Abstract
Objective. To describe patient safety instruction in health professional curricula, including medicine, nursing, pharmacy, and dentistry.
Methods. A systematic review of the literature from 1966 through 2010 was conducted using 6 databases and based on 3 search criteria: safety management, patient safety, and curriculum.
Results. One hundred fifty-four articles were identified and 23 met inclusion criteria. A variety of educational methods have been used in health profession curricula to promote patient safety including lectures, workshops, objective structured clinical examinations, standardized patients, simulation exercises, root cause analysis, quality assurance projects, and other interactive learning methods. The development of patient safety curricula has been primarily discipline-specific, with little interdisciplinary research found.
Conclusions. Safe, patient-centered care is directly influenced by the quality of education that healthcare professions students receive. From this literature review, research is needed to guide curricular change, specifically focusing on instructional methods and interdisciplinary collaborations.
Keywords: patient safety, health profession, curriculum, medication safety
INTRODUCTION
Approximately 98,000 people die each year in US hospitals from preventable medical errors, and these errors cost $30 billion in lost income and increased health expenditures.1 The impact of these errors has led hospitals and regulatory agencies to focus on reducing the number of deaths and adverse events attributed to unintended and preventable medical errors.1-3 In To Err Is Human: Building a Safer Health System, the Institute of Medicine (IOM) called for reevaluation of health professions education and the incorporation of patient safety into the curriculums of all health professions.1
In Crossing the Quality Chasm, the Institute of Medicine emphasized the need for healthcare professional educators to create new approaches in developing patient safety and quality improvement skills in their students.4 In a follow-up report, Health Professions Education: A Bridge to Quality, the IOM clarified their vision, recommending that “all health professionals should be educated to deliver patient-centered care as members of an interdisciplinary team, emphasizing evidence-based practice, quality improvement approaches, and informatics.”5-6
In light of this recommendation, educators should consider the development of a revised set of competencies for health professions’ curriculums.5,7 Health professionals, using scientific evidence, should be able to describe the components of patient-centered care, identify deviations from patient-centered care in their practices, and determine what actions should be initiated, if necessary, to correct those deviations.8 Educators in medicine, nursing, and other health professions are challenged to develop learning experiences that provide the foundation for professional identity and enable graduates to deliver patient-centered care as members of an interdisciplinary team while emphasizing evidence-based practice, quality improvement approaches, and informatics.4 Schools of nursing are addressing patient safety education through the Quality and Safety Education for Nurses initiative.9 Additionally, the Accreditation Council for Pharmacy Education (ACPE) strongly encourages the addition of quality improvement education to pharmacy curricula.10
Although patient safety has been acknowledged as necessary in the provision of quality patient-centered care, few studies have been published that describe the design, implementation, and assessment of patient safety education. Describing the state of patient safety education in the health professions would provide educators with additional resources to develop patient safety initiatives. The purpose of this article was to describe research conducted on patient safety instruction in the health professions in order to inform health professions educators of ways to incorporate this type of instruction in their curricula.
METHODS
A search of the following databases was conducted for articles published between 1966 and December 2010: PubMed, Cochrane, MEDLINE, ERIC, Academic Search Premier, and ISI Web of Science. The following MeSH terms were used: ‘‘safety management’’ or ‘‘patient safety’’ and ‘‘education, dental’’ or ‘‘education, medical’’ or ‘‘education, nursing’’ or ‘‘education, pharmacy’’ and ‘‘curriculum.’’ Only articles that described patient safety education in US health professions curriculum (medicine, nursing, pharmacy, and/or dentistry) were included.
One hundred fifty-four articles were identified and the abstracts evaluated for inclusion and exclusion criteria. Studies that were not about curriculum (30 articles) or patient safety (31 articles), or were not in English (3 articles) were excluded. Articles that focused on curriculums outside the United States (50 articles), as well as editorials, letters to the editor, and commentaries (12 articles), also were excluded. Also, 2 continuing education articles and 3 articles pertaining to other health-related professions were eliminated.
