Abstract
Osteoma is a benign osteogenic lesion with a very slow growth, characterized by proliferation of either cancellous or compact bone. Depending on its location, osteoma may be classified as central, peripheral or extraskeletal type. Although peripheral osteomas of the upper jaw are rare, diagnosticians can however encounter them in their clinical practice, which are probably misdiagnosed. These should be considered in the differential diagnosis of any slow-growing, non-tender, bony hard, non-compressible, non-fluctuant and non-pulsatile swelling present on the Oral and Maxillofacial region. We report a rare case of maxillary peripheral osteoma in a 50-year-old female patient. To best of our knowledge this is the eleventh case of maxillary osteoma reported in the English language literature.
Keywords: Maxilla, maxillofacial region, osteoma, peripheral
Introduction
Osteoma is a benign osteogenic tumor arising from the proliferation of the cancellous or compact “ivory osteoma” bone.[1,2] It can be central osteoma arising from the endosteum, peripheral osteoma (PO) arising from the periosteum or extra-skeletal soft tissue osteoma that usually develops within the muscle.[3,4] PO of the maxillofacial areas is uncommon. These occur frequently in the sinuses, most common in the frontal sinus, followed by the ethmoidal and maxillary sinus.[5,6]
Most cases of PO appear to have a very slow growth rate, are asymptomatic and produce swelling and asymmetry. Its pathogenesis is unclear; some believe it to be a true neoplasm while others classify it as a developmental anomaly.[7] Trauma or infection as a source of triggering factors has also been suggested.[8] Association between maxillofacial osteomas, cutaneous sebaceous cysts, multiple supernumerary teeth and colorectal polyposis has also been reported (Gardner's syndrome).[5]
Case Report
A 50-year-old female patient reported with a chief complaint of swelling in the anterior region of the upper jaw, present since 10 years. History revealed that the swelling initially started as a peanut size and had gradually increased to the present size. The patient gave a past history of trauma to the upper jaw 15 years back during a road accident. She had visited a local dentist for pain and swelling in the same region. Extraoral and intraoral radiographs were taken, which were insignificant. She was given some drugs (patient was unaware of this) and, within 1 week, she was asymptomatic. After 4 years, she observed an asymptomatic peanut-sized swelling in the same region of the jaw, which has been slowly increasing in size.
Extraoral examination revealed a diffuse swelling measuring about 1 cm × 1 cm in the midline below the nose, with slight obliteration of the left nasolabial fold [Figure 1]. Skin overlying the swelling was normal. On palpation, the swelling was non-tender and bony hard. Borders of the swelling were distinct and smooth. Lymph node examination was insignificant. No other marked deformity was noted.
Figure 1.

Facial view showing the extraoral diffuse swelling
Intraoral examination revealed a well-circumscribed swelling of about 2 cm × 2 cm on the alveolar process obliterating the labial vestibule in the 11-22 region. Mucosa overlying the swelling appeared blanched [Figure 2]. The oral hygiene of the patient was poor. She had multiple carious teeth, stains, calculus and generalized periodontitis. On palpation, the swelling was non-tender, bony hard (non-compressible), non-fluctuant and non-pulsatile. The pulp vitality test confirmed all the anterior teeth (13, 12, 11, 21, 22, 23) to be vital. The intra-oral periapical radiograph revealed a well-demarcated radio-opaque mass superimposing the roots of 21 and 22, clearly demarcated from the surrounding normal bone. Based on the clinical and radiological findings, a provisional differential diagnosis of peripheral ossifying fibroma, osteoma and maxillary torus was made.
Figure 2.

Intraoral photograph revealing the extension and appearance of the swelling
The lesion was excised under local anesthesia. The gross specimen was bony hard, round in shape and measured about 2 cm × 2 cm. The superficial surface appeared pale and smooth whereas the cut surface was rough [Figure 3]. The tissue was fixed in 10% neutral buffered formalin, decalcified in 5% formic acid and was routinely processed.
Figure 3.

