Abstract
As colleges and schools of pharmacy develop core courses related to patient safety, course-level outcomes will need to include both knowledge and performance measures. Three key performance outcomes for patient safety coursework, measured at the course level, are the ability to perform root cause analyses and healthcare failure mode effects analyses, and the ability to generate effective safety communications using structured formats such as the Situation-Background-Assessment-Recommendation (SBAR) situational briefing model. Each of these skills is widely used in patient safety work and competence in their use is essential for a pharmacist's ability to contribute as a member of a patient safety team.
Keywords: performance outcomes, patient safety, root cause analysis, failure mode and effects analysis, structured communication
The 1995 background papers of the Commission to Implement Change in Pharmaceutical Education set forth key elements to train pharmacists capable of participating in the healthcare system of the future.1 Yanchick demonstrated that the broad competency categories identified in background paper 52 aligned well with the 2003 recommendations of the Health Professions Education Summit, which called for all health professionals to be able to demonstrate proficiency in delivering patient-centered care, working in interdisciplinary teams, employing evidence-based practice, applying quality improvement approaches, and using informatics.3 As pharmacy programs establish coursework to prepare student pharmacists to participate in patient safety and quality improvement activities, both knowledge-based outcomes and performance outcomes must be developed. This paper discusses 3 performance outcomes that should be included and assessed at the course level to ensure that pharmacists on health care teams are able to effectively implement quality assurance programs and communicate patient safety concerns. Two of the competencies deal with widely-adopted formal approaches to assessing or predicting potential medical errors: root cause analysis (RCA) and failure mode and effects analysis (FMEA). The third competency is the ability to effectively use situational briefing formats; specifically, the Situation-Background-Assessment-Recommendation (SBAR) model, which is becoming the primary format for communication among nurses, physicians, and other health care providers regarding specific patient care situations.
RESIDENCY COMPETENCIES AS GUIDES FOR A PATIENT SAFETY CURRICULUM
In response to the growing awareness of morbidity and mortality arising from medical errors, and to the recommendations of the Health Professions Education Summit, health professions residency directors have increased their programs’ attention to patient safety skills and behaviors. The Accrediting Council on Graduate Medical Education (ACGME) has established 6 core competencies that should form the basis of medical residency training: patient care, medical knowledge, practice-based learning, communication, professionalism, and system-based practice.4 Patient safety competencies are imbedded in each of these areas.
Two reports have examined specific performance outcomes that should be included in a medical residency. A needs assessment for a patient safety curriculum for residencies at the Mayo School of Graduate Medical Education surveyed the medical directors and key informants in 8 of the school's largest specialty programs.5 Four content areas were identified as critical by all of the programs: training the resident to explicitly seek help when in doubt; achieving residents’ understanding of the role of fatigue in medical error; life support skills; and sentinel event reporting and management.
Faculty members from the schools of medicine, nursing, and pharmacy at the State University of New York - Buffalo developed the following patient safety performance objectives, which correspond to the 6 ACGME competencies, for their family medicine residency program6:
Patient care: (a) recognize and understand team behaviors that strengthen/weaken patient safety; (b) Incorporate effective team behaviors into their practices
Medical knowledge: (a) recognize and analyze inappropriate prescribing in elderly patients; (b) practice appropriate prescribing for elderly patients
Practice-based learning: (a) identify errors in their practices, analyze them, and learn from them; (b) develop system-based strategies to prevent recurrence of errors
Communication: (a) recognize and understand communication behaviors that strengthen/weaken patient safety; (b) incorporate effective communication behaviors into their practices
Professionalism: (a) understand ethical and legal issues surrounding error disclosure; (b) provide appropriate disclosure to patients when errors occur
System-based practice: (a) identify and prioritize vulnerabilities in their practice systems; (b) develop and implement system-based solutions to the identified vulnerabilities
The curriculum is divided into 3 modules taught across the 3 residency years. The curriculum in the first postgraduate year (PGY1) focuses on a behavioral skills cluster, including patient care, communications, and professionalism. The curriculum for PGY2 focuses on polypharmacy or the medication safety cluster, including medical knowledge and practice-based learning, with a pharmacist faculty member directly involved in the training. In the final, PGY3, year, the curriculum focuses on systems approaches in a systems safety cluster featuring practice-based learning and systems-based practice competencies. Two key objectives included in PGY3 are demonstration of ability to take part in RCA and FMEA processes.
