Abstract
Objective. To understand technicians’ attitudes toward teaching student pharmacists and students’ attitudes toward learning from technicians.
Methods. Survey data concerning technicians’ perceived importance of pharmacy skills and their confidence in teaching those skills to student pharmacists were collected, as was survey data concerning students’ comfort level with learning skills from technicians. Skills included in each survey aligned with common student pharmacist competencies and the pharmacy technician certification examination.
Results. Fifty-eight (92.1%) responses were received from technicians and 141(97.9%) student survey instruments were returned. The skills that pharmacy technicians perceived to be most important and felt most comfortable teaching included filling a prescription and communicating effectively with patients. With the exception of communication, these skills also aligned with what the students were most comfortable learning from technicians.
Conclusions. Student pharmacists have learning goals that align with the daily tasks of pharmacy technicians. The survey results highlight areas in which technicians could be used to educate student pharmacists.
Keywords: introductory pharmacy practice experiences, pharmacy technicians, survey
INTRODUCTION
In 2007, the Accreditation Council for Pharmacy Education (ACPE) instituted new standards to guide pharmacy curricula, which included a minimum of 300 hours of introductory pharmacy practice experiences (IPPEs) to occur in the first 3 years.1 This new requirement significantly increased the number of student pharmacists doing early practice experiences in hospital and community pharmacies. The goal of IPPEs is to provide student pharmacists opportunities to explore different career paths, apply knowledge learned in the didactic setting to real-world situations, and increase their ability and confidence before entering advanced pharmacy practice experiences in their fourth year.
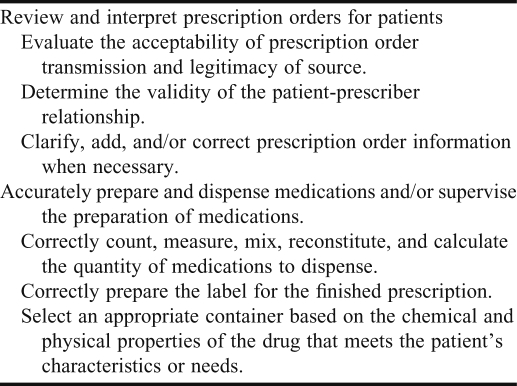
Several of the competencies from the Center for Advancement of Pharmacy Education for student pharmacist on IPPEs align with distributive functions (Table 1).2 As pharmacists move toward providing pharmaceutical care and spending more of their time identifying and resolving drug-therapy problems and counseling patients, pharmacy technicians are positioned to teach distributive competencies. Efforts are under way by the Pharmacy Technician Certification Board (PTCB), American Society of Health-System Pharmacists (ASHP), and many state boards of pharmacy to ensure consistent training among technicians. ASHP has developed a Model Curriculum for the training of pharmacy technicians, but it does not mention their role as educators and is not yet mandatory.3 Based on this model, we can justify that several of the competencies of early student experiences fall within the professional responsibilities of a technician; however, little of the professional literature assesses technicians’ motivation and confidence regarding teaching these skills or student pharmacists’ receptiveness to it.
Table 1.
Distributive Competencies From the Center for Advancement of Pharmacy Education2
METHODS
The 55-item technician survey instrument was developed to gather data about demographics, working environments, technician-perceived importance of specific skills and tasks, and confidence in ability to teach those tasks to IPPE students. The 35-item student pharmacist survey instrument was designed to collect information pertaining to experience working as a technician, experience with technicians while on IPPEs, comfort level learning specific tasks from pharmacy technicians, and top items students would like to learn from a pharmacist while on IPPEs. To solicit the tasks that students had learned from technicians and what they would like to learn from pharmacists, the survey allowed them to manually enter up to 3 additional items.
For both survey instruments, items soliciting attitudinal information were collected using a 5-point Likert scale, ranging from strongly disagree to strongly agree.4 A 5-point scale was selected based on a consensus that having 5 response options allows respondents a sufficiently wide range of intensities from which to choose.5
Demographic variables were collected using dichotomous responses, multiple-response items, and fill-in-the-blank statements. Data included gender, age, experience as a technician, whether they were certified by PTCB, and for the technician survey, whether their worksites host pharmacy students.