RESULTS
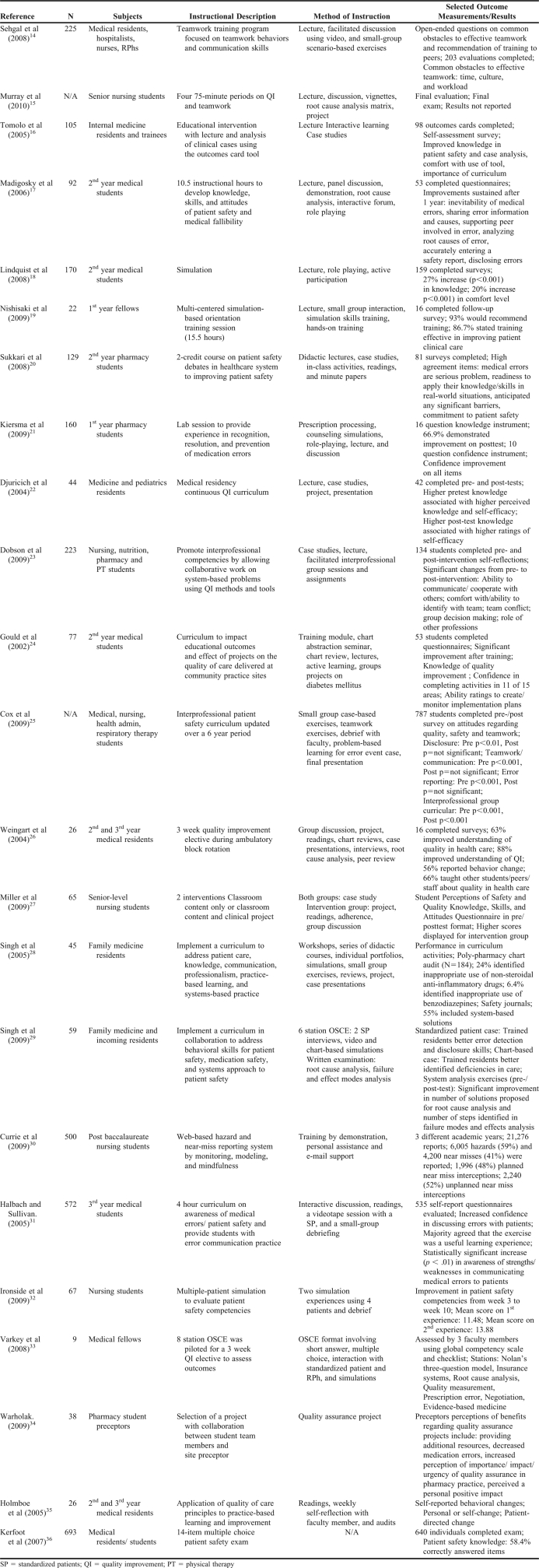
Twenty-three articles met all criteria for inclusion in the review. For all studies included in this review (Appendix 1), the following data were gathered: title, authors, date, type and total number of subjects, description of the course or initiative, method of instruction, and outcome measurements or assessments (if applicable).
Since 2000, several discipline-specific surveys have been conducted to determine types of instruction and content offered in patient safety at health professions schools.11-13 However, a systematic review of patient safety initiatives in the health professions has not been conducted. For the majority (69.5%) of studies included in this review, the focus was to educate students on aspects of patient safety using multiple methods. Several programs were in place for medical residents or fellows (39.1%), as well as other licensed health practitioners (13%). There were no articles describing patient safety initiatives in dentistry. Various methods of instruction were used to educate health professions students on patient safety. Thirteen of the studies were completed by medicine, 4 by nursing, and 3 by pharmacy, and 3 were interprofessional efforts.
Instructional Pedagogy
A wide variety of instructional approaches were used among the studies. The most frequently used instructional approaches in the studies were lectures,14-24 case-based exercises,16,20,22-23,24-29 active-learning exercises,14,16-19,24-25,28,30-31 and discussion.14-15,17,21,26-27,31,32 Simulation exercises were common, including the use of standardized patients29,31-33 and role-plays.17,18,21 Projects and presentations also were used as a way to engage participants with patient safety topics.15,22,24-28,34,35 Of all the initiatives, only 1 described a self-directed curriculum, which was focused on diabetes quality care principles for medical residents.36 The curriculum included readings, weekly self-reflections, and medical record audits. In the appendix, a compilation of the patient safety topics offered by these initiatives is provided.
