Abstract
Objective:
To evaluate our preliminary experience with interventional sialendoscopy for the diagnosis and treatment of juvenile recurrent parotitis (JRP).
Materials and Methods:
Three consecutive pediatric patients with JRP who underwent interventional sialendoscopy were identified. Interventional sialendoscopy consisted of serial dilation of the Stenson's duct, endoscopy of the ductal system and saline irrigation followed by instillation of triamcinolone acetate. Clinical, demographic, procedure-related data and complications were documented. End points of the study were technical success, defined as completion of the procedure, subjective improvement in symptoms as indicated by the patients or their parents and assessment of safety in terms of complications.
Results:
Three male patients with a mean age of 9 years (range 6–11 years) underwent interventional sialendoscopy for JRP. Endoscopic findings included a blanched stenotic duct with intraductal debris in those who were symptomatic. Technical success was 100%. The mean number of episodes of JRP in the year prior to presenting to our service among the three patients was 5 (range 4–6 per year). There were no new episodes of JRP reported at the last follow-up. There were no major complications.
Conclusion:
Our preliminary experience concurs with the current literature and suggests that interventional sialendoscopy is effective for the management of JRP and can be considered for patients who fail conservative medical management.
KEY WORDS: Juvenile parotitis, recurrent parotitis, salivary endoscopy, sialendoscopy
INTRODUCTION
Juvenile recurrent parotitis (JRP) or recurrent parotitis of childhood is a well-recognized salivary gland disorder and is the second most common salivary disease in children. The clinical presentation of JRP involves recurrent, non-obstructive, non-suppurative swelling of either one or both of the parotid glands.[1] The exact etiology of this disease is unknown.[1,2] The diagnosis of JRP is based on the clinical presentation, and is one of exclusion of neoplastic, inflammatory and infectious etiologies. The treatment for JRP ranges from medical management with warm compresses, sialogogues and antibiotic therapy to surgical management with a superficial parotidectomy and facial nerve dissection for patients resistant to medical management.[3] Other treatments investigated for JRP include parotid duct ligation or tympanic neurectomy[4] and sialography.[5] These traditional treatment options have found to have limited effectiveness or carry a high morbidity associated with them. More recently, interventional sialendoscopy has been proposed as a treatment option for JRP. Our objective is to present our preliminary experience and a relevant literature review on sialendoscopic management of JRP and to discuss the technical challenges associated with the endoscopic management of JRP.
MATERIALS AND METHODS
During October 2008 to November 2009, three children with JRP failing conservative medical management were referred to the LSU Department of Otolaryngology Head Neck Surgery at the Children's Hospital of New Orleans, Louisiana. An informed consent was obtained from the parents of the patients for management with interventional sialendoscopy. Before sialendoscopy, the children had received medical management only with no prior procedures having been performed for the treatment of JRP. Indication for endoscopic treatment was at least two episodes of parotid swelling within 6 months despite treatment with antibiotics. The procedure was performed in a non-acute setting after resolution of the most recent episode of parotitis. Interventional sialendoscopy was performed under general anesthesia on the affected gland(s) only. Empiric sialendoscopy for asymptomatic glands was not performed.
Surgical Procedure
Sialendoscopy is a relatively new procedure introduced by Marchal et al.[6] Sialendoscopy is a minimally invasive procedure that allows endoscopic visualization of the salivary ductal system and permits diagnosis and treatment of inflammatory and obstructive pathology of the ductal system thus providing an alternative to open surgery and its related complications.[7] There are multiple endoscopes available, ranging in external diameter from 0.8 to 1.6 mm [Figure 1a and b]. Sialendoscopy is performed in the operating room under general anesthesia. The surgical procedure can be divided into the following major steps: exposure, access to the salivary ductal system, endoscopy of the salivary ductal system and intervention.
Figure 1.
