Abstract
One hundred and sixty human permanent central incisors were enlarged to a 120 file size after crown removal procedure to simulate immature teeth. The root canals were filled with calcium hydroxide and stored for 15 days (phase I), 30 days (phase II), 90 days (phase III), and 180 days (Phase IV). At the end of these selected time periods, calcium hydroxide was cleaned off the root canals of forty teeth that were randomly selected and obturated with gutta-percha points in the apical 2 mm of the root canals with a sealer. The specimens were further equally divided into four groups. Unrestored Group I served as control and the root canals of teeth in the other three group specimens were reinforced with resin modified glassionomer cement (RMGIC) (Group II), Flowable Compomer (Group III), and Flowable Composite (Group IV), respectively, using a translucent curing post. All specimens were subjected to compressive force using an Instron Testing machine, until fracture occurred. All the materials evaluated substantially reinforced the root specimens compared to the control. At the end of 180 days, Flowable composites showed maximum reinforcement compared to the other groups; however, no significant differences were found between the reinforcement capabilities of Flowable Compomer and RMGIC.
Keywords: Calcium hydroxide, Flowable composite, Flowable compomer, immature permanent teeth, intraradicular reinforcement, resin modified glassionomer cement, light transmitting posts
Introduction
Dental trauma is the most frequent cause of pulp necrosis in immature anterior permanent teeth. Deep proximal fractures, especially if left untreated, can jeopardize vitality of the tooth.[1] Endodontic treatment of non-vital immature permanent teeth is often complicated. The walls of the root canals are frequently divergent, and the apices immature, making debridement and obturation difficult. Calcium hydroxide is the material most commonly used for induction of the apical barrier formation in non-vital teeth.[2–4] The long term usage of calcium hydroxide could alter the collagen matrix of dentin due to its high alkalinity.[5–9] This would leave the dentin structure with reduced organic support, which may adversely influence the mechanical properties of dentin(i.e., flexural strength), thus making teeth more susceptible to fracture from secondary injuries.[8–10] The newer adhesive materials can significantly increase the resistance to fracture of these weakened roots to the levels of intact teeth.[10–20] This study compares the reinforcing effects of resin modified glassionomer cement (RMGIC), Flowable compomer, and Flowable composite on the root canal walls of simulated immature central incisor teeth treated with calcium hydroxide for varying periods of time.
Materials and Methods
Human permanent maxillary central incisor teeth extracted due to periodontal disease without signs of caries, obvious defects, or attrition[21] were selected and stored in distilled water until further use. The mesiodistal (MD) and buccolingual (BL) diameters of the specimens were determined at the crown limit of the root using a caliper. The mean values obtained were 6.02 mm for MD and 6.64mm for BL dimensions. Samples presenting a difference of 20% from the mean were discarded,[14] leaving a total of 160 central incisor teeth. The crowns of these specimens were removed to obtain a standard root length of 13 mm [Figure 2]. Root canals were enlarged to a 120 file size at a working length of 12 mm. Copious irrigation with sterile saline was completed between file systems. The canals were then dried with paper points.[22]
Figure 2.
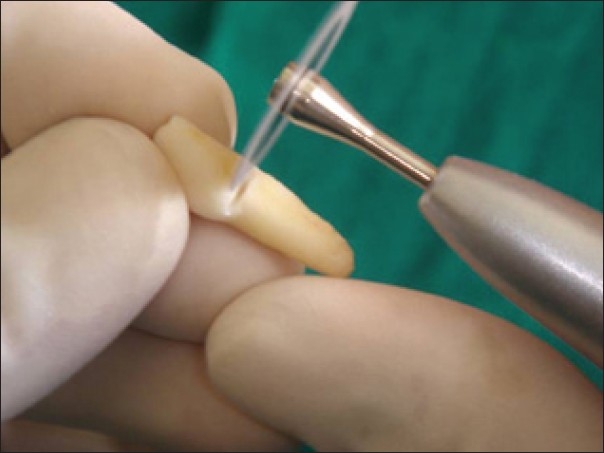
Sectioning of tooth at the cervical level
A thick mixture of pure calcium hydroxide powder mixed with distilled water was condensed into the root canals using plastic amalgam condenser and pluggers till the coronal limit of the root,[23] and then the canals were sealed with restorative glassionomer cement (GIC) at the coronal end. The apical ends of the specimen were sealed with intermediate restorative material (IRM). These specimens were thermo cycled using a regime of 250 cycles from 6°C to 60°C with a dwell time of 30 seconds and stored in a humidator at 37°C.
