Abstract
Over the years Consultation-Liaison (C-L) psychiatry has contributed significantly to the growth of the psychiatry and has brought psychiatry very close to the advances in the medicine. It has also led to changes in the medical education and in the providing comprehensive management to the physically ill. In India, although the General Hospital Psychiatric units were established in 1930s, C-L Psychiatry has never been the main focus of training and research. Hence there is an urgent need to improve C-L Psychiatry services and training to provide best and optimal care to the patients and provide best education to the trainees.
Keywords: Consultation, liaison, psychosomatic, India
“Consultation-Liaison Psychiatry provides a fit vantage point for watching the changes that permit prediction of future directions in psychiatry as a medical discipline. The kind of psychiatry that the consultants practice and the type of training, skills, and professional attitudes that their work requires represent a model that is likely to prevail in psychiatry in the coming years”.[1]
INTRODUCTION
Consultation-liaison (C-L) psychiatry as a subspecialty has been defined as the area of clinical psychiatry that encompasses clinical, teaching and research activities of psychiatrists and allied mental health professionals in the non-psychiatric divisions of a general hospital.[1] C-L Psychiatry is derived conceptually from the old tradition, which advocates a ceaseless dynamic interaction between mind and body. It has brought psychiatry out of the mental asylums to the general hospitals and has also contributed significantly to the reduction of stigma that follows mental illness not only among members of the public but within the medical professionals and establishments also. Over the years C-L Psychiatry has contributed significantly to the growth of the psychiatry and has brought psychiatry very close to the advances in the medicine. It has also led to changes in the medical education and in the providing comprehensive management to the physically ill.
UNDERSTANDING THE TERM CONSULTATION-LIAISON
According to Lipowski, the designation “Consultation-Liaison” reflects two interrelated roles of the consultants. “Consultation” refers to the provision of expert opinion about the diagnosis and advice on management regarding a patient's mental state and behavior at the request of another health professional. The term “Liaison” refers to linking up of groups for the purpose of effective collaboration. In the context of current C-L Psychiatry, liaison involves interpretation and mediation i.e., the consultant psychiatrist mediates between patients and members of the clinical team and between mental health and other health professionals, respectively.[1–4] Further the consultation and liaison are mutually complementary. A consultation encompass three interlocked foci i.e., the patient, the consultee, and the therapeutic team. Hence for consultation to be most effective the consultant psychiatrist need to have personal contact with both the patient (including his family) and those taking care of him.[1]
However it, is important to understand the differences between the terms C-L Psychiatry and “Psychosomatic Medicine”. Psychosomatic medicine is conceptualized as a non-clinical discipline that is concerned with ideas such as “the interplay of biological and psychosocial factors in the development, course and outcome of all diseases.” In fact, the idea of psychological factors play an important role in the etiology of various physical disorders emerged from practice and theory of psychodynamic principles.[5] Hence, some authors consider C-L Psychiatry as the practical/clinical arm or an applied form of psychosomatic medicine.[6,7] The basic assumption of C-L Psychiatry is to integrate the information so as to provide optimal health care, which is sensitive to people's needs, mindful of prevention, and economically sound.[1]
HISTORY OF GENERAL HOSPITAL PSYCHIATRIC UNITS, POSTGRADUATE TRAINING AND C-L PSYCHIATRY IN INDIA
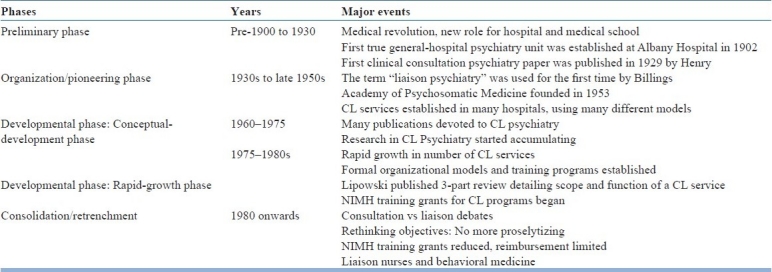
Prior to 1930, mental health services in this country were confined to the mental hospitals. The C-L Psychiatry as a subspecialty started in 1930s with the establishment of general hospital psychiatric units (GHPUs). Dr Girindra Shekhar at R. G. Kar Medical College and Hospital, Calcutta started the first GHPU in 1933.[8] When one looks at this beginning, it can be said that we were not far behind United States, were the first viable general hospital psychiatric unit was opened in the Albany Hospital in 1902 by JM Mosher to bring psychiatrists into proximity with non-psychiatrists for training purposes and to provide psychiatric treatment that would favorably compare with the quality of care offered to medical patients. This effort is considered to be a forerunner of the later med-psych unit.[9] In the context of history of C-L Psychiatry [Table 1],[10] C-L Psychiatry made a beginning in India when it was in the Organization/Pioneering phase in other parts of the world.
Table 1.
Phases and history of Consultation-Liaison Psychiatry (adapted with permission)[10]
Unfortunately, initially establishment of GHPU in India was faced with strong resistance from the medical personnel and health administrators, who did not think beyond asylum concept of mental illness management. Due to this, till 1960 there were few GHPUs that were initially established in collaboration with Department of Neurology and were often called as neuropsychiatric clinics. However, 1960s saw a major rise in number of GHPUs and by late 60s-early 70s there were 90 GHPUs.[11] Some of these units also started running the residency training programs. All India Institute of Medical Sciences was the first GHPU unit to start postgraduate psychiatric training in 1962 and the first batch of post-graduate students passed out in 1964.[12]
Over the years GHPUs became popular and were found to be more accessible than the custodial care. With a firm footing in the general hospital these GHPUs also started providing C-L Psychiatry services in which psychiatrists showed their knowledge and skills in the management of neurotic and psychosomatic disorders. When one compares this growth of C-L Psychiatry in India with worldwide development [Table 1], the rapid growth of C-L Psychiatry services in India coincided with that of development of the subspecialty in other parts of the world. In a survey of postgraduate training centres in India done in mid eighties, it was reported that 75% of the postgraduate training centres were in the general hospital setting. Although this survey did not assess the functioning of C-L Psychiatry services but pointed out that there was indifference to the psychosomatic rounds.[13] A National workshop on general hospital psychiatry was held in 1984 in Chandigarh and a series of articles were published in Indian Journal of Psychiatry in 1984 after the national workshop and with respect to post graduate training it was pointed out that “A workable knowledge of psychiatry subspecialties like Child psychiatry, mental retardation, psychotherapy, alcoholism, drug dependence and psychogeriatric is advisable. Familiarity with psychosomatic medicine and liaison psychiatry is advisable”[14] However it was pointed out that GHPUs should make efforts to organize suitable training programmes to provide training in liaison psychiatry, psychosomatic medicine and organic brain disorders.[14]
Over the years general hospital psychiatry became more popular and with the exception of few centres postgraduate psychiatry training in India is now more or less confined to the general hospitals. As per recent data of Medical Council of India, 112 Centres are providing postgraduate training in psychiatry and 246 MDs are awarded every year. Of these 112 centres, 109 are in the medical colleges or postgraduate institutes in a general hospital setting. Every year 124 candidates are awarded the degree of Diploma in Psychological Medicine by 55 centres; again 52 of these centres are in general hospital setting.[15]
Although most of the psychiatry training in last 50 years has been provided in the general hospital psychiatric units in India, the C-L Psychiatry has never been the focus. Although Indian Psychiatric Society has made long strides in improving the psychiatry training in India and providing clinical care to general public, somehow, C-L Psychiatry has never been the focus. Over the years Indian Psychiatric Society has constituted specialty sections and task forces for various sub specialties; somehow C-L Psychiatry has never received a sub-specialty status. It is quite possible that C-L Psychiatry has always being considered as part of general adult psychiatry and it is presumed that all the training centres are providing adequate training.