Assessment
Assessment of the effectiveness of the instruction varied from measuring student attitudes to administering examinations. Self-assessment was commonly used among all the initiatives to quantify changes in knowledge, confidence, attitude, and skills. Eight medical education studies used self-assessment. In the studies, participants reported improvements in attitude,17,26 knowledge,16,18,24 confidence,18,19,24,31 and/or skills17,19,24,35 as a result of patient safety instruction. In nursing, Miller and colleagues administered a self-assessment survey instrument to determine students’ perceptions of safety and quality knowledge, skills, and attitudes.27 As in medicine, improvement was seen as a result of a safety initiative. Two of the pharmacy education studies used self-assessment survey instruments and reported improvements in knowledge,20,21 confidence,20,21 attitudes,20 and/or skills.20 Two of 3 of the interprofessional safety initiatives reported improvements in attitudes14 or skills23 after completion of safety instruction through the use of a self-assessment instrument.
Seven of the studies used knowledge examinations or objective structured clinical examinations (OSCEs) to assess student knowledge regarding patient safety.15,22,28-29,32,33,36 In 2 of the studies, a multiple station objective structured clinical examination (OSCE) was used to assess students’ performance on a variety of patient safety issues including detecting a medication error, addressing an adverse event or deficient care, and conducting a root cause analysis.28,33 Participants performed well in both studies (100% pass rate) in areas including: root cause analysis, prescription error, negotiation, and evidence-based medicine stations33 or improved error detection and disclosure skills and identification of deficiencies of care.28
Study Design
The most commonly employed study design was postassessment, after completion of the patient safety content. However, several initiatives used a more complex design, including a control group,27 mixed methods,27 pre- and postassessment,21-23,25,29 and/or an assessment 1 year after completion of content.17
DISCUSSION
Conservative estimates rank medical errors as the eighth leading cause of death in the United States. In fact, deaths from medical errors are greater than those from motor vehicle accidents, breast cancer, and acquired immunodeficiency syndrome (AIDS) combined.1 The Institute of Medicine report To Err Is Human addressed the need for safer systems of care and an increased focus on patient safety and systems engineering.1 A general strategy that has been proposed to create safer systems is to provide specific education on patient safety in the health professions curriculum.4 According to Kirch and Boysen, there are 5 critical success factors in the development of a culture of safety: (1) explicit leadership; (2) early engagement of health profession students; (3) the use of residents to educate students about patient safety; (4) the use of health information technology; and (5) promoting teamwork among the health professions.37
From the 23 articles reviewed, we found that some of these factors were considered as part of the safety initiatives described, including the promotion of teamwork and use of health information technology. Although teamwork was reported as a part of these initiatives, few interdisciplinary patient safety initiatives were identified in this review. In some of these programs, teamwork was discussed but no interaction with other disciplines took place. Also, other critical factors were not emphasized, such as the use of medical residents in teaching and early engagement of health professions students. In 9 of the initiatives, the focus was on training medical residents rather than on using them to educate students.
In Contemporary Issues in Medicine: Quality of Care, the Association of American Medical Colleges (AAMC) advocated adding patient safety education to undergraduate curricula.38 Despite evidence of curricular innovation at a few institutions, it is unclear to what extent medical schools have initiated patient safety training for their undergraduate students 5 years after the AAMC's call for national implementation of instructional programs.17,31,39 The articles identified in this review suggest that efforts are being made to implement patient safety training; however, they do not appear to be widespread. Instead, most efforts to introduce patient safety education appear to have been directed toward residents and physicians already in practice.40,41
An interdisciplinary group of healthcare providers, senior healthcare administration, students, residents, patient advocacy leaders, and curriculum development/assessment experts met to develop a patient safety undergraduate medical curriculum and identified 11 specific elements essential to an effective patient safety curriculum for medical students42: the history of the medical error crisis, interdisciplinary teamwork skills, time and stress management, healthcare microsystems, informatics, electronic medical records, and healthcare technology, error science, error management, and human factor science, communication skills, techniques of full-disclosure, risk management and root cause analysis, continuous quality improvement including outcome measures, and medication errors and reconciliation.42 Many of the programs cited in this review included these elements as part of their patient safety initiatives. However, some of the initiatives were limited in scope and emphasized only a subset of the 11 specific elements, while others were embedded in the curriculum and included all of these elements. Although these elements are recognized by many health professions educators as essential, the inclusion of every element may not be found in all health professions schools.