Phase I
Forty specimens were randomly selected from the lot at the end of 15 days and calcium hydroxide was cleaned off the root canals of the specimens using gentle instrumentation and saline irrigation,[23] and these root specimens were obturated with gutta percha using lateral condensation technique with a ZOE sealer[15] and stored in a humidator at 37°C until further use. At the end of 7 days, gutta-percha was removed using a No.6 Peeso Reamer creating 10 mm of post space, leaving 2 mm of apical gutta-percha fill.
Further grouping of the specimen was done as follows:
Group I-10: non-reinforced root specimens served as control.
Group II-10: root specimens reinforced with RMGIC [Figure 1]. The root canals of the specimens were gently dried using an absorbent point and treated with the primer provided by the manufacturer for 30 seconds, air dried for 15 seconds, and light cured for 20 seconds. Vitremer™ (3M) powder and Vitremer liquid was dispensed according to the manufacturer's instructions and mixed on a paper pad for 45 seconds. The material was back loaded into delivery tip and the restorative was syringed into the root canal.
Group III- 10: root specimens reinforced with Flowable Compomer (Prima Flow®) Preparation of Group III specimens
The root canals of the specimens were gently dried using an absorbent point and treated with the Contax primer and bond according to manufacturer's instructions and light cured for 20 seconds. The canals were filled with Flowable Compomer (Prima Flow®) [Figure 1], which was applied directly from syringe in layers of maximum 2 mm.
Group IV-10: root specimens reinforced with Flowable composite (Filtek™ Z350) [Figure 2]. The 10 root specimens were etched with 37% phosphoric acid (Scotch Bond™ multipurpose) for 15–20 seconds, rinsed with sterile water for 20 seconds, and then blot dried. Two coats of Adper™ Single bond 2 (3M) bonding agent was applied, gently air dried, and light cured for 20 seconds. The specimens were then filled with Flowable Composite (Filtek flow™ Z350 (3M) directly from the syringes.
Figure 1.
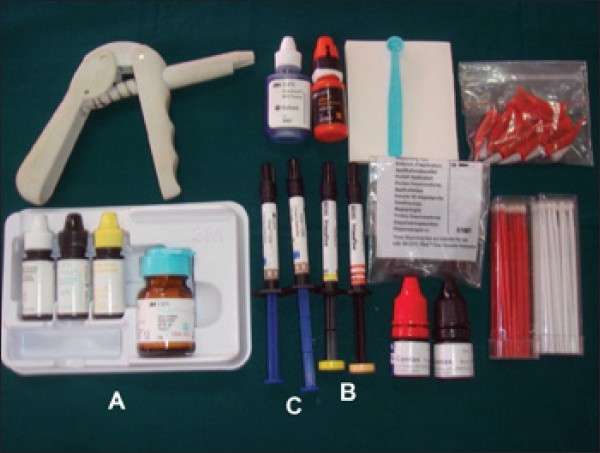
Restorative materials; A - RMGIC, B - Flowable compomer-Flowable composite
To cure the restorative materials, a transilluminating post (Luminex) was used making sure it reaches the cervical limit of the apical filling [Figure 3]. After placing the post inside the canal and removing the excess, the material was light cured according to the manufacturer's instructions. The post was then withdrawn. The root specimens were then re-subjected to thermo cycling regime for 250 cycles at 6°C–60°C, with a dwell time of 30 seconds.