Pharmacy practice residency accreditation guidelines also include standards that require residents to gain skills to ensure patient safety and improve quality of care in their practice settings. For example, the American Society of Health-System Pharmacists/American Pharmacists Association's required outcomes for PGY1 community pharmacy practice residents include that they be able to “Identify, design, and implement quality improvement changes to the organization's (eg, community pharmacy, corporation, health-system) medication-use system.” The objectives for this goal include an understanding of the role of RCA and FMEA as tools for analyzing medication use processes.7
As pharmacy curricula better emphasize interdisciplinary training, patient safety, and quality improvement, pharmacy educators should be able to recognize how these performance outcomes in medical and pharmacy residencies also are skills needed by pharmacy graduates entering practice. Because the system-based practice outcomes depend on effective team activities, and because effective communication among team members is essential to patient safety and quality clinical outcomes,8 doctor of pharmacy programs should teach approaches that are currently being taught to and used by other health professionals who will be participating with pharmacists on patient care teams.
THREE KEY PERFORMANCE OUTCOMES
Root Cause Analysis
Root cause analysis is a retrospective assessment used “to identify the critical underlying reasons for the occurrence of an adverse event or close call (near miss).”9 In an early description of RCA in 1991, Dew contrasted the importance of distinguishing between finding blame for a catastrophic event and determining the underlying, or root, cause of the disaster.10 He summarized the search for the root cause as identifying the problem, finding the immediate cause, taking action to resolve immediate concerns, and then looking for root causes which, when found, will aid in system redesign to prevent future catastrophes. “In nature,” Dew wrote, “roots are found in the soil. In organizations, the soil is the systematic factors that deal with how management plans, organizes, controls, and provides assurance of quality and safety in 5 key areas …” Dew introduced 3 tools to aid in finding root causes: the event and causal factor diagram, safeguard analysis (safeguards that can be put in place to reduce hazards, enforce compliance, or make targets invulnerable to hazards), and change analysis (a comparison of the current state with the prior state of the organization or system). Dew's 5 key areas for system analysis include personnel, procedures, equipment, materials, and environment.
RCA and FMEA are required elements of patient safety programs in inpatient and acute care institutions, but they are applicable to all practice settings. The Department of Veterans Affairs adopted a system of RCA in 1998 as 1 of 3 major tools for its Patient Safety Initiative, along with a patient safety reporting system and a Veterans Affairs version of FMEA.11 The initiative is applied in both inpatient and outpatient settings. The Joint Commission subsequently adopted a requirement for accredited institutions, centers, and clinics, to identify sentinel events and investigate each using RCA.12 Jackson urged that continuous quality improvement (CQI) be undertaken in community pharmacies, as well; he further advocated that “the entire pharmacy staff should be invited” to participate in the CQI effort, and he discussed RCA and FMEA as 2 important tools for identifying CQI priority targets.13 The Institute for Safe Medication Practices has announced a goal for 2011 to “develop a root cause analysis workbook for community pharmacies.”14
Great Britain and other European countries have adopted RCA for assessing errors in community pharmacies as well as inpatient pharmacies. An interdisciplinary team in Denmark performed RCAs on transcription errors in 40 Danish community pharmacies.15 In England, CQI is referred to as clinical governance and engaging in clinical governance is an essential requirement of the contract between primary care trusts (the 151 regional organizations in England that govern and administer primary, community, and secondary care under the National Health Service16) and community pharmacies.17 The South East Essex NHS Primary Care Trust includes basic information on RCA in a “clinical governance resource pack for community pharmacies,” and provides specific training to pharmacists in the Trust.18
In the United States, California expects new pharmacy graduates, regardless of their eventual practice setting, to be trained in the concepts of RCA, and includes questions regarding RCA in the California Practice Standards and Jurisprudence Examination for Pharmacists. The examination's content outline provides a good example of an outcome measure related to patient safety, indicating that the candidate should be able to “Participate in a system for medication error prevention, assessment, and reporting (eg, root cause analysis, National Patient Safety Goals, medication error reduction program).”19 The Massachusetts Board of Registration in Pharmacy adopted new rules in 2005 mandating CQI programs for community pharmacies, built on the experience in hospitals; its “best practices” suggested quarterly reviews of quality-related events and investigation of the root causes for quality-related events. The 23 best practice recommendations in its report provide a large variety of potential policy issues that could form the basis for student assignments or group case work.20
One national safety consultant has identified 4 classes of personnel who participate on RCA training teams (program champion, super-users, facilitators [safety practitioners], and participants) and their training needs, which range from attendance at a 3-day class/seminar to completion of an online computer learning program.21 Of the 4 personnel categories, doctor of pharmacy (PharmD) graduates entering practice fit best under the “participants” category, those who will be asked to serve on RCA teams and need to be able to perform basic RCA on individual problems and address the causes identified. Without more than institution-specific training by an employer, PharmD graduates should be prepared to participate effectively on RCA teams and identify and properly report sentinel events.