In this context, Indian psychiatry has lagged behind many of the Western countries. In 2003, C-L Psychiatry was given the accredited subspecialty status in the field of psychiatry under the name “Psychosomatic Medicine” in United States. With well-established C-L Psychiatry subspecialty there are training guidelines with respect to C-L Psychiatry in United States and Europe.[16,17] In United States American Psychiatric Association Council on Psychosomatic Medicine, the Psychosomatic Committee of American Board of Psychiatry and Neurology, and the Academy of Psychosomatic Medicine have defined the core competencies for Fellowship Training in Psychosomatic Medicine.[16] The European Association of Consultation–Liaison Psychiatry and Psychosomatics (EACLPP) have given recommendations for the European countries which covers various aspects as to when during the training C-L rotation should be done, what should be the goals and objectives of the training and also lays down guidelines about the basic acquisition of knowledge, skills and attitudes for practice of C-L Psychiatry. Also provides guidelines for fellowship programme.[17]
CONSULTATION LIAISON MODELS WORLD WIDE VIS-A-VIS INDIA
Various models of psychiatric consultation are described in literature depending on the focus of consultation, function and focus of work. These models based on the focus of consultation include patient oriented approach, crisis oriented approach, consultee-oriented approach, situation oriented approach and expanded psychiatric consultation. In the patient oriented approach, patient is the primary focus of the consultant's interest. It not only includes diagnostic interview and assessment of the patient but also includes a psychodynamic evaluation of the patient's personality and reaction to illness.[3] The crisis-oriented approach involves a rapid assessment of patient's problem and coping styles and immediate therapeutic intervention to address the problem.[18] In the consultee-oriented approach the motive of the consultee and his related difficulties and expectations are the major focus.[19] The situation oriented approach focuses on the interpersonal interactions of all the members of the clinical team involved in the care of the patient for whom consultation had been sought are taken into consideration to understand the patient's behavior and the consultee's concern about it.[20] The expanded psychiatric consultation model includes an operational group that involves the patient, the clinical staff, other patients, and the patient's family, however the central focus is the patient for whom consultation has been sought.[21]
Depending on the function the models of consultation-liaison include consultation model, liaison model, bridge model, hybrid model and autonomous psychiatric model. The traditional consultation model has patient as the focus. The liaison model has the consulting physician as the center of focus and in addition to providing consultation for the patient also involves teaching psychiatric and psychological aspects of patient's problem to the physician and the clinical team. The bridge model basically involves the teaching role of a C-L psychiatrist for the primary care physicians. The hybrid model has psychiatrist as part of multidisciplinary team. In the autonomous psychiatric model the C-L psychiatrist is not affiliated to any department but is hired by primary care services.[22] Depending on the focus of work the different models include critical care model, biological model, Milieu model and integral model. In the critical care model the C-L psychiatrists is attached to a critical care unit, like intensive care unit, cardiac care unit who is involved in patient care and redressal of issues of staff. The biological model lays emphasis on neuroscience, psychopharmacology and psychological management. The milieu model is based on interpersonal theory and involves group aspects of patient care, reaction and interaction of staff and understanding of ward environment. The integral model is usually agency based and involves providing psychological care as an integral factor of clinical and administrative need.[23]
Depending on the model and available resources the composition of C-L team has been discussed in the Western literature. Accordingly the composition of C-L services has varied from single remote consultant to multidisciplinary teams. In general a multidisciplinary team is recommended. In recent times collaboration at the outpatient level with physicians and surgeons or primary care has also started and there are no fixed recommendations for the composition of the team. In general the composition of team is determined by local and feasibility factors.[5]
As with other subspecialties of psychiatry, broadly the functions of a C-L psychiatrist can be divided into clinical work, teaching, administration and clinical research. The clinical work involves facilitation of the medical treatment of the patient. The liaison of C-L Psychiatry in general denotes the educational function of the same and the C-L Psychiatrists is expected to cater the patients, requesting physicians, nursing staff, patients’ families and friends, and the health care system.[24] In addition to this C-L Psychiatrist may be required to teach the trainees. The administrative functions of the C-L Psychiatrist depends on the setting in which they work and may involve measures like holding the patient in the emergency, involuntary hospitalization of patients and assessment of suicidal and homicidal patients. The C-L Psychiatry setting provides unique opportunity for research in the areas that are at the interface of psychiatry and medicine. Depending on the medical set-up over the years based on these functions of C-L psychiatrists many further sub-specialties like psycho-oncology and psycho-obstetrics have emerged.
Further, C-L psychiatrists are viewed as the most suitable persons to prepare primary care clinicians to manage these psychiatric patients. Further, due to biomedical sophistication in medical care, busy physician specialists have started expecting the hospital-based psychiatrists to assume some of the traditional roles of the primary clinical caretaker for their patients. Due to all this, consultation-oriented model has begun to prevail.[10]
Unfortunately the practice of C-L Psychiatry is not well described in India. In a recent review of studies on C-L Psychiatry, Parkar and Sawant[25] commented, “there is no specific philosophy or particular clinical context being identified in liaison psychiatry in India”.
Based on the studies available from India, broadly the C-L Psychiatry services at various centres focus on inpatient and outpatients. Studies which have been published in relation to the inpatient Consultation-Liaison Psychiatry services, most of these have been silent on the functional aspect of the services. What is evident is that, the C-L services are mostly in the line with the consultation model, in which on receiving a referral from the physician/surgeon, a psychiatrist evaluates the patient and psychiatric inputs are provided.