Figure 3.
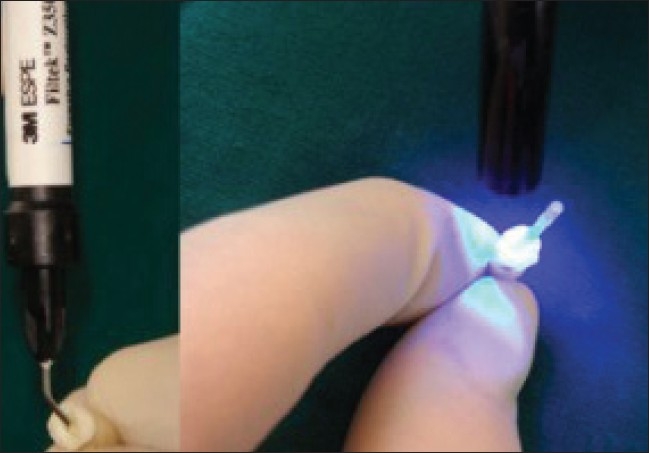
Process of reinforcement and light curing through the post
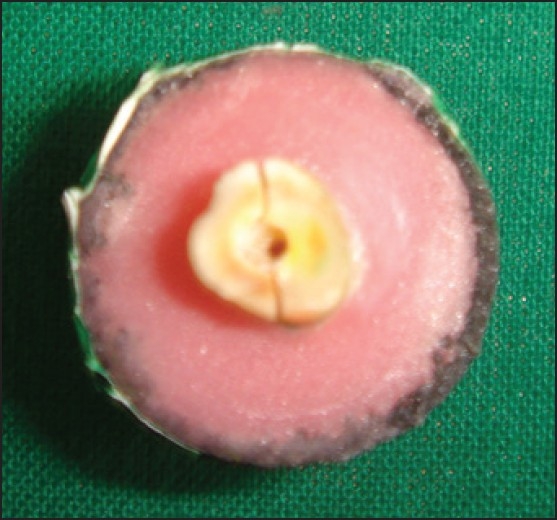
Sample preparation
The roots were embedded in color-coded acrylic blocks using a flat ended rod held vertically by a Ney surveyor to position the roots during mounting so that they were parallel to the acrylic base with an exposure of 4 mm of the cervical portion of root above the acrylic. The acrylic was contained in a ¾ inch diameter PVC pipe 2 cm in length to standardize the size of the base. A stainless steel cone measuring 1.5 cm at the base and 3 cm in length[14] was placed against the canal so that it was in line with the acrylic block.
Resistance to testing
Each specimen was tested for its failure using Hounsfield Universal testing machine with a cross head speed of 1 mm/min [Figures 4–5]. The values obtained were recorded, tabulated, and subjected to stastical analysis. The same procedure was repeated at the end of 1 month (Phase II), 3 months (Phase III), and 6 months (Phase IV), on the remaining prepared specimens and the results tabulated. The recorded values were statistically analyzed using ANOVA and Newman-Keul's Studentized range test.
Figure 4.

Testing of specimen for failure load
Figure 5.
Fractured specimen
Results
The results show that there were no significant differences in the reinforcement provided by the Group I, Group II, Group III, and Group IV specimens at phase II and III when compared to phase I [Tables 1–3]. However, at phase IV, specimens of Group I, Group II, and Group III showed statistically significant differences when compared to phase I and Group IV, but did not show statistical significant difference from phase I [Figure 6 and Table 4].
Table 1.
Intercomparison of failure load between various reinforcing materials at Phase I
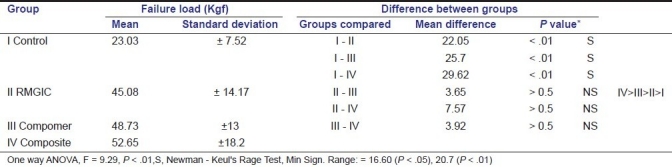
Table 3.
