Abstract
Purpose
The Pictorial Representation of Illness and Self Measure-Revised 2 (PRISM-R2) has been developed as generic measure to assess suffering. The aim of this study was to evaluate the ability of this instrument to identify long-term cancer survivors with high levels of suffering who may need additional support.
Methods
1299 cancer survivors completed the PRISM-R2, the Short Form Health Survey (SF-36), and the Quality of Life-Cancer Survivors questionnaire (QoL-CS). The PRISM-R2 distinguishes between the Self-Illness Separation (SIS) and Illness Perception Measure (IPM), both measuring aspects of suffering.
Results
112 (9%) cancer survivors reported high suffering according to IPM. This group had a higher cancer stage at diagnosis, more cancer recurrences, more comorbidities, and were lower educated compared to people reporting less suffering. The PRISM-R2 could explain substantial amounts of variance (10–14%) in the psychological aspects of the SF-36 and QoL-CS. The IPM also discriminated statistically and clinically significant between high- and low-health status.
Conclusion
The PRISM-R2 proved to be able to discriminate between individuals with good and deteriorated levels of QoL. Further evaluation of its validity and screening potential is recommended.
Keywords: Oncology, Survivors, PRISM-R2, Suffering, Quality of life
Introduction
According to Cassell, suffering is evoked by “the immediate onslaught of distress-physical, emotional, or social” and that the main objective of medicine is to alleviate suffering [1]. He further emphasizes that the intactness of a person needs to be threatened and that “the interpretation of events determines whether suffering or merely distress is experienced” [1]. In this sense, suffering can be seen as a qualitatively different and more severe state of physical, emotional, or social distress. Based on these conceptualizations, the authors suggest that (especially in the long run) the (re)interpretations, explanations, and understanding of what has happened are essential for cancer survivors to come to terms with their former disease and to place it/accept it in their lives. Research has shown that some people surviving cancer report fear of recurrences and/or long-term complications, restrictions in daily (social) life, working life, and sexual functioning resulting in deteriorated levels of quality of life (QoL) and increased distress [2, 3]. Depending on how these (and other) aspects dominate or arise in a cancer survivor’s life, a state of suffering could be developed.
The Pictorial Representation of Illness and Self Measure-Revised 2 (PRISM-R2) is a modified version of the original Pictorial Representation of Illness and Self Measure (PRISM) [4] which can be used to assess the extent to which people suffer from an (somatic) illness. As of now the PRISM and PRISM-R2 have been exclusively administered and evaluated in patients with current diseases or symptoms [4–16]. This study wants to take a step further and examines to what extent cancer survivors still suffer from the aftermath of their disease. The authors aim to bring together suffering with the construct of QoL and it was assumed that those who suffer more, may be more likely in need of additional support and care.
This study sets out two foci: the investigation of the survivors and the instrument. First, the authors examine if and to what extent, cancer survivors are still affected by their former disease and treatment. Second, it was to evaluate the properties of the PRISM-R2 by examining its associations with QoL and health status as well as testing its possible screening capacity. The authors expect the PRISM-R2 to be an efficient, quick, and easy-to-use tool for both health care provider and patient because of the implicit strong statement that can be made by the patient with this visual task.
Method
Design and recruitment
This is a secondary analysis of a population-based, cross-sectional survey on long-term survivors of prostate cancer, endometrial cancer, Hodgkin’s, and non-Hodgkin’s lymphoma that was conducted at the Eindhoven Cancer Registry (ECR) in 2004. The ECR collects data from all patients newly diagnosed with cancer in the southern part of the Netherlands, which is an area that has 2.3 million inhabitants. The ECR was used to select all patients who were diagnosed with endometrial or prostate cancer between 1994 and 1998 and patients who were diagnosed with Hodgkin’s and non-Hodgkin’s lymphoma between 1989 and 1998. Participants older than 75 years at diagnosis were excluded because it was expected that they would have difficulties completing the measures without assistance. To exclude all patients who had died before November 2004, the database was linked with the database of the Central Bureau for Genealogy, which collects Dutch mortality statistics through the civil municipal registries. After excluding all deceased patients, data collection was started in November 2004. Medical specialists sent their (former) patients a letter to inform them about the study, together with the questionnaires. The letter explained that, by returning the completed questionnaires, the patient agreed to participate and consented to linkage of the questionnaire data with their disease history as registered in the ECR. Patients were reassured that non-participation would not have any consequences for their follow-up care or treatment. Approval for this study was obtained from a local certified Medical Ethics Committee.