Department of Psychiatry at Post Graduate Institute of Medical Education and Research, Chandigarh has been one of the premier training center in general hospital setting, which provides training opportunity in C-L Psychiatry. The model followed at this center is described here and it is presumed that many other centres in India also follow similar model. Department runs C-L Psychiatry services round the clock to provide psychiatry inputs to all the inpatients and patients attending the emergency outpatients. The patients who are referred from other outpatients are usually seen in the psychiatry outpatient Walk-in-clinic. The C-L Psychiatry services have a faculty member who is incharge of the administrative part of the services and carries out regular audits on weekly basis with respect to the functioning of the services. All the faculty members provide supervision to the junior resident and the senior resident on daily rotation basis. With respect to the functioning part the services are organized as a three-tier system, in which all the cases are first evaluated by a trainee psychiatrist under the supervision of a senior resident psychiatrist and finally reviewed by a consultant psychiatrist. The trainee junior resident is usually posted for 3 months in the C-L Psychiatry services, besides having exposure of the same during the two-and-half year of his training in the form of evening on call duty on rotation for providing emergency on call C-L Psychiatry services. The junior resident is supervised by a senior resident who is posted in C-L Psychiatry services for a period of 6 months. The clinical evaluation focuses on psychiatric morbidity and its attribution to physical illness. The diagnoses are made according to the ICD system, and appropriate treatment plan is formulated, implemented and periodically reviewed. The teaching of clinical skills focuses on the elicitation of psychiatric signs and symptoms, establishing the relationship of psychological morbidity and physical illness, documentation of history from the medico-legal point of view, confidentiality issues, providing psychotherapeutic interventions and psychopharmacological intervention wherever required. All the patients are followed up on regular basis by the C-L Psychiatry team till discharge or death. Besides documenting the history in the primary treating team case records, the C-L Psychiatry team maintains its own records in which patient's history (physical and psychological), treatment, investigation findings and follow-up etc are documented. The information from the C-L Psychiatry case records is summarized in a referral register under the following headings: age, sex, source of referral, physical diagnosis, reason for psychiatric referral, psychiatric diagnosis, management done and outcome. These case records and the register are monitored weekly for completeness by the consultant in charge of C-L Psychiatry services. Once the patient is discharged from the hospital, the case records are transferred to psychiatric outpatient service where the same psychiatric team provides the continuity of psychiatric care. In all cases, an effort is made to communicate with the primary physician about the psychological morbidity, its relationship with physical illness and treatment of the same. In all cases the C-L Psychiatry team regularly also communicates with the other staff of the hospital involved in the patient care (e.g. nursing staff). The family members are also informed about the psychological morbidity and in cases, which require intensive psychiatric management; patient and family are advised to follow-up in the psychiatry outpatient. Patients who come for follow-up in the psychiatric outpatients are seen by the same C-L team (the junior resident, senior resident or the faculty members) to maintain the continuity of care.
Besides providing clinical services, the C-L Psychiatry services has two other basic components, i.e., teaching the trainee junior residents in psychiatry and other specialties, and having joint academic rounds. While the senior resident and the faculty members evaluate the case in the medical-surgical wards, it also provides good opportunity to teach basic clinical skills to the junior resident. The academic activities involve monthly psychosomatic rounds with Internal Medicine, General surgery, Pediatrics and Neurology. The psychosomatic rounds is attended by faculty members from psychiatry and the other concerned specialty in which a case of common interest is presented by a trainee junior resident of psychiatry and a trainee junior resident of the other specialty.
With respect to outpatient C-L Psychiatry services in India, again a consultation model is mostly followed at various centers[26] or only some research activities with special focus have been carried out[27–30] and a true liaison model is not evident from the available studies.
RESEARCH IN C-L PSYCHIATRY SUBSPECIALTY AND CONTRIBUTION TO MEDICINE: WORLDWIDE VIS-À-VIS INDIAN SCENARIO
C-L Psychiatry research has made major contribution to the practice of medicine. Broadly speaking C-L Psychiatry has brought forward the concept of psychiatric sequelae of medical disorders, contribution of psychiatric manifestations to the etiology, course and outcome of various medical illnesses. There have been landmark studies in diabetes, HIV/AIDS, coronary artery disease, cancer, and stroke. C-L Psychiatry has also highlighted the issues of management of various psychiatric disorders in the presence of comorbid medical illnesses, drug interactions of psychotropics with other medications, and medication induced psychiatric symptoms. The importance of role of psychiatric disorders in medicine can be understood from the fact that over the years there has been evolution of terms like psycho-oncology, transplant psychiatry, psycho-nephrology, cardiac psychiatry etc. The role of C-L psychiatrist in identification and appropriate management of delirium has contributed significantly to reduce the hospital morbidity and health care costs.[10,31] In fact proper identification of causes of delirium has led to change in designs of intensive care unit (ICU) and procedural changes in ICU management in the form of providing more periods of uninterrupted sleep, providing orientation as to time and place, and transfer of patients out of ICU setting as soon as possible.[31] Proper understanding of panic attacks in 1970s and 1980s, led to application of this knowledge in the C-L Psychiatry and demonstration of panic disorder in significant number of patients with chest pain and normal coronary angiograms.[32,33] This led to consideration of panic disorder as an important differential diagnosis of cardiac symptoms. This has led to more accurate diagnosis and therefore fewer unnecessary angiograms and more appropriate treatment of a relatively common and often disabling disorder.[34] Depression as an important risk factor for myocardial infarction and unrecognized depression leading to poor outcome in coronary artery disease patients is now an established fact.[31] Many clinical trials have been done to evaluate the effect of antidepressant on the outcome in the post myocardial infarction phase.[34–39] Findings on similar lines have been reported about impact of depression on the outcome of post-stroke patients.[40]
The liaison with neurologist has led to identification of various psychiatric manifestations of Parkinsonism and psychiatric symptoms in epilepsy. C-L Psychiatry has also played an important role in managing the medically ill patient who come up with the request to leave the hospital against medical advise and it has been found that most of these patients are very angry, very anxious, psychotic or demented.[31] By showing that sleep deprivation leads to higher number of errors and dysphoric mood in interns who are on duty for 48-72 hours C-L Psychiatry has also contributed to changes in the hospital policies with respect to the training and posting of the interns.[41] Studies have also highlighted how various surgical procedures can lead to different psychological outcome and hence have influenced what kind of surgery is practiced for a particular ailment.[42–44] C-L Psychiatry has also contributed to discussion about diagnosis like cancer more openly and acceptance of the same. It has also influenced the policy of “truth telling” in medicine and individualization of information disclosure as to “What truth, for which patient, at what time?”.[31,45] With the advancement in the field of organ transplant, C-L psychiatrists are not only required for pre- and post-operative evaluation of the recipient and potential donors, but they are also required to deal with a situation in which a potential donor, related to the patient, is reluctant to give up an organ but is unable to tell their family.[31] The role of C-L psychiatrists in HIV/AIDS can’t be underestimated in the present era. Studies have also shown that teaching primary care physicians as to how to apply psychiatric principles to the treatment of outpatients with hypochondriasis has lead to reduction in the medical cost.
