Abstract
Background
Progressive multifocal leukoencephalopathy (PML) is a demyelinating central nervous system disease caused by JC virus (JCV) reactivation in immunocompromised patients. The disease course of PML is often progressive, fatal and at present, there are few reports on successful treatment outcomes.
Case Report
A 45-year-old man with systemic sarcoidosis presented with rapidly progressive dementia and right hemiparesis. The patient was diagnosed with PML as confirmed via brain biopsy and JCV PCR. With a combination treatment of cidofovir and mirtazapine, there was significant improvement of neurological symptoms without measurable functional deficit.
Conclusion
This case suggests that dual therapy with cidofovir and mirtazapine might be an effective treatment option in PML patients with sarcoidosis.
Key words: Progressive multifocal leukoencephalopathy, Sarcoidosis, Cidofovir, Mirtazapine
Introduction
Progressive multifocal leukoencephalopathy (PML) is a deadly demyelinating central nervous system disease caused by reactivation of the JC virus (JCV). It can occur in immunocompromised patients including those with acquired immune deficiency syndrome, hematological malignancies, post-transplantation on immunosuppressive therapy and sarcoidosis [1]. The disease course of PML is usually progressive and fatal. Recent studies have revealed potential therapeutic agents for PML but their efficacy has remained inconsistent. Here, we report a case of PML in a sarcoidosis patient who showed nearly complete recovery after a dual therapy regimen with cidofovir and mirtazapine.
Case Report
A 45-year-old man was admitted with progressive cognitive impairment and right hemiparesis that began 1 month prior. Four months prior to admission, he had been diagnosed with systemic sarcoidosis involving his lungs, liver, spleen, abdominal and mediastinal lymph nodes, as revealed through bronchoscopic lung biopsy. Treatment for sarcoidosis began with 15 mg of prednisone, once daily for 5 weeks, proceeded by 10 mg for the following 4 weeks, and then 5 mg of prednisone as a maintenance dose.
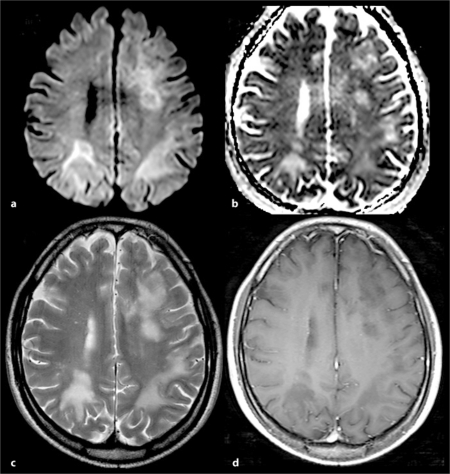
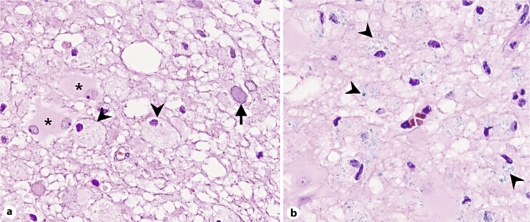
Upon admission, neurological examination revealed right facial palsy (central type) and right hemiparesis (MRC grade III in his right arm and grade IV in his right leg). He also displayed decreased cortical sensation on his right side, Gerstmann syndrome, ideomotor apraxia, optic ataxia and optic apraxia. His Mini-Mental State Examination (MMSE) score (Korean version) was 19/30 with errors in orientation for time, orientation for place, delayed recall, serial sevens, writing and interlocking pentagon drawing. Results of the Seoul Neuropsychological Screening Battery showed cognitive impairment in multiple domains including language, visuospatial, memory and frontal executive function. Serum anti-HIV antibody and HIV antigen tests were negative. Cerebrospinal fluid (CSF) findings were within the normal range. Brain MRI demonstrated bilateral multifocal white matter lesions which were hypointense on T1-weighted imaging and hyperintense on T2-weighted imaging with surrounding edema. No such enhancement occurred on gadolinium-enhanced T1-weighted imaging. Diffusion-weighted imaging revealed a diffusion-restricted peripheral rim with central vasogenic edema, consistent with demyelinating plaques (fig. 1). A brain biopsy was performed, revealing virus-infected oligodendrocytes, active demyelination and reactive astrocytes within the lesion (fig. 2). The JCV PCR test performed on brain tissue was positive, establishing the diagnosis of PML.
Fig. 1.
Brain MRI showing bilateral multifocal white matter lesions. The lesions contain high signal-intense rims on diffusion-weighted images (a). With low signal intensity on an afferent diffusion coefficient map (b). The findings are consistent with demyelinating plaque. c T2-weighted images display hyperintense lesions with surrounding edema. d Gadolinium-enhanced T1-weighted image does not reveal an enhanced lesion area.
