Abstract
Signet ring cell carcinoma (SRCC) of the prostate is rare, with approximately 100 case reports to date. Here we report a very aggressive case of SRCC of the prostate in a Japanese man. The patient received estramustine, docetaxel, and carboplatin combination chemotherapy, followed by TS-1 and CPT-11 combination therapy. Unfortunately, the disease progressed, and he died of general metastatic disease treated over 16 month with systemic chemotherapy.
Key words: Signet ring cell carcinoma, Prostate, Chemotherapy
Introduction
Signet ring cell carcinoma (SRCC) of the prostate is rare and characterized by its unique histopathologic features and prostate-specific antigen (PSA) productivity, and it is considered a high-grade carcinoma with poor prognosis [1]. Here we report an aggressive case of SRCC of the prostate.
Case Report
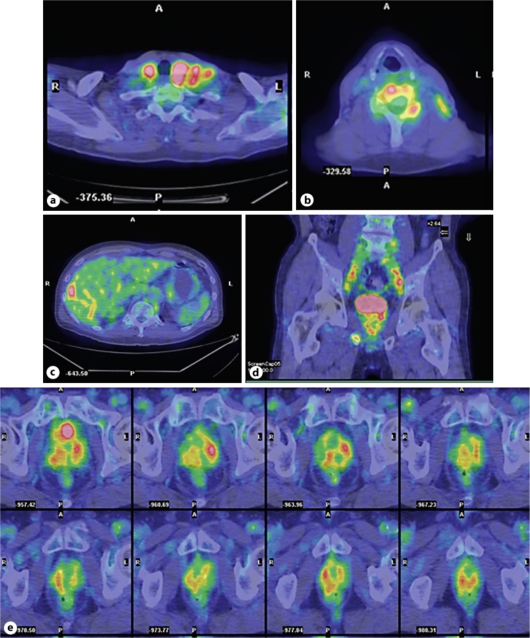
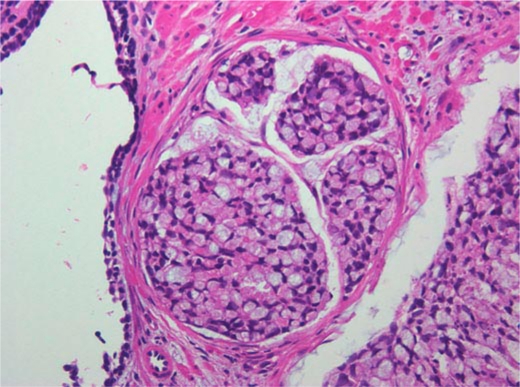
In May 2008, a 61-year old Japanese man diagnosed with left cervical lymphadenopathy visited Hirosaki University Hospital. A left neck lymph node biopsy was performed, and SRCC metastasis was diagnosed. Positron emission tomography CT (PET-CT) was performed and fluorodeoxyglucose (FDG) uptake was detected in the left neck, right lobe of liver, the cervical vertebrae (C5-C7), the right ischium, the pelvic lymph nodes and the prostate lesions (fig. 1). Although FDG uptake was recognized in thyroid, it was diagnosed as chronic thyroiditis as a result of close inspection. Gastrointestinal examination detected no abnormality and the patient was referred to our clinic in June 2008. Digital rectal examination revealed an enlarged and stony hard prostate. The serum PSA level was 0.19 ng/ml. Urethrocystoscopy revealed a normal bladder and prostatic urethra. We obtained 10 prostate samples by transrectal ultrasound-guided prostate biopsy. Histopathological examination revealed SRCC in all specimens (fig. 2).
Fig. 1.
PET-CT showed FDG uptake in the left neck (a), C5-7 (b), right lobe of liver (c), right ischium, pelvic lymph node (d) and prostate (e).
Fig. 2.
The microscopic finding of prostatic specimens. More than 50% of atypical cells were signet ring cells (HE stain, original magnification ×200).
PSA was negative for the carcinoma cells by immunohistochemistry. However, there were no responsible lesions other than prostate in spite of extensive general examinations. Finally, the patient was diagnosed as SRCC with a clinical stage of T3N2M2.
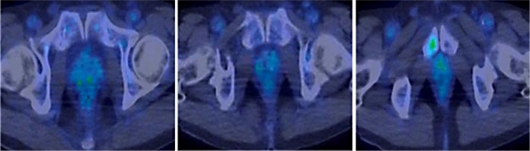
The patient received estramustine, docetaxel, and carboplatin chemotherapy (estramustine, 280 mg p.o./day; carboplatin, AUC [5] on a 28-day cycle; and docetaxel, 70 mg/m2 on a 28-day cycle) for high-grade prostate cancer [2, 3, 4]. After 2 courses of therapy, PET-CT revealed reductions in the prostate size as well as FDG uptake in the prostate and metastatic sites were observed (fig. 3). The patient received 2 additional courses of estramustine, docetaxel, and carboplatin chemotherapy, but liver metastasis progressed. Therefore, he received TS-1 and CPT-11 combination therapy (TS-1, 80 mg/m2 day 1-21 and CPT-11, 80 mg/m2 day 1 and 15, every 5 weeks), which is a second line chemotherapy for non-curatively resected gastrointestinal carcinoma [5]. He received 2 courses of the therapy, but his disease progressed. In October 2009, he died of the disseminated disease 16 months after his first appearance.