Other important contribution of C-L Psychiatry to practice of whole medicine despite proliferation of technologies has been an attempt to preserve humanism in medicine, direction provided to communication skills of physicians and preservation of medical ethics in difficult situations. Today clinical ethics goes beyond issues of legal competency and theoretical ethical principles such as “autonomy” and “beneficence” and it requires a knowledgeable clinician with an understanding of psychological factors that are inherent in making life-and-death decisions. The role of C-L psychiatrist in end of life issues has also received significant attention.[31]
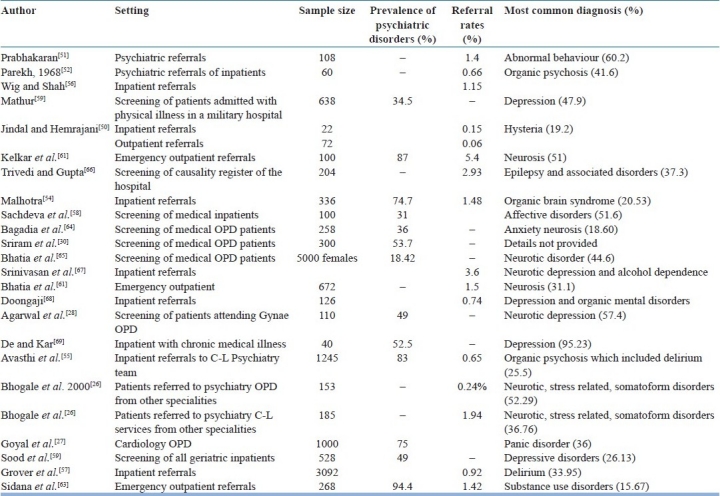
In contrast to West, research in C-L Psychiatry in India has been meager and has been recently reviewed by many authors.[25,46–49] Earlier studies [Table 2] have focused on the routine referral rates from the medical-surgical inpatients and in general concluded that the referrals rates in India are much lower (0.15-3.6%).[50–57] However, studies, which have screened all the patients for psychiatric morbidity, have reported higher morbidity rates (31%-34.5%)[58,59] and a study, which specifically evaluated the psychiatric morbidity in geriatric inpatients, reported morbidity rate of 49%.[60] Besides evaluation of psychiatric referrals rates, some of the studies have also presented the rate of psychiatric morbidity and usually these have been reported to be high (74.7%-83%).[54,55] Few studies have also evaluated the referral rates from emergency outpatients [Table 2].[61–63] Studies have also screened patients presenting to various outpatient departments (General Medicine, Cardiology, Gynecology)[27,28,30,64,65] for psychiatric morbidity and have reported a prevalence rate of 18.42% to 53.7%.
Table 2.
Studies showing psychiatric referral rates, prevalence of psychiatric morbidity in psychiatric referrals and the most common psychiatric diagnosis
Studies have also evaluated the prevalence of various psychiatric disorders, personality features and influence of various interventions in patients with various physical illnesses. However, the studies have been few in number.
A review of studies published in Indian Journal of Psychiatry from 1950-2010 shows that there are only 117 studies on psychiatric aspects of various physical illnesses [Figure 1].[70–186] Among the various group of patients studied issues of women mental health has received considerable attention. In general most of the studies which have been done have included smaller samples and have methodological limitations. There is lack of data originating in the form of a multicentric study. Besides the studies published in Indian Journal of Psychiatry, many studies have been published in other national and international journals. But in general the studies are few in number and limited group of researchers have worked consistently in these areas. The major areas of research by psychiatrists have been cancer (for details see review),[47] pain,[187] gynecological issues,[188–195] HIV,[196–198] dermatological disorders,[199,200] diabetes mellitus[201,202] and chest pain.[203] Occasional studies have evaluated psychiatric morbidity and other aspects in diseases like Cushing disease,[204,205] Acromegaly[206] and Delirium.[207–210] Some studies have also evaluated the usefulness of screening instruments in diagnosing common mental disorders in medically ill.[211,212] Another major area of focus has been patients with deliberate self harm.[213]
Figure 1.
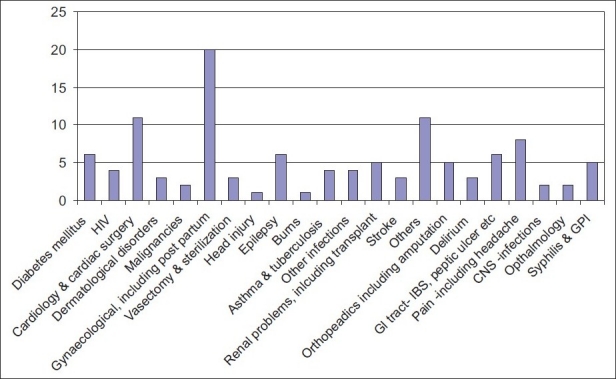
Number of Studies published in Indian Journal of Psychiatry from 1949 to 2010 on psychiatric aspects of various physical disorders
SOME OF THE IMPORTANT RECENT TRENDS
An important change in recent times has been the focus on the physical health of mentally ill subjects. Studies have shown that about 50% of mentally ill subjects have some or other form of physical illness.[214] Further with the increase in life span, there is rise in geriatric population in India.[215] These important trends again alarm us that a psychiatrist with good knowledge of C-L Psychiatry may be able to manage his patients in a better way in general.
OTHER SIDE OF THE COIN: PSYCHIATRIC KNOWLEDGE AND AWARENESS ABOUT PSYCHOLOGICAL ISSUES IN MEDICALLY ILL SUBJECTS IN PHYSICIANS AND SURGEONS
There has been a great debate about the dismal psychiatric training in the under-graduate level and most of the graduates who pass out from the medical colleges are unaware about the psychiatric disorders and the role of psychological factors in the manifestation, course and prognosis of various medical and surgical illnesses. Indian Psychiatric Society has made many attempts to improve the training in psychiatry at the undergraduate level and recently also submitted its recommendations to the Medical Council of India for the undergraduate training in psychiatry. The lack of knowledge about psychiatric disorders at the undergraduate level is never rectified if a trainee opts for any other branch and hence remains deficient in these skills. However, some of the physicians and surgeons because of their own interest make efforts to gain this knowledge and apply the same in their clinical practice. The fact that many physicians and surgeons are deficient in their psychiatry knowledge was exemplified in a survey in which 87% of the physicians and surgeons opined that they would have been helped if there undergraduate training in psychiatry had been better.[216] Ninety-one percent of the physicians and surgeons also opined that development of C-L psychiatric units would definitely help in improving the care of the patients with psychiatric problems in non-psychiatric units in general hospitals. It was also seen that many of the clinicians under-estimated the psychiatric morbidity in their patients. Some of the clinicians also pointed out that there was a need for public awareness and education about the psychiatric disorders.[216] Another survey of general practitioners and specialist also showed that they felt deficient in their psychiatric skills provided to them during their training and were eager to learn more about management of their psychiatric cases.[217] However, if we want to sensitize the undergraduate students about psychiatry, besides providing knowledge about primary psychiatric disorders, there is equal need to educate them about the role of psychological factors in causation, precipitation and management of various physical illnesses.