Fig. 2.
Neuropathological findings. a The enlarged oligodendrocyte (arrow) contains a glassy nucleus, characteristic of viral inclusion bodies combined with reactive astrocytes (asterisks) (hematoxylin-eosin, ×400). The macrophages (arrowheads) contain cytoplasmic myelin particles, indicating active demyelination. b Myelin particles (arrowheads), stained in blue (Luxol fast blue, ×400).
During the 10 days of hospitalization before treatment, the patient's neurological status displayed continuing deterioration, despite discontinuance of prednisone. Dual therapy with cidofovir and mirtazapine (5 mg/kg intravenous cidofovir weekly for the first 2 weeks followed by biweekly administration of the same dose, and 15 mg of oral mirtazapine daily) was started. The patient's symptoms began to improve gradually from 4 days after treatment. At discharge, 3 weeks after initiation of treatment, motor power had recovered to MRC grade IV on the upper extremity and MRC grade V on the lower extremity, while the MMSE score had improved to 22/30. Four months after being discharged, treatment was discontinued due to increased levels of urine protein (105 mg/dl). At that point, a marked clinical improvement was observed. Motor power in the right arm and leg was nearly completely restored and the MMSE score was 30. There has been no reported relapse of neurological symptoms during the 16 months of follow-up after discharge.
Discussion
The clinical and pathological findings suggested that the rapidly progressive dementia displayed in this patient with sarcoidosis was a direct result of PML. Our case report suggests that dual therapy with cidofovir and mirtazapine could be a viable therapeutic option for PML patients with sarcoidosis.
To date, there exist few reports of PML associated with sarcoidosis. In one study summarizing 58 non-HIV patients with PML, 9% of the patients had sarcoidosis as an underlying disease [2]. Whether the cause of coincidental sarcoidosis and PML is secondary to immunosuppressive treatment or a reflection of underlying immunological defect remains unclear. Although most of the reported patients with sarcoidosis were on immunosuppressive treatment such as oral corticosteroids or azathioprine [3, 4, 5], it could have been the first manifestation of sarcoidosis [6] or possibly have developed in patients with untreated sarcoidosis [7]. There are several explanations of pathogenesis for the development of PML in sarcoidosis. A state of anergy (poor response to antigens) and/or increased activity of regulatory T lymphocytes, commonly observed in patients with sarcoidosis may be the cause of PML [8]. Additionally, the shift in CD4/CD8-ratio due to a lack of JC virus-specific cytotoxic T cells may also induce the development of PML [4].
The diagnosis of PML in patients with sarcoidosis remains challenging. Initially, our case could also have been considered to be neurosarcoidosis due to the symptoms occurring during steroid dose tapering. Although the most common abnormality of neurosarcoidosis is involvement of the basal meninges that subsequently affect the cranial nerves, accumulation of granulomas in the brain can lead to progressive dementia [9]. Additionally, current imaging techniques often cannot distinguish PML from neurosarcoidosis. Neurosarcoidosis often presents with multiple supratentorial or infratentorial white matter lesions without meningeal involvement, which is similar to the lesions occurring in PML [9]. However, it is highly important to differentiate PML from neurosarcoidosis due to their different treatment requirements. Neurosarcoidosis is usually treated with steroid therapy, whereas steroid therapy would enhance JCV activity in PML. Therefore, we recommend that a brain biopsy or CSF JCV PCR be promptly performed in cases where rapidly progressive dementia is thought to be the result of neurosarcoidosis or PML.
The disease course of PML is generally known to be progressive and fatal. The median survival of patients without HIV infection is only a few months. Previous animal studies have shown that several therapeutic agents may be effective in the treatment of PML [10]. More recent case reports suggest that cidofovir and a 5-HT2A blocker could be effective against PML [3, 7]. Cidofovir is a nucleotide analogue, displaying effective anti-JCV activity in a mouse polyomavirus model [11]. The anti-depressant mirtazapine blocks a substantial number of 5-HT2A receptors that JCV employs to infect human glial cells [12]. In this case study, the ongoing neurological deterioration until the introduction of cidofovir and mirtazapine suggests that this therapeutic agent played a role in the patient's recovery. However, there exist case reports that did not show cidofovir to be effective in PML patients with sarcoidosis [4, 5,13]. All of these previous cases were initially treated with a high dose of intravenous methylprednisolone, due to a misdiagnosis of neurosarcoidosis or acute disseminated encephalomyelitis followed by further deterioration. They were later correctly diagnosed as having PML by brain biopsy. Although cidofovir was administered, all the patients died. Thus, we believe that PML should be considered in patients with sarcoidosis presenting with rapidly progressive dementia, and in such cases, the diagnosis must be confirmed before steroid therapy is initiated. Further studies are needed to determine the causal relationship, optimal dose and duration for treatment.
