Abstract
Few data are available on the predictors of decline in antihypertensive medication adherence and the association of decline in adherence with subsequent blood pressure (BP) control. The current analysis included 1,965 adults from the Cohort Study of Medication Adherence among Older Adults (CoSMO) recruited between August 2006 and September 2007. Decline in antihypertensive medication adherence was defined as a ≥ 2 point decrease on the 8-item Morisky Medication Adherence Scale assessed during telephone surveys 1 and 2 years following baseline. Risk factors for decline in adherence were collected using telephone surveys and administrative databases. BP was abstracted from outpatient records. The annual rate for a decline in adherence was 4.3% (159 participants experienced a decline). After multivariable adjustment, a decline in adherence was associated with an odds ratio (OR) for uncontrolled BP (≥140/90 mm Hg) at follow up of 1.68 (95% CI: 1.01, 2.80). Depressive symptoms (OR 1.84, 95%CI 1.20, 2.82) and a high stressful life events score (OR 1.68, 95% CI 1.19, 2.38) were associated with higher ORs for a decline in adherence. Female gender (OR 0.61, 95% CI 0.42, 0.88); being married (OR 0.68, 95% CI 0.47, 0.98); and calcium channel blocker use (OR 0.68, 95% CI 0.48, 0.97) were associated with lower ORs for decline. In summary, a decline in antihypertensive medication adherence was associated with uncontrolled BP. Modifiable factors associated with decline were identified. Further research is warranted to determine if interventions can prevent the decline in antihypertensive medication adherence and improve BP control.
Keywords: hypertension, medication adherence, blood pressure control, older women and men, cohort, risk factors
Introduction
Although there has been progress in the prevention, detection, awareness and treatment of hypertension, it persists as a major public health challenge affecting approximately 65 million people in the US and over a billion people worldwide (1-3). Effective medical therapies exist; yet, only 69% of US adults treated for hypertension have controlled blood pressure (2). Low adherence to prescribed medications has been implicated as one of the major contributors to uncontrolled blood pressure (4-6).
Hypertension requires continuous adherence (i.e. persistence) to pharmacologic treatment over time to achieve and maintain blood pressure control and reduce the risk for cardiovascular disease and related deaths (7-9). In a Canadian cohort, persistence with antihypertensive medications, assessed using prescription data for patients with established hypertension was only 82% at 4.5 years (10); blood pressure data and risk factors for non-persistence beyond age and gender were not reported. A decline in antihypertensive medication adherence over time could negatively impact hypertension control; thus, data on the association between decline in adherence, blood pressure control and potential risk factors are needed.
A conceptual model outlining risk factors associated with poor adherence and uncontrolled hypertension has been previously described (11). A decline in adherence reflects a change in behavior over time, and risk factors predicting decline may differ from those that are associated with poor adherence at one point in time. However, few data are available regarding the decline in adherence over time and its associated risk factors.
We assessed the rate of decline in self-reported antihypertensive medication adherence over 2 years of follow-up and its association with blood pressure control and risk factors in older adults with established hypertension. We hypothesized that a decline in self-reported antihypertensive medication adherence would be associated with worsening of blood pressure and sought to identify factors associated with a decline in adherence. To address these hypotheses, we analyzed data from community-dwelling participants 65 years of age and older enrolled in the Cohort Study of Medication Adherence among Older Adults (CoSMO) (6).
Methods
Study Population and Timeline
The CoSMO study design, recruitment flowchart, response rates and baseline characteristics of participants have been previously described (6). In brief, adults 65 years and older under treatment for essential hypertension were randomly selected from the roster of a large managed care organization in southeastern Louisiana. Between August 2006 and September 2007, 2194 individuals were recruited and completed a baseline survey. Participants were resurveyed one and two years later. The recapture rate was 93.6% for the follow-up surveys.
The present analysis includes data from the baseline and two follow-up surveys and was limited to 1965 participants who completed the baseline and first follow-up survey. There were 1756 CoSMO participants who did not experience a decline in medication adherence by the first follow up and were considered at risk for the second time period. There were no differences by age, gender, race, marital status, education, comorbidity or hypertension duration between CoSMO participants excluded from the analyses (primarily for non-response to the first follow up survey) and participants included in this analysis (P> 0.10 for all comparisons). All participants provided verbal informed consent (6;12), and CoSMO was approved by the Ochsner Clinic Foundation's Institutional Review Board and the privacy board of the managed care organization.
Study Measures
Based on a conceptual model (11), items (e.g. socio-demographic, psychosocial, treatment, clinical, healthcare system, and unconventional therapies) were included in the baseline and the follow-up surveys which were administered by telephone using trained interviewers and lasted 30 to 45 minutes. In addition, information regarding co-morbid conditions and pharmacy fills (include drug name, date filled, drug class, drug tier) for antihypertensive medications was obtained from the administrative databases of the managed care organization.
Socio-demographic, Clinical and Treatment Factors
Age, gender, race, marital status, education, height and weight (for calculation of body mass index), and duration of hypertension were obtained through self-report. Hypertension knowledge was assessed using a validated tool; participants with scores in the lowest tertile were defined as having low knowledge (13;14). Comorbid conditions were identified; the Charlson comorbidity index score was calculated and dichotomized as <2 versus ≥2 (15). The number and classes of antihypertensive medications filled in the year prior to the baseline survey were categorized as <3 versus ≥ 3. Each component of combination medications was classified in its respective class. The use of antihypertensive medication was defined as having at least 90 days of medication within the medication class in the prior year.
