Abstract
A radicular cyst is one of the most common odontogenic cysts of anterior maxilla, not commonly seen in adolescence. Here, we present a rare, atypical case, of bilateral radicular cysts of the mandibular posterior region in a 13-year-old girl. The patient management comprised surgical enucleation of cystic sac under general anesthesia followed by rehabilitation of the same area. The purpose of this article is to lay emphasis on the pedodontist's role in early diagnosis and treatment of such lesions.
Keywords: Bilateral mandibular radicular cysts, rehabilitation, surgical enucleation
Introduction
Radicular cysts are the most common inflammatory cysts arising from the epithelial residues in the periodontal ligament as a result of periapical periodontitis following necrosis of the pulp, remains asymptomatic and left unnoticed until detected during routine periapical radiography.
These cysts comprise about 52% to 68% of all the cysts affecting the human jaw.[1] Their incidence is highest in third and fourth decade of life with male predominance.[2] Anatomically the periapical cysts occur in all tooth-bearing sites of the jaw but are more frequent in the maxillary than the mandibular region.[1,3]
Radicular cysts can heal spontaneously after endodontic treatment or extraction. However, some authors propose that suspected radicular cysts must be totally enucleated surgically to remove all epithelial remnants.[4]
Case Report
A 13-year-old girl repoted to the Dept. of Pedodontics and Preventive Dentistry with a complaint of dull pain and swelling in the right posterior mandibular region since past 15 days. The patient had pain in the same region 1 year before and had taken medication for that. She had undergone extraction of the carious mandibular right first molar 3 days before.
Extraoral examination revealed a smooth superfacial swelling of about 3 × 2.5 cm extending from the corner of mouth to the angle of mandible and from the infraorbital margin to the lower border of mandible [Figure 1]. The swelling was tender and firmwith egg shell crackling on palpation. The inferior border of mandible was intact. The right submandibular lymph nodes were palpable and tender. Intraorally, the extraction socket of the mandibular right first molar [Figure 2] was present and remaining first molars were grossly carious. Vestibular obliteration and buccal and lingual plate expansion was observed in the area of right body of mandible [Figure 2].
Figure 1.

Pre-operative extra-oral photograph showing right mandibular swelling and facial asymmetry
Figure 2.

Pre-operative intraoral view showing vestibular obliteration and extraction socket related to the mandibular right first molar
A definite radiolucency was seen in intraoral periapical views of the mandibular right and left first molar regions. The orthopantamograph (OPG) showed a large, well-defined unilocular radiolucency with a sclerotic border periapically on the right side extending from the distal of the mandibular second premolar to mesial of the third molar leaving about 1 mm of sound bone at the inferior border of mandible. A root piece of the mandibular right first molar was seen inside the cystic cavity as radio-opaque foreign body. The mandibular canal was obliterated inferiorly [Figure 3]. A unilocular, well-defined radiolucency with a sclerotic border was accidentally found on the left side of mandible involving the roots of first and second molars [Figure 3].
Figure 3.

Preoperative orthopantamograph showing periapical unilocular radiolucencies in mandibular right and left first molar regions
Fine needle aspiration cytology (FNAC) revealed straw coloured fluid. Therefore, based on patient's clinical findings, radiographic investigations, and FNAC report, the provisional diagnosis of bilateral mandibular radicular cysts was made.
The patient was subjected to enucleation of the bilateral cysts under general anaesthesia. On the right side, a crevicular incision was made from the distal surface of the mandibular first premolar until distal surface of the second molar, the mucoperiosteal flap was raised, the mandibular second premolar and the second molar were extracted and the cyst was removed in toto along with the root piece of the first molar. There was an intact inferior alveolar neurovascular bundle [Figure 4]. On the left side, a crevicular incision was made from the distal of the mandibular second premolar to the distal of the second molar, the mucoperiosteal flap was raised, mandibular first and second molars were extracted, and the cyst was removed in toto [Figure 5]. Flaps were repositioned and sutures were taken. The tissue specimens were sent for histopathologial examination.
Figure 4.

Intraoperative view of enucleation of a cyst and intact neurovascular bundle on the right side
Figure 5.