Gross surgical specimen showing the superficial and cut surfaces
The decalcified section was stained with Hematoxylin and Eosin, which revealed surface epithelium overlying the stromal tissue, consisting of lamellar bone and adipose tissue in the lamina propria and submucosa. The epithelium was stratified squamous non-keratinized type. The lamina propria consisted of multiple trabeculae of mature lamellar bone with a variable amount of fibro-fatty marrow tissue [Figures 4 and 5]. Large and small trabeculae of lamellar bone were seen extending into the submucosa, suggestive of cancellous bone. Based on these histopathologic features, a diagnosis of peripheral cancellous osteoma was made.
Figure 4.
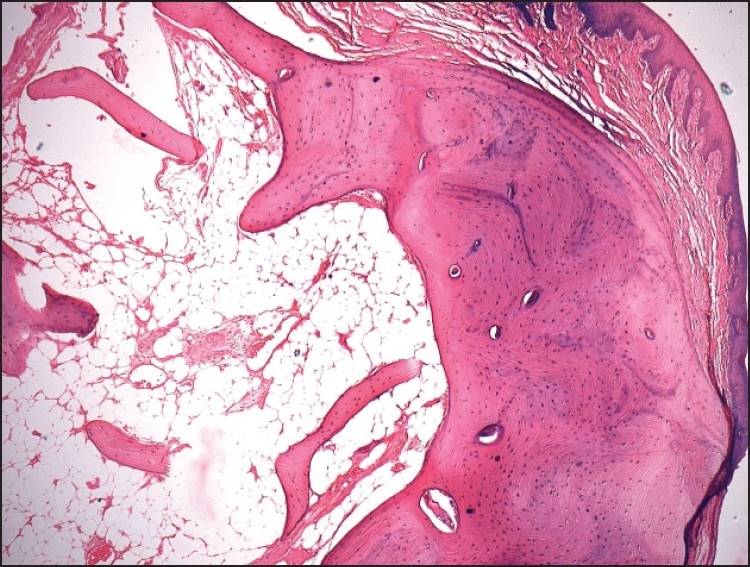
Photomicrograph showing stratified squamous epithelium overlying the stroma consisting of trabeculae of mature lamellar bone (hematoxylin and eosin, original magnification ×4)
Figure 5.
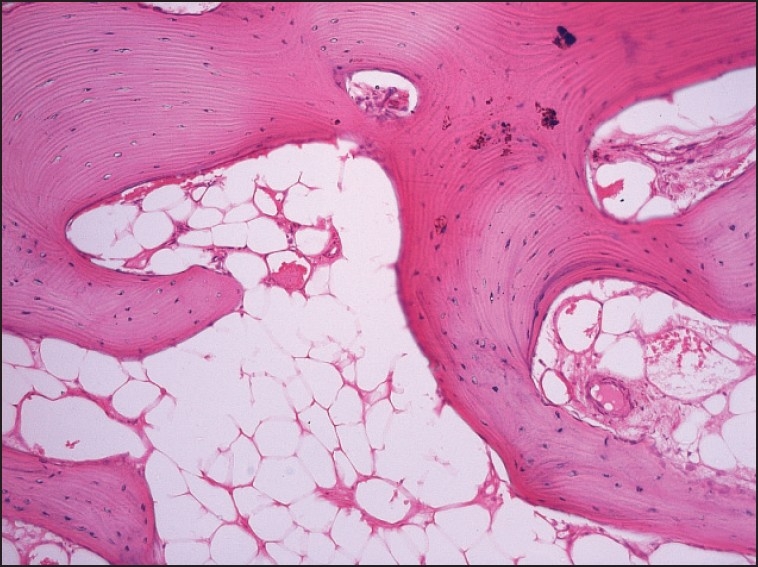
Photomicrograph showing trabeculae of mature lamellar bone with a variable amount of fibro-fatty marrow tissue (hematoxylin and eosin, original magnification ×40)
Discussion
Osteoma is a rare benign tumor characterized by excessive and persistent proliferation of the bone.[1] It may arise from proliferation of the medullary bone (endosteal) or on the bone surface as a polypoid or sessile growth (periosteal).[7,8] Depending on the location, it can be central osteoma, PO or extraskeletal osteoma.[3,4] It usually shows slow growth and is asymptomatic. In many cases, the diagnosis of the PO is an incidental finding. In some cases, the size of the tumor may cause facial deformity.[1] In the maxillofacial region, these tumors are mainly located on the skull.[9] PO occurs most frequently in the sinuses, of which the frontal sinus is the most common site, followed by ethmoidal and maxillary sinuses. PO has also been described in the external auditory canal and, rarely, in the temporal bone and pteygoid plate.[5,6]
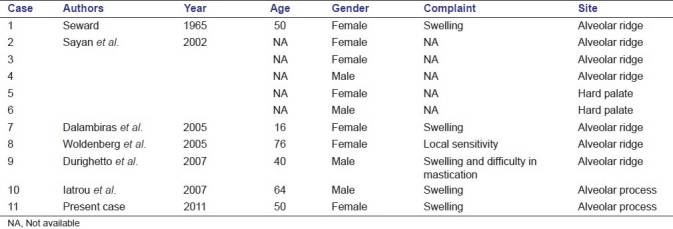
PO of the jaw bones is quite rare. These lesions usually appear as a unilateral pedunculated mushroom-like mass. The mandible is more commonly affected than the maxilla. The most common affected sites are angle and lower border of the body of the mandible, the sites most susceptible to trauma.[3,7,10] There is a 3:1 female predilection, but different authors have reported both female and male predilection in case series of osteomas of the maxillofacial region.