Disclosure Statement
The authors declare no financial conflicts of interest.
Acknowledgement
The authors thank Lee Farrand at Seoul National University for English editing.
References
- 1.Koralnik IJ. Progressive multifocal leukoencephalopathy revisited: has the disease outgrown its name? Ann Neurol. 2006;60:162–173. doi: 10.1002/ana.20933. [DOI] [PubMed] [Google Scholar]
- 2.Aksamit AJ. Review of progressive multifocal leukoencephalopathy and natalizumab. Neurologist. 2006;12:293–298. doi: 10.1097/01.nrl.0000250948.04681.96. [DOI] [PubMed] [Google Scholar]
- 3.Owczarczyk K, Hilker R, Brunn A, Hallek M, Rubbert A. Progressive multifocal leucoencephalopathy in a patient with sarcoidosis-successful treatment with cidofovir and mirtazapine. Rheumatology (Oxford) 2007;46:888–890. doi: 10.1093/rheumatology/kem049. [DOI] [PubMed] [Google Scholar]
- 4.Volker HU, Kraft K, Arnold E, Steinhoff S, Kolios G, Sommer S. Progressive multifocal leukoencephalopathy developing in advanced pulmonal sarcoidosis. Clin Neurol Neurosurg. 2007;109:624–630. doi: 10.1016/j.clineuro.2007.05.009. [DOI] [PubMed] [Google Scholar]
- 5.Granot R, Lawrence R, Barnett M, Masters L, Rodriguez M, Theocharous C, Pamphlett R, Hersch M. What lies beneath the tent? JC-virus cerebellar granule cell neuronopathy complicating sarcoidosis. J Clin Neurosci. 2009;16:1091–1092. doi: 10.1016/j.jocn.2008.07.091. [DOI] [PubMed] [Google Scholar]
- 6.De Raedt S, Lacor P, Michotte A, Flamez A, Ebinger G. Progressive multifocal leukoencephalopathy as first manifestation of sarcoidosis. Clin Neurol Neurosurg. 2008;110:186–189. doi: 10.1016/j.clineuro.2007.09.012. [DOI] [PubMed] [Google Scholar]
- 7.Yagi T, Hattori H, Ohira M, Nakamichi K, Takayama-Ito M, Saijo M, Shimizu T, Ito D, Takahashi K, Suzuki N. Progressive multifocal leukoencephalopathy developed in incomplete Heerfordt syndrome, a rare manifestation of sarcoidosis, without steroid therapy responding to cidofovir. Clin Neurol Neurosurg. 2010;112:153–156. doi: 10.1016/j.clineuro.2009.10.005. [DOI] [PubMed] [Google Scholar]
- 8.Miyara M, Amoura Z, Parizot C, Badoual C, Dorgham K, Trad S, Kambouchner M, Valeyre D, Chapelon-Abric C, Debre P, Piette JC, Gorochov G. The immune paradox of sarcoidosis and regulatory T cells. J Exp Med. 2006;203:359–370. doi: 10.1084/jem.20050648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nowak DA, Widenka DC. Neurosarcoidosis: a review of its intracranial manifestation. J Neurol. 2001;248:363–372. doi: 10.1007/s004150170175. [DOI] [PubMed] [Google Scholar]
- 10.Hartman EA, Huang D. Update on PML: lessons from the HIV uninfected and new insights in pathogenesis and treatment. Curr HIV/AIDS Rep. 2008;5:112–119. doi: 10.1007/s11904-008-0018-0. [DOI] [PubMed] [Google Scholar]
- 11.Andrei G, Snoeck R, Vandeputte M, DeClercq E. Activities of various compounds against murine and primate polyomaviruses. Antimicrob Agents Ch. 1997;41:587–593. doi: 10.1128/aac.41.3.587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Elphick GF, Querbes W, Jordan JA, Gee GV, Eash S, Manley K, Dugan A, Stanifer M, Bhatnagar A, Kroeze WK, Roth BL, Atwood WJ. The human polyomavirus, JCV, uses serotonin receptors to infect cells. Science. 2004;306:1380–1383. doi: 10.1126/science.1103492. [DOI] [PubMed] [Google Scholar]
- 13.Neeb L, Diekmann S, Blechschmidt C, Meisel H, Hofmann J, Harms L, Endres M. Infratentorial progressive multifocal leukencephalopathy in a patient with pulmonary sarcoidosis. J Neurol. 2009;256:1936–1938. doi: 10.1007/s00415-009-5265-5. [DOI] [PubMed] [Google Scholar]