WHERE DO WE GO FROM HERE: VISION FOR FUTURE
The role of psychological factors in the etiology of various physical disorders emerged from practice and theory of psychodynamic principles. However, over the years, focus of mind and body has not received much attention. This is understandable, because over the years the main focus has been on improving the reliability of psychiatric diagnosis. With the improvement in reliability of psychiatric diagnosis and understanding of neurobiology, there is evidence to suggest that psychiatric disorders have underlying biological underpinnings. The neurobiological research in primary psychiatric disorders, suggests that there are neurochemical, neuroanatomical, functional changes in the brain and dysfunction in the endocrine system in various psychiatric disorders. However, in the process of improving the reliability of psychiatric disorders and understanding their biological correlates, the mind-body interaction has somehow not received its due attention.
Physical comorbidity in mentally ill subjects has generated significant interest in the recent times and importance of the same in holistic management of psychiatrically ill patients cannot be over-emphasized. Further now there is emphasis on providing psychiatric care at the primary care level, where patients frequently have physical comorbidity and psycho-somatic symptoms. Hence, whatever way it is looked at now, it is increasingly been accepted that mind and body cannot be seen separately and both the aspects need to be addressed together for better patient outcome.
Although most of the psychiatric care in India is provided through the Government funded GHPUs, GHPUs in private medical colleges, multispecialty private hospitals, the focus of training has never been on C-L Psychiatry. One argument can be that there is mismatch between the available trained manpower and the requirement of the community; hence the focus of services and training has been on treating the patients with primary psychiatric illnesses. However, it is now important to remember that we can not see patients of psychiatric disorders and those with physical illnesses in isolation and there is a need to focus on both the aspects while catering to these patients and training the residents. Hence, integrated approach, which focuses on both the aspects, i.e., psychological aspects of physical illnesses and physical comorbidity and its impact on psychiatric disorders, is important. Besides training the resident in diagnosing and managing primary psychiatric disorders, the training should also focus on C-L Psychiatry. Further, C-L Psychiatry as a subspecialty should be looked as an important component of child psychiatry, geriatric psychiatry and community psychiatry training. Efforts to enhance C-L Psychiatry services so as to improve clinical services, training and research at the GHPUs can enhance the quality of care to large extent. Taking the availability of the human resources into consideration, consultation model at the start can be useful. The centers which have well established consultation model should go beyond it and establishment of true consultation-liaison model with certain medico-surgical specialties; in which psychosocial issues are very important in overall management can be very useful.
With regard to training of residents, making a proper diagnosis, communicating with the primary treating physician and other treating team members, documentation of psychiatric history from medico-legal point of view, reviewing the cases from time to time, learning to provide non-pharmacological treatment in a non-psychiatric set up and use of psychotropic medications in medically ill subjects must be emphasized. Psychiatry resident should at least have 3-4 months of training exclusively focusing on the C-L Psychiatry. Besides the resident undergoing training in psychiatry, trainee doctors undergoing residency in other medical and surgical specialties can also be targeted, so that they are sensitive to the psychological aspects of medical illnesses. Having common clinical case conferences or psychosomatic rounds can do this to some extent. In addition didactic lectures covering various topics can be helpful. Centers with well-established C-L services can start fellowships programmes of 6 months to 1 year to provide training to interested candidates. Starting of this kind of programme will have 2 fold advantages. One, it would help in enhancing the available human resource in providing services and second it would also enhance the skills and training of the candidate. Besides focusing on the psychiatrist there is need to enhance the training of other mental health professionals like nurses, clinical psychologists and social workers so that they can provide some of the basic inputs to improve the mental health and care of medically ill subjects.
Beyond the efforts of establishing services and training at the specific institute levels, having a task force of Indian Psychiatric society on psychosomatic medicine/C-L Psychiatry may be useful, which can focus on holding regular continuing medical education (CMEs) programmes on various aspects of C-L Psychiatry. Further, coordinating with other scientific societies of various disciplines in holding joint conferences to enhance skills of specialist from either discipline can be considered.
In future elderly with medical illnesses, those with metabolic syndrome and diabetes, patients with heart disease with depression and anxiety, the HIV-infected population living under conditions of stress and depression, and those patients in need of physical rehabilitation will require lot of psychiatric inputs. Many of these patients will require use of behavioral measures like relaxation exercises and cognitive behaviour therapy. The training and research should focus on some of these areas with priority to meet the need of the needy population.
There is an urgent need to carry out research in this area with the aim of developing indigenous instruments, models of practice and intervention to improve overall outcome of patients. Many of the patients seen in C-L Psychiatry services also don’t fit into clear diagnostic categories as described by the current nosological systems. Hence there is need to develop diagnostic models which can fit the symptomatology of various disorders in the C-L Psychiatry set up. Further it is important to carry out multicentric studies to have a better countrywide data that can ultimately be translated in providing mental health care at the primary care level.
CONCLUSIONS
C-L Psychiatry has a rich tradition knowledge base. The relationship of psychiatry with other medical illnesses has progressed from the phases of psychodynamic understanding of medical symptoms, subsyndromal symptoms of various primary psychiatric disorders to diagnosing syndromal psychiatric disorders. In future, with emerging research and role of epigenetic in various psychiatric and physical illnesses, new clinical challenges are going to emerge which will further enhance the role of a psychiatrist who is well equipped to deal with psychological issues in medically ill subjects and has better understanding of the comorbidity. Hence there is a need to improve CL psychiatry to provide best and optimal care to the patients and provide best education to the trainees.
ACKNOWLEDGMENTS
I dedicate this oration to all my teachers and colleagues who have taught me and guided me; to all my students who have worked with me from time to time and to my family, which has supported me.