To educate students on the elements proposed in the patient safety curriculum, a variety of educational methods and strategies could be used including plenaries, small-group learning, experiential learning, simulation, role-plays with standardized patients, case-based learning, individual and team-based learning, and supportive audio-visual materials.43 Structured activities with immediate assessment and feedback are essential to effective learning and retention of information, as well as necessary skills and attitudes.43,44 Many of these approaches were found in the studies cited, either used in isolation or as a multi-faceted approach.
Prompted by national initiatives, the majority of nursing organizations, agencies, and educational programs have increased the emphasis on patient safety and competence in clinical practice.45,46 Evidence of the value of quality and safety competencies is apparent in nursing publications,47-50 standards of practice,51 and accreditation guidelines.52,53 Finkelman and Kenner describe the incorporation of IOM recommendations into the nursing curricula.54 The Quality and Safety Education for Nurses initiative developed competencies, including competencies related to safety, that would apply to all registered nurses.55,56
Although there is extensive nursing literature describing safety and its place in curriculum, few nursing studies were identified in this review, making the extent to which patient safety is addressed in the nursing curriculum unclear. Smith and colleagues conducted a survey to describe quality and safety education in nursing programs.11 From the 195 completed surveys instruments, the majority (>95%) of respondents reported the inclusion of content related to each Quality and Safety Education for Nurses competency (evidence-based practice, teamwork and collaboration, informatics, safety and quality improvement) in their programs. The content was presented in several courses, though a small percentage of schools reported having dedicated courses to teach the competencies. The differentiation between elective and required courses was not assessed. The most common educational methods were: readings (84%), lecture (83%), clinical (75%), case study (57%), paper assignments (56%), course modules (52%), Web-based learning (52%), problem-based learning (49%), interprofessional learning (43%), simulation (43%), return demonstration (36%).12 Simulation was used less frequently than all other pedagogical strategies except return demonstrations. Based on this data, nurse educators appear to have implemented initiatives in the curriculum to address safety competencies.
In 2001, Johnson and Latif surveyed schools of pharmacy to assess the manner and extent to which medication errors were incorporated into the curriculum.13 Of the responding institutions, the majority had embedded medication error instruction in pharmacy administration, therapeutics, or law courses. The majority of instruction was lecture based, with content in human error, medical errors, medication errors, quality or process improvement, root cause analysis, and failure mode and effects analysis. Active learning was incorporated within laboratories at a few responding institutions. Few articles have been published since the 2001 study regarding specific initiatives addressing safety in pharmacy curricula. Patient safety is a component of Standard 9 of accreditation guidelines, indicating ACPE's expectation that it be included in the curriculum.10
The Educating Pharmacy Students and Pharmacists to Improve Quality (EPIQ) program could assist educators in meeting accreditation guidelines.57 EPIQ was developed as a quality improvement education resource to educate students, pharmacists, and other stakeholders in measuring, reporting, and improving quality in pharmacy practice.57 The EPIQ program contains 5 modules (17 sessions on quality improvement that address: the status of quality improvement and reporting in the US healthcare system, patient safety concepts and definitions, measurement, interventions and incentives, and application to the pharmacy practice setting.57 The modules are not sequential and can be used in any order. Each module contains several education sessions, which include a lecture, a learner-centered activity (eg, group activities, case studies), and a discussion, as well as supplemental readings and other relevant topic-specific materials.57
Dental schools are unique among US health care education sites. Unlike medical, nursing, and pharmacy schools, dental schools are the only healthcare education sites that consistently provide patient care within their schools. As expected, the current dental school accreditation process focuses primarily on the educational outcomes of the school, with limited attention to patient safety issues. No studies from dentistry were found in this review. The magnitude and complexity of patient safety issues in dentistry differ from those found in hospitals; thus, patient safety may not be considered a high priority because of the lower morbidity, mortality, and financial impact resulting from human error.13
To influence student behavior, research has shown classroom content should be applied to clinical activities and projects.58 However, safety and quality have remained primarily in classroom content. Three reasons have been suggested for the lack of widespread engagement of health professions learners with quality and safety issues in the past: (1) quality and safety issues were not identified as educational priorities in the United States until recently, (2) faculty members do not feel confident teaching this content, and (3) quality care and systems improvements have not reached the forefront of clinical practice.59
CONCLUSIONS
As healthcare becomes more complex, safe patient-centered care is directly influenced by the quality of the education that health care professionals receive. Based on a review of the literature, further research to support and guide curricular change and more studies focused on instructional methods are needed.