Failure Mode and Effects Analysis
While RCA is retrospective, FMEA is a forward-looking assessment of systems and processes designed to predict ways in which things can go wrong (failure modes), and the likely degree of injury or cost (effects) associated with each failure mode. FMEA thus provides a way to predesign systems and processes to improve their safety, and also serves as a tool to establish the highest priorities for investment of time and money to reduce harm. The Joint Commission sees FMEA as the logical follow up to RCA, providing the institution a means for “designing and implementing an action plan for improvement.”22
Two major forms of FMEA are currently in use. The VA uses a system called healthcare failure mode effects analysis (HFMEA),23 and many other institutions follow the guidelines for FMEA provided by the Institute for Healthcare Improvement (IHI). The principles of FMEA can be effectively taught by having students practice either approach; however, learning outcomes should assess students’ understanding of the differences in how each form implements these principles.
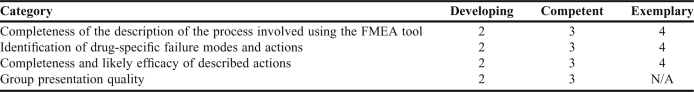
The IHI Web site features significant training materials and an interactive FMEA tool that can be used to provide teams of students with hands-on experience in developing an FMEA from an instructional case (personal memberships in IHI are available to faculty members and students without a fee.)24 In a patient safety course at Washington State University, we have assigned students to work in teams to develop an FMEA (using the IHI tool) relating to newly-released drugs that have required risk evaluation and mitigation strategies (REMS) as a condition of marketing. The grading rubric for this assignment is shown in Table 1. This project arose from Cohen's suggestion that FMEA is one approach to “proactively identify” ways in which high-risk drugs could lead to harm and allow for the design of safeguards for high-alert medications.25
Table 1.
Example Rubric for a 15-Point FMEA Group Assignment Involving a Written FMEA and a Group Presentation
As they should for RCA, PharmD graduates entering practice should be able to participate on a team assigned to undertake FMEA or HFMEA. Because the scope of an FMEA can be limited to a specific process, entry-level pharmacists may be asked to lead a focused-FMEA and should be capable of using or adapting available FMEA tools.
Situational Briefing Model
Recognizing that the majority of sentinel events reported to the Joint Commission include communication difficulties as a contributing factor, the Joint Commission established a National Patient Safety Goal in 2006 to improve the effectiveness of communication among caregivers, and a requirement that facilities implement standardized approaches to hand-offs (ie, transfer of care of the patient from one practitioner to another) that include opportunities to ask questions and respond to them.26 Perhaps the most widely adopted approach to communicating information about a patient's condition and immediate needs is a situational briefing model adapted from practices in the US Navy. SBAR stands for situation-background-assessment-recommendation, which are the 4 organizing elements around which a message is structured.
Prior to the phone call or face-to-face consultation, a practitioner seeking to communicate information about a patient's condition or needs uses a standardized template to organize his or her message. Relevant records or other patient information is kept at hand, and the important elements are placed into the appropriate SBAR sections of the template. The situation section of the SBAR message contains the reason for the contact, where the practitioner identifies him- or herself; the patient's name; location; and a brief statement of the problem; when it happened or started; and how severe the situation is. Pope and colleagues recommend that this should be done in no more than 10 seconds.27 The background section contains the patient's essential and relevant medical history. The assessment section should state the practitioner's analysis of what might be going on or what drug-therapy-related problem is at issue. The assessment should include information on severity and urgency. The recommendation section should present an explanation to the other provider of what the practitioner believes must be done or what action he or she is requesting of the other provider.