Measures
PRISM-R2
The original PRISM [4] examines the degree of suffering by using a visual task performance. It consists of a disk (labeled as “self”) placed in the lower right corner of a white A4-sheet which is labeled as one’s living environment. Patients are requested to place a so-called illness-disk (labeled “my medical problem”) in relation to their self-disk and living environment. Since the developers of the PRISM-R2 [10] felt that the self should be in the centre of one’s life, they modified it into a circle with the self-disk in its centre. In addition, they included three different sizes of the illness-disk (smaller, equal to, and bigger than the self-disk). Picture 1a and b both illustrate the design and possible applications of the PRISM-R2. Two outcome variables, both tapping aspects of suffering, are obtained with this instrument. First, the distance from the centre of the self to the centre of the illness-disk represents the Self-Illness Separation (SIS), ranging from 0 to 93 mm. Following Pincus and Morley [17], a separation between illness and self schema is assumed to signify a healthy adjustment to the illness. The PRISM, assessing the subjective position of one’s illness in relation to the self, seems to match this definition rather well [11]. Second, the chosen illness disk size stands for the so-called Illness Perception Measure (IPM) which represents the perceived severity of the former disease. Therefore, a smaller disk (lower IPM) corresponds to lower levels of perceived severity of the aftermath of cancer. The participants received a written instruction to choose the illness-disk which represented the perceived impact of their former cancer on their current life best, and put it in relation to themselves and their environment. In this study, a paper-version of the PRISM-R2 was used and the illness-disks were provided as stickers to allow completion of all measures in the home situation and returning the package by mail.
Picture 1.
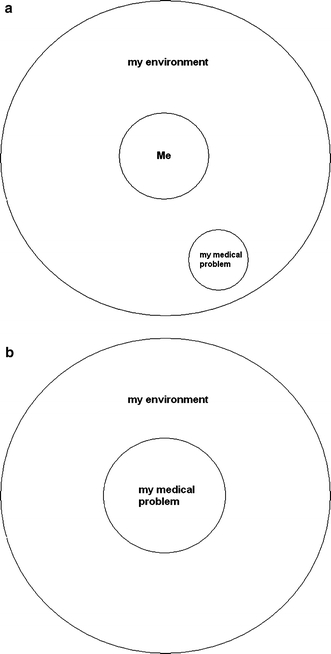
a Illustration of PRISM with adequate coping and integration (small illness-disk far away from self). b Illustration of PRISM with large continued impact of cancer (large illness-disk close to self)
SF-36
The 36-Item Short Form Health Survey (SF-36) [18] measures health status on eight subscales: physical functioning (PF), role physical functioning (RP), bodily pain (BP), general health (GH), vitality (VT), social functioning (SF), role emotional functioning (RE), and mental health (MH). The scores of these scales are converted into a 0–100 scale with higher scores indicating a better functioning. Furthermore, the eight scales can be summed up into two domains: the physical component summary (PCS) and mental component summary (MCS).
QoL-CS
The Quality of Life-Cancer Survivors questionnaire (QoL-CS) assesses QoL in connection to cancer survivorship [19]. It is a 44-item visual analog scale, based on a scale from 0 (worst outcome) to 10 (best outcome). The items can be transformed into four scales: physical, psychological, social, and spiritual well-being. Furthermore, a total score can be calculated incorporating all four scales and displaying an estimate of the overall QoL. The QoL-CS examines issues of particular concern to cancer survivors, such as distress since diagnosis, sexuality, employment, uncertainty about the future, and the role of spirituality and religion. The QoL-CS has been demonstrated to be a reliable and valid instrument [19–22], although the subscale spiritual well-being showed low reliability in the Dutch population [19]. The same pattern has been found in this sample: a low Cronbach’s alpha for spiritual well-being (.49) while the other subscales and the total score showed satisfying to high-internal consistencies ranging from .71 (social), .86 (physical), .88 (psychological), to .90 (total score).
Statistical analyses
All statistical analyses were performed using the Statistical Package for Social Sciences (SPSS, version 17.0 Chicago, IL, USA). Socio-demographic and clinical data were tested for differences between the respondents and non-respondents using χ2 analyses for categorical variables and t-tests for continuous variables. Furthermore, analyses of variance (ANOVA) and χ2 tests were used (respectively for SIS and IPM) to examine differences on the PRISM-R2 related to socio-demographic or clinical data such as: age at diagnosis, time since diagnosis, gender, marital status, socio-economical status (SES), education, cancer stage at diagnosis, primary treatment, comorbidity, cancer recurrence, and the use of counseling. SES has been rated using the guidelines of the institute Statistics Netherlands which has developed an indicator of SES for each postal code (on average, 17 households) based on aggregated individual fiscal data concerning the economic value of the home and household income. SES was categorized into tertiles: low (decile 1–3), medium (4–7), or high (8–10) [23]. Comorbidity was assessed with a slightly adapted version of the Charlson comorbidity index [24]. For a more adequate interpretation of the SF-36-results, the scores of the patient sample were compared with a large, random, nationwide normative sample of adults (n = 1742) taken from the general Dutch population [18]. The authors matched this sample with the sample in terms of age and gender. Given the large amount of simultaneous comparisons, it was adjusted the alpha-level was adjusted using the Bonferroni-method. Subsequently, it was used Norman’s rule of thumb was used, stating that the threshold of discrimination for changes in health status scores for a chronic disease is approximately half a standard deviation, to assess the magnitude of differences [25].
In order to evaluate the convergent validity of the PRISM-R2, correlations with the subscales and summary scores of the SF-36 and QoL-CS were computed. Correlations lower than .3 were considered weak and correlations above .5 strong [26]. Finally, it was tested how much variance the PRISM-R2 could predict in the health status and QoL in this sample of long-term cancer survivors controlling for socio-demographic and clinical data. Socio-demographic and clinical data included: age, survival time, gender, marital status, socio economical status, education, cancer type, stage, amount of comorbid disorders, and cancer recurrence.