I gratefully acknowledge the contribution of my students Dr. Uma Maheshswari and Dr. Aarya KR who helped me organize the material for this oration.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Lipowski ZJ. Current trends in consultation-liaison psychiatry. Can J Psychiatry. 1983;28:329–38. doi: 10.1177/070674378302800501. [DOI] [PubMed] [Google Scholar]
- 2.Lipowski ZJ. Review of consultation psychiatry and psychosomatic medicine. I. General principles. Psychosom Med. 1967;29:153–71. doi: 10.1097/00006842-196703000-00007. [DOI] [PubMed] [Google Scholar]
- 3.Lipowski ZJ. Review of consultation psychiatry and psychosomatic medicine. II. Clinical aspects. Psychosom Med. 1967;29:201–24. doi: 10.1097/00006842-196705000-00001. [DOI] [PubMed] [Google Scholar]
- 4.Lipowski ZJ. Consultation-liaison psychiatry in a general hospital. Compr Psychiatry. 1971;12:461–5. doi: 10.1016/0010-440x(71)90086-1. [DOI] [PubMed] [Google Scholar]
- 5.Mayou R. The development of general hospital psychiatry. In: Lloyd G, Guthrie E, editors. Handbook of Liaison Psychiatry. Cambridge, UK: Cambridge University Press; 2007. [Google Scholar]
- 6.Rogers MP, Fricchione G, Reich P. Psychosomatic medicine and consultation-liaison psychiatry. In: Nicholi AM Jr, editor. The Harvard Guide to Psychiatry. Cambridge MA: Belknap Press; 1999. pp. 362–89. [Google Scholar]
- 7.Lipowski ZJ, Wise TN. History of consultation-liaison psychiatry. In: Wise MG, Rundell JR, editors. Textbook of Consultation Liaison Psychiatry. Washington, DC: American Psychiatric Publishing; 2002. pp. 3–11. [Google Scholar]
- 8.Parkar SR, Dawani VS, Apte JS. History of psychiatry in India. J Postgrad Med. 2001;47:73–6. [PubMed] [Google Scholar]
- 9.Lipsitt DR. Consultation-Liaison Psychiatry and Psychosomatic Medicine: The Company They Keep. Psychosom Med. 2001;63:896–909. doi: 10.1097/00006842-200111000-00008. [DOI] [PubMed] [Google Scholar]
- 10.Ali S, Ernst C, Pacheco M, Fricchione G. Consultation-liaison psychiatry: How far have we come? Curr Psychiatry Rep. 2006;8:215–22. doi: 10.1007/s11920-006-0026-y. [DOI] [PubMed] [Google Scholar]
- 11.Sarada Menon M. Mental Health in Independent India: The Early Years. In: Agarwal SP, editor. Mental Health and Indian Perspective. New Delhi: Directorate General of Health Services Ministry of Health and Family Welfare; 2005. pp. 30–6. [Google Scholar]
- 12.Mohan D. General Hospital-Based Psychiatric Training: The All India Institute of Medical Sciences Experience. In: Agarwal SP, editor. Mental Health and Indian Perspective. 2005. pp. 221–6. [Google Scholar]
- 13.Kulhara P. Postgraduate Psychiatric traiing centres: Findings of a survey. Indian J Psychiatry. 1985;27:221–6. [PMC free article] [PubMed] [Google Scholar]
- 14.Kulhara P. General hospital in postgraduate psychiatric training and research. Indian J Psychiatry. 1984;26:281–5. [PMC free article] [PubMed] [Google Scholar]
- 15.Medical Council of India. [last accessed on 2010 Dec 15]. Available from: http://www.mciindia.org/InformationDesk/Colleges Courses .
- 16.Worley LL, Levenson JL, Stern TA, Epstein SA, Rundell JR, Crone CC, et al. Core competencies for fellowship training in psychosomatic medicine: A collaborative effort by the APA Council on Psychosomatic Medicine, the ABPN Psychosomatic Committee, and the Academy of Psychosomatic Medicine. Psychosomatics. 2009;50:557–62. doi: 10.1176/appi.psy.50.6.557. [DOI] [PubMed] [Google Scholar]
- 17.Söllner W, Creed F. European Association of Consultation-Liaison Psychiatry and Psychosomatics Workgroup on Training in Consultation-Liaison.European guidelines for training in consultation-liaison psychiatry and psychosomatics: Report of the EACLPP Workgroup on Training in Consultation-Liaison Psychiatry and Psychosomatics. J Psychosom Res. 2007;62:501–9. doi: 10.1016/j.jpsychores.2006.11.003. [DOI] [PubMed] [Google Scholar]
- 18.Weisman AD, Hackett TP. Organization and function of a psychiatric consultation service. Int Rec Med. 1960;173:306–11. [PubMed] [Google Scholar]
- 19.Schiff SK, Pilot ML. An approach to psychiatric consultation in the general hospital. Arch Gen Psychiatry. 1959;1:349–57. doi: 10.1001/archpsyc.1959.03590040019001. [DOI] [PubMed] [Google Scholar]
- 20.Greenberg IM. Approaches to psychiatric consultation in a research hospital setting. Arch Gen Psychiatry. 1960;3:691–7. doi: 10.1001/archpsyc.1960.01710060123017. [DOI] [PubMed] [Google Scholar]
- 21.Meyer E, Mendelson M. Psychiatric consultations with patients on medical and surgical wards: Patterns and processes. Psychiatry. 1961;24:197–220. doi: 10.1080/00332747.1961.11023268. [DOI] [PubMed] [Google Scholar]
- 22.Strain JJ. Liaison Psychiatry. In: Rundell JR, Wise MG, editors. Textbook of Consultation-Liaison Psychiatry. Washington DC: American Psychiatric Press; 1996. pp. 37–51. [Google Scholar]
- 23.Greenhill MH. The development of liaison programs. In: Usdin G, editor. Psychiatric Medicine. New York: Brunner Mazel; 1977. pp. 115–91. [Google Scholar]
- 24.Leigh H. Evolution of Consultation-Liaison Psychiatry and Psychosomatic Medicine. In: Leigh H, Streltser J, editors. Handbook of Consultation-Liaison Psychiatry. Springer; 2008. pp. 3–11. [Google Scholar]
- 25.Parkar SR, Sawant NS. Liaison Psychiatry and Indian research. Indian J Psychiatry. 2010;52:S386–8. doi: 10.4103/0019-5545.69274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bhogale GS, Katte RM, Heble SP, Sinha UK, Patil PA. Psychiatric referrals in multi speciality hospital. Indian J Psychiatry. 2000;42:188–94. [PMC free article] [PubMed] [Google Scholar]
- 27.Goyal A, Bhojak MM, Verma KK, Singhal A, Jhirwal OP, Bhojak M. Psychiatric morbidity among patients attending cardiac OPD. Indian J Psychiatry. 2001;43:335–9. [PMC free article] [PubMed] [Google Scholar]
- 28.Agrawal P, Malik SC, Padubidri V. A study of psychiatric morbidity in Gynaecology outpatient clinic. Indian J Psychiatry. 1990;32:57–63. [PMC free article] [PubMed] [Google Scholar]