In addition to its widespread adoption in the United States, SBAR also has become the standard structured communication model in the United Kingdom's National Health Service for all professionals, including pharmacists in hospitals and in community pharmacies. The University Hospitals of Coventry and Warwickshire have created a “community pharmacy escalation” training video on the use of SBAR between a community-based pharmacist and a physician's office.28
Although the VA and many institutional pharmacies have adopted SBAR, there is little documentation that pharmacy educators teach SBAR as an integral part of the communications curriculum. Searches in PubMed Central using “SBAR” or “Situational Briefing” and “pharmacy,” or “Am J Pharm Educ,” yielded a single citation to a report by Brownlee and Bruce that described their use of SBAR presentations by student pharmacists as an element of pharmacy skills assessments conducted at 3 stages of the curriculum prior to student entry into advanced pharmacy practice experiences.29
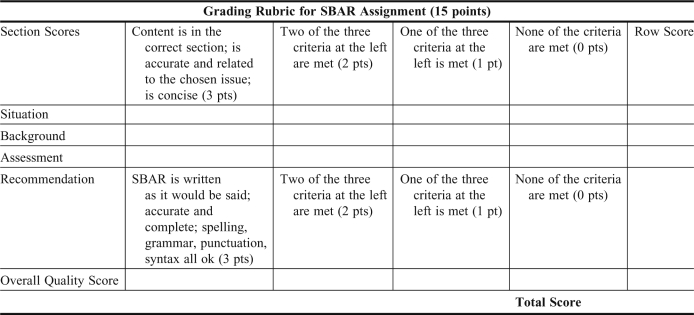
Using SOAP (subjective, objective, assessment, plan) notes to document patient encounters and treatment plans is firmly entrenched in PharmD curricula; a search on PubMed Central using “SOAP Am J Pharm Educ” yielded 42 articles in the Journal mentioning SOAP notes since 2006. The use of SBAR should be taught routinely as well. In the patient safety course at Washington State University, which is taught in the third year, students are assigned to develop SBARs from cases analyzed in other courses, choosing one of the recommendations from their case work to be the subject of the SBAR. A grading rubric for such an SBAR assignment is shown in Appendix 1.
RECOMMENDATIONS
The outcomes discussed here measure only a subset of the knowledge, skills, and attitudes necessary to promote a culture of patient safety and which must be acquired and assessed throughout the PharmD curriculum. Early instruction and practice in setting patient care goals, monitoring their achievement, and ensuring effective communication with others is essential to build the habits needed for safe professional practice. In-depth knowledge of risks and benefits of pharmacotherapy must be part of the pharmacist's expertise, especially as it is applied to geriatric and pediatric patients. Finally, PharmD graduates must have the informatics and systems skills to participate effectively in patient care and safety initiatives.
SBAR, RCA, and FMEA are well-established patient safety tools in inpatient and acute care settings. However, their use in community pharmacy practice is not the norm at present. This paper's emphasis on the need for community pharmacists to become greater participants on the health care team was not intended to deemphasize the need for these skills in inpatient practice, but to build the case for teaching SBAR, RCA, and FMEA in the PharmD curriculum as skills that graduates would need upon entry into practice rather than abilities used solely during or following postgraduate training.
Structured communication models, such as SBAR, should be taught early and practiced often, at least as early and often as the development of SOAP notes. In our experience, the SBAR format is best learned by requiring students in every skill laboratory or experiential practice setting to take time to develop an SBAR message for any brief communication intended to communicate a patient need to another practitioner. Students should not be expected to master SBAR messages in a single patient safety course.
RCA and FMEA approaches are probably best taught in the context of a specific patient safety curriculum component. Because RCA is retrospective, we have found it difficult for students to fully practice participating in an RCA team unless they can be provided with richly-detailed cases. Also, because an RCA in actual practice is performed in response to sentinel events, it is challenging to provide a student with a guaranteed opportunity to be involved on an RCA team while completing advance pharmacy practice experiences. Our current outcome objectives relating to RCA are primarily knowledge-based and focus on students’ ability to articulate on an examination the goals, purposes, and process of RCA.
FMEA, on the other hand, is used to anticipate possible ways in which a system can fail and does not depend on an adverse event to trigger its application. FMEA also may be used to improve existing systems, even in the absence of sentinel events. Group projects, ideally undertaken in an interdisciplinary setting with nursing, medical, dental, and other health professions students, provide the best approach to developing students’ skills as potential FMEA team members. Improvement stories at IHI include reports on successful redesign of processes in ambulatory pharmacy, medication dispensing and distribution, inpatient pharmacy services, oncology pharmacotherapy, and many other pharmacy-related areas.30 These reports provide a wide range of subjects that are suitable for student teams to build upon in practicing development of an FMEA.