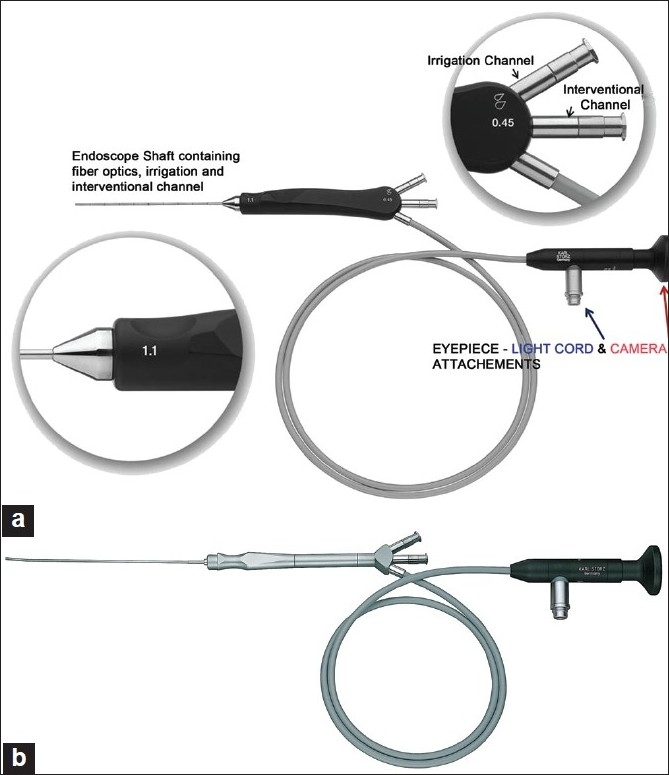
(a) Erlangen 1.1 mm “all-in-one” sialendoscope. (b) 1.3 mm marchal “all-in-one” sialendoscope (Photographs courtesy Karl Storz, Germany)
Exposure: Nasotracheal intubation is preferred although not mandatory, as this allows a more complete access to the oral cavity. The oral cavity can be kept open using splints.
Access: The identification and dilation of the parotid duct opening is the rate-limiting step of this procedure. Identification can be improved using optical magnification. In difficult cases, where the opening of the papilla cannot be visualized, application of methylene blue has been shown to improve visualization of the papilla.[8] The dilation of the papilla is most commonly performed using a set of specialized ductal dilators of increasing diameter (Marchal dilator system, Karl Storz, Tuttlingen, Germany) [Figure 2]. These dilators start from a No. 0000 to a maximum size of No. 8. Usually, for pediatric sialendoscopy, dilation up to No. 3 or 4 is adequate to introduce the 1.1 mm Erlangen or 1.3 mm Marchal interventional sialendoscope. Other methods for dilation of the papilla that have been described include the use of guide wires and bougies of increasing diameter via the Seldinger technique, threading the sialendoscope over a guide wire[9] and also use of a papillotomy to facilitate introduction of the sialendoscope. The serial dilation method is preferred as it is atraumatic and allows precise dilation of the duct that will allow introduction of the endoscope but prevent backflow of saline that is infused to maintain an adequate surgical view.
Figure 2.