[1,7] To best of our knowledge, and apart from osteomas located in the maxillary sinuses, there are only 10 cases of maxillary osteomas previously described in the English language literature [Table 1],[1,11–14] of which complete clinical data of five cases is not available. Their age ranged from 16 to 76 years, with a mean age of 45.5 years. The mean age range of the patients with osteoma in the maxillofacial region has been reported to be 29.4 and 40.5 years.[1,8] PO mostly presents as an asymptomatic, slow-growing swelling. However, local sensitivity and difficulty in mastication have also been reported.[1,15] The most common site of maxillary osteoma is the alveolar process. The exact etiology and pathogenesis of PO is still unclear. Various hypotheses have been put forward, which include congenital and hereditary disorder, a developmental origin, neoplastic or a reactive mechanism to trauma or infection. Location of PO of the jaws is usually in close proximity to the area of muscle attachment, suggesting that muscle traction may also play an important role in its development. The combination of trauma and muscle traction has also been suggested in the pathogenesis of PO.[1,7,8,10,16] Differential diagnosis includes exostosis, but these tend to stop growing after puberty; periosteal osteoblastoma, osteoid osteoma and paraosteal osteosarcoma usually present as a rapidly growing painful swelling.[7,15]
Table 1.
Summary of clinical data of maxillary osteomas previously published in the English language literature, including the present case
Surgical removal of PO is not generally necessary unless and until there are symptoms like facial asymmetry or other secondary problems.[17] Recurrence after surgical procedure is rare.[15] There are no reports of malignant transformation of PO in the literature.[1]
The present case of PO was seen in a 50-year-old female patient with swelling in the anterior region of the upper jaw that was present since 10 years following a history of trauma. The swelling was solitary, sessile, slow growing, non-tender, non-compressible, non-fluctuant and non-pulsatile. The lesion was surgically excised, histopathological examination revealed the presence of a surface-stratified squamous non-keratinized epithelium overlying the stromal tissue, consisting of lamellar bone and adipose tissue. The stromal tissue consisted of multiple trabeculae of mature lamellar bone with osteocytes. Medullary spaces consist of fibro-fatty marrow tissue with endothelial-lined blood vessels. A diagnosis of peripheral cancellous osteoma was made. The patient has been asymptomatic, with no evidence of recurrence since 2 years after surgery.