Health profession students could benefit from a problem-based learning curriculum, which encourages discussion, collaboration, quality improvement, and the value of learning from errors in a variety of domains related to clinical practice. Also, simulated experiences would provide students with a more realistic view of practice and allow them to visualize how they will be able to practice within complex situations.60 As health profession disciplines continue to investigate methods to train the next generation of students for practice and to ascertain the achievement of patient safety competencies prior to entry into the workforce, evidence is needed to document the effectiveness of these efforts.
Appendix 1.
REFERENCES
- 1.Kohn L, Corrigan J, Donaldson M, editors. To Err Is Human: Building a Safer Health System. Washington, DC: National Academy Press; 2000. [PubMed] [Google Scholar]
- 2.The Joint Commission. National Patient Safety Goals. 2009. http://www.jointcommission.org/standards_information/npsgs.aspx. Accessed August 27, 2010.
- 3.Jha A, Orav EJ, Li Z, Epstein AM. The inverse relationship between performance in the hospital quality alliance measures and mortality rates. Health Aff. 2007;26(4):1104–1110. doi: 10.1377/hlthaff.26.4.1104. [DOI] [PubMed] [Google Scholar]
- 4.Committee on Quality of Health Care in America, Institute of Medicine. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC: National Academy of Sciences Press; 2001. [Google Scholar]
- 5.Greiner AC, Knebel E, editors. Health Professions Education: A Bridge to Quality. Washington, DC: National Academies Press; 2003. [PubMed] [Google Scholar]
- 6.Thompson SA, Tilden VP. Embracing quality and safety education for the 21st century: building interprofessional education. J Nurs Educ. 2009;48(12):698–701. doi: 10.3928/01484834-20091113-13. [DOI] [PubMed] [Google Scholar]
- 7.VanGeest JB, Cummins DS. An educational needs assessment for improving patient safety: results of a national study of physicians and nurses. National Patient Safety Foundation White Paper Report. 2003 http://www.npsf.org/download/EdNeedsAssess.pdf. Accessed on September 15, 2011. [Google Scholar]
- 8.Batalden P. Developing health professionals capable of continually improving health care quality, safety and value: the health professional educator's work. http://www.ihi.org/offerings/ihiopenschool/resources/Pages/ImprovementStories/DevelopingHealthProfessionalsCapableOfContinuallyImprovingHealthCare.aspx. Accessed on September 15, 2011.