Healthcare System Variables
Participants “not satisfied” with healthcare were defined as having a poor or fair satisfaction score using three scales of the Group Health Association of America Consumer Satisfaction Survey (16). Participants were asked whether they had reduced antihypertensive medication because of the cost. Number of visits to a primary healthcare provider in the year prior to each survey was captured by self-report and dichotomized as <6 versus ≥6. As a surrogate for medication costs, fill of an antihypertensive medication in drug tier three (reflecting higher medication costs) versus fills in drug tier one or two (reflecting lower medication costs) only was captured in the pharmacy database
Psychosocial/Behavioral variables
Cigarette smoking (17) and alcohol use were assessed via self report. Reduced sexual functioning was defined as values below the median for the sample on the Massachusetts General Hospital Sexual Functioning Questionnaire (18). The presence of depressive symptoms was defined as a score of 16 or greater using the Center for Epidemiologic Studies Depression Scale (19). Low social support was defined as scores in the lowest tertile using the RAND Medical Outcomes Study Social Support Survey (20). Low coping was defined as scores below the median using an adapted John Henry Active Coping scale (21). High perceived stress levels were defined as having a score in the highest tertile for the sample using the Perceived Stress Scale (22). High stressful life events were defined as scores of 150 or greater using the Holmes Rahe Social Readjustment Rating Scale (23). Low mental and physical health-related quality of life were defined as scores in lowest tertile in the study sample using the RAND Medical Outcomes Study 36-item tool (24;25).
Self-management Behaviors
Home blood pressure checks and use of lifestyle modifications (weight control; salt reduction, fruit and vegetable consumption) to lower blood pressure were ascertained by self-report (26). Assessment of complementary and alternative therapies (including general use, health food and herbal supplements, and relaxation techniques) to help control blood pressure was adapted from a published survey tool (27;28).
Blood pressure
Using standardized forms, trained research staff abstracted seated systolic and diastolic blood pressure measurements from medical records for clinic visits occurring the year prior to the baseline and each follow-up interview. Blood pressure levels were averaged for visits with more than one measurement taken. Then, the average blood pressure level for the year prior to the baseline survey and for each follow-up was calculated. Blood pressure data were available for 1,845 CoSMO participants.
Medication Adherence
Antihypertensive medication adherence was ascertained using the self-report eight-item Morisky Medication Adherence Scale (MMAS-8). Scores on the MMAS-8 range from zero to eight. This measure was designed to facilitate the identification of barriers to and behaviors associated with adherence to chronic medications and has been determined to be significantly associated with blood pressure control (p<0.05) in cross-sectional studies (29). Also, it has been shown to be associated with antihypertensive medication pharmacy fill rates (6;30).
Recently published work established a within-person change in MMAS-8 score of two or more points over time to represent a true change in adherence (31). Thus, decline in adherence was defined as a decrease in MMAS-8 score of two or more points in the current study.
Statistical Analyses
Participant baseline characteristics were calculated. Decline in adherence was calculated between the baseline and first follow-up and between the first and second follow-up survey administrations (31). Pooled logistic regression models were used to compute the adjusted odds ratios for an increase in blood pressure associated with a decline in adherence. For individuals with controlled blood pressure at baseline (systolic and diastolic BP < 140/90 mm Hg), the odds ratio for uncontrolled blood pressure (systolic or diastolic BP ≥ 140 or 90 mm Hg) associated with a decline in adherence was calculated. Because there are no previously validated cut points to define a clinically meaningfully increase in blood pressure, we analyzed two different increases in blood pressure: > 0.5 and > 1 standard deviations in systolic and diastolic blood pressure (1 standard deviation of change in systolic blood pressure = 12.3 mm Hg, 1 standard deviation of change in diastolic blood pressure = 6.8 mm Hg). Based on clinical judgment and known confounders, adjustment included age, gender, race, education, marital status, history of diabetes mellitus and cardiovascular disease (myocardial infarction, heart failure, cerebrovascular accident, peripheral vascular disease), number of medications, number of primary care physician visits, hypertension duration, and reduction of antihypertensive medication due to cost.
Pooled logistic regression models, adjusted for age, gender, race, marital status, education and comorbidity, were also used to determine associations between risk factors outlined in the previously published conceptual model (11) and described in the Methods section above and a decline in adherence. Then, a multivariable-adjusted pooled logistic regression model including all variables that were significant at the p<0.05 level and potential confounders (i.e. age, race, education, hypertension duration and comorbidity) was assembled to identify the factors associated with decline in adherence. Perceived stress was not considered for this final model because it was co-linear with both the stressful life events and depressive symptoms scores. All analyses were performed using SAS version 9.2 (SAS Institute, Cary, NC).
Results
At the baseline assessment, the mean age was 75.0 ± 5.6 years, 30.2% were black, 59.0% were women, 56.8% were married, 62.7% had hypertension duration ≥10 years, and 44.3% filled three or more classes of antihypertensive medications in the prior year (Table 1). At baseline 14.3% of participants had low adherence while, 34.0% and 51.7% had median and high adherence, respectively. Overall, 66.6% had controlled BP.