Conclusion
PO is a rare benign osteogenic lesion occurring in the Oral and Maxillofacial region. The possibility of PO should be kept in mind as a differential diagnosis for any peripheral, solitary, bony hard, slowly growing painless swelling encountered in the Oral and Maxillofacial region. To best of our knowledge this is the eleventh case of maxillary osteoma reported in the English language literature. Although the exact etiology and pathogenesis of this type of lesion is unclear, additional molecular and genetic research is required to improve the understanding.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Woldenberg Y, Nash M, Bodner L. Peripheral osteoma of the maxillofacial region: Diagnosis and management: A study of 14 cases. Med Oral Pathol Oral Cir Bucal. 2005;10:E139–42. [PubMed] [Google Scholar]
- 2.Cawson RA, Binnie WH, Barrett AW, Wright JM. 3rd ed. Mosby; 2001. Oral Disease; pp. 7.2–7.3. [Google Scholar]
- 3.Regezi JA, Sciubba J. 2nd ed. Philadelphia PA: Saunders; 1993. Oral Pathology; p. 407. [Google Scholar]
- 4.Junquera-Gutierrez L, Lopez-Arranz JS, Albertos-Castr JM, De Vicente-Rodriguez JC. Odontogenic tumors: Classification, clinical features, diagnosis and treatment. Med Oral. 1997;2:94–101. [PubMed] [Google Scholar]
- 5.Lew D, DeWitt A, Hicks RJ, Cavalcanti MG. Osteomas of the condyle associated with Gardner's syndrome causing limited mandibular movement. J Oral Maxillofac Surg. 1999;57:1004–9. doi: 10.1016/s0278-2391(99)90026-5. [DOI] [PubMed] [Google Scholar]
- 6.Batsakis JG. 2nd ed. Baltimore, MD: Williams and Wilkins; 1979. Tumors of the head and neck: Clinical and pathological consideration; pp. 405–6. [Google Scholar]
- 7.Sayan NB, Ucok C, Karasu HA, Gunhau O. Peripheral osteoma of the Oral and Maxillofacial region: A study of 35 new cases. J Oral Maxillofac Surg. 2002;60:1299–301. doi: 10.1053/joms.2002.35727. [DOI] [PubMed] [Google Scholar]
- 8.Kaplan I, Calderon S, Buchner A. Peripheral osteoma of the mandible: A study of 10 new case and analysis of the literature. J Oral Maxillofac Surg. 1994;52:467–70. doi: 10.1016/0278-2391(94)90342-5. [DOI] [PubMed] [Google Scholar]
- 9.Cutilli BJ, Quinn PD. Traumatically induced peripheral osteoma: Report of a case. Oral Surg Oral Med Oral Pathol. 1992;73:667–9. doi: 10.1016/0030-4220(92)90006-c. [DOI] [PubMed] [Google Scholar]
- 10.Lucas RB. Edinburgh, Scotland: Churchill Livingstone; 1984. Pathology of tumors of the Oral Tissues; pp. 191–4. [Google Scholar]
- 11.Seward MH. An osteoma of the maxilla. Br Dent J. 1965;5:27–30. [PubMed] [Google Scholar]
- 12.Dalambiras S, Boutsioukis C, Tilaveridis I. Peripheral osteoma of the maxilla: Report of an unusual case. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2005;100:E19–24. doi: 10.1016/j.tripleo.2005.03.011. [DOI] [PubMed] [Google Scholar]
- 13.Durighetto AF, de Moraes Ramos FM, da Rocha MA, da Cruz Perez DF. Peripheral osteoma of the maxilla: Report of a case. Dentomaxillofac Radiol. 2007;36:308–10. doi: 10.1259/dmfr/52795470. [DOI] [PubMed] [Google Scholar]
- 14.Iatrou IA, Leventis MD, Dais PE, Tosios KI. Peripheral osteoma of the maxillary alveolar process. J Craniofac Surg. 2007;18:1169–73. doi: 10.1097/SCS.0b013e31812f76d8. [DOI] [PubMed] [Google Scholar]
- 15.Johann AC, Freitas JB, Aguiar MC, de Araujo NS, Mesquita RA. Peripheral osteoma of the mandible: Case report and review of the literature. J Craniomaxillofac Surg. 2005;33:276–81. doi: 10.1016/j.jcms.2005.02.002. [DOI] [PubMed] [Google Scholar]
- 16.Bessho K, Murakami K, Iizuka T, Ono T. Osteoma in mandibular condyle. Int J Oral Maxillofac Surg. 1987;16:372–5. doi: 10.1016/s0901-5027(87)80162-5. [DOI] [PubMed] [Google Scholar]
- 17.Jones K, Korzcak P. The diagnostic significance and management of Gardner's syndrome. Br J Oral Maxillofac Surg. 1990;28:80–4. doi: 10.1016/0266-4356(90)90126-6. [DOI] [PubMed] [Google Scholar]