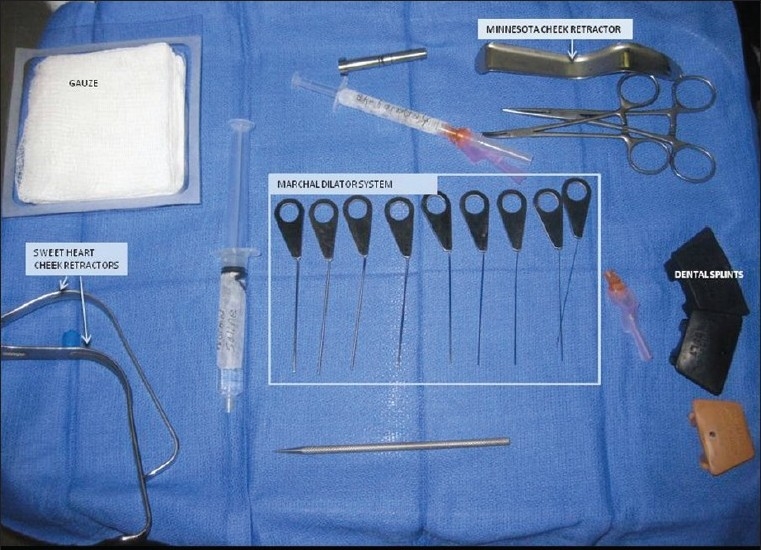
Dilator set (Marchal dilator system, Karl Storz, Tuttlingen, Germany)
Endoscopy: Salivary endoscopy is performed to visualize the main duct looking for debris, areas of stenosis and obstructive sialoliths. A constant infusion of saline helps maintain a surgical endoscopic view. In parotid sialendoscopy, the masseter muscle can often create a turn within the duct that is difficult to navigate and has been termed the “masseteric bend.” Pinching the cheek between the thumb and index finger with forward traction and using the other fingers of the hand to manipulate the salivary gland, it is often possible to straighten the duct and navigate the “masseteric bend.” A complete endoscopy includes visualization of the main duct as well as secondary and tertiary ductal systems [Figure 3].
Figure 3.
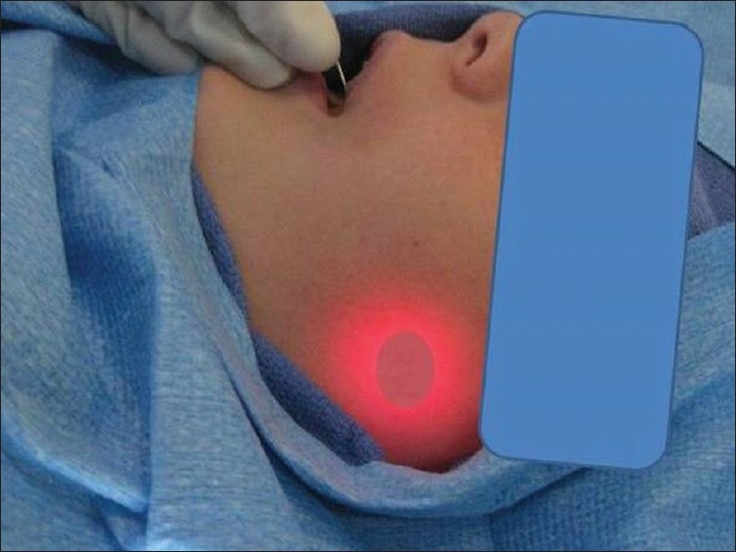
Parotid sialendoscopy with transillumination of the tip of the scope within the parotid glandular system
Intervention: Interventional sialendoscopes allow the introduction of pharmacological agents as well as specialized tools such as wire baskets for stone extraction, laser fibers for stone fulguration or release of ductal stenosis and hand-held micro burr. Specialized balloon dilators for management of ductal stenosis are also available. The surgical intervention used for management of JRP included serial dilation of the parotid papilla using serial dilator probes. This was followed by a sialendoscopy for visualization of Stenson's duct, robust irrigation with normal saline and instillation of Kenalog (triamcinolone acetate 40 mg diluted in 5 ml of normal saline). A papillotomy was performed for access or stenosis of the papilla if necessary. The papillotomy was not routinely marsupialized to the buccal mucosa. Patients were counseled to expect a swelling of the salivary gland. The patients were discharged home the same day with instructions for the use of parotid massage and sialogogues. Pain medication was prescribed, but no post-operative antibiotics or steroids were prescribed. Initial follow-up was conducted 2 weeks after surgery to ensure adequate salivary flow and rule out iatrogenic stenosis of the papilla. Follow-up assessments of subjective symptom control were performed by telephone.