Table 1. Baseline Characteristics of the Study Population (n=1,965).
| Participant Characteristics | N (%) |
|---|---|
| Socio-Demographics and Patient Characteristics | |
| Age ≥ 75 years | 952 (48.5%) |
| Female | 1,160 (59.0%) |
| Black race | 594 (30.2%) |
| Married | 1,116 (56.8%) |
| High school education or greater | 1,566 (79.7%) |
| Low hypertension knowledge | 616 (31.4%) |
| Clinical / Treatment Variables | |
| Hypertension duration ≥ 10 Years | 1,228 (62.7%) |
| Charlson Comorbidity Index score ≥ 2* | 967 (49.2%) |
| Body mass index: ≥ 30 kg/m2 | 747 (38.1%) |
| 3+ classes of antihypertensive medication* | 854 (44.3%) |
| Calcium channel blocker use* | 855 (44.3%) |
| Beta blocker use* | 905 (46.9%) |
| Angiotension receptor blocker use* | 452 (23.4%) |
| Diuretic use* | 1,177 (61.0%) |
| Ace inhibitor use* | 998 (51.7%) |
| Health Care System Variables | |
| Not satisfied with overall health care | 87 (4.4%) |
| Not satisfied with communication | 201 (10.3%) |
| Not satisfied with access to healthcare | 80 (4.1%) |
| Reduced antihypertensive medications due to cost | 68 (3.5%) |
| 6+ visits to primary care physician* | 436 (22.3%) |
| Filled antihypertensive medications in drug tier 3* | 422 (21.9%) |
| Psychosocial / Behavioral Factors | |
| Never a smoker | 964 (49.4%) |
| < 2 alcoholic beverages per week | 1,541 (78.7%) |
| Reduced sexual functioning | 1,166 (59.3%) |
| Depressive symptoms present | 244 (12.4%) |
| Low health-related quality of life (mental) | 637 (32.5%) |
| Low health-related quality of life (physical) | 629 (32.1%) |
| Low Social Support | 649 (33.0%) |
| Low Coping | 934 (47.6%) |
| High Stress | 659 (33.5%) |
| High Stressful Life Event Score | 585 (32.2%) |
| Self-Management Behaviors | |
| Complementary and alternative medicine use | 521 (26.5%) |
| Blood pressure checks at home | 997 (50.7%) |
| Trying to control or lose weight | 1,254 (63.8%) |
| Cutting down on sodium intake | 1,581 (80.5%) |
| Increasing number of fruits and vegetables | 1,347 (68.6%) |
in the prior year
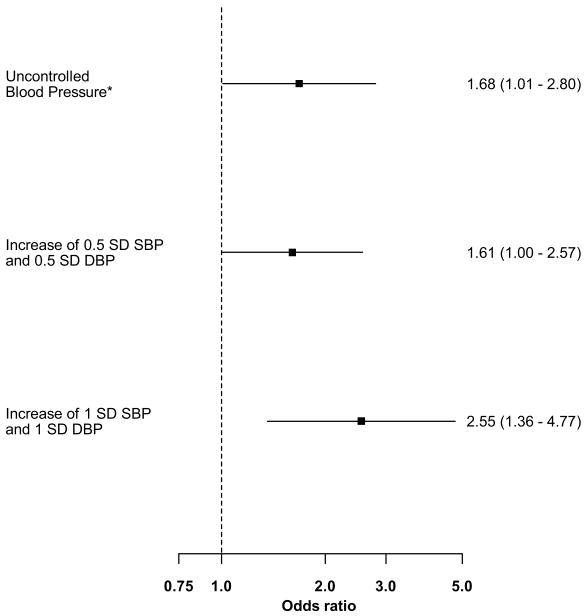
Over the 2 years of follow up, 159 participants experienced a decline in antihypertensive medication adherence. The annual rate for a decline in adherence was 4.3%. Of 1229 participants who had controlled blood pressure at baseline, 17.0% had uncontrolled blood pressure at follow up. After multivariable adjustment, a decline in adherence was associated with an odds ratio for uncontrolled blood pressure of 1.68 (95% confidence interval (CI) 1.01, 2.80; Figure 1). Increases greater than 0.5 standard deviation and 1 standard deviation in systolic and diastolic blood pressures were identified in 12.3% and 4.2% participants, respectively. After multivariable adjustment, decline in adherence was associated with odds ratios for 0.5 and 1 standard deviation increases in systolic and diastolic blood pressure of 1.61 (95% CI 1.00, 2.57) and 2.55 (95% CI 1.36, 4.77), respectively.
Figure 1. Decline in Medication Adherence associated with Increased Blood Pressure at Follow up.
*Uncontrolled blood pressure was defined as ≥ 140/90 at follow-up among those with controlled BP at baseline
Odds Ratios adjusted for age, gender, race, education, marital status, history of diabetes or cardiovascular disease (myocardial infarction, heart failure, cerebrovascular accident, peripheral vascular disease), number of medications, number of primary care physician visits, hypertension duration, and reduction of antihypertensive medication due to cost.
SBP-systolic blood pressure; DBP-diastolic blood pressure
SD-standard deviation
Note: 1 standard deviation of change in systolic blood pressure = 12.3 mm Hg; 1 standard deviation of change in diastolic blood pressure = 6.8 mm Hg
The annual rate of decline in antihypertensive medication adherence is reported by participant characteristics in Supplemental Table 1 (please see http://hyper.ahajournals.org). Being female, married and taking calcium channel blockers were associated with a lower adjusted odds ratio for a decline in adherence (Table 2). Depressive symptoms, low health-related quality of life–physical, high perceived stress, and having a high stressful life event score were associated with an increased adjusted odds ratio for a decline in adherence. In the final multivariable-adjusted model, depressive symptoms and a high stressful life events score were associated with a decline in adherence whereas female gender, being married, and taking calcium channel blockers remained protective of a decline in adherence (Table 3).