Intercomparison of Failure load between various reinforcing material at Phase - III
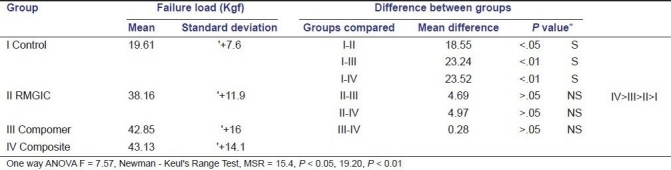
Figure 6.
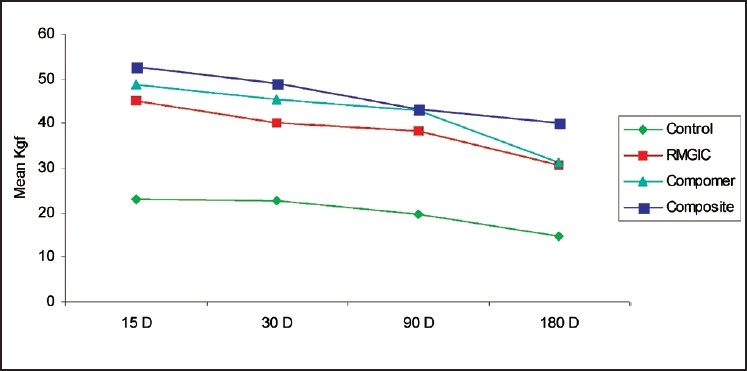
Load failures of various materials at determined time intervals
Table 4.
Inter-comparison of failure load between various reinforcing materials at Phase - IV
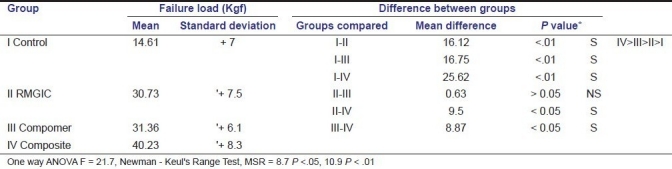
Table 2.
Intercomparison of failure load between various reinforcing materials at Phase II
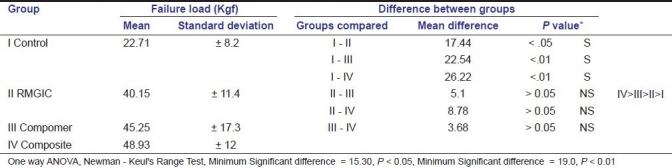
When intergroup comparisons in the mean failure load values between various groups at four different phases were made, the experimental groups had significant differences when compared to control group at each phase.
Among the experimental groups, Flowable Composite group had a statistically significant difference when compared to RMGIC and Flowable Compomer groups. No statistical differences were found between the Flowable Compomer and RMGIC.
Discussion
In this study, experimental models that simulate immature teeth with total crown loss after apexification were used. Permanent maxillary central incisors were chosen because these teeth are most commonly affected by dental impact injuries.[14] They were selected according to their MD and BL dimensions in order to reduce variables related to the different anatomical structures. In order to create a wide root canal with thin dentinal walls, the root canals were enlarged till 120 file size, 1 mm short of their apex.
In this study, it was decided to evaluate the failure load of the root specimens at the end of 15, 30, 90, and 180 days. The rationale behind this choice of carefully spaced periods was done keeping in mind the number of days of calcium hydroxide therapy when used as an interappointment intracanal medicament, as a remedy for weeping canals and as an agent for apexification.[4,24]
A review by Goodacre and Spolnik recommended post length equal to ¾ of root canal length, if possible or at least equal to the length of the crown and 8 mm was the minimum length required for a post.[25] In our study, a post length of 10 mm was left behind for reinforcement of the canals.