RESULTS
Three male patients with a mean age of 9 years (range 6–11 years) were identified with a diagnosis of JRP that were referred for sialendoscopy. All three patients had unilateral symptoms. Of the three patients with unilateral gland involvement, two patients had left-sided symptoms and one had right-sided involvement. The mean number of episodes of JRP in the year prior to presenting to our service among the three patients was 5 (range 4–6 per year).
Interventional sialendoscopy was technically possible in all three patients and, consequently, the technical success was 100% (3/3). Interventional sialendoscopes with diameters of 0.8, 1.1 and 1.3 mm were used. Endoscopic findings included a blanched stenotic duct with intraductal debris in symptomatic patients (2/3; 66%) [Figure 4]. In the third patient, the duct mucosa appeared normal without the presence of intraductal debris [Figure 5]. In all cases, parents and patients were satisfied with results, and no new episodes of parotid swelling were reported at the last follow-up (mean 9 months, range 3–16 months).
Figure 4.
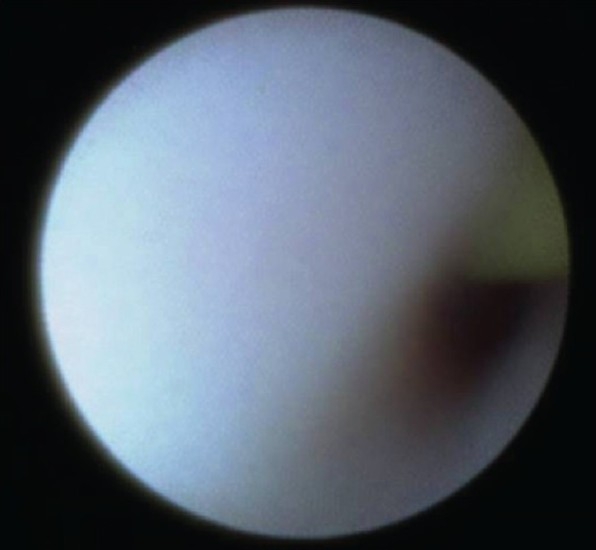
Sialendoscopic view showing a blanched duct with a guide wire in the ductal lumen
Figure 5.

Sialendoscopic view of a normal-appearing duct
Complications were minor, including an acute masseteric bend that posed a challenge for navigating the scope in one patient. Proximal ductal stenosis at the papilla was observed in two patients, of which one patient required marsupialization of Stenson's duct. There were no major procedure-related complications.
All patients were discharged on the same day. On follow-up, none of the patients reported new episodes of parotitis, with healed papillotomy incisions and good salivary flow.
DISCUSSION
In 2004, Nahlieli et al. proposed an endoscopic technique for both the diagnosis and the treatment of JRP.[1] Their long-term experience with the endoscopic diagnosis and treatment of JRP has encouraging results.[10] Diagnosis was achieved by clinical history of two episodes of parotid swelling in a 12-month period, physical examination as well as ultrasound. Bilateral sialography of the parotid ducts was also performed in all patients for primary diagnosis. Patients in this study underwent bilateral sialendoscopy of Stensen's ducts regardless of laterality of symptoms, and lavage with 60 cc of normal saline was performed. All patients were then infused with 100 mg hydrocortisone through the sialendoscope. These patients received 25 mg/kg of intravenous amoxicillin–clavulanic acid and intravenous dexamethosone post-operatively. Results over the course of 14-year study were promising, with only nine of 70 patients having one subsequent episode of parotid swelling after treatment and only five requiring a repeat endoscopic treatment. One patient had unresolved repeated parotid swelling after repeat sialendoscopy. Follow-up ranged from 6 to 36 months.