Table 2. Association between participant characteristics and decline in self-reported antihypertensive medication adherence.
| Participant Characteristics | Odds Ratio (95% CI) * for MMAS-8 decline |
|---|---|
| Socio-Demographics and Patient Characteristics | |
| Age ≥ 75 years | 1.28 (0.87, 1.89) |
| Female | 0.67 (0.48, 0.95)† |
| Black race | 1.00 (0.69, 1.45) |
| Married | 0.67 (0.48, 0.95)† |
| High school education or greater | 1.15 (0.75, 1.76) |
| Low hypertension knowledge | 1.20 (0.85, 1.69) |
| Clinical / Treatment Variables | |
| Hypertension duration ≥ 10 Years | 1.08 (0.78, 1.51) |
| Charlson Comorbidity Index score ≥ 2§ | 1.07 (0.77, 1.48) |
| Body mass index: ≥ 30 kg/m2 | 0.95 (0.65, 1.39) |
| 3+ classes of antihypertensive medication§ | 0.85 (0.61, 1.19) |
| Calcium channel blocker use§ | 0.69 (0.49, 0.98)† |
| Beta blocker use§ | 1.02 (0.73, 1.42) |
| Angiotension receptor blocker use§ | 1.07 (0.73, 1.58) |
| Diuretic use§ | 0.89 (0.64, 1.25) |
| Ace inhibitor use§ | 1.05 (0.76, 1.46) |
| Health Care System Variables | |
| Not satisfied with overall health care | 1.20 (0.58, 2.49) |
| Not satisfied with communication | 1.48 (0.91, 2.41) |
| Not satisfied with access to healthcare | 1.10 (0.51, 2.40) |
| Reduced antihypertensive medications due to cost | 1.47 (0.63, 3.45) |
| 6+ visits to primary care physician§ | 0.85 (0.58, 1.25) |
| Filled antihypertensive medications in drug tier 3 § | 0.90 (0.59, 1.38) |
| Psychosocial / Behavioral Variables | |
| Never a smoker | 0.82 (0.58, 1.15) |
| < 2 alcoholic beverages per week | 0.95 (0.64, 1.42) |
| Reduced sexual functioning | 1.19 (0.85, 1.67) |
| Depressive symptoms | 1.90 (1.27, 2.85)‡ |
| Low health-related quality of life (mental) | 1.27 (0.91, 1.79) |
| Low health-related quality of life (physical) | 1.53 (1.10, 2.14)† |
| Low Social Support | 1.35 (0.98, 1.88) |
| Low Coping | 0.93 (0.68, 1.28) |
| High Stress | 1.70 (1.21, 2.38)‡ |
| High Stressful Life Event Score | 1.98 (1.41, 2.77)‡ |
| Self-Management Behaviors | |
| Complementary and alternative medicine use | 1.02 (0.70, 1.48) |
| Blood pressure checks at home | 0.94 (0.68, 1.30) |
| Trying to control or lose weight | 1.03 (0.74, 1.43) |
| Cutting down on sodium intake | 0.86 (0.59, 1.26) |
| Increasing number of fruits and vegetables | 0.98 (0.69, 1.39) |
MMAS-8 decline -Morisky Medication Adherence Scale-8 item score decline of 2 or more points
OR-odds ratio; CI-confidence interval
Adjusted for age, gender, race, marital status, education, and comorbidity
p<0.05
p<0.01
in the prior year
Reference groups: age <75 years, male, non-black race, unmarried, < high school education, medium or high hypertension knowledge, hypertension duration <10 years, Charlson comorbidity score <2, Body Mass Index <30, < 3 classes of antihypertensive medication, no calcium channel blocker use, no beta-blocker use, no angiotensin receptor blocker use, no diuretic use, no ace-inhibitor use, satisfied with overall health care, satisfied with communication, satisfied with access to health care, no reduction of medications due to cost, <6 visits to the primary care physician, did not purchase antihypertensive medication in tier 3, ever smoker, ≥2 alcoholic beverages per week, normal sexual functioning, no depressive symptoms, medium or high health-related quality of life (mental), medium or high health-related quality of life (physical), medium or high social support, medium or high coping, medium or low stress, stressful life events score <150, no complementary and alternative medicine use, no report of each lifestyle modification (ie blood pressure checks at home, trying to control or lose weight, cutting down on sodium intake, increasing number of fruits and vegetables)
Table 3. Multivariable adjusted odds ratios for a decline in self-reported antihypertensive medication adherence.
| Baseline Characteristics | Odds Ratio (95% CI) * for MMAS-8 decline |
|---|---|
| Age 75 years or older | 1.24 (0.88, 1.75) |
| Female | 0.61 (0.42, 0.88)‡ |
| Black race | 1.00 (0.66, 1.50) |
| Married | 0.68 (0.47, 0.98)† |
| High school education or more | 1.26 (0.80, 1.98) |
| Charlson comorbidity Index score ≥ 2§ | 0.96 (0.67, 1.36) |
| Hypertension duration ≥ 10 | 1.04 (0.73, 1.47) |
| Calcium channel blocker use§ | 0.68 (0.48, 0.97)† |
| Depressive symptoms | 1.84 (1.20, 2.82)† |
| Low health-related quality of life (physical) | 1.40 (0.98, 2.00) |
| High stressful life event score | 1.68 (1.19, 2.38)‡ |
MMAS-8 decline -Morisky Medication Adherence Scale-8 item score decline of 2 or more points
OR-odds ratio; CI-confidence interval
Adjusted for all other variables shown
p<0.05
p<0.01
in the prior year
Discussion
In this large cohort of patients with hypertension, only 51.7% had high adherence and 66.6% had controlled blood pressure at baseline. The annual rate of decline in adherence was 4.3%, and a decline in adherence was associated with a 1.68 fold increase in uncontrolled blood pressure at follow-up. Two modifiable factors (depressive symptoms and use of specific antihypertensive medication classes) associated with decline in adherence were identified. Other non-modifiable factors (e.g., gender, marital status) which may still be helpful in identifying patients at risk for decline in antihypertensive medication adherence and worsening blood pressure were also identified. Despite the growing interest in patient adherence to antihypertensive medications, few data are available on changes in adherence over time. The current study extends prior work by providing new data on decline in self-reported antihypertensive medication adherence, blood pressure control and risk factors for decline.