The inherent problem with the light cured dentin bonded composites is the inability of the light to penetrate to a depth greater than 5 mm or 6 mm. Since it has been impossible so far to transmit light down the length of the canal, this often presented a problem in the intraradicular space. The introduction of a light transmitting post enables the clinician to complete polymerization of a light-cured or dual-cured Composite resin along the length and circumference of a prepared post channel.[26] Thus, a Luminex light transmitting post was used to cure the materials.
The testing force was directed along the long axis of the specimens, resulting in primarily a splitting stress applied above the cervical limit of the root. Although previous studies[10,11] applied the load 45°–130° to the long axis of the tooth, we decided to use a wedge effect on the root because of the absence of the crown and also since this is also the force the post induces once installed.[14]
A consistent finding in our study was that all the experimental groups at the end of each phase, significantly reinforced the calcium hydroxide-treated simulated immature incisor teeth compared to the control group. This finding confirmed the results of previous studies by Ketabzadeh N, Dalton C and Trope M,[5] Goldberg F, Kaplan A. Roitman M, Manfre S, Picca M,[14] and Pene JR, Nicholls JI and Harrington GW[20] who showed that restorative materials which bond chemically or micromechanically to teeth increased the resistance to fracture of roots with canals having increased diameters such as immature teeth.
In a study conducted by Andreason JO, Farik B, Munksgaard EC, they found that in teeth treated with calcium hydroxide for a period of one year, fracture resistance reduced by 45%–50%.[8] In our study, the failure load of the control group was significantly reduced by almost 40% at the end of 6 months when compared to the control specimens at 15 days. This shows that the long term therapies like apexification, which involved exposure of teeth to calcium hydroxide for time periods of six months or even greater resulted in significant weakening of the remaining tooth structure.
At the end of 180 days, it was evident that the reinforcement provided by Flowable Composites was significantly greater than those provided by the Flowable Compomers and RMGIC.
The results of our study were comparable to the results of Meyer JN, Cattni-Lorente MA and Dupuis V,[27] and that of I H El, kalla F and Garcia-Godoy,[28] who evaluated the mechanical properties of RMGIC, Compomer, and Composite and concluded that among the evaluated materials, the weakest was RMGIC followed by Compomer with the strongest being Composite.
The Flowable Composite group at the end of 180 days showed no significant reduction in the reinforcement values compared to that at the end of 15 days indicating that they were more effective in reinforcing the root specimens, despite the drastic drop in the failure load of control specimens at the end of 6 months. Previous studies[18,29] have postulated that one of the apparent short comings of composites used for reinforcement of root canals is the propogation of microcracks resulting from inherent porosities and flexure in the material, leading to subsequent failure of the restoration. The use of a Flowable Composite probably abridged and overcame the above problem.
This study was an unpretentious attempt to evaluate the time bound effects of exposing simulated immature root specimens to calcium hydroxide for varying periods of time and evaluating the reinforcing capabilities of three commonly used adhesive restorative materials. Since the benefits of calcium hydroxide in dentistry are well documented, this material will continue to receive the patronage of dental practitioners for a variety of applications despite its inherent shortcomings. Our study has described a restorative method to strengthen internally, immature traumatized incisors using Luminex post system. Hence, it would be prudent that the practitioners use Flowable composites in conjunction with a light transmitting post when reinforcing calcium hydroxide-treated immature teeth.
Conclusions
All the materials evaluated substantially increased resistance of the root specimens to fracture when compared with the non-reinforced specimens.
Flowable composites provided maximum reinforcement effect at the end of 180 days, followed by Flowable Compomer, and RMGIC, which exhibited reduced reinforcement effects.