On both survey instruments, the sections pertaining to specific skills and tasks mirrored the types of basic knowledge functions that are represented on the Pharmacy Technicians Certification Examination (PTCE).6 Variables were drawn from all 3 areas of this examination: assisting the pharmacist in serving patients, maintaining medication and inventory control systems, and participating in the administration and management of pharmacy practice.
After the first draft of the student survey instrument was created, a focus group of 5 students was convened to ensure the survey was clear, comprehensive, and acceptable. After the focus group had reviewed the survey instrument, several revisions were made before the final version was distributed. This study received institutional review board exemption prior to data collection.
Study participants were considered a convenience sample. Technicians attending the 2009 annual meeting of the American Association of Pharmacy Technicians were invited to participate. Paper survey instruments were distributed to the 43 attendees prior to a presentation on their role in experiential education. An additional 20 survey instruments were distributed to technicians in the community pharmacy environment to ensure this group was adequately represented. The student survey instrument was distributed during the fall 2010 orientation to 144 students starting their second or third year of the doctor of pharmacy (PharmD) degree program. At this point in the curriculum, the second-year students had completed 1 semester of IPPEs focusing on distributive functions in either the hospital or retail setting. The third-year students had completed 3 semesters: 2 in the community setting and 1 in the hospital setting. A response rate of at least 50% was desired.5
All analyses were done using SPSS,Version 15.0 for Windows. As a quality-control measure, a codebook was used for data entry and organization.5 After the data were collected, a randomly selected sample (10%) of the papers was checked for errors. Responses to open-ended questions were scanned to identify frequently recurring answers. In the codebook, major groups of responses were assigned a number. For responses that did not fall into 1 of the listed categories, a category of “other” was used. Frequencies were calculated for descriptive items. Variables that were measured as continuous data were converted to ordinal data because statistical procedures are not commonly used to compare an ordinal dependent variable with a continuous independent variable.7 Spearman's rho (ρ) was calculated to assess correlation between variables. To determine how much variance, r values were used to calculate the coefficient of determination for the 2 variables. The Mann-Whitney U test was used to compare mean rankings between groups. In these cases, z values were used to calculate an approximate value of r. R values were interpreted as follows: small correlation (0.10 – 0.29), medium correlation (0.3 – 0.49), and large correlation (0.5 – 1.0).8 These guidelines are also appropriate to interpret r values for mean differences.8 Significance was set a priori at <0.05.
For missing data, the SPSS option “excluded cases pairwise” was used so that survey instruments with missing data were excluded only if they were missing the data required for the specific analysis. To test the survey's internal consistency, the Cronbach α was calculated for each section of the survey instrument. A minimum level of 0.7 was considered an appropriate level of reliability.
RESULTS
On the technician survey instrument, the sections on working conditions, perceived importance of skill, and confidence to teach a specific skill achieved a Cronbach α of 0.899, 0.857, and 0.925, respectively. The Cronbach α for the section of the student survey pertaining to comfort learning specific tasks was 0.886. These results indicate that the items on both survey instruments measured the same underlying attribute and were internally consistent and reliable.
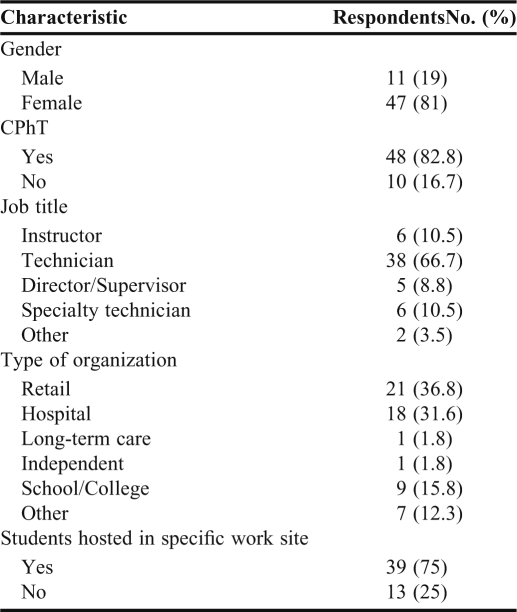
Fifty-eight (92.1%) of the 63 technician survey instruments distributed were returned. Demographic and work characteristics are provided in Tables 2 and 3, and frequencies calculated for responses in the 3 sections of the technician survey are presented in Tables 4, 5, and 6. There was a moderate positive correlation between perception of adequate training and overall comfort with teaching others in the workplace (ρ = 0.477, n = 56, P = 0.001). Perception of adequate training helps explain 23% of the variance in respondents’ rating of their level of comfort with teaching. There was either a moderate or large positive correlation between perceived level of importance of a specific task and the confidence to teach that task, except for filling a prescription (ρ = 0 .277, n = 53, P = 0.102).