- 9.Cronenwett L, Sherwood G, Barnsteiner J, et al. Quality and safety education for nurses. Nurs Outlook. 2007;55(3):122–131. doi: 10.1016/j.outlook.2007.02.006. [DOI] [PubMed] [Google Scholar]
- 10.American Council for Pharmacy Education. Chicago: Accreditation Council for Pharmacy Education; 2007. Accreditation standards and guidelines for the professional program in pharmacy leading to the Doctor of Pharmacy degree. [Google Scholar]
- 11.Smith EL, Cronenwett L, Sherwood G. Current assessments of quality and safety education in nursing. Nurs Outlook. 2007;55(3):132–137. doi: 10.1016/j.outlook.2007.02.005. [DOI] [PubMed] [Google Scholar]
- 12.Leong P, Afrow J, Weber HP, Howell H. Attitudes toward patient safety standards in U.S. dental schools: a pilot study. J Dent Educ. 2008;72(4):431–437. [PubMed] [Google Scholar]
- 13.Johnson MS, Latif DA, Gordon B. Medication error instruction in schools of pharmacy curricula: a descriptive study. Am J Pharm Educ. 2002;66(4):364–371. [Google Scholar]
- 14.Sehgal NL, Fox M, Vidyarthi AR, Sharpe BA, et al. A multidisciplinary teamwork training program: the triad for optimal patient safety (TOPS) experience. J Gen Intern Med. 2008;23(12):2053–2057. doi: 10.1007/s11606-008-0793-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Murray ME, Douglas S, Girdley D, Jarzemsky P. Teaching quality improvement. J Nurs Educ. 2010;49(8):466–469. doi: 10.3928/01484834-20100430-09. [DOI] [PubMed] [Google Scholar]
- 16.Tomolo A, Caron A, Perz ML, Fultz T, Aron DC. The outcomes card: development of a systems-based practice educational tool. J Gen Intern Med. 2005;20(8):769–771. doi: 10.1111/j.1525-1497.2005.0168.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Madigosky WS, Headrick LA, Nelson K, et al. Changing and sustaining medical students’ knowledge, skills, and attitudes about patient safety and medical fallibility. Acad Med. 2006;81(1):94–101. doi: 10.1097/00001888-200601000-00022. [DOI] [PubMed] [Google Scholar]
- 18.Lindquist LA, Gleason KM, McDaniel MR, Doeksen A, Liss D. Teaching medication reconciliation through simulation: A Patient safety Initiative for second year medical students. J Gen Intern Med. 2008;23(7):998–1001. doi: 10.1007/s11606-008-0567-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Nishisaki A, Hales R, Biagas K, Cheifetz I. A multiinstitutional high-fidelity simulation boot camp orientation and training program for first year pediatric critical care fellows. Pediatr Crit Care Med. 2009;10(2):157–162. doi: 10.1097/PCC.0b013e3181956d29. [DOI] [PubMed] [Google Scholar]
- 20.Sukkari SR, Sasich LD, Tuttle DA, Abu-Baker AM, Howell H. Development and evaluation of a required patient safety course. Am J Pharm Educ. 2008;72(3):Article 65. doi: 10.5688/aj720365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kiersma ME, Darbishire PL, Plake KS, Oswald C, Walters BM. Laboratory session to improve first-year pharmacy students’ knowledge and confidence concerning the prevention of medication errors. Am J Pharm Educ. 2009;73(6):Article 99. doi: 10.5688/aj730699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Djuricich AM, Ciccarelli M, Swigonski NL. A continuous quality improvement curriculum for residents: addressing core competency, improving systems. Acad Med. 2004;79(10):S65–S67. doi: 10.1097/00001888-200410001-00020. [DOI] [PubMed] [Google Scholar]
- 23.Dobson RT, Stevenson K, Busch A, Scott DJ, Henry C, Wall PA. A quality improvement activity to promote interprofessional collaboration among health professions students. Am J Pharm Educ. 2009;73(4):Article 64. doi: 10.5688/aj730464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gould BE, Grey MR, Huntington CG, et al. Improving patient care outcomes by teaching quality improvement to medical students in community-based practices. Acad Med. 2002;77(10):1011–1018. doi: 10.1097/00001888-200210000-00014. [DOI] [PubMed] [Google Scholar]