Results
Participants
One thousand four hundred and seventy-five people returned complete questionnaires (80%). In comparison to the respondents, the non-respondents were on average somewhat older (66 vs. 69 years; t = −3.189; P = .001). Both groups did not differ regarding their gender and survival time. Of the 1475 respondents, 176 people (12%) did not complete the PRISM-R2 and these patients were on average older (74 vs. 67 years; t = −9.996; P < .0001), more often widowed (24% vs. 12%; χ2 = 23.908; P < .0001), and more often lower educated (60% vs. 42%; χ2 = 31.336; P < .0001).
The final sample of 1299 participants consisted of long-term prostate cancer survivors (n = 651; 50%), endometrial cancer survivors (n = 265; 20%), and survivors of non-Hodgkin’s (n = 258; 20%) and Hodgkin’s lymphoma (n = 125; 10%). Socio-demographic and clinical characteristics of the participants are displayed in Table 1.
Table 1.
Socio-demographic and clinical description for the whole sample and separated by IPM; comparisons of differences in distributions between the IPM-groups
| Small disk n = 861 |
Medium disk n = 326 |
Large disk n = 112 |
F diff. | Whole sample n = 1299 |
|
|---|---|---|---|---|---|
| Mean (SD) Range |
Mean (SD) Range |
Mean (SD) Range |
Mean (SD) Range |
||
| Age at diagnosis | 57.6 (14.2) | 59.4 (12.3) | 59.0 (10.2) | 58 (13.4) | |
| 9–75 | 7–75 | 30–75 | 7–75 | ||
| Years since diagnosis | 8.7 (2.0) | 8.6 (1.8) | 8.7 (1.6) | 9 (1.9) | |
| 6–15 | 6–15 | 6–14 | 6–15 | ||
| n (%) | n (%) | n (%) | χ2 | n (%) | |
| Cancer type | |||||
| Endometrial | 179 (20.8) | 64 (19.6) | 22 (19.6) | 265 (20.4) | |
| Hodgkin | 97 (11.3) | 22 (6.7) | 6 (5.4) | 125 (9.6) | |
| Non-Hodgkin | 173 (20.1) | 64 (19.6) | 21 (18.8) | 258 (19.9) | |
| Prostate | 412 (47.9) | 176 (54) | 63 (56.3) | 651 (50.1) | |
| Sex | |||||
| Female | 312 (36.2) | 105 (32.2) | 33 (29.5) | 450 (34.6) | |
| Male | 549 (63.8) | 221 (67.8) | 79 (70.5) | 849 (65.4) | |
| Marital status | |||||
| Single | 637 (74) | 242 (74.2) | 88 (78.6) | 967 (74.4) | |
| Married | 75 (8.7) | 20 (6.1) | 5 (4.5) | 99 (7.6) | |
| Divorced | 37 (4.3) | 16 (4.9) | 2 (1.8) | 55 (4.2) | |
| Widowed | 104 (12.1) | 43 (13.2) | 16 (14.3) | 163 (12.4) | |
| Unknown | 8 (0.9) | 5 (1.5) | 1 (0.9) | 15 (1.2) | |
| SESa | |||||
| Low | 177 (20.6) | 78 (23.9) | 31 (27.7) | 286 (22.0) | |
| Medium | 354 (41.1) | 141 (43.3) | 47 (42.0) | 542 (41.7) | |
| High | 302 (35.1) | 99 (30.4) | 31 (27.7) | 432 (33.3) | |
| Unknown | 28 (3.3) | 8 (2.4) | 3 (2.7) | 39 (3.0) | |
| Educational level | |||||
| Low | 310 (36.0) | 172 (52.8) | 68 (60.7) | 46.056** | 550 (42.3) |
| Medium | 325 (37.7) | 101 (31.0) | 27 (24.1) | 454 (34.9) | |
| High | 209 (24.3) | 47 (14.4) | 16 (14.3) | 272 (20.9) | |
| Unknown | 17 (2.0) | 6 (1.8) | 1 (0.9) | – | |
| Stage | |||||
| I | 370 (43.0) | 134 (41.1) | 33 (29.5) | 15.307* | 537 (41.3) |
| II | 326 (37.9) | 133 (40.8) | 48 (42.9) | 507 (39.0) | |
| III | 56 (6.5) | 15 (4.6) | 7 (6.3) | 78 (6.0) | |
| IV | 68 (7.9) | 29 (8.9) | 19 (17.0) | 116 (8.9) | |
| Unknown | 41 (4.8) | 15 (4.6) | 5 (4.5) | 61 (4.7) | |
| Primary treatment Surgery | |||||
| Chemotherapy | 388 (45.1) | 151 (46.3) | 47 (42.0) | 586 (45.1) | |
| Radiotherapy | 177 (20.6) | 61 (18.7) | 19 (17.0) | 257 (19.8) | |
| Hormonal therapy | 170 (19.7) | 55 (16.9) | 21 (18.8) | 246 (19.8) | |
| Wait and see | 78 (9.1) | 36 (11.0) | 17 (15.2) | 131 (10.1) | |
| Unknown | 42 (4.9) | 21 (6.4) | 8 (7.1) | 71 (5.5) | |
| 6 (0.7) | 2 (0.6) | – | 8 (0.6) | ||
| Comorbidity | |||||
| None | 267 (31.0) | 66 (20.2) | 24 (21.4) | 27.162** | 357 (27.5) |
| 1 | 315 (36.6) | 108 (33.1) | 39 (34.8) | 463 (35.6) | |
| ≥2 | 278 (32.3) | 152 (46.6) | 49 (43.8) | 479 (36.9) | |
| Cancer recurrence | 128 (14.9) | 77 (23.6) | 42 (37.5) | 38.964** | 247 (19) |
| Counseling | |||||
| GPb | 89 (10.3) | 44 (13.5) | 24 (21.4) | 12.290* | 157 (12.1) |
| Physiotherapist | 34 (3.9) | 22 (6.7) | 12 (10.7) | 11.154* | 68 (5.2) |
| Psychologist | 32 (3.7) | 18 (5.5) | 8 (7.1) | 58 (4.5) | |
a SES socio economical status
b GP general practitioner
* P < .05; ** P < .0001
PRISM-R2
Within the whole sample, the SIS ranged from 0 to 172 mm (mean: 59.1, SD: 27.8). Twenty-nine participants placed their illness-disk (against the instructions) outside of the circle (94–172 mm) labeled as environment. However, these people did not differ from those that placed the illness-disk on the boundaries of the circle (n = 457; SIS range: 76–93 mm) regarding socio-demographic and clinical data.