- 29.Bagadia VN, Ayyar KS, Lakdawala PD, Sheth SM, Acharya VN, Pradhan PV. Psychiatric morbidity among patients attending medical outpatient department. Indian J Psychiatry. 1986;28:139–44. [PMC free article] [PubMed] [Google Scholar]
- 30.Sriram TG, Shamasunder C, Mohan KS, Shanmugham V. Psychiatric morbidity in the medical outpatients of a general hospital. Indian J Psychiatry. 1986;28:325–8. [PMC free article] [PubMed] [Google Scholar]
- 31.Kornfeld DS. Consultation-liaison psychiatry: contributions to medical practice. Am J Psychiatry. 2002;159:1964–72. doi: 10.1176/appi.ajp.159.12.1964. [DOI] [PubMed] [Google Scholar]
- 32.Katon W, Hall ML, Russo J. Chest pain: Relationship of psychiatric illness to coronary arteriographic results. Am J Med. 1988;84:1–9. doi: 10.1016/0002-9343(88)90001-0. [DOI] [PubMed] [Google Scholar]
- 33.Beitman BD, Mukerji V, Lamberti JW, Schmid L, DeRosear L, Kushner M, et al. Panic disorder in patients with chest pain and angiographically normal coronary arteries. Am J Cardiol. 1989;63:1399–403. doi: 10.1016/0002-9149(89)91056-4. [DOI] [PubMed] [Google Scholar]
- 34.Mazza M, Lotrionte M, Biondi-Zoccai G, Abbate A, Sheiban I, Romagnoli E. Selective serotonin reuptake inhibitors provide significant lower re-hospitalization rates in patients recovering from acute coronary syndromes: Evidence from a meta-analysis. J Psychopharmacol. 2010;24:1785–92. doi: 10.1177/0269881109348176. [DOI] [PubMed] [Google Scholar]
- 35.Hansen BH, Hanash JA, Rasmussen A, Hansen JF, Birket-Smith M. Rationale, design and methodology of a double-blind, randomized, placebo-controlled study of escitalopram in prevention of Depression in Acute Coronary Syndrome (DECARD) Trials. 2009;10:20. doi: 10.1186/1745-6215-10-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Cowan MJ, Freedland KE, Burg MM, Saab PG, Youngblood ME, Cornell CE, et al. Predictors of treatment response for depression and inadequate social support--the ENRICHD randomized clinical trial. Psychother Psychosom. 2008;77:27–37. doi: 10.1159/000110057. [DOI] [PubMed] [Google Scholar]
- 37.Glassman AH, O’Connor CM, Califf RM, Swedberg K, Schwartz P, Bigger JT, Jr, et al. Sertraline treatment of major depression in patients with acute MI or unstable angina: Sertraline Antidepressant Heart Attack Randomized Trial. JAMA. 2002;288:701–9. doi: 10.1001/jama.288.6.701. [DOI] [PubMed] [Google Scholar]
- 38.Serebruany VL, Glassman AH, Malinin AI, Nemeroff CB, Musselman DL, van Zyl LT, et al. Platelet/endothelial biomarkers in depressed patients treated with the selective serotonin reuptake inhibitor sertraline after acute coronary events: The Sertraline Anti Depressant Heart Attack Randomized Trial (SADHART) Platelet Substudy. Circulation. 2003;108:939–44. doi: 10.1161/01.CIR.0000085163.21752.0A. [DOI] [PubMed] [Google Scholar]
- 39.van den Brink RH, van Melle JP, Honig A, Schene AH, Crijns HJ, Lambert FP, et al. Treatment of depression after myocardial infarction and the effects on cardiac prognosis and quality of life: rationale and outline of the Myocardial INfarction and Depression-Intervention Trial (MIND-IT) Am Heart J. 2002;144:219–25. [PubMed] [Google Scholar]
- 40.Morris PL, Robinson RG, Andrzejewski P, Samuels J, Price TR. Association of depression with 10-year poststroke mortality. Am J Psychiatry. 1993;150:124–9. doi: 10.1176/ajp.150.1.124. [DOI] [PubMed] [Google Scholar]
- 41.Friedman RG, Bigger TJ, Kornfeld DS. The intern and sleep loss. N Engl J Med. 1971;285:201–3. doi: 10.1056/NEJM197107222850405. [DOI] [PubMed] [Google Scholar]
- 42.Druss RG, O’Conner JF, Prudden JF, Stern LO. Psychological response to colectomy. Arch Gen Psychiatry. 1968;18:53–9. doi: 10.1001/archpsyc.1968.01740010055008. [DOI] [PubMed] [Google Scholar]
- 43.Stevens L, McCarthy M. The psychological impact of immediate breast reconstruction for women with early breast cancer. Plast Reconstr Surg. 1984;73:619–26. doi: 10.1097/00006534-198404000-00018. [DOI] [PubMed] [Google Scholar]
- 44.Wellisch DK, Di Matteo R, Silverstein M, Landsverk J, Hoffman R, Waisman J, et al. Psychosocial outcomes of breast cancer therapies—lumpectomy vs mastectomy. Psychosomatics. 1989;30:365–73. doi: 10.1016/S0033-3182(89)72241-6. [DOI] [PubMed] [Google Scholar]
- 45.Kornfeld DS. Doctor's dilemma: ,what truth for which patient at what time?’. CA Cancer J Clin. 1978;28:256. doi: 10.3322/canjclin.28.4.256. [DOI] [PubMed] [Google Scholar]
- 46.Pinto C. Indian research on acute organic brain syndrome: Delirium. Indian J Psychiatry. 2010;52:139–47. doi: 10.4103/0019-5545.69226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Mehrotra S. Psycho-Oncology Research in India: Current Status and Future Directions. J Indian Acad Appl Psychol. 2008;34:7–18. [Google Scholar]
- 48.Mattoo SK, Grover S, Gupta N. Delirium in general practice. Indian J Med Res. 2010;131:387–98. [PubMed] [Google Scholar]
- 49.Gautam S. Fourth revolution in psychiatry - Addressing comorbidity with chronic physical disorders. Indian J Psychiatry. 2010;52:213–9. doi: 10.4103/0019-5545.70973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Jindal RC, Hemrajani DK. A study of psychiatric referrals in a general hospital. Indian J Psychiatry. 1980;22:108–10. [PMC free article] [PubMed] [Google Scholar]
- 51.Prabhakaran NN. In-patient psychiatric referrals in a general hospital. Indian J Psychiatry. 1968;10:73–7. [Google Scholar]
- 52.Parekh HC, Deshmukh DK, Bagadia VN, Vahia NS. Analysis of indoor psychiatric referrals in a general hospital. Indian J Psychiatry. 1968;10:81–3. [Google Scholar]
- 53.Chatterjee SB, Kutty PR. A study of psychiatric referrals in Military practice in India. Indian J Psychiatry. 1977;19:32–8. [Google Scholar]
- 54.Malhotra S, Malhotra A. Liaison Psychiatry in an Indian general hospital. Gen Hosp Psychiatry. 1984;6:266–70. doi: 10.1016/0163-8343(84)90020-3. [DOI] [PubMed] [Google Scholar]