Though not the only skill sets needed by pharmacists to engage in protecting patient safety, these 3 performance outcomes – using SBAR regularly to communicate to other providers, participating effectively in RCA teams, and participating effectively in FMEA teams –are so widely taught and adopted by other health professions that they are essential to PharmD graduates’ ability to be members of interdisciplinary teams when they enter practice. Thus, these performance outcomes deserve special attention from curriculum developers in PharmD programs.
Appendix 1. Example of a rubric used to assess a 15-point SBAR assignment. A mark is placed in each column for the rows labeled S, B, A, R to indicate that the student met 3, 2, 1, or none of the criteria. A row score is placed in the far right column for each of the elements assessed. The overall quality score is similarly rated based on the student meeting 3, 2, 1 or none of the criteria listed, a check mark is placed in the appropriate column of the overall quality score row, and the score is entered in the right most column. The 5 row scores are added to determine the student's total score.
REFERENCES
- 1.Commission to Implement Change in Pharmaceutical Education. Arlington, VA: American Association of Colleges of Pharmacy; 1995. Background Paper V: Maintaining our Commitment to Change. [Google Scholar]
- 2.Yanchick VA. Greater implementation of competency guidelines in the pharmacy curriculum needed. Am J Pharm Educ. 2005;59(2):Article 37. [Google Scholar]
- 3.Greiner AC, Knebel E, editors. Health Professions Education: A Bridge to Quality. Washington, DC: Institute of Medicine; 2003. [PubMed] [Google Scholar]
- 4.Accreditation Council for Graduate Medical Education. Common program requirements: general competencies. 2007. http://www.acgme.org/outcome/comp/GeneralCompetenciesStandards21307.pdf. Accessed August 27, 2011.
- 5.Varkey P, Karlapudi S, Rose S, Swensen S. A patient safety curriculum for graduate medical education: results from a needs assessment of educators and patient safety experts. Am J Med Qual. 2009;24(3):214–221. doi: 10.1177/1062860609332905. [DOI] [PubMed] [Google Scholar]
- 6.Singh R, Naughton B, Taylor JS, et al. A comprehensive collaborative patient safety residency curriculum to address the ACGME core competencies. Med Educ. 2005;39(12):1195–1204. doi: 10.1111/j.1365-2929.2005.02333.x. [DOI] [PubMed] [Google Scholar]
- 7.American Society of Health-Systems Pharmacists and American Pharmacists Association. Required and Elective Educational Outcomes, Goals, Objectives and Instructional Objectives for Postgraduate Year One (PGY1) Community Pharmacy Residency Programs. http://www.ashp.org/DocLibrary/Accreditation/RTPCommunityCareGoalsObj2010.aspx. Accessed August 27, 2011.
- 8.Kohn LT, Corrigan JM, Donaldson MS, editors. To Err is Human: Building a Safer Health System. Washington, DC: National Academy Press; 2000. pp. 173–174. [PubMed] [Google Scholar]
- 9.Burkhardt M, Lee C, Taylor L, Williams R, Bagian J. Root cause analysis of medication errors. In: Cohen MR, editor. Medication Errors. 2nd ed. Washington, DC: American Pharmacists Association; 2007. p. 67. [Google Scholar]
- 10.Dew JR. In search of the root cause. Qual Progress. 1991;24(3):97–102. [Google Scholar]
- 11.Bagian JP, Gosbee J, Lee CZ, Williams L, McKnight SD, Mannos DM. The Veterans Affairs root cause analysis system in action. Jt Comm J Qual Improv. 1998;28(10):531–545. doi: 10.1016/s1070-3241(02)28057-8. [DOI] [PubMed] [Google Scholar]
- 12.McKee J, editor. Joint Commission Resources: Root Cause Analysis in Health Care. 3rd ed. Oakbrook Terrace, IL: Joint Commission Resources; 2005. p. 2. [Google Scholar]
- 13.Jackson TL. Ensuring quality in pharmacy operations. In: Deselle SP, Zgarrick DP, editors. Pharmacy Management: Essentials for All Practice Settings. New York: McGraw-Hill; 2005. pp. 132–133. [Google Scholar]
- 14.Institute for Safe Medication Practices. Key Plans for 2011. http://www.ismp.org/about/support.asp. Accessed August 27, 2011.