Socio-demographic and clinical differences associated with the SIS scores were found in such way that the highest educated participants reported higher average SIS scores. Whereas participants who experienced new primary tumors or relapses obtained significantly lower SIS scores.
The majority of the participants (66%) chose the smallest illness-disk (IPM = 1) to symbolize the perceived impact of their former cancer disease whereas 112 (9%) chose the largest disk (IPM = 3). Examining differences on the IPM yielded results comparable to SIS. Higher educated people as well as participants who did not have any new tumors or relapses, chose smaller illness-disks (χ2 = 46.056; P < .0001 and χ2 = 38.964; P < .0001, respectively). Furthermore, participants with a higher amount of comorbid disorders, or those previously diagnosed with stage IV disease, were more likely to choose the large illness-disk (χ2 = 27.162; P < .0001 and χ2 = 15.307; P = .018, respectively; see Table 1). Interestingly, people with a shorter time since diagnosis compared to people with a longer survival time (median split: 8.3 years) did not differ on SIS and IPM.
The association between SIS and IPM was found to be moderate (r = −.33; P < .0001) and indicated that smaller IPMs were generally associated with larger SISs and vice versa.
Cancer survivors versus normative population
Cancer survivors, as a whole group, reported statistically significant (P < .001) lower levels of health status, as measured with the SF-36, compared to the age- and sex-matched normative population, except for the subscales social functioning and mental health that failed to reach the adjusted level of significance (P = .005). However, the differences between cancer patients and the normative population ranged from 1 to 7 points and were therefore not considered clinically meaningful [25] (see Table 2).
Table 2.
Mean scores and standard deviations (SD) from the whole sample and stratified by IPM regarding every psychological measurement (PRISM-R2, SF-36, and QoL-CS); One-way ANOVA testing group differences
| Whole sample n = 1299 | IPM = 1 n = 861 (66%) (1) | IPM = 2 n = 326 (25%) (2) | IPM = 3 n = 112 (9%) (3) | Sign. diff. | Norma | |
|---|---|---|---|---|---|---|
| PRISM-SIS | 59.12 (27.8) 0–172 | 65.7 (27.0) 0–172 | 47.9 (23.8) 0–140 | 41.2 (26.8) 0–135 | 1 > 2, 3** | |
| SF-36 | ||||||
| PF | 69.2† (27.2) | 74.5† (24.9) | 60.1† (28.5) | 53.3† (28.7) | 1 > 2, 3** | 72.1 |
| RP | 63.6† (42.6) | 73.3† (38.5) | 47.2† (44.6) | 32.9† (39.8) | 1 > 2 > 3** | 68.8 |
| BP | 77.9† (24.1) | 82.6† (21.3) | 70.7 (25.1) | 62.8† (28.9) | 1 > 2 > 3** | 72.3 |
| GH | 57.4† (21.8) | 63.4 (19.7) | 47.5† (19.8) | 40.0† (22.3) | 1 > 2 > 3** | 64.6 |
| VT | 63.4† (21.1) | 68.4 (19.2) | 55.2† (20.7) | 48.7† (22.6) | 1 > 2 > 3** | 67.0 |
| SF | 79.8 (23.4) | 85.4† (19.6) | 71.2† (24.4) | 61.7† (29.9) | 1 > 2 > 3** | 81.5 |
| RE | 75.1† (39.3) | 84.1† (32.5) | 60.5† (44.8) | 47.1† (45.4) | 1 > 2 > 3** | 80.9 |
| MH | 75.4 (18.1) | 79.3† (15.7) | 70.0† (18.1) | 60.7† (23.3) | 1 > 2 > 3** | 76.5 |
| PCS | 44.3† (11.2) | 46.8† (10.1) | 40.0† (11.7) | 37.3† (10.9) | 1 > 2 > 3** | 45.4 |
| MCS | 51.6† (9.9) | 54.0† (8.2) | 47.9† (10.8) | 43.2† (12.3) | 1 > 2 > 3** | 52.9 |
| QoL-CS | ||||||
| Physical | 7.4 (2.1) | 7.9 (1.9) | 6.7 (2.2) | 6.1 (2.1) | 1 > 2 > 3** | |
| Psychol.b | 6.5 (1.6) | 6.9 (1.4) | 5.8 (1.6) | 4.9 (1.8) | 1 > 2 > 3** | |
| Social | 6.9 (1.7) | 7.3 (1.4) | 6.3 (1.8) | 5.6 (1.9) | 1 > 2 > 3** | |
| Spiritual | 4.7 (1.5) | 4.8 (1.5) | 4.6 (1.4) | 4.4 (1.5) | 1 > 3* | |
| QoLc | 6.5 (1.3) | 6.8 (1.1) | 6.0 (1.2) | 5.1 (1.4) | 1 > 2 > 3** | |
a Norm normative population
b Psychol. psychological
c QoL quality of life total score
† Significantly different from normative population (P < .0001), but see text for clinical meaningfulness