Since the initial description of this method, one other study has documented a separate experience with interventional sialendoscopy involving patients with JRP. Quenin et al. reported a series of 10 patients in 2008.[4] In this study, patients were diagnosed via clinical history, physical examination and an ultrasound. Indication for an endoscopic procedure in this study involved two episodes of parotid swelling in a 6-month period. Initial sialography was not performed. Quenin et al. performed endoscopic intervention on the affected side only with saline and steroid irrigation. Patients were hospitalized for 24 h and received post-operative amoxicillin–clavulanic acid and prednisolone for 48 h. This study reported the need for only one repeat endoscopic procedure out of 10 patients with follow-up ranging from 2 to 24 months.
Our experience with sialendoscopy has also had promising results with technical success and subjective improvement in symptoms in all patients at a mean follow-up of 9 months (range 3–16 months). We feel that although ultrasound is the imaging study of choice, clinical history and physical examination are sufficient to provide an indication for endoscopic treatment, as recent studies have shown sialendoscopy to be a sufficient tool for the diagnosis of JRP.[4] In the event that sialolithiasis is misdiagnosed as JRP, salivary stones can also be diagnosed and managed with sialendoscopy.[6] Our study differed from previous reports in that all of our patients were able to undergo same day surgery and leave the hospital without antibiotics or steroid therapy. None of the patients had a diagnostic sialogram, which can confound results as it has been reported for the management of JRP.[5] We directed our intervention to only symptomatic glands akin to Quenin et al.[11] All three patients have remained free from parotid swelling after sialendoscopy. However, long-term follow-up data is needed to confirm these preliminary observations, which are encouraging.
There appears to be a learning curve with the use of sialendoscope. From our own experience, we feel that pediatric sialendoscopy is more challenging and, if possible, should be incorporated into one's practice after developing a comfort level and an initial experience of sialendoscopy in an adult population. However, this may not always be feasible in exclusively pediatric practices. Consequently, training in sialendoscopy and collaboration with someone experienced in sialendoscopy can help bridge these difficulties.
Endoscopic findings in our study were consistent with the previous literature on the subject, including a white, avascular appearance of the ductal layer of Stenson's duct with intraductal debris present.[10] One patient in our series had normal endoscopic findings. Interestingly, this patient had the last episode of parotitis 6 months prior to the procedure as opposed to the other two patients who had episodes of JRP within 3–4 months of the procedure. We hypothesize that it may be possible that normal endoscopic findings in patients with documented JRP can help to predict the incidence of future episodes or resolution of this self-limiting disease process. However, accurate long-term prospective data would be essential to confirm this hypothesis.
Some studies have shown that the parotid system may be approximately the same size in children as in adults,[12] and an ideal scope size has not been recommended for the management of JRP to date. However, our experience and previous studies report that the duct of a patient with JRP is likely to be stenotic, which would therefore call for a smaller endoscope to be used. Faure et al. reported that a 1.3-mm sialendoscope can be used without difficulty for diagnostic sialendoscopy.[13] However, we found that the 1.3-mm sialendoscope was technically more challenging to navigate as compared with the 0.8 and 1.1 mm endoscope. This may be due to the fact that we are treating a patient with diseased and stenotic ductal systems associated with JRP. The limitation of our observations is the small sample size and also not having the resources to use scopes of differing diameters in each case. It would seem likely that having a range of scopes with varying interventional capabilities would be of value in performing successful sialendoscopy (0.8 and 1.1 scopes for endoscopy in small diameter/stenotic ducts) and also managing endoscopic removal of debris using wire baskets (1.1 and 1.3 mm scopes).