Table 2.
Demographics of Pharmacy Technicians Who Responded to a Survey Regarding Their Role as Instructors for Student Pharmacists (n = 58)
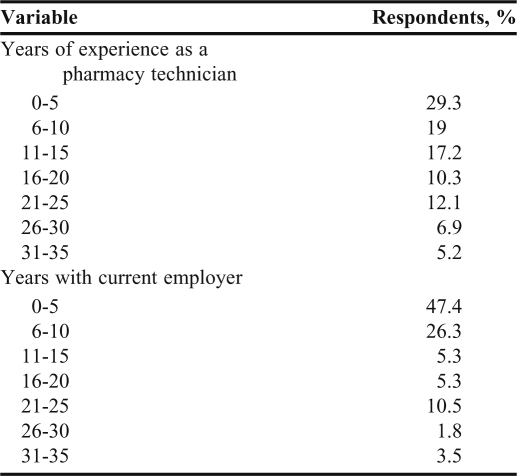
Table 3.
Work History of Pharmacy Technicians Who Responded to a Survey Regarding Their Role as Instructors for Student Pharmacists
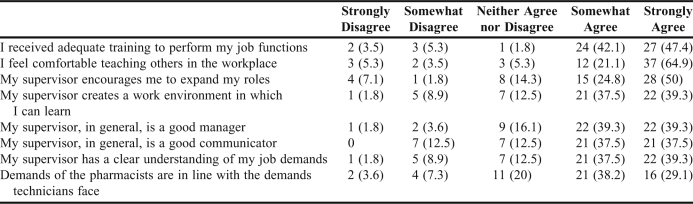
Table 4.
Pharmacy Technicians’ Perceptions of Working Conditions, No. (%)
Table 5.
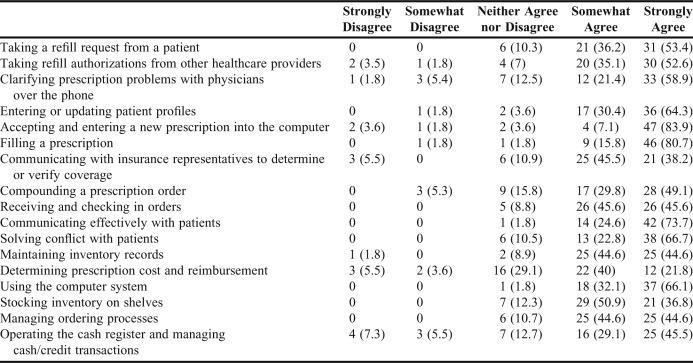
Pharmacy Technicians’ Perceptions About the Importance of Specific Skills, No. (%)
Table 6.