Intraoperative view of enucleation of a cyst on the left side
The surgically excised lesion of right side was about 4.5×3 cm in size [Figure 6] and left side was about 2×1 cm in size [Figure 7]. Both specimens were creamish brown in colour and soft in consistency.
Figure 6.

Photograph showing the tissue specimen of the right side
Figure 7.

Photograph showing the tissue specimen of the left side
Histopathological examination of the surgical specimens showed nonkeratinized stratified squamous epithelial lining with chronic inflammatory cells infiltration, discontinuous arcading pattern of epithelial lining, hemosiderin pigmentation, and hyaline bodies [Figures 8 and 9]. In connective tissue, there were moderate amount of collagen bundles and blood vessels with infiltration of chronic inflammatory cells [Figures 8 and 9]. All these findings were confirmatory for the radicular cyst.
Figure 8.
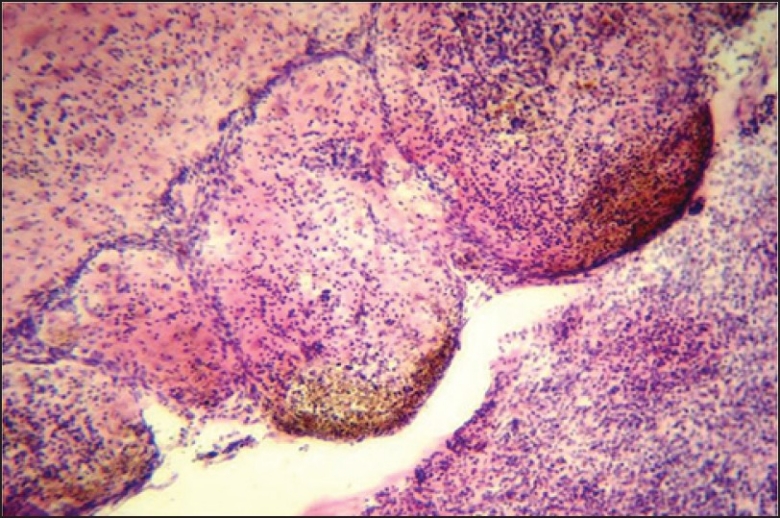
Microscopic image of the right side lesion (H and E stain ×40)
Figure 9.
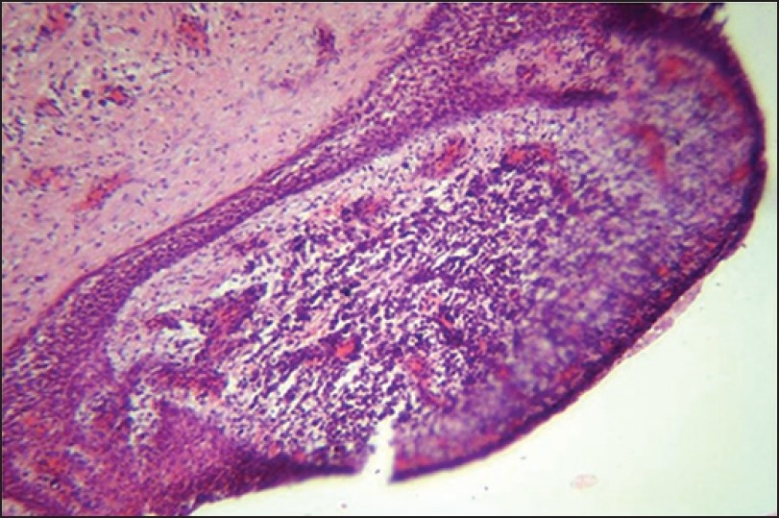
Microscopic image of the left side lesion (H and E stain ×40)
The patient was recalled after 7 days for removal of sutures; the extraoral swelling was resolved [Figure 10]. The healing on left side was uneventful. On the right side, after enucleation of the cyst the cavity was quite large so to enhance the healing, an acrylic stent was given to the patient and patient was recalled after every 15 days for check up of healing and necessary adjustments.
Figure 10.