* P < .05; ** P < .0001
Subsequently, survivors were divided into three groups on the basis of IPM and comparisons of these three groups to the normative population showed a different picture. Those who chose a large illness-disk (9%) reported statistically (P < .001) and clinically significant lower levels of scores on all domains of the SF-36. In contrasts, survivors who chose a small illness-disk reported statistically significant higher levels of health status compared to the normative population, except for the subscales general health and vitality, which both failed to reach statistical significance. Again the mean differences were quite small, suggesting comparable levels of health status between the normative population and cancer survivors with a small IPM. The group that chose a medium illness-disk took an intermediate position. All subscales (except for bodily pain) turned out to be significantly lower compared to the normative population, but these were clinically meaningful on only five subscales: RP, GH, VT, FF, RE.
After comparing each IPM-group to the normative group, the authors additionally explored whether the IPM discriminated within the sample of cancer survivors with respect to health status and QoL. Significant differences emerged on every subscale of the SF-36 and QoL-CS where the small illness-disk was always associated with the highest levels of health status and QoL. The two groups choosing the medium- and large-IPMs did not always appear to be significantly different from another (i.e., SF-36-physical functioning and QoL-CS-spiritual well-being; see Table 2).
Associations of PRISM-R2 with SF-36 and QoL-CS
SIS correlated weakly (r = .12 to .23; P < .0001) with the subscales of the SF-36 and QoL-CS, while IPM showed weak to moderate negative associations with these subscales (r = −.10 to −.45; all P < .0001; Table 3). The highest association was found between IPM and the QoL-CS-total score (r = −.45; P < .0001; see also Table 3). See also Fig. 1 for an overview of the results of all self-report measures stratified by the chosen illness-disk (IPM).
Table 3.
Correlations of the SIS and IPM with the subscales of the SF-36 and QoL-CS
| Subscale | PRISM-SIS | PRISM-IPM |
|---|---|---|
| PRISM-SIS | – | −.329 |
| SF-36-PF | .142 | −.280 |
| SF-36-RP | .176 | −.334 |
| SF-36-BP | .123 | −.283 |
| SF-36-GH | .227 | −.391 |
| SF-36-VT | .186 | −.335 |
| SF-36-SF | .172 | −.350 |
| SF-36-RE | .198 | −.331 |
| SF-36-MH | .156 | −.331 |
| SF-36-PCS | .168 | −.312 |
| SF-36-MCS | .187 | −.363 |
| QoL-CS-physical | .166 | −.325 |
| QoL-CS-psychological | .261 | −.412 |
| QoL-CS-social | .198 | −.362 |
| QoL-CS-spiritual | .086 | −.088 |
| QoL-CS-total score | .263 | −.445 |
All displayed correlations are significant at the 1%-level
Fig. 1.
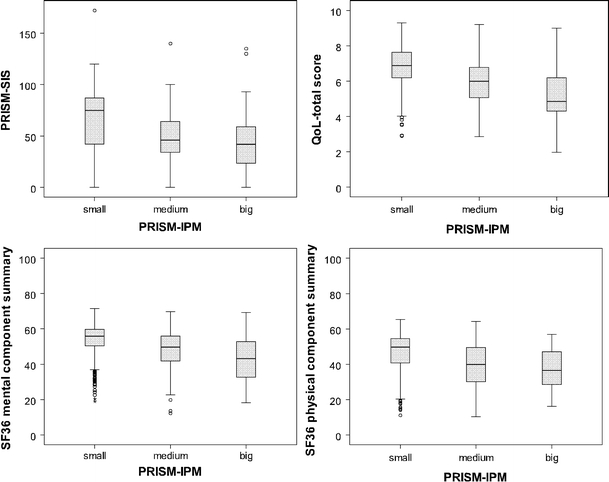
Outcome on the PRISM–SIS, QoL–total score and the SF36–component summaries by sicker sizes [small n=861; medium n=326; big n=112]
When predicting the SF-36-MCS and QoL-CS-total score using multiple linear regressions, a rather small amount of variance (8 and 17%, respectively) could be explained in the first step using socio-demographic and clinical data. However, the addition of SIS and IPM in the second step led to a substantial increase in the explained variance up to 20 and 34% (F = 16.121; P < .0001 and F = 32.025; P < .0001, respectively). The same overall patterns were found for the SF-36-PCS, but the PRISM-R2 did not add as much value as in more psychologically related aspects. In this case, socio-demographic and clinical data already explained 25% of the variance and the final model, also including the PRISM-R2 values, explained a variance of 32% (F = 29.406; P < .0001).