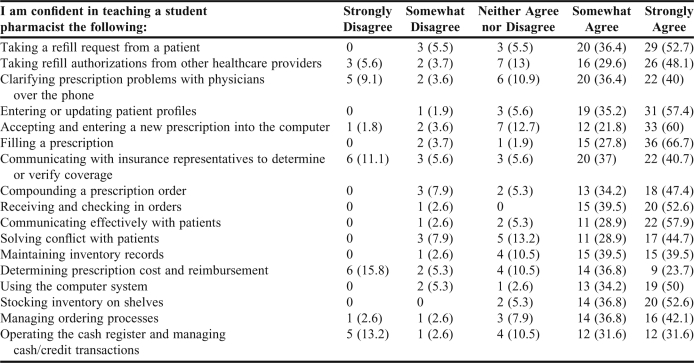
Technicians’ Confidence in Teaching Student Pharmacists Specific Skills, No. (%)
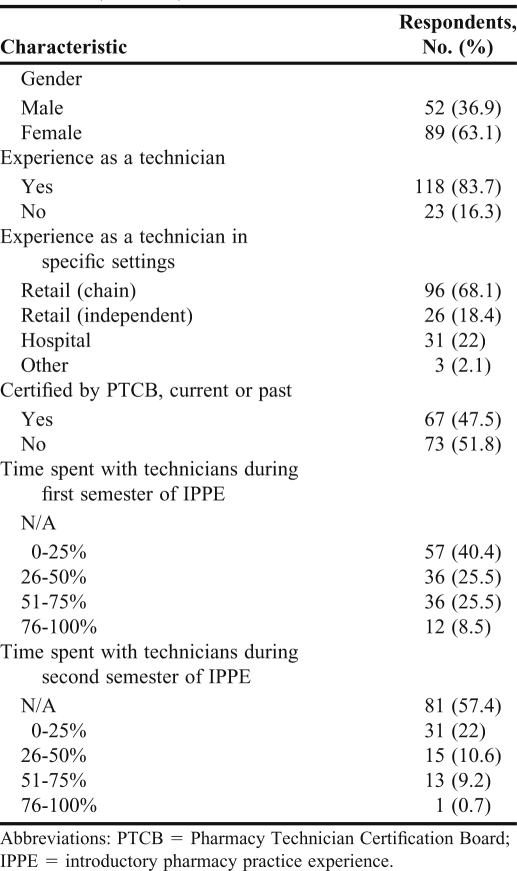
One hundred forty-one (97.9%) of the 144 student survey instruments were returned (Table 7). The average student age was 26 years. For students with experience as a technician, 42 (56%) indicated that they played a role in educating student pharmacists during that time. One hundred thirty-three (94.3%) students believed that pharmacists need to have the knowledge and skills to perform distributive functions in the retail setting even if the profession moves toward an emphasis on providing pharmaceutical care.
Table 7.
Characteristics of Student Pharmacists Who Responded to a Survey Regarding Pharmacy Technicians as Instructors (N = 141)
Table 8 lists the top 5 tasks that students reported being most comfortable and least comfortable learning from pharmacy technicians. Students who had completed 3 semesters of IPPEs were more comfortable learning the following from technicians: how to fill a prescription (U = 1944, z = -0.606, P = 0.026, r = -0.05), determining prescription cost (U = 1974, z = -2.068, P = 0.039, r = -0.17), and taking a refill request from a patient (U = 2009, z = -2.395, P = 0.017, r =-0.20). There was no significant difference between the 2 classes’ comfort levels for other tasks.
Table 8.
Top 5 Tasks Student Pharmacists Were Most and Least Comfortable Learning from Technicians
There were no significant differences in comfort level associated with learning from a technician between students with experience as a technician and those with no experience, with the exception of operating a cash register (U = 1089, z = -2.068, P = 0.039, r = -0.17). Students who obtained certification from the PTCB were more comfortable learning how to take a refill request from a patient (U = 2000.5, z = -2.282, P = 0.023, r = -0.19) and how to solve conflicts with patients (U = 1636, z = -3.336, P = 0.001, r = -0.28) from technicians than were those who had technician experience but did not have PTCB certification.
Students who had spent a significant amount of time with technicians during the first semester of IPPE were more comfortable learning how to determine insurance eligibility (ρ = 0.211, n = 141, P = 0.012), inventory ordering needs (ρ = 0.226, n = 141, P = 0.007), and solving conflict with patients (ρ = 0.219, n = 140, P = 0.009) from technicians than were students who had spent little time with technicians.
Students who had spent a significant amount of time with technicians during the second semester of IPPE were more comfortable learning the following tasks from a technician: how to take a refill request from a patient, how to fill a prescription, how to determine prescription cost, how to determine ordering needs, how to check in an order once it was received, how to use the computer system, how to stock the shelves, and how to maintain inventory records.