Prior studies using pharmacy data have revealed that persistence to pharmacologic antihypertensive therapy declines over time. In one study, 3% of patients with established hypertension became non-persistent (determined using prescription data) to their antihypertensive medication regimen at one year and 18% at 4.5 years; (10). In our analysis of adults with established hypertension, a 4.3% annual rate of decline in self-reported antihypertensive medication was present. The current study goes beyond previous research using prescription data and identified an association of decline in self-reported adherence with uncontrolled blood pressure obtained from routine outpatient visit data. This finding may increase confidence that assessment of changes in antihypertensive medication adherence may be useful in managing patients in real world clinical practice.
The current longitudinal analysis is consistent with cross-sectional studies reporting being female and married are associated with better adherence rates (10;32). Our results extend prior cross-sectional data by revealing a significant protective effect of being female and married on decline in adherence.
Depression is common in patients with hypertension. Depressive symptoms are associated with poor blood pressure control, complications of hypertension (33) and low antihypertensive medication adherence (34-36). Less is known about the relationship between depressive symptoms and changes in antihypertensive medication adherence over time. In our study, the presence of depressive symptoms was the strongest risk factor for a decline in antihypertensive medication adherence over two years of follow up. Co-management of hypertension and depression has been suggested to improve adherence rates and health care outcomes for both conditions (37;38).
In the current analyses, more stressful life events were associated with a decline in adherence. Previous research suggests that patients experiencing stressful life events may have reduced motivation or ability to continue psychiatric medications (39). Increased stressful life events have also been associated with the onset or exacerbation of chronic disease (40-42). Although the stress from major life changes could result in exacerbation of disease directly, the disruption of medication-taking routines associated with major life events could mediate this relationship.
Although other studies have shown class-specific benefits on medication-taking behavior for drugs with once daily dosing and favorable tolerability (43-48), the protective effect of calcium channel blockers on decline in adherence observed in the present study can only be speculated. First, calcium channel blockers are recommended for patients with a compelling indication (i.e. high coronary disease risk or diabetes) or higher levels of blood pressure (49). Thus, patients taking these drugs may have more severe disease reinforcing the importance of medication adherence. Furthermore, significant improvements in depressive symptoms in patients randomized to verapamil versus atenolol suggest positive mood-related effects of this calcium channel blocker (50) which may impact adherence. Lastly, the reduced intra-individual variation in systolic blood pressure observed in patients taking calcium channel blockers (51) may result in more balanced blood pressure levels over time, patients feeling better and higher adherence. The current study findings support consideration of medication class effects on medication-taking behavior when treating older patients with established hypertension.
Limitations and Strengths
The medication adherence measure was based on self-report, which may have led to over-estimation of adherence due to social desirability and recall biases. However, prior work found no association between the MMAS-8 and social desirability (29). Of note, there is no gold standard for measuring medication adherence, and each method has limitations (32;52). Although pharmacy fill has been widely reported from managed care organizations, less than 30% of US adults receive care in settings where pharmacy fill data are readily available (53). Blood pressure was abstracted from medical records and not measured using a study protocol. The current study was limited to English-speaking adults 65 years of age and older with health insurance in one region of the US. However, almost all US citizens ≥ 65 years of age have health insurance and pharmacy benefits through Medicare (2;54).
Despite these limitations, the inclusion of a large sample of diverse community-dwelling older adults, longitudinal design, broad data collection, availability of administrative data, and high follow-up capture rate are strengths of this study. The restriction of our sample to older adults in a managed care setting minimizes the confounding effects of health insurance, access to medical care, and employment status in older adults.
Perspectives
Low adherence to medications is a growing concern because of increasing evidence that it is common and associated with adverse outcomes and higher healthcare costs (55). Furthermore, the use of performance measures that reward quality based on the attainment of blood pressure control reinforces the importance of continuous medication adherence (56)and prevention of decline in adherence. Nevertheless, routine assessment of medication adherence is not done (57). Providers may not think of a decline in adherence as the reason for uncontrolled blood pressure, are uncertain about quantifying adherence (30;58), or are unaware of modifiable factors associated with decline in adherence. Our study provides information about decline in self-reported adherence in older adults which may be used to identify patients at risk for worsening adherence and blood pressure control in clinical practice. Further research is warranted to determine if interventions to overcome barriers to adherence can prevent the decline in adherence over time.
Supplementary Material
Acknowledgments
Source of Support: The project described was supported by Grant Number R01 AG022536 from the National Institute on Aging (Dr. Krousel-Wood, principal investigator). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute on Aging or the National Institutes of Health.
Footnotes
Financial disclosure: None
Dr, Krousel-Wood had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Conflicts of Interest: None
Permission for use of MMAS-8 is required. Licensure agreement is available from Donald E. Morisky, ScD, UCLA School of Public Health, 650 Charles E. Young Drive South, Los Angeles, CA 90095-1772.