CONCLUSION
Sialendoscopy is an excellent tool for managing non-neoplastic disorders of the salivary glands. To date, it has been widely reported for its use in the management of sialolithiasis.[14] However, its use for other indications such as for the management of JRP is still evolving. Our study concurs with current evidence to suggest that sialendoscopy is a safe and effective intervention with low morbidity and few complications for the management of JRP. Prospective multicenter studies will be required to define the utility of this intervention and to develop future clinical protocols.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Nahlieli O, Shacham R, Shlesinger M, Eliav E. Juvenile recurrent parotitis: a new method of diagnosis and treatment. Pediatrics. 2004;114:9–12. doi: 10.1542/peds.114.1.9. [DOI] [PubMed] [Google Scholar]
- 2.Konno A, Ito E. A study on the pathogenesis of recurrent parotitis in childhood. Ann Otol Rhinol Laryngol Suppl. 1979;88:1–20. doi: 10.1177/00034894790886s301. [DOI] [PubMed] [Google Scholar]
- 3.Sadeghi N, Black MJ, Frenkiel S. Parotidectomy for the treatment of chronic recurrent parotitis. J Otolaryngol. 1996;25:305–7. [PubMed] [Google Scholar]
- 4.Motamed M, Laugharne D, Bradley PJ. Management of chronic parotitis: A review. J Laryngol Otol. 2003;117:521–6. doi: 10.1258/002221503322112923. [DOI] [PubMed] [Google Scholar]
- 5.Galili D, Marmary Y. Juvenile recurrent parotitis: Clinicoradiologic follow-up study and the beneficial effect of sialography. Oral Surg Oral Med Oral Pathol. 1986;61:550–6. doi: 10.1016/0030-4220(86)90091-5. [DOI] [PubMed] [Google Scholar]
- 6.Marchal F. The Endoscopic Approach to Salivary Gland Ductal Pathologies. Tuttlingen, Germany: Endo-Publishing; 2003. [Google Scholar]
- 7.Walvekar RR, Bomeli SR, Carrau RL, Schaitkin B. Combined approach technique for the management of large salivary stones. Laryngoscope. 2009;119:1125–9. doi: 10.1002/lary.20203. [DOI] [PubMed] [Google Scholar]
- 8.Luers JC, Vent J, Beutner D. Methylene blue for easy and safe detection of salivary duct papilla in sialendoscopy. Otolaryngol Head Neck Surg. 2008;139:466–7. doi: 10.1016/j.otohns.2008.05.023. [DOI] [PubMed] [Google Scholar]
- 9.Chossegros C, Guyot L, Richard O, Barki G, Marchal F. A technical improvement in sialendoscopy to enter the salivary ducts. Laryngoscope. 2006;116:842–4. doi: 10.1097/01.mlg.0000214665.74330.96. [DOI] [PubMed] [Google Scholar]
- 10.Shacham R, Droma EB, London D, Bar T, Nahlieli O. Long-term experience with endoscopic diagnosis and treatment of juvenile recurrent parotitis. J Oral Maxillofac Surg. 2009;67:162–7. doi: 10.1016/j.joms.2008.09.027. [DOI] [PubMed] [Google Scholar]
- 11.Quenin S, Plouin-Gaudon I, Marchal F, Froehlich P, Disant F, Faure F. Juvenile recurrent parotitis: Sialendoscopic approach. Arch Otolaryngol Head Neck Surg. 2008;134:715–9. doi: 10.1001/archotol.134.7.715. [DOI] [PubMed] [Google Scholar]
- 12.Faure F, Querin S, Dulguerov P, Froehlich P, Disant F, Marchal F. Pediatric salivary gland obstructive swelling: Sialendoscopic approach. Laryngoscope. 2007;117:1364–7. doi: 10.1097/MLG.0b013e318068657c. [DOI] [PubMed] [Google Scholar]
- 13.Faure F, Froehlich P, Marchal F. Paediatric sialendoscopy. Curr Opin Otolaryngol Head Neck Surg. 2008;16:60–3. doi: 10.1097/MOO.0b013e3282f45fe1. [DOI] [PubMed] [Google Scholar]
- 14.Marchal F, Becker M, Dulguerov P, Lehmann W. Interventional sialendoscopy. Laryngoscope. 2000;110:318–20. doi: 10.1097/00005537-200002010-00026. [DOI] [PubMed] [Google Scholar]