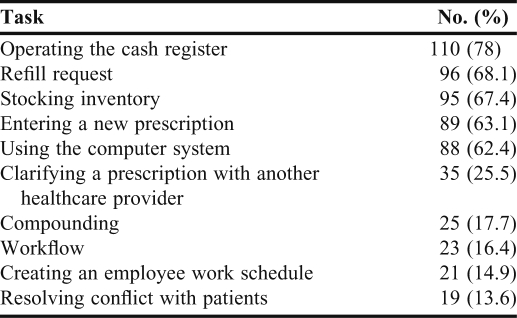
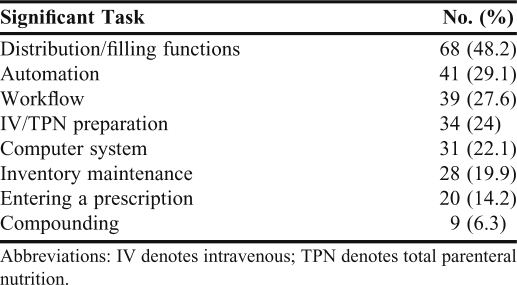
Students were asked to list the most significant tasks they learned from technicians while on IPPEs. The top answers are provided in Table 9. Examples of comments that fell into the “other” category were operating the cash register, printing labels, and decreasing dispensing errors.
Table 9.
Most Significant Tasks Student Pharmacists Felt They Learned From Technicians While on Practice Experiences
Students with technician experience who had the responsibility of educating student pharmacists were no more comfortable learning from technicians than were those without that experience. Students who indicated that they did not feel comfortable learning from a technician cited the following reasons: they were training to become pharmacists and, therefore, felt they should learn from pharmacists (n = 59, 41.8%), they had reservations about technicians’ abilities (n = 52, 36.9%), and they felt the technicians would have a hard time adding teaching to their normal routine (n = 17, 12.8%).
In response to being asked which tasks they wanted to learn from a pharmacist while on IPPEs, a majority of students cited performing a drug-use review (n = 129, 91.5%), followed by verifying the correctness of a filled prescription (n = 112, 79.4%). Sixteen students entered additional tasks they wanted to learn, of which the most commonly cited were communication skills (n = 5, 31.3%) and how to conduct medication therapy management sessions (n = 2, 12.5%).
DISCUSSION
According to the technicians surveyed, the skills perceived to be the most important were filling prescriptions, entering a new prescription into the computer, and communicating effectively with patients. These skills coincide with those the technicians felt most comfortable teaching. A majority felt comfortable learning these tasks from technicians, with the exception of communication skills, which 25% reported they would not be comfortable learning from technicians. One reason for this difference may be the various types of information generally communicated by each. Technicians tend to focus on questions relating to prescription preparation and insurance, while pharmacists focus on medications and disease states.
The tasks technicians felt least comfortable teaching student pharmacists included communicating with insurance companies, determining cost and reimbursement, and clarifying a prescription with a physician. Possibly, this is because expertise in these tasks comes with time as one learns the nuances of the healthcare system. The nature of these tasks also makes it more difficult to provide a clear-cut description of how each situation could be handled. Conversely, students felt comfortable learning these tasks from technicians, perhaps because students do not view them as requiring clinical judgment.
There was no correlation found between technicians’ years of experience and their overall comfort with teaching others. This may be attributable to 52% of the respondents having more than 10 years of experience, suggesting that respondents with less experience were underrepresented in this survey.
When comparing the technicians’ perceived importance of a skill to the confidence to teach that skill, there was no correlation for filling a prescription. This finding may result from the fact that filling a prescription is possibly the most frequent activity performed by community pharmacy technicians, and therefore did not stand out to them as exceptionally important.
For technicians, the time in current position did not help to explain confidence in teaching. Although 64.3% of the respondents had been in their position for 5 years or less, they may have had experience from previous jobs.
The main tasks the students wanted to learn in IPPEs (performing a drug-utilization review and verifying the correctness of a prescription) require a higher level of drug knowledge than may be possessed by students beginning their second or third year of pharmacy school. However, shadowing a pharmacist performing these duties can be a significant component of IPPEs.