Reference List
- 1.Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, Jr, Jones DW, Materson BJ, Oparil S, Wright JT, Jr, Roccella EJ. Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension. 2003;42:1206–1252. doi: 10.1161/01.HYP.0000107251.49515.c2. [DOI] [PubMed] [Google Scholar]
- 2.Egan BM, Zhao Y, Axon RN. US trends in prevalence, awareness, treatment, and control of hypertension, 1988-2008. JAMA. 2010;303:2043–2050. doi: 10.1001/jama.2010.650. [DOI] [PubMed] [Google Scholar]
- 3.Ong KL, Cheung BM, Man YB, Lau CP, Lam KS. Prevelance, awareness, treatment and control of hypertension among United States adults 1999-2004. Hypertension. 2007;49:69–75. doi: 10.1161/01.HYP.0000252676.46043.18. [DOI] [PubMed] [Google Scholar]
- 4.DiMatteo MR, Giordani PJ, Lepper HS, Croghan TW. Patient adherence and medical treatment outcomes: a meta-analysis. Med Care. 2002;40:794–811. doi: 10.1097/00005650-200209000-00009. [DOI] [PubMed] [Google Scholar]
- 5.Kravitz RL, Melnikow J. Medical adherence research: time for a change in direction? Med Care. 2004;42:197–199. doi: 10.1097/01.mlr.0000115957.44388.7c. [DOI] [PubMed] [Google Scholar]
- 6.Krousel-Wood MA, Muntner P, Islam T, Morisky DE, Webber LS. Barriers to and determinants of medication adherence in hypertension management: perspective of the cohort study of medication adherence among older adults. Med Clin North Am. 2009;93:753–769. doi: 10.1016/j.mcna.2009.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Prevention of stroke by antihypertensive drug treatment in older persons with isolated systolic hypertension. Final results of the Systolic Hypertension in the Elderly Program (SHEP). SHEP Cooperative Research Group. JAMA. 1991;265:3255–3264. [PubMed] [Google Scholar]
- 8.Gueyffier F, Froment A, Gouton M. New meta-analysis of treatment trials of hypertension: improving the estimate of therapeutic benefit. J Hum Hypertens. 1996;10:1–8. [PubMed] [Google Scholar]
- 9.Neaton JD, Grimm RH, Jr, Prineas RJ, Stamler J, Grandits GA, Elmer PJ, Cutler JA, Flack JM, Schoenberger JA, McDonald R. Treatment of Mild Hypertension Study. Final results. Treatment of Mild Hypertension Study Research Group. JAMA. 1993;270:713–724. [PubMed] [Google Scholar]
- 10.Caro JJ, Salas M, Speckman JL, Raggio G, Jackson JD. Persistence with treatment for hypertension in actual practice. CMAJ. 1999;160:31–37. [PMC free article] [PubMed] [Google Scholar]
- 11.Krousel-Wood M, Thomas S, Muntner P, Morisky D. Medication adherence: a key factor in achieving blood pressure control and good clinical outcomes in hypertensive patients. Curr Opin Cardiol. 2004;19:357–362. doi: 10.1097/01.hco.0000126978.03828.9e. [DOI] [PubMed] [Google Scholar]
- 12.Krousel-Wood M, Muntner P, Jannu A, Hyre A, Breault J. Does waiver of written informed consent from the institutional review board affect response rate in a low-risk research study? J Investig Med. 2006;54:174–179. doi: 10.2310/6650.2006.05031. [DOI] [PubMed] [Google Scholar]
- 13.Sanne S, Muntner P, Kawasaki L, Hyre A, DeSalvo KB. Hypertension knowledge among patients from an urban clinic. Ethn Dis. 2008;18:42–47. [PubMed] [Google Scholar]
- 14.Williams MV, Baker DW, Parker RM, Nurss JR. Relationship of functional health literacy to patients' knowledge of their chronic disease. A study of patients with hypertension and diabetes. Arch Intern Med. 1998;158:166–172. doi: 10.1001/archinte.158.2.166. [DOI] [PubMed] [Google Scholar]
- 15.Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol. 1992;45:613–619. doi: 10.1016/0895-4356(92)90133-8. [DOI] [PubMed] [Google Scholar]
- 16.Meng YY, Jatulis DE, McDonald JP, Legorreta AP. Satisfaction with access to and quality of health care among Medicare enrollees in a health maintenance organization. West J Med. 1997;166:242–247. [PMC free article] [PubMed] [Google Scholar]
- 17.Centers for Disease Control and Prevention. Behavioral risk factor surveillance system survey questionnaire. Atlanta Georgia: US Department of Health and Human Services; 2010. [Google Scholar]
- 18.Labbate LA, Lare SB. Sexual dysfunction in male psychiatric outpatients: validity of the Massachusetts General Hospital Sexual Functioning Questionnaire. Psychother Psychosom. 2001;70:221–225. doi: 10.1159/000056257. [DOI] [PubMed] [Google Scholar]
- 19.Knight RG, Williams S, McGee R, Olaman S. Psychometric properties of the Centre for Epidemiologic Studies Depression Scale (CES-D) in a sample of women in middle life. Behav Res Ther. 1997;35:373–380. doi: 10.1016/s0005-7967(96)00107-6. [DOI] [PubMed] [Google Scholar]
- 20.Sherbourne CD, Stewart AL. The MOS social support survey. Soc Sci Med. 1991;32:705–714. doi: 10.1016/0277-9536(91)90150-b. [DOI] [PubMed] [Google Scholar]
- 21.Fernander AF, Duran RE, Saab PG, Llabre MM, Schneiderman N. Assessing the reliability and validity of the John Henry Active Coping Scale in an urban sample of African Americans and white Americans. Ethn Health. 2003;8:147–161. doi: 10.1080/13557850303563. [DOI] [PubMed] [Google Scholar]
- 22.Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24:385–396. [PubMed] [Google Scholar]
- 23.Holmes TH, Rahe RH. The Social Readjustment Rating Scale. J Psychosom Res. 1967;11:213–218. doi: 10.1016/0022-3999(67)90010-4. [DOI] [PubMed] [Google Scholar]
- 24.Hays RD, Sherbourne CD, Mazel RM. The RAND 36-item health survey 1.0. Health Econ. 1993;2:217–227. doi: 10.1002/hec.4730020305. [DOI] [PubMed] [Google Scholar]
- 25.Holt EW, Muntner P, Joyce CJ, Webber L, Krousel-Wood MA. Health-related quality of life and antihypertensive medication adherence among older adults. Age Ageing. 2010;39:481–487. doi: 10.1093/ageing/afq040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.National Health and Nutrition Examination Study. [Accessed 2-1-2011];2011 http://www.cdc.gov/nchs/data/nhanes/nhanes_03_04/sp_bpq_c.pdf.