Overall, IPM was by far the most weighted factor predicting health status and QoL in all of these regression analyses.
Discussion
Given the two foci on the study, the aims were threefold: (1) to examine suffering in long-term cancer survivors; (2) to investigate the properties of the PRISM-R2; and (3) to obtain a better insight into its possible use as a measure to identify cancer survivors who may need additional support and care.
The majority of participants chose a small illness-disk (66%) and tended to place it quite far away from their self symbolizing the separation between themselves and their former cancer diagnosis and treatment. This may be interpreted as indicating adequate coping and the integration of the cancer experience in their current life. On the other hand, still 9% of long-term (6–15 years after diagnosis) cancer survivors chose the large illness-disk, which was associated with distress and suffering. This mainly concerned patients with lower education, cancer recurrence, more comorbid conditions, and a higher tumor stage at diagnosis. Lower education indeed might be expected to have a negative impact on one’s capacity to deal with diseases like cancer. As already suggested in the literature [27, 28], higher educated people may have more resources or coping skills allowing more effective coping with their former disease. Cancer recurrences, higher comorbidity, and more severe tumor stages are all very plausibly associated with more suffering. It should be noted that comorbid conditions may occur independent of the cancer and treatment itself, but are nevertheless experienced as additionally burdensome and challenging one’s coping resources which might result in higher levels of suffering. Interestingly, time since diagnosis did not have an impact on the chosen IPM and SIS, suggesting that a longer time since diagnosis is not necessarily associated with less suffering.
A limited number of participants (n = 29) also chose to place their illness-disk outside of their environment which was not statistically meaningful, but the authors feel that the opportunity to do so gave the participants optimal freedom to visualize their experienced level of suffering.
A serious drawback of most QoL measures is that they never cover all aspects of the disease that patients consider as relevant for one’s well-being. In case of the PRISM-R2, however, the lack of such a predetermined list of aspects may be regarded as a major asset, because the patient has optimal freedom to make an internal calculation of all pros and cons, each with his or her personal weight factor. In that way, this measure may be considered a more qualitative screening measure that overcomes some of the most serious difficulties of QoL measures [29].
The obtained pattern of correlations of the PRISM-R2 with the SF-36 and QoL-CS met the expectations and also corroborated previous findings [10]. Of major significance is the finding that IPM and SIS were both stronger associated with subscales assessing psychological and social well-being, rather than physical health, which is in line with Cassell’s conceptualizations of suffering as a predominantly psychological construct.
Cancer survivors with small illness-disks (low IPM) proved to be comparable to the normative population with respect to health status, while participants who chose a large illness-disk (high IPM) reported significantly lower levels of health status. This result was supported by the regression analyses which consistently showed IPM to be by far the most important factor predicting health status and QoL. Small Illness-disks were always associated with higher levels of health status and QoL compared to the normative population, suggesting that they are not likely to be characterized by severely deteriorated levels of well-being. On the other hand, patients choosing a medium or large illness-disk are more likely in need of attention in clinical practice. Overall, the discriminative ability of the IPM supports the notion of a good specificity of the PRISM-R2 by producing right-negative results. Small illness-disks indicate low levels of suffering and need no or little clinical attention while medium and especially large illness-disks should raise concern since they can be interpreted as indicating extra need for attention and support. Nonetheless, it is crucial to also take the SIS into account in order to obtain a more complete impression of the degree of suffering.
This study was the first to examine the properties of the PRISM-R2 in a cohort not currently suffering from a severe disease and suggests provisional support of its validity and screening ability which should encourage further evaluation. Nevertheless, one major limitation needs to be addressed: lower educated people appeared to have more problems to complete the PRISM-R2 task, indicating that a certain cognitive capacity is needed to understand this more abstract measure. This also suggests a limited applicability for the generic use of the PRISM-R2. However, in a clinical setting (different from the study presented here), patients can be better instructed and have the opportunity to ask questions about the task and completion could be facilitated also for low educated individuals.
The PRISM, like most screening tools, should always be followed by a closer and more thorough examination of the patient as the information gained from this screening tool will not provide adequate understanding of the actual needs of the survivor to identify what actions might be taken to eliminate/alleviate their self-perceived suffering.
Future research is needed to obtain insight into the cognitive processes and considerations that result in the decision why to select a specific illness-disk and where to place it, in order to examine this instrument’s construct validity. More in depth investigations are needed that investigate the associations between suffering and coping, denial, distraction, and other defense mechanisms, because low suffering does not necessarily imply anything about the way a person has dealt with a life-threatening disease.