While these surveys serve as a good starting point for assessing technicians’ motivation and perceived abilities to teach student pharmacists as well as students receptiveness to being taught by technicians, there are some limitations to this study. The technician sample size was relatively small. This may be the reason that several of the analyses were not significant. Because the sample populations were obtained through nonprobability sampling, the results cannot be generalized beyond the sample. Another confounding factor may have been that the technicians in this survey were well established in their positions, possibly indicating a higher level of teaching confidence compared with that of other technicians.
Despite these limitations, the resulting data provide a preliminary understanding of some of the key issues underlying the educational relationship between pharmacy technicians and student pharmacists. Future studies should be conducted to refine the survey instrument and generate results that are more representative of the 2 populations.
One survey found that the most frequent factors that contribute to errors in medication preparation are interruptions and inadequate staffing, which is an important consideration to take into account when adding student pharmacist education to a technician's responsibilities.9 Although having an inexperienced student pharmacist at a site could lead to both of these conditions, there are ways to overcome these obstacles, such as providing student pharmacists with adequate site orientation and training. The survey also emphasized the importance of technicians buying into the educational process. As technicians are becoming more important players in pharmacy education, their contributions are invaluable. In addition to pharmacist training for preceptors, colleges and schools of pharmacy need to provide similar training targeted toward technicians.
CONCLUSION
With implementation of the 2007 accreditation standards requiring 300 IPPE hours, student pharmacists will be spending a significant amount of time in hospital and community pharmacy settings. While it is important for them to learn the tasks and responsibilities of the profession from pharmacists, there are some competencies that are appropriate for them to learn from pharmacy technicians. This study demonstrates that technicians feel they have the ability to educate and that student pharmacists are receptive to the idea. To ensure a successful exchange, technicians need to have clear expectations of their roles as educators and students need a clear understanding of the competencies they are expected to learn during their IPPEs.
ACKNOWLEDGEMENT
The authors acknowledge Paul Henkel, DSocSc Candidate, for his assistance during the development of the technician survey instrument.
REFERENCES
- 1.Accreditation Council for Pharmacy Education. Accreditation standards. http://www.acpe-accredit.org/pdf/FinalS2007Guidelines2.0.pdf. Accessed August 13, 2011.
- 2.American Association of Colleges of Pharmacy. Center for the Advancement of Pharmaceutical Education. Pharmacy Practice Supplement. http://www.aacp.org/resources/education/Documents/PharmacyPracticeDEC006.pdf. Accessed August 13, 2011.
- 3.Model Curriculum for Pharmacy Technician Training. American Society of Health-System Pharmacists. http://www.ashp.org/Import/ACCREDITATION/TechnicianAccreditation/StartingaTrainingProgram/ModelCurriculum.aspx. Accessed August 13, 2011.
- 4.Desselle SP. Construction, implementation, and analysis of summated rating attitude scales. Am J Pharm Educ. 2005;(5):69. Article 97. [Google Scholar]
- 5.Draugalis JR, Coons SJ, Plaza CM. Best practices for survey research reports: a synopsis for authors and reviewers. Am J Pharm Educ. 2008;(1):72. doi: 10.5688/aj720111. Article 11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Exam Preparation. Pharmacy Technician Certification Board. https://www.ptcb.org/AM/Template.cfm?Section=About_the_Exam1&Template=/CM/ContentDisplay.cfm&ContentID=3057. Accessed August 13, 2011.
- 7.Riegelman RK. Studying a Study & Testing a Test: How to Read the Medical Evidence. 5th ed. Philadelphia: Lippincott Williams & Wilkins; 2005. p. 346. [Google Scholar]
- 8.Cohen J. Statistical Power Analysis for the Behavioral Sciences. 2nd ed. New York: Lawrence Erlbaum Associates; 1988. pp. 79–83. [Google Scholar]
- 9.Desselle SP. Certified pharmacy technicians’ views on their medication preparation errors and educational needs. Am J Health-Syst Pharm. 2005;62(19):1992–1997. doi: 10.2146/ajhp040549. [DOI] [PubMed] [Google Scholar]