- 27.Krousel-Wood MA, Muntner P, Joyce CJ, Islam T, Stanley E, Holt EW, Morisky DE, He J, Webber LS. Adverse effects of complementary and alternative medicine on antihypertensive medication adherence: findings from the cohort study of medication adherence among older adults. J Am Geriatr Soc. 2010;58:54–61. doi: 10.1111/j.1532-5415.2009.02639.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lengacher CA, Bennett MP, Kipp KE, Berarducci A, Cox CE. Design and testing of the use of a complementary and alternative therapies survey in women with breast cancer. Oncol Nurs Forum. 2003;30:811–821. doi: 10.1188/03.ONF.811-821. [DOI] [PubMed] [Google Scholar]
- 29.Morisky DE, Ang A, Krousel-Wood MA, Ward H. Predictive validity of a medication adherence measure in an outpatient setting. J Clin Hypertens. 2008;10:348–354. doi: 10.1111/j.1751-7176.2008.07572.x. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 30.Krousel-Wood M, Islam T, Webber LS, Re RN, Morisky DE, Muntner P. New medication adherence scale versus pharmacy fill rates in seniors with hypertension. Am J Manag Care. 2009;15:59–66. [PMC free article] [PubMed] [Google Scholar]
- 31.Muntner P, Joyce C, Holt E, He J, Morisky D, Webber LS, Krousel-Wood M. Defining the minimal detectable change in scores on the eight-item Morisky Medication Adherence Scale. Ann Pharmacother. 2011;45:569–575. doi: 10.1345/aph.1P677. [DOI] [PubMed] [Google Scholar]
- 32.Morris AB, Li J, Kroenke K, Bruner-England TE, Young JM, Murray MD. Factors associated with drug adherence and blood pressure control in patients with hypertension. Pharmacotherapy. 2006;26:483–492. doi: 10.1592/phco.26.4.483. [DOI] [PubMed] [Google Scholar]
- 33.Scalco MZ, de Almeida OP, Hachul DT, Castel S, Serro-Azul J, Wajngarten M. Comparison of risk of orthostatic hypotension in elderly depressed hypertensive women treated with nortriptyline and thiazides versus elderly depressed normotensive women treated with nortriptyline. Am J Cardiol. 2000;85:1156–8. A9. doi: 10.1016/s0002-9149(00)00717-7. [DOI] [PubMed] [Google Scholar]
- 34.DiMatteo MR, Lepper HS, Croghan TW. Depression is a risk factor for noncompliance with medical treatment: meta-analysis of the effects of anxiety and depression on patient adherence. Arch Intern Med. 2000;160:2101–2107. doi: 10.1001/archinte.160.14.2101. [DOI] [PubMed] [Google Scholar]
- 35.Kim MT, Han HR, Hill MN, Rose L, Roary M. Depression, substance use, adherence behaviors, and blood pressure in urban hypertensive black men. Ann Behav Med. 2003;26:24–31. doi: 10.1207/S15324796ABM2601_04. [DOI] [PubMed] [Google Scholar]
- 36.Krousel-Wood M, Islam T, Muntner P, Holt E, Joyce C, Morisky DE, Webber LS, Frohlich ED. Association of depression with antihypertensive medication adherence in older adults: cross-sectional and longitudinal findings from CoSMO. Ann Behav Med. 2010;40:248–257. doi: 10.1007/s12160-010-9217-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bogner HR, de Vries HF. Integration of depression and hypertension treatment: a pilot, randomized controlled trial. Ann Fam Med. 2008;6:295–301. doi: 10.1370/afm.843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Lichtman JH, Bigger JT, Jr, Blumenthal JA, Frasure-Smith N, Kaufmann PG, Lesperance F, Mark DB, Sheps DS, Taylor CB, Froelicher ES. Depression and coronary heart disease: recommendations for screening, referral, and treatment: a science advisory from the American Heart Association Prevention Committee of the Council on Cardiovascular Nursing, Council on Clinical Cardiology, Council on Epidemiology and Prevention, and Interdisciplinary Council on Quality of Care and Outcomes Research: endorsed by the American Psychiatric Association. Circulation. 2008;118:1768–1775. doi: 10.1161/CIRCULATIONAHA.108.190769. [DOI] [PubMed] [Google Scholar]
- 39.Magura S, Laudet AB, Mahmood D, Rosenblum A, Knight E. Adherence to medication regimens and participation in dual-focus self-help groups. Psychiatr Serv. 2002;53:310–316. doi: 10.1176/appi.ps.53.3.310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Magni G, Corfini A, Berto F, Rizzardo R, Bombardelli S, Miraglia G. Life events and myocardial infarction. Aust N Z J Med. 1983;13:257–260. doi: 10.1111/j.1445-5994.1983.tb04653.x. [DOI] [PubMed] [Google Scholar]
