication, preservation of periodontal tissue integrity, patient compliance and ease in assessing the occlusion after reduction.
Conclusion
The anatomical complexity of the developing mandible and teeth and concerns regarding biocompatability of implanted hardware often mandate the use of surgical techniques that differ markedly from those used in adults. In cases of mandibular fractures of a young child, disruption of periosteal envelope may have unpredictable effects on growth. Thus, if intervention is required, closed reduction is favored. Due to the technical difficulties of IMF, acrylic splints with circumferential wiring are recommended.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Tandon S. Textbook of Pedodontics. 1st ed. Hyderabad: Paras Medical Publisher; 2001. p. 490. [Google Scholar]
- 2.Aizenbud D, Hazan-Molina H, Emodi O, Rachmiel A. The management of mandibular body fractures in young children. Dental Traumatol. 2009;25:565–70. doi: 10.1111/j.1600-9657.2009.00815.x. [DOI] [PubMed] [Google Scholar]
- 3.McGraw BL, Cole RR. Pediatric maxillofacial trauma, age related variations in injury. Arch Otolaryngol Head Neck Surg. 1990;116:41–5. doi: 10.1001/archotol.1990.01870010045014. [DOI] [PubMed] [Google Scholar]
- 4.Zimmermann CE, Troulis MJ, Kaban LB. Pediatric facial fractures, recent advances in prevention, diagnosis and management. Int J. Oral Maxillofacial Surg. 2006;35:2–13. doi: 10.1016/j.ijom.2005.09.014. [DOI] [PubMed] [Google Scholar]
- 5.Crean ST, Sivarajasingam V, Fardy MJ. Conservative approach in the management of mandibular fractures in the early dentition phase: A case report and review of the literature. Int J Pediatr Dent. 2000;10:229–33. doi: 10.1046/j.1365-263x.2000.00196.x. [DOI] [PubMed] [Google Scholar]
- 6.Posnick JC, Wells M, Pron GE. Pediatric facial fractures: Evolving patterns of treatment. J Oral Maxillofacial Surg. 1993;51:836–44. doi: 10.1016/s0278-2391(10)80098-9. discussion 44-5. [DOI] [PubMed] [Google Scholar]
- 7.Kaban LB. Diagnosis and treatment of fractures of the facial bones in children 1943-1993. J Oral Maxillofacial Surg. 1993;51:722–9. doi: 10.1016/s0278-2391(10)80409-4. [DOI] [PubMed] [Google Scholar]
- 8.Kocabay C, Atac MS, Oner B, Gungor N. The conservative approach of pediatric mandibular fractures with prefabricated surgical splint: A case report. Dent Traumatol. 2007;23:247–50. doi: 10.1111/j.1600-9657.2005.00445.x. [DOI] [PubMed] [Google Scholar]
- 9.Laster Z, Musaka EA, Nagler R. Pediatric mandibular fractures: Introduction of a novel therapeutic modality. J Trauma. 2008;64:225–9. doi: 10.1097/TA.0b013e318068fc77. [DOI] [PubMed] [Google Scholar]
- 10.Magennis P, Craven P. Modification of orthodontic brackets for use in intermaxillary fixation. Br J Oral Maxillofac Surg. 1990;28:136–7. doi: 10.1016/0266-4356(90)90143-9. [DOI] [PubMed] [Google Scholar]
- 11.Aizenbud D, Emodi O, Rachmiel A. Nonsurgical orthodontic splinting of mandibular fracture in a young child: 10-year follow-up. J Oral Maxillofac Surg. 2008;66:575–7. doi: 10.1016/j.joms.2007.09.022. [DOI] [PubMed] [Google Scholar]
- 12.Rowe NL. Fracture of the jaws in children. J Oral Surg. 1969;27:497–507. [PubMed] [Google Scholar]
- 13.Schiller E, Bratu E, Bratu C, Talpos M. Traumatic injuries to the primary teeth and their impact on permanent teeth. Timisoara Medical Journal. 2003:2. [Google Scholar]
- 14.Ben Bassat Y, Fuks A, Brin I, Zilberman Y. Effect of trauma to the primary incisors on permanent successors in different development stages. Pediatr Dent. 1985;7:37–40. [PubMed] [Google Scholar]