- 25.Cox KR, Scott SD, Hall LW, Aud MA. Uncovering differences among health professions trainees exposed to an interprofessional patient safety curriculum. Q Manage Health Care. 2009;18(3):182–193. doi: 10.1097/QMH.0b013e3181aea237. [DOI] [PubMed] [Google Scholar]
- 26.Weingart SN, Tess A, Driver J, Aronson MD, Sands K. Creating a quality improvement elective for medical house officers. J Gen Intern Med. 2004;19(8):861–87. doi: 10.1111/j.1525-1497.2004.30127.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Miller CL, LaFramboise L. Student learning outcomes after integration of quality and safety education competencies into a senior-level critical care course. J Nurs Educ. 2009;48(12):678–685. doi: 10.3928/01484834-20091113-07. [DOI] [PubMed] [Google Scholar]
- 28.Singh R, Naughton B, Taylor JS, et al. A comprehensive collaborative patient safety residency curriculum to address the ACGME core competencies. Med Educ. 2005;39(12):1195–1204. doi: 10.1111/j.1365-2929.2005.02333.x. [DOI] [PubMed] [Google Scholar]
- 29.Singh R, Singh A, Fish R, McLean D, Anderson DR, Singh G. A patient safety objective structured clinical examination. J Patient Saf. 2009;5(2):55–60. doi: 10.1097/PTS.0b013e31819d65c2. [DOI] [PubMed] [Google Scholar]
- 30.Currie LM, Desjardins KS, Levine ES, et al. Web-based hazard and near-miss reporting as part of a patient safety curriculum. J Nurs Educ. 2009;48(12):669–677. doi: 10.3928/01484834-20091113-03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Halbach JL, Sullivan LL. Teaching medical students about medical errors and patient safety: evaluation of a required curriculum. Acad Med. 2005;80(6):600–606. doi: 10.1097/00001888-200506000-00016. [DOI] [PubMed] [Google Scholar]
- 32.Ironside PM, Jeffries PR, Martin A. Fostering patient: safety competencies using multiple-patient simulation experiences. Nurs Outlook. 2009;57(6):332–337. doi: 10.1016/j.outlook.2009.07.010. [DOI] [PubMed] [Google Scholar]
- 33.Varkey P, Natt N, Lesnick T, Downing S, Yudkowsky R. Validity evidence for an OSCE to assess competency in systems-based practice and practice-based learning and improvement: a preliminary investigation. Acad Med. 2008;83(8):775–780. doi: 10.1097/ACM.0b013e31817ec873. [DOI] [PubMed] [Google Scholar]
- 34.Warholak TL. Preceptor Perceptions of pharmacy student team quality assurance projects. Am J Pharm Educ. 2009;73(3):Article 47. doi: 10.5688/aj730347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Holmboe ES, Prince L, Green M. Teaching and improving quality of care in a primary care internal medicine residency clinic. Acad Med. 2005;80(6):571–577. doi: 10.1097/00001888-200506000-00012. [DOI] [PubMed] [Google Scholar]
- 36.Kerfoot BP, Conlin PR, Travison T, McMahon GT. Patient safety knowledge and its determinants in medical trainees. J Gen Intern Med. 2007;22(8):1150–1154. doi: 10.1007/s11606-007-0247-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kirch DG, Boysen PG. Changing the culture in medical education to teach patient safety. Health Aff. 2010;29(9):1600–1603. doi: 10.1377/hlthaff.2010.0776. [DOI] [PubMed] [Google Scholar]
- 38.Association of American Medical Colleges. Report V: Contemporary Issues in Medicine: Quality of Care. http://laico.org/v2020resource/files/quality_of_care.pdf. Accessed September 15, 2011.
- 39.Moskowitz E, Veloski JJ, Fields SK, Nash DB. Development and evaluation of a 1-day interclerkship program for medical students on medical errors and patient safety. Am J Med Qual. 2007;22(1):13–17. doi: 10.1177/1062860606296669. [DOI] [PubMed] [Google Scholar]
- 40.American Board of Internal Medicine. Practice Improvement Modules. http://www.abim.org/moc/practical-advice/PIM.aspx. Accessed September 15, 2011. [DOI] [PMC free article] [PubMed]
- 41.Kachalia A, Johnson JK, Miller S, Brennan T. The incorporation of patient safety into board certification examinations. Acad Med. 2006;81(4):317–325. doi: 10.1097/00001888-200604000-00004. [DOI] [PubMed] [Google Scholar]