Within the limitations of this study and among the materials tested, Flowable Composites were found to be the best reinforcing material to strengthen the roots of teeth with weakened dentinal walls.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Andreason JO, Andreason FM. Text book and Color Atlas of Traumatic Injuries to the Teeth. Andreason. (3rd edition) 1994:172–382. [Google Scholar]
- 2.Ghose LJ, Baghdady VS, Hikmat YM. Apexification of immature apices of pulpless permanent anterior teeth with calcium hydroxide. J Endod. 1987;13:285–90. doi: 10.1016/s0099-2399(87)80045-6. [DOI] [PubMed] [Google Scholar]
- 3.Yates JA. Barrier formation time in non-vital teeth with immature apices. Int Endod J. 1988;21:313–9. doi: 10.1111/j.1365-2591.1988.tb01141.x. [DOI] [PubMed] [Google Scholar]
- 4.Mackie IC, Bentley EM, Worthington HV. The closure of open apices in non-vital immature incisor teeth. Br Dent J. 1988;165:169–73. doi: 10.1038/sj.bdj.4806553. [DOI] [PubMed] [Google Scholar]
- 5.Ketabzadeh N, Dalton C, Trope M. Strengthening immature teeth during and after apexification. J Endod. 1998;24:256–9. doi: 10.1016/s0099-2399(98)80108-8. [DOI] [PubMed] [Google Scholar]
- 6.Hasselgren G, Kerkes K, Nellestam P. pH changes in calcium hydroxide covered dentin. J Endod. 1982;8:502–5. doi: 10.1016/s0099-2399(82)80076-9. [DOI] [PubMed] [Google Scholar]
- 7.Nerwich A, Figdor D, Messer HH. pH Changes in root dentin over a 4-week period following root canal dressing with calcium hydroxide. J Endod. 1993;19:302–5. doi: 10.1016/s0099-2399(06)80461-9. [DOI] [PubMed] [Google Scholar]
- 8.Andreason JO, Farik B, Munksgaard EC. Long-term Calcium hydroxide as a root canal dressing may increase risk of root fracture. Dent Traumatol. 2002;18:134–7. doi: 10.1034/j.1600-9657.2002.00097.x. [DOI] [PubMed] [Google Scholar]
- 9.Andreason JO, Munksgaard EC, Bakland LK. Comparison of fracture resistance in root canals of immature sheep teeth after filling with calcium hydroxide or MTA. Dent Traumatol. 2006;22:154–6. doi: 10.1111/j.1600-9657.2006.00419.x. [DOI] [PubMed] [Google Scholar]
- 10.Carvalho CA, Valera MC, Oliveira L, Camargo CH. Structural resistance in immature teeth using root reinforcements in vitro. Dent Traumatol. 2005;21:155–9. doi: 10.1111/j.1600-9657.2005.00312.x. [DOI] [PubMed] [Google Scholar]
- 11.Stuart CH, Schwartz SA, Beeson TJ. Reinforcement of Immature Roots with a New Resin Filling Material. J Endod. 2006;32:350–3. doi: 10.1016/j.joen.2005.08.001. [DOI] [PubMed] [Google Scholar]
- 12.Cvek M. Prognosis of Non-vital maxillary, incisors treated with calcium hydroxide and filled with gutta-percha.A retrosposective clinical study. Endod Dent Traumatol. 1992;8:45–55. doi: 10.1111/j.1600-9657.1992.tb00228.x. [DOI] [PubMed] [Google Scholar]
- 13.Hernandes R, Bader S, Boston D, Trope M. Resistance to fracture of endodontically treated premolars, restored with new generation dentin bonding systems. Int Endod J. 1994;27:281–4. doi: 10.1111/j.1365-2591.1994.tb00269.x. [DOI] [PubMed] [Google Scholar]