Conclusion
The PRISM-R2 might be a valuable addition to the currently available tools to evaluate suffering and well-being, and to identify patients with additional need for care and support, because of the following four aspects: (1) it gives patients optimal freedom to consider any personally important aspect when assessing suffering; (2) it facilitates communication between patients and health care providers; (3) it has the capacity to stimulate patients to uncover hidden problems; and finally (4) it may be useful to evaluate all kinds of interventions. In the present cohort of cancer survivors, 66% were identified as not suffering based on the PRISM-R2 variables, in particular IPM. This group was characterized by similar levels of health status and QoL compared to an age- and sex-matched normative population. The authors are aware that the PRISM-R2 is a rather qualitative measure that cannot yield or withstand any hard criteria concerning psychometric properties with the cross-sectional data. However, the authors are confident that this study is the first (successful) attempt to get more insight into the usefulness of the PRISM-R2 for cancer survivors by relating it to QoL and health status measures.
Acknowledgments
The authors would like to thank all patients and their doctors for their participation in the study.
Conflict of interest
None.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Abbreviations
- ANOVA
Analyses of variance
- BP
Bodily pain
- ECR
Eindhoven Cancer Registry
- GH
General health
- IPM
Illness Perception Measure
- MH
Mental health
- MCS
Mental component summary
- PCS
Physical component summary
- PRISM
Pictorial Representation of Illness and Self Measure
- PRISM-R2
Pictorial Representation of Illness and Self Measure-Revised 2
- PF
Physical functioning
- QoL
Quality of Life
- QoL-CS
Quality of Life-Cancer Survivors questionnaire
- RE
Role emotional functioning
- RP
Role physical functioning
- SIS
Self-Illness Separation
- SF-36
Short Form Health Survey
- SF
Social functioning
- VT
Vitality
References
- 1.Cassell EJ. The nature of suffering and the goals of medicine. New York: Oxford University; 1991. [Google Scholar]
- 2.Stein KD, Syrjala KL, Andrykowski MA. Physical and psychological long-term and late effects of cancer. Cancer. 2008;112(11 Suppl):2577–2592. doi: 10.1002/cncr.23448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Foster C, Wright D, Hill H, Hopkinson J, Roffe L. Psychosocial implications of living 5 years or more following a cancer diagnosis: A systematic review of the research evidence. European Journal of Cancer Care. 2009;18(3):223–247. doi: 10.1111/j.1365-2354.2008.01001.x. [DOI] [PubMed] [Google Scholar]
- 4.Buchi S, Sensky T, Sharpe L, Timberlake N. Graphic representation of illness: A novel method of measuring patients’ perceptions of the impact of illness. Psychotherapy and Psychosomatics. 1998;67(4–5):222–225. doi: 10.1159/000012284. [DOI] [PubMed] [Google Scholar]
- 5.Buchi S, Sensky T. PRISM: Pictorial Representation of Illness and Self Measure. A brief nonverbal measure of illness impact and therapeutic aid in psychosomatic medicine. Psychosomatics. 1999;40(4):314–320. doi: 10.1016/S0033-3182(99)71225-9. [DOI] [PubMed] [Google Scholar]
- 6.Buchi S, Villiger P, Kauer Y, Klaghofer R, Sensky T, Stoll T. PRISM (Pictorial Representation of Illness and Self Measure)- a novel visual method to assess the global burden of illness in patients with systemic lupus erythematosus. Lupus. 2000;9(5):368–373. doi: 10.1191/096120300678828479. [DOI] [PubMed] [Google Scholar]
- 7.Buchi S, Buddeberg C, Klaghofer R, Russi EW, Brandli O, Schlosser C, Stoll T, Villiger PM, Sensky T. Preliminary validation of PRISM (Pictorial Representation of Illness and Self Measure)—a brief method to assess suffering. Psychotherapy and Psychosomatics. 2002;71(6):333–341. doi: 10.1159/000065994. [DOI] [PubMed] [Google Scholar]
- 8.Rumpf HJ, Lontz W, Uesseler S. A self-administered version of a brief measure of suffering: First aspects of validity. Psychotherapy and Psychosomatics. 2004;73(1):53–56. doi: 10.1159/000074440. [DOI] [PubMed] [Google Scholar]
- 9.Denton F, Sharpe L, Schrieber L. PRISM: Enmeshment of illness and self-schema. Psychotherapy and Psychosomatics. 2004;73(1):57–63. doi: 10.1159/000074441. [DOI] [PubMed] [Google Scholar]
- 10.Wouters EJ, Reimus JL, van Nunen AM, Blokhorst MG, Vingerhoets AJ. Suffering quantified? Feasibility and psychometric characteristics of 2 revised versions of the Pictorial Representation of Illness and Self Measure (PRISM) Journal of Behavioral Medicine. 2008;34(2):65–78. doi: 10.3200/BMED.34.2.65-78. [DOI] [PubMed] [Google Scholar]
