Abstract
Laparoscopic splenectomy has been performed with an average of 4 trocars since the early 1990s, and it has become the gold standard for elective splenectomy. Recently, single-port laparoscopic (SPL) surgery has emerged as an alternative to multiport laparoscopy, but SPL splenectomy in a patient with idiopathic thrombocytopenic purpura (ITP) has not been reported to date in Saudi Arabia or the region. A case report of SPL splenectomy in a patient with ITP is briefly described along with the surgical technique needed for such a procedure. The patient was an otherwise healthy 24-year-old female woman with medically refractory ITP and a platelet count of 2200. A standard splenectomy was performed using a SPL technique. The patient did well intraoperatively and postoperatively, was happy with her incision, and was discharged home with no complications 3 days after the procedure. In conclusion, SPL splenectomy is feasible in select patients and may provide a less painful, cosmetically better alternative.
Laparoscopic splenectomy is the gold standard approach for normal or slightly enlarged spleens.1 Conventional laparoscopic splenectomy has been performed since the early 1990s and requires on an average 4 trocars (5-12 mm).1,2 The current trend is to improve the cosmetic outcome when applying minimally invasive procedures if feasible, and single-port surgery is one of the options to achieve this goal. Single-port laparoscopic (SPL) surgery for splenectomy has not been reported in Saudi Arabia or the region but has been safely applied to the spleen in other countries.3 This case report describes the use of an SPL technique for splenectomy in a patient with idiopathic thrombocytopenic purpura (ITP).
CASE
A 24-year-old female woman was diagnosed with refractory ITP. Her platelet count was 2200 per μL despite adequate medical therapy. The patient had no previous surgery, and preoperative ultrasound revealed a normal-sized spleen. Standard splenectomy using a SPL technique was offered. The procedure was explained in full to the patient, and written informed consent was obtained.
The patient was placed in the supine position with extra care being taken to provide patient support and strapping to allow safe changes in operative table movements. A 20-mm supraumbilical incision was made and was used to gain access to the peritoneal cavity. A multiinstrument flexible single-incision port (SILS) was used (Figure 1). The port was designed to hold 3 trocars as well as an insufflation port that can also accommodate a fourth trocar. Pneumoperitoneum was initiated using CO2 gas at 15 mm Hg. After exploration of the abdominal cavity with a flexible-tip 10-mm HD scope through a 12-mm trocar, three 5-mm trocars were inserted through the SILS port. We used the side port of one of the 5-mm trocars for gas insufflation. This allowed us to have 3 working instruments and the camera at the same time. A 5-mm articulated grasper, a conventional 5-mm graspers, as well as a 5-mm vessel-sealing instrument were used. Using these instruments, it was possible to mobilize the splenic colon flexure. The next step was dividing the short gastric vessels; the table was tilted in many directions for optimal exposure and to take advantage of gravity. The splenorenal attachments were also freed. The lateral attachment of the spleen was kept to be done last and was divided only after controlling the hilum. This kept the spleen suspended and allowed natural traction.
Figure 1.
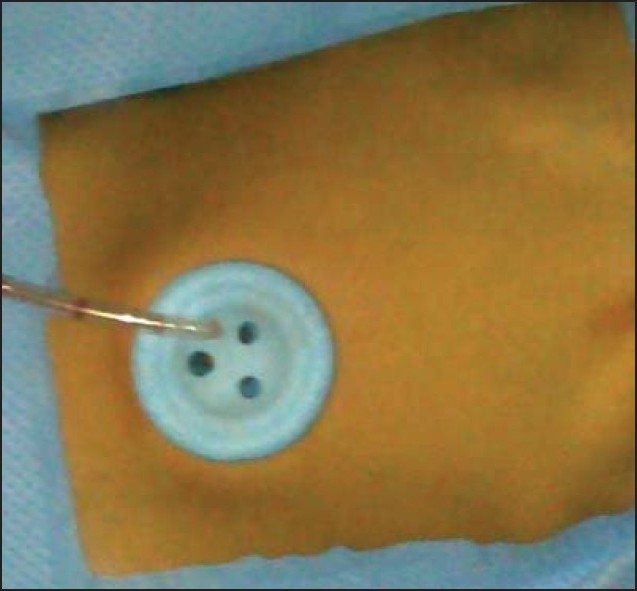
Multiple Instrument Access Port.