Fig. 3.
The image of PET-CT after 2 courses of estramustine, docetaxel, and carboplatin combined chemotherapy. After chemotherapy, FDG uptake and prostatic volume were extremely reduced.
Discussion
SRCC of the prostate is rare, with approximately 100 case reports [1]. The characteristic cytoplasmic clearing observed in SRCC of the prostrate is rarely mucicarminophilic, in contrast to that of the bladder, urachus, stomach, and other sites.
SRCC diagnosis requires that 25% or more of the tumor be composed of signet ring cells [6, 7]. Clinically, SRCC of the prostate is usually diagnosed in an advanced stage of disease through elevated PSA levels. However, some cases with SRCC have high carcinoembryonic antigen immunoreactivity, while PSA is negative [8].
In our case, more than half of the tumor consisted of signet ring cells. Tumor cells were immunohistochemically negative for Lens culinaris agglutinin (LCA) lectin. The patient's serum PSA was not elevated, and PSA immunostaining was negative. However, the present case did not have any responsible lesions for the disseminated disease other than prostate. Thus, we diagnosed him as SRCC of the prostate.
Some authors suggested that PSA may be absent, particularly in poorly differentiated prostate cancers. Yamamoto et al. [9] reported on 8 patients with clinically assessed metastatic prostate cancer, and their serum PSA levels were less than 10 ng/ml. Most of them had poorly differentiated or undifferentiated tumors with poor prognosis compared with the usual metastatic prostate cancer. They also noted that androgen deprivation therapy was not effective in these cases and therefore that systemic chemotherapy and irradiation therapy should be recommended [9].
In our case, estramustine, docetaxel, and carboplatin chemotherapy, a standard regimen for high-grade prostate cancer, was given. The initial 2 courses of therapy produced a partial response, but liver metastasis occurred. Second-line chemotherapy was subsequently initiated according to an alternative regimen for non-curatively resected gastrointestinal cancer. However, the patient's disease progressed and he died of the disease.
To our knowledge, this is the first report of SRCC of the prostate that was treated with systemic chemotherapy from the initiation of the treatment. In this case, estramustine, docetaxel, and carboplatin combination chemotherapy were partially effective, indicating their potential utility in future treatment.
References
- 1.Warner JN, Nakamura LY, Pacelli A, Humphreys MR, Castle EP. Primary signet ring cell carcinoma of the prostate. Mayo Clin Proc. 2010;85:1130–1136. doi: 10.4065/mcp.2010.0463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Oh WK, Halabi S, Kelly WK, Werner C, Godley PA, Vogelzang NJ, Small EJ. A phase II study of estramustine, docetaxel, and carboplatin with granulocyte-colony-stimulating factor support in patients with hormone-refractory prostate carcinoma: Cancer and Leukemia Group B 99813. Cancer. 2003;98:2592–2598. doi: 10.1002/cncr.11829. [DOI] [PubMed] [Google Scholar]
- 3.Oh WK, Hagmann E, Manola J, George DJ, Gilligan TD, Jacobson JO, Smith MR, Kaufman DS, Kantoff PW. A phase I study of estramustine, weekly docetaxel, and carboplatin chemotherapy in patients with hormone-refractory prostate cancer. Clin Cancer Res. 2005;11:284–289. [PubMed] [Google Scholar]
- 4.Oh WK. High-risk localized prostate cancer: integrating chemotherapy. Oncologist. 2005;10(suppl 2):18–22. doi: 10.1634/theoncologist.10-90002-18. [DOI] [PubMed] [Google Scholar]
- 5.Kawamura S, Yamagishi D, Tei M, Sumi Y, Shimada E, Okumura S. A case of non-curatively resected gastric cancer successfully treated over 17 months with TS-1 and irinotecan combination therapy. Gan To Kagaku Ryoho. 2006;33:1309–1311. [PubMed] [Google Scholar]
- 6.Randolph TL, Amin MB, Ro JY, Ayala AG. Histologic variants of adenocarcinoma and other carcinomas of prostate: pathologic criteria and clinical significance. Mod Pathol. 1997;10:612–629. [PubMed] [Google Scholar]
- 7.Grignon DJ. Unusual subtypes of prostate cancer. Mod Pathol. 2004;17:316–327. doi: 10.1038/modpathol.3800052. [DOI] [PubMed] [Google Scholar]
- 8.Remmele W, Weber A, Harding P. Primary signet-ring cell carcinoma of the prostate. Hum Pathol. 1988;19:478–480. doi: 10.1016/s0046-8177(88)80501-x. [DOI] [PubMed] [Google Scholar]
- 9.Yamamoto S, Ito T, Akiyama A, Aizawa T, Miki M, Tachibana M. M1 prostate cancer with a serum level of prostate-specific antigen less than 10 ng/ml. Int J Urol. 2001;8:374–379. doi: 10.1046/j.1442-2042.2001.00316.x. [DOI] [PubMed] [Google Scholar]