Postoperative photograph showing the facial asymmetry corrected
Seven months after surgery, OPG exhibited good amount of bone formation [Figure 11]. Clinically, the healing was complete. So, the stent was replaced by removable partial prosthesis for oral rehabilitation [Figure 12]. Right now the patient is on a regular follow up.
Figure 11.

Postoperative orthopantamograph taken 7 months after surgery
Figure 12.

Intraoral view showing removable partial prosthesis
Discussion
A radicular cyst, also known as a peri-apical cyst, is usually associated with carious, nonvital, discolored, or fractured tooth.[5,6] The cyst is believed to form by proliferation of the epithelial cell rests of Malassez in inflammed periradicular tissues.[7] Its size rarely exceeds 1 cm and is often seen in patients between30 and 50 years old with higher incidence in the maxillary anterior region.[6,8] In this case, patient's age, sex, size of the cyst, and its bilateral presentation in the mandibular posterior region is considered rare.
The radicular cyst is usually symptomless and detected incidentally on plain OPG while investigating for other diseases. However, as some of them grow, they can cause mobility and displacement of teeth and once infected, lead to pain and swelling, after which the patient usually becomes aware of the problem.[2,6,9,10] The swelling is slowly enlarging and initially bony hard to palpate which later becomes rubbery and fluctuant.[2,6]
Several treatment options are available for a radicular cyst such as surgical endodontic treatment, extraction of the offending tooth, enucleation with primary closure, and marsupialization followed by enucleation.[6] In this case, surgical enucleation was preferred and was performed uneventfully.
To conclude, a radicular cyst is a common condition found in the oral cavity. However, it usually goes unnoticed and rarely exceeds the palpable dimension. This case illustrates a common condition that occurs in an uncommon age group and location.
Acknowledgments
Dr. Kiran Desai, Head of the Department of Oral and Maxillofacial Surgery, K. M. Shah Dental College and Hospital, Piparia.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Nair PN. Review New perspectives on radicular cysts: Do they heal? Int Endod J. 1998;31:155–60. doi: 10.1046/j.1365-2591.1998.00146.x. [DOI] [PubMed] [Google Scholar]
- 2.3rd ed. Singapore: Varghese Publication House; 1992. Mervyn Shear, Cysts of oral regions; pp. 136–70. [Google Scholar]
- 3.Rees JS. Conservative management of a large maxillary cyst. Int Endod J. 1997;30:64–7. doi: 10.1111/j.1365-2591.1997.tb01100.x. [DOI] [PubMed] [Google Scholar]
- 4.Walton RE. The residual radicular cyst: Does it exist? Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1996;82:471. doi: 10.1016/s1079-2104(96)80185-5. [DOI] [PubMed] [Google Scholar]
- 5.Scholl RJ, Kellett HM, Neumann DP, Lurie AG. Cysts and Cystic Lesions of the Mandible: Clinical and Radiologic-Histopathologic Review. Radiographics. 1999;19:1107–24. doi: 10.1148/radiographics.19.5.g99se021107. [DOI] [PubMed] [Google Scholar]
- 6.Shafer HL. 6th ed. Amsterdam: Elsevier; 2006. Textbook of Oral Pathology. [Google Scholar]
- 7.Lin LM, Huang GT, Rosenberg PA. Proliferation of epithelial cell rests, formation of apical cysts, and regression of apical cysts after periapical wound healing. J Endod. 2007;33:908–16. doi: 10.1016/j.joen.2007.02.006. [DOI] [PubMed] [Google Scholar]
- 8.Weber AL. Imaging of cysts and odontogenic tumors of the jaw. Radiol Clin North Am. 1993;31:101–20. [PubMed] [Google Scholar]
- 9.Gallego Romero D, Torres Lagares D, GarcIa Calderón M, Romero Ruiz MM, Infante Cossio P, Gutiérrez Pérez JL. Differential diagnosis and therapeutic approach to periapical cysts in daily dental practice. Medicina Oral. 2002;7:54–62. [PubMed] [Google Scholar]
- 10.Irfan M, Alauudin M, Roselinda A, Saifulizan A. Big Radicular Cyst In A 12 Year-Old Girl: A Case Report. Int Med J. 2007;6:C5. [Google Scholar]