- 42.Mayer D, Klamen DL, Gunderson A, Barach P. Designing a patient safety undergraduate medical curriculum: the Telluride interdisciplinary roundtable experience. Teach Learn Med. 2009;21(1):52–58. doi: 10.1080/10401330802574090. [DOI] [PubMed] [Google Scholar]
- 43.Phye GD, Andre T. Delayed retention effect: attention, perseveration, or both? Contemporary Educ Psychol. 1989;1989;14(2):173–185. [Google Scholar]
- 44.Karl KA, O'Leary-Kelly AM, Martocchio JJ. The impact of feedback and self-efficacy on performance in training. J Org Behav. 1993;14(4):379–394. [Google Scholar]
- 45.Hofler LD. Nursing education and transition to the work environment: a synthesis of national reports. J Nurs Educ. 2008;47(1):5–12. doi: 10.3928/01484834-20080101-06. [DOI] [PubMed] [Google Scholar]
- 46.Lenburg CB. The influence of contemporary trends and issues on nursing education. In: Cherry B, Jacob S, editors. Contemporary Nursing: Issues, Trends, and Management. 4th ed. St Louis, MO: Elsevier Mosby; 2008. [Google Scholar]
- 47.Cronenwett L. Educating health professional heroes of the future: the challenge for nursing. Front Health Serv Manage. 2001;18(2):15–21. [PubMed] [Google Scholar]
- 48.Maddox PJ, Wakefield M, Bull J. Patient safety and the need for professional and educational change. Nurs Outlook. 2001;49(1):8–13. doi: 10.1067/mno.2001.113642. [DOI] [PubMed] [Google Scholar]
- 49.Arnold L, Campbell A, Dubree M, et al. Priorities and challenges of health system chief nurse executives: insights for nursing educators. J Prof Nurs. 2006;22(4):213–220. doi: 10.1016/j.profnurs.2006.06.002. [DOI] [PubMed] [Google Scholar]
- 50.Armstrong GE, Spencer TS, Lenburg CB. Using quality and safety education for nurses to enhance competency outcome performance assessment: a synergistic approach that promotes patient safety and quality outcomes. J Nurs Educ. 2009;48(12):686–693. doi: 10.3928/01484834-20091113-02. [DOI] [PubMed] [Google Scholar]
- 51.American Nurses Association. Silver Spring, MD: ANA; 2004. Nursing: Scope and standards of practice. [Google Scholar]
- 52.American Association of Colleges of Nursing. The essentials of baccalaureate education for professional nursing practice. Washington, DC: AACN; 1998. [Google Scholar]
- 53.National Organization of Nurse Practitioner Faculties and the American Association of Colleges of Nursing. Nurse Practitioner Primary Care Competencies in Specialty Areas. Washington, DC: US DHHS; 2002. HRSA, Bureau of Health Professions, Division of Nursing. [Google Scholar]
- 54.Finkelman AW, Kenner C. Teaching the IOM: Implications of the IOM Reports for Nursing Education. Silver Spring, MD: American Nurses Association; 2009. [Google Scholar]
- 55.Sherwood G, Drenkard K. Quality and safety curricula in nursing education: matching practice realities. Nurs Outlook. 2007;55(3):151–155. doi: 10.1016/j.outlook.2007.02.004. [DOI] [PubMed] [Google Scholar]
- 56.Preheim GJ, Armstrong GE, Barton AJ. The new fundamentals in nursing: introducing beginning quality and safety education for nurses’ competencies. J Nurs Educ. 2009;48(12):694–697. doi: 10.3928/01484834-20091113-10. [DOI] [PubMed] [Google Scholar]
- 57.Warholak TL, West D, Holdford DA. The educating pharmacy students and pharmacists to improve quality program: tool for pharmacy practice. J Am Pharm Assoc. 2010;50(4):534–538. doi: 10.1331/JAPhA.2010.10019. [DOI] [PubMed] [Google Scholar]
- 58.Durham CF, Sherwood GD. Education to bridge the quality gap: a case study approach. Urol Nurs. 2008;28(6):431–438. [PubMed] [Google Scholar]
- 59.Ladden MD, Bednash Stevens DP, Moore GT. Educating interprofessional learners for quality, safety and systems improvement. J Interprof Care. 2006;20(5):497–505. doi: 10.1080/13561820600935543. [DOI] [PubMed] [Google Scholar]
- 60.Taylor PA. Strategies for enhancing student learning by managing ambiguities in clinical settings. Nurs Educ. 2000;25(4):173–174. doi: 10.1097/00006223-200007000-00012. [DOI] [PubMed] [Google Scholar]