- 11.Klis S, Vingerhoets AJ, de Wit M, Zandbelt N, Snoek FJ. Pictorial Representation of Illness and Self Measure Revised II (PRISM-RII): A novel method to assess perceived burden of illness in diabetes patients. Health and Quality of Life Outcomes. 2008;6:104. doi: 10.1186/1477-7525-6-104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Streffer ML, Buchi S, Morgeli H, Galli U, Ettlin D. PRISM (pictorial representation of illness and self measure): A novel visual instrument to assess pain and suffering in orofacial pain patients. Journal of Orofacial Pain. 2009;23(2):140–146. [PubMed] [Google Scholar]
- 13.Muhleisen B, Buchi S, Schmidhauser S, Jenewein J, French LE, Hofbauer GF. Pictorial Representation of Illness and Self Measure (PRISM): A novel visual instrument to measure quality of life in dermatological inpatients. Archives of Dermatology. 2009;145(7):774–780. doi: 10.1001/archdermatol.2009.121. [DOI] [PubMed] [Google Scholar]
- 14.Kassardjian CD, Gardner-Nix J, Dupak K, Barbati J, Lam-McCullock J. Validating PRISM (Pictorial Representation of Illness and Self Measure) as a measure of suffering in chronic non-cancer pain patients. Journal of Pain. 2008;9(12):1135–1143. doi: 10.1016/j.jpain.2008.06.016. [DOI] [PubMed] [Google Scholar]
- 15.Reinhardt S, Bischof G, Grothues J, John U, Rumpf HJ. Performance of the pictorial representation of illness and self measure in individuals with alcohol dependence, alcohol abuse or at-risk drinking. Psychotherapy and Psychosomatics. 2006;75(4):249–256. doi: 10.1159/000092896. [DOI] [PubMed] [Google Scholar]
- 16.Buchi S, Brandli O, Klingler K, Klaghofer R, Buddeberg C. Inpatient rehabilitation in inpatients with chronic obstructive lung diseases (COPD): Effect on physical capacity for work, psychological wellbeing and quality of life. Schweizerische medizinische Wochenschrift. 2000;130(5):135–142. [PubMed] [Google Scholar]
- 17.Pincus T, Morley S. Cognitive-processing bias in chronic pain: A review and integration. Psychological Bulletin. 2001;127(5):599–617. doi: 10.1037/0033-2909.127.5.599. [DOI] [PubMed] [Google Scholar]
- 18.Aaronson NK, Muller M, Cohen PD, Essink-Bot ML, Fekkes M, Sanderman R, Sprangers MA, te Velde A, Verrips E. Translation, validation, and norming of the Dutch language version of the SF-36 Health Survey in community and chronic disease populations. Journal of Clinical Epidemiology. 1998;51(11):1055–1068. doi: 10.1016/S0895-4356(98)00097-3. [DOI] [PubMed] [Google Scholar]
- 19.van Dis FW, Mols F, Vingerhoets AJ, Ferrell B, van de Poll-Franse LV. A validation study of the Dutch version of the Quality of Life-Cancer Survivor (QOL-CS) questionnaire in a group of prostate cancer survivors. Quality of Life Research. 2006;15(10):1607–1612. doi: 10.1007/s11136-006-0015-y. [DOI] [PubMed] [Google Scholar]
- 20.Ferrell BR, Dow KH, Grant M. Measurement of the quality of life in cancer survivors. Quality of Life Research. 1995;4(6):523–531. doi: 10.1007/BF00634747. [DOI] [PubMed] [Google Scholar]
- 21.Ferrell BR, Dow KH, Leigh S, Ly J, Gulasekaram P. Quality of life in long-term cancer survivors. Oncology Nursing Forum. 1995;22(6):915–922. [PubMed] [Google Scholar]
- 22.Zebrack BJ, Chesler MA. A psychometric analysis of the Quality of Life-Cancer Survivors (QOL-CS) in survivors of childhood cancer. Quality of Life Research. 2001;10(4):319–329. doi: 10.1023/A:1012228823115. [DOI] [PubMed] [Google Scholar]
- 23.van Duin C, Keij I. Sociaal-economische status indicator op postcodeniveau. Maandstatistiek van de bevolking. 2002;50:32–35. [Google Scholar]
- 24.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. Journal of Chronic Diseases. 1987;40(5):373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 25.Norman GR, Sloan JA, Wyrwich KW. Interpretation of changes in health-related quality of life: The remarkable universality of half a standard deviation. Medical Care. 2003;41(5):582–592. doi: 10.1097/01.MLR.0000062554.74615.4C. [DOI] [PubMed] [Google Scholar]
- 26.Cohen J. Statistical power analysis for the behavioral sciences. 2. New Jersey: Psychology; 1988. [Google Scholar]
- 27.Ell KO, Nishimoto RH. Coping resources in adaptation to cancer: Socioeconomic and racial differences. Social Service Review. 1989;63:433–446. doi: 10.1086/603712. [DOI] [Google Scholar]
- 28.McEwen BS, Seeman T. Protective and damaging effects of mediators of stress, elaborating and testing the concepts of allostasis and allostatic load. Annals of the New York Academy of Sciences. 1999;896:30–47. doi: 10.1111/j.1749-6632.1999.tb08103.x. [DOI] [PubMed] [Google Scholar]
- 29.Higginson IJ, Carr AJ. Measuring quality of life: Using quality of life measures in the clinical setting. British Medical Journal. 2001;322(7297):1297–1300. doi: 10.1136/bmj.322.7297.1297. [DOI] [PMC free article] [PubMed] [Google Scholar]