- 41.Rafanelli C, Roncuzzi R, Milaneschi Y, Tomba E, Colistro MC, Pancaldi LG, Di PG. Stressful life events, depression and demoralization as risk factors for acute coronary heart disease. Psychother Psychosom. 2005;74:179–184. doi: 10.1159/000084003. [DOI] [PubMed] [Google Scholar]
- 42.Tosevski DL, Milovancevic MP. Stressful life events and physical health. Curr Opin Psychiatry. 2006;19:184–189. doi: 10.1097/01.yco.0000214346.44625.57. [DOI] [PubMed] [Google Scholar]
- 43.Bloom BS. Continuation of initial antihypertensive medication after 1 year of therapy. Clin Ther. 1998;20:671–681. doi: 10.1016/s0149-2918(98)80130-6. [DOI] [PubMed] [Google Scholar]
- 44.Bourgault C, Senecal M, Brisson M, Marentette MA, Gregoire JP. Persistence and discontinuation patterns of antihypertensive therapy among newly treated patients: a population-based study. J Hum Hypertens. 2005;19:607–613. doi: 10.1038/sj.jhh.1001873. [DOI] [PubMed] [Google Scholar]
- 45.Conlin PR, Gerth WC, Fox J, Roehm JB, Boccuzzi SJ. Four-Year persistence patterns among patients initiating therapy with the angiotensin II receptor antagonist losartan versus other artihypertensive drug classes. Clin Ther. 2001;23:1999–2010. doi: 10.1016/s0149-2918(01)80152-1. [DOI] [PubMed] [Google Scholar]
- 46.Marentette MA, Gerth WC, Billings DK, Zarnke KB. Antihypertensive persistence and drug class. Can J Cardiol. 2002;18:649–656. [PubMed] [Google Scholar]
- 47.Wogen J, Kreilick CA, Livornese RC, Yokoyama K, Frech F. Patient adherence with amlodipine, lisinopril, or valsartan therapy in a usual-care setting. J Manag Care Pharm. 2003;9:424–429. doi: 10.18553/jmcp.2003.9.5.424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kronish IM, Woodward M, Sergie Z, Ogedegbe G, Falzon L, Mann DM. Meta-analysis: impact of drug class on adherence to antihypertensives. Circulation. 2011;123:1611–1621. doi: 10.1161/CIRCULATIONAHA.110.983874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, Jr, Jones DW, Materson BJ, Oparil S, Wright JT, Jr, Roccella EJ. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA. 2003;289:2560–2572. doi: 10.1001/jama.289.19.2560. [DOI] [PubMed] [Google Scholar]
- 50.Ried LD, Tueth MJ, Handberg E, Kupfer S, Pepine CJ. A Study of Antihypertensive Drugs and Depressive Symptoms (SADD-Sx) in patients treated with a calcium antagonist versus an atenolol hypertension Treatment Strategy in the International Verapamil SR-Trandolapril Study (INVEST) Psychosom Med. 2005;67:398–406. doi: 10.1097/01.psy.0000160468.69451.7f. [DOI] [PubMed] [Google Scholar]
- 51.Webb AJ, Fischer U, Mehta Z, Rothwell PM. Effects of antihypertensive-drug class on interindividual variation in blood pressure and risk of stroke: a systematic review and meta-analysis. Lancet. 2010;375:906–915. doi: 10.1016/S0140-6736(10)60235-8. [DOI] [PubMed] [Google Scholar]
- 52.Hawkshead J, K-W M. Techniques of measuring medication adherence in hypertensive patients in outpatient settings: advantages and limitations. Dis Manag Health Outcomes. 2007;15:109–118. [Google Scholar]
- 53.National Center for Health Statistics. Health, United States, 2007 Chartbook on trends in the health of Americans. Hyattsville, MD: 2007. [PubMed] [Google Scholar]
- 54.Schober SE, Makuc DM, Zhang C, Stephenson JK, Burt V. NCHS Data Brief. Vol. 57. Hyattsville, MD: National Center for Health Statistics; 2011. Health insurance affects diagnosis and control of hypercholesterolemia and hypertension among adults aged 20-64. United States 2005-2008. Morbidity and Mortality Weekly Report. [PubMed] [Google Scholar]
- 55.Osterberg L, Blaschke T. Adherence to medication. N Engl J Med. 2005;353:487–497. doi: 10.1056/NEJMra050100. [DOI] [PubMed] [Google Scholar]
- 56.Ho PM, Bryson CL, Rumsfeld JS. Medication adherence: its importance in cardiovascular outcomes. Circulation. 2009;119:3028–3035. doi: 10.1161/CIRCULATIONAHA.108.768986. [DOI] [PubMed] [Google Scholar]
- 57.Bokhour BG, Berlowitz DR, Long JA, Kressin NR. How do providers assess antihypertensive medication adherence in medical encounters? J Gen Intern Med. 2006;21:577–583. doi: 10.1111/j.1525-1497.2006.00397.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Grymonpre R, Cheang M, Fraser M, Metge C, Sitar DS. Validity of a prescription claims database to estimate medication adherence in older persons. Med Care. 2006;44:471–477. doi: 10.1097/01.mlr.0000207817.32496.cb. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.