- 14.Goldberg F, Kaplan A, Roitman M, Manfre S, Picca M. Reinforcing effect of a resin glass ionomer in the restoration of immature roots in vitro. Dent Traumatol. 2002;18:70–2. doi: 10.1034/j.1600-9657.2002.00083.x. [DOI] [PubMed] [Google Scholar]
- 15.Teixeira FB, Teixeira EC, Thompson JY, Trope M. Fracture resistance of roots endodontically treated with a new resin filling material. J Am Dent Assoc. 2004;135:646–52. doi: 10.14219/jada.archive.2004.0255. [DOI] [PubMed] [Google Scholar]
- 16.Lui JL. A technique to reinforce weakened roots with post canals. Endod Dent Traumatol. 1987;3:310–4. doi: 10.1111/j.1600-9657.1987.tb00641.x. [DOI] [PubMed] [Google Scholar]
- 17.Lui JL. Depth of composite polymerization with simulated root canals using light transmitting posts. Oper Dent. 1994;19:165–8. [PubMed] [Google Scholar]
- 18.Jhonson ME, Stewart GP, Neilsen CJ, Hatton JF. Evaluation of root reinforcement of endodontically treated teeth. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2000;90:360–4. doi: 10.1067/moe.2000.108951. [DOI] [PubMed] [Google Scholar]
- 19.Trope M, Malyz DO, Tronstad L. Resistance to Fracture of Endodontically Treated Teeth. Endod Dent Traumatol. 1985;1:108–11. doi: 10.1111/j.1600-9657.1985.tb00571.x. [DOI] [PubMed] [Google Scholar]
- 20.Pene JR, Nicholls JI, Harrington GW. Evaluation of Fiber-Composite Laminate in the Restoration of Immature, nonvital Maxillary Central Incisors. J Endod. 2001;27:18–22. doi: 10.1097/00004770-200101000-00006. [DOI] [PubMed] [Google Scholar]
- 21.Windley W, 3rd, Ritter A, Trope M. The effect of short-term calcium hydroxide treatment on dentin bond strengths to composite resin. Dent Traumatol. 2003;19:79–84. doi: 10.1034/j.1600-9657.2003.00160.x. [DOI] [PubMed] [Google Scholar]
- 22.Schumacher JW, Rutledge RE. An Alternative to Apexification. J Endod. 1993;19:529–31. doi: 10.1016/S0099-2399(06)81497-4. [DOI] [PubMed] [Google Scholar]
- 23.Webber RT, Schiwiebert KA, Cathey GM. A technique for placement of calcium hydroxide on the root canal system. J Am Dent Assoc. 1981;13:417–20. doi: 10.14219/jada.archive.1981.0346. [DOI] [PubMed] [Google Scholar]
- 24.Sheehy EC, Roberts GJ. Use of Calcium hydroxide for apical barrier formation and healing in non-vital immature permanent teeth: A review. Br Dent J. 1997;183:241–6. doi: 10.1038/sj.bdj.4809477. [DOI] [PubMed] [Google Scholar]
- 25.Schwartz RS, Robbins JW. Post Placement and Restoration Of Endodontically Treated Teeth: A Literature Review. J Endod. 2004;30:289–301. doi: 10.1097/00004770-200405000-00001. [DOI] [PubMed] [Google Scholar]
- 26.Freedman G, Novak IS, Serota KS, Glassman GD. Intra-Radicular Rehabilitation: A Clinical Approach. Pract Perio Aesthet dent. 1994;6:33–9. [PubMed] [Google Scholar]
- 27.Meyer JN, Cattni-Lorente MA, Dupuis V. Compomers: Between glass ionomer cements and composite. Biomaterials. 1998;19:529–39. doi: 10.1016/s0142-9612(97)00133-6. [DOI] [PubMed] [Google Scholar]
- 28.el-Kalla IH, García-Godoy F. Mechanical Properties of Compomer Restorative Materials. Oper Dent. 1999;24:2–8. [PubMed] [Google Scholar]
- 29.Yap AU, Chung SM, Chow WS, Tsai KT, Lim CT. Fracture Resistance of Compomer and Composite Restoratives. Oper Dent. 2004;29:29–34. [PubMed] [Google Scholar]