Once the spleen was completely mobile except for the lateral attachment, the flexible 10-mm scope was retrieved and changed to a 30° 5-mm scope introduced through the 5-mm trocar; this allowed us to insert the vascular stapler through the 12-mm port to control the hilum. The lateral attachment of the spleen was scheduled to be done at a later stage, as it provided natural traction of the spleen and allowed better exposure of the Hilum. A stapler with a 60-mm white cartridge was used to control the splenic hilum. The lateral attachment was then divided, and the spleen was completely free. After checking for homeostasis, a 15-mm specimen retrieval pouch was inserted, replacing the 12-mm trocar. The spleen was placed in the bag. The bag was pulled up to the umbilical incision, and the spleen was morcellated and retrieved. The operative time was 180 minutes, with minimal blood loss.
The patient did well intraoperatively and postoperatively, was satisfied with her incision, and was discharged home with no complications 3 days after the procedure. The patient was found to be doing well when she reported for follow-up 2 weeks later.
DISCUSSION
Previous reports showed that SILS for splenectomy is feasible and safe.3,4 The aim of using the SILS technique was to reduce abdominal wound size and improve cosmetic outcome. Our report illustrates the feasibility of this approach, which was implemented at a tertiary care center in Saudi Arabia, and describes the technical challenges involved. We found that liberal movements of the table and the use of a flexible-tip scope and articulating instrumentation, as well as leaving the lateral attachment of the spleen to be done at the end of the operation, made this procedure possible. The limitations of this approach are clearly the necessity to go through the learning curve and the lack of adequate familiarity with the new instruments. It was slightly difficult to place the stapler, a vessel-sealing system can be used to control the hilum, if the surgeon stays close to the spleen and the vessels are less than 6 mm in size. We strongly recommend a 5-mm flexible scope to free up the 12-mm trocar for other instruments like a 10-mm vessel-sealing system, which, in our opinion, would have made the operation much easier. In this case, we used the stapler as we are more familiar with this technique. Insertion of the specimen retrieval pouch and extraction of the spleen through the umbilicus did not imply any difficulty. The application of this technique could be extended to other classic minimally invasive procedures. It may also serve as a superior technique to be used when multiorgan resections are needed, to avoid multiple incisions. Further studies are needed to prove the usefulness of this technique in achieving a quicker recovery and better patient satisfaction.
In conclusion, SPL splenectomy is feasible in select patients and may enable patients to achieve quicker recovery and better cosmetic results.
REFERENCES
- 1.Park A, Targarona EM, Trias M. Laparoscopic surgery of the spleen: State of the art. Langenbecks Arch Surg. 2001;386:230–9. doi: 10.1007/s004230100222. [DOI] [PubMed] [Google Scholar]
- 2.Habermalz B, Sauerland S, Decker G, Delaitre B, Gigot JF, Leandros E, et al. Laparoscopic splenectomy: The clinical practice guidelines of the European Association for Endoscopic Surgery (EAES) Surg Endosc. 2008;22:821–48. doi: 10.1007/s00464-007-9735-5. [DOI] [PubMed] [Google Scholar]
- 3.Targarona EM, Balague C, Martinez C, Pallares L, Estalella L, Trias M. Single-port access: A feasible alternative to conventional laparoscopic splenectomy. Surg Innov. 2009;16:348–52. doi: 10.1177/1553350609353765. [DOI] [PubMed] [Google Scholar]
- 4.Malladi P, Hungness E, Nagle A. Single access laparoscopic splenectomy. JSLS. 2009;13:601–4. doi: 10.4293/108680809X12589999538039. [DOI] [PMC free article] [PubMed] [Google Scholar]