- 15.Knudsen P, Herborg H, Mortensen AR, Knudsen M, Hellebek A. Preventing medication errors in community pharmacy: root-cause analysis of transcription errors. Qual Saf Health Care. 2007;16(4):285–290. doi: 10.1136/qshc.2006.022053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.NHS Choices. A-Z of NHS authorities and trusts; Primary care trusts. http://www.nhs.uk/NHSEngland/thenhs/about/Pages/authoritiesandtrusts.aspx#primary. Accessed August 27, 2011.
- 17.Pharmacy Services Negotiating Committee (United Kingdom) Essential Service: Clinical Governance. http://www.psnc.org.uk/pages/essential_service_clinical_governance.html. Accessed August 27, 2011.
- 18.Anon . Southend-on-Sea, Essex, United Kingdom: National Health Service, South East Essex Primary Care Trust; 2010. A clinical governance resource pack for community pharmacists. http://www.see-pct.nhs.uk/content/file/Clinical%20Governance%20resource%20pack%20for%20community%20pharmacists.pdf. Accessed August 27, 2011. [Google Scholar]
- 19.California State Board of Pharmacy. California Practice Standards and Jurisprudence Examination for Pharmacists: Candidate Information Bulletin. March 21, 2011. http://www.pharmacy.ca.gov/publications/phy_handbook_psi.pdf. Accessed August 27, 2011.
- 20.Massachusetts Board of Registration in Pharmacy. Report on analysis of quality related events (medication errors) 2005. http://www.mass.gov/Eeohhs2/docs/dph/quality/boards/report_med_errors.doc. Accessed August 27, 2011.
- 21.Apollo Associated Services, LLC. Apollo Root Cause Analysis Program Institutionalization. 2008. pp. 4–5. http://www.apollorca.com/_public/site/files/2008_Program_Institutionalization.pdf. Accessed August 27, 2011.
- 22.McKee J, editor. Joint Commission Resources: Root Cause Analysis in Health Care. 3rd ed. Oakbrook Terrace, IL: Joint Commission Resources; 2005. p. 105. [Google Scholar]
- 23.DeRosier J, Stalhandske E, Bagian JP, Nudell T. Using health care failure mode and effect analysis: the VA National Center for Patient Safety's prospective risk analysis system. Jt Comm Qual Improv. 2002;28(5):248–267. doi: 10.1016/s1070-3241(02)28025-6. [DOI] [PubMed] [Google Scholar]
- 24.Institute for Healthcare Improvement. Failure Mode and Effects Analysis (FMEA) Tool. http://www.ihi.org/knowledge/Pages/Tools/FailureModesandEffectsAnalysisTool.aspx. Accessed September 7, 2011.
- 25.Cohen MR, Smetzer JL, Tuohy NR, Kilo CM. High-alert medications: safeguarding against errors. In: Cohen MR, editor. Medication Errors. 2nd ed. Washington, DC: American Pharmacists Association; 2007. pp. 317–328. [Google Scholar]
- 26.Haig KM, Sutton S, Whittington J. SBAR: a shared mental model for improving communication between clinicians. Jt Comm J Qual Pat Safety. 2006;32(3):167–175. doi: 10.1016/s1553-7250(06)32022-3. [DOI] [PubMed] [Google Scholar]
- 27.Pope BB, Rodzen L, Spross G. Raising the SBAR: how better communication improves patient outcomes. Nursing. 2008;38(3):41–43. doi: 10.1097/01.NURSE.0000312625.74434.e8. [DOI] [PubMed] [Google Scholar]
- 28.University Hospitals of Coventry and Warwickshire. SBAR – Community Pharmacy Escalation. http://www.mededcoventry.com/Guidelines/SBAR/Video/Escalation/CommunityPharmacy.aspx. Accessed August 27, 2011.
- 29.Brownlee SP, Bruce SP. Development of Pharmacy Skills Assessments (PSA) to evaluate clinical and communication skills of pharmacy students [abstract]. 111th annual meeting of the American Association of Colleges of Pharmacy, Seattle, Washington, July 10-14, 2010. Am J Pharm Educ. 2010;74(5):Article 96. [Google Scholar]
- 30.Institute for Healthcare Improvement. Improvement stories. http://www.ihi.org/knowledge/Pages/ImprovementStories/default.aspx. Accessed September 7, 2011.