- 55.Avasthi A, Sharan P, Kulhara P, Malhotra S, Varma VK. Psychiatric Profiles in Medical-Surgical Populations: Need for a focused approach to consultation-liaison psychiatry in developing countries. Indian J Psychiatry. 1998;40:224–30. [PMC free article] [PubMed] [Google Scholar]
- 56.Wig NN, Shah DK. Psychiatric unit in a general hospital in India: Patterns of inpatient referrals. J Indian Med Assoc. 1973;60:83–6. [PubMed] [Google Scholar]
- 57.Grover S, Subodh BN, Avasthi A, Chakrabarti S, Kumar S, Sharan P, et al. Prevalence and clinical profile of Delirium: A study from a tertiary care hospital in north India. Gen Hosp Psychiatry. 2009;31:25–9. doi: 10.1016/j.genhosppsych.2008.06.001. [DOI] [PubMed] [Google Scholar]
- 58.Sachdeva JS, Shergill CS, Sidhu BS. Prevalence of psychiatric morbidity among medical in-patients. Indian J Psychiatry. 1986;28:293–6. [PMC free article] [PubMed] [Google Scholar]
- 59.Mathur RS. Psychiatric morbidity in soldiers hospitalised for physical ailments. Indian J Psychiatry. 1977;19:89–96. [Google Scholar]
- 60.Sood A, Singh P, Gargi PD. Psychiatric morbidity in non-psychiatric geriatric inpatients. Indian J Psychiatry. 2006;48:56–61. doi: 10.4103/0019-5545.31621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Kelkar DK, Chaturvedi SK, Malhotra S. A study of emergency psychiatric referrals in a teaching general hospital. Indian J Psychiatry. 1982;24:366–9. [PMC free article] [PubMed] [Google Scholar]
- 62.Bhatia MS, Agrawal P, Khastbir U. A study of emergency psychiatric referrals in a government hospital. Indian J Psychiatry. 1988;30:363–8. [PMC free article] [PubMed] [Google Scholar]
- 63.Sidana A, Sharma RP, Chavan BS, Arun P, Lokraj Psychiatric profile of patients attending General Emergency room services- A prospective study. J Ment Health Hum Behav. 2009;14:80–3. [Google Scholar]
- 64.Bagadia VN, Ayyar KS, Lakdawala PD, Sheth SM, Acharya VN, Pradhan PV. Psychiatric morbidity among patients attending medical outpatient department. Indian J Psychiatry. 1986;28:139–44. [PMC free article] [PubMed] [Google Scholar]
- 65.Bhatia MS, Balakrishna NK, Dhar, Bohra N, Gupta H, Malik SC. Psychiatric morbidity in patients attending medical OPD. Indian J Psychiatry. 1987;29:243–6. [PMC free article] [PubMed] [Google Scholar]
- 66.Trivedi JK, Gupta AK. A study of patients attending emergency out-patient services of a large teaching institution. Indian J Psychiatry. 1982;24:360–5. [PMC free article] [PubMed] [Google Scholar]
- 67.Srinivasan K, Babu RK, Appaya P, Subrahmanyam HS. A study of inpatient referral patterns to a general hospital psychiatry unit in India. Gen Hosp Psychiatry. 1987;9:372–5. doi: 10.1016/0163-8343(87)90072-7. [DOI] [PubMed] [Google Scholar]
- 68.Doongaji DR, Nadkarni RP, Bhatawdekar ML. Psychiatric referrals in two general hospitals. J Postgrad Med. 1989;35:171–7. [PubMed] [Google Scholar]
- 69.De AK, Kar P. Psychiatric disorders in medical in-patients- A study in a teaching hospital. Indian J Psychiatry. 1998;40:73–8. [PMC free article] [PubMed] [Google Scholar]
- 70.Bagadia VN, Nayak DV, Havaldar PP, Pradhan PV, Shah LP, Dhirwani MK. Diabetes mellitus a psychosomatic study of 100 cases. Indian J Psychiatry. 1974;16:83–90. [Google Scholar]
- 71.Dass J, Dhavale HS, Rathi A. Psychosocial profile of juvenile diabetes. Indian J Psychiatry. 1999;41:307–13. [PMC free article] [PubMed] [Google Scholar]
- 72.Jainer A, Sharma M, Agarwal CG, Singh B. Frequency and severity of depressive symptoms among diabetic patients. Indian J Psychiatry. 1992;34:162–7. [PMC free article] [PubMed] [Google Scholar]
- 73.Mishra DN, Shukla GD. Sexual disturbances in male diabetics: Phenomenological and clinical aspects. Indian J Psychiatry. 1988;30:135–43. [PMC free article] [PubMed] [Google Scholar]
- 74.Parveen S, Singh SB. Stress and adjustment in Diabetes Mellitus. Indian J Psychiatry. 1999;41:66–9. [PMC free article] [PubMed] [Google Scholar]
- 75.Sanyal D, Basu J. The role of life events in short term metabolic control of non-insulin dependent diabetes mellitus. Indian J Psychiatry. 1998;40:350–6. [PMC free article] [PubMed] [Google Scholar]
- 76.Edwin T, Nammalvar N, Sabhesan S, Ganesh R, Devarajan H. Neurocognitive impairments in HIV Infection. Indian J Psychiatry. 1999;41:30–6. [PMC free article] [PubMed] [Google Scholar]
- 77.Satapathy R, Krishna M, Babu AM, Vijayagopal M. A study of psychiatric manifestations of physically asymptomatic HIV-I seropositive individuals. Indian J Psychiatry. 2000;42:427–33. [PMC free article] [PubMed] [Google Scholar]
- 78.Thakur LC, Anand KS, Sagar RS. Neuropsychiatric and psychological aspects related to Human Immuno Deficiency Virus (HIV) infection. Indian J Psychiatry. 1992;34:114–23. [PMC free article] [PubMed] [Google Scholar]
- 79.Rao VA, Swaminathan R, Venkataram MK, Ramajayam S, Parhee R, Kumar N, et al. A clinical and behavioral study of HIV infected subjects – A comparison with STD subjects. Indian J Psychiatry. 1991;33:95–103. [PMC free article] [PubMed] [Google Scholar]
- 80.Bathla M, Murthy KK, Chandna S. Cognitive dysfunctions in intensive cardiac care unit. Indian J Psychiatry. 2010;52:159–63. doi: 10.4103/0019-5545.64598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Bhargava SC, Sharma SN, Agarwal BV. Neuroticism profile in coronary artery disease. Indian J Psychiatry. 1980;22:61–2. [PMC free article] [PubMed] [Google Scholar]
- 82.Cornelio N, Sarada Menon M, Senthilnathan Myocardial infarction-psychological study. Indian J Psychiatry. 1977;19:27–31. [Google Scholar]
- 83.Kidson MA. Personality factors in hypertension. Indian J Psychiatry. 1972;14:235–6. doi: 10.3109/00048677109159638. [DOI] [PubMed] [Google Scholar]
- 84.Lal N, Ahuja RC. Perception of distress by patients of myocardial infarction. Indian J Psychiatry. 1987;29:259–62. [PMC free article] [PubMed] [Google Scholar]
- 85.Madhukar, Prakash R, Ahuja RC, Lal N. A Psychosocial study of essential hypertension. Indian J Psychiatry. 1979;21:109–13. [Google Scholar]
- 86.Ramachandran V, Parikh GJ, Srinivasan V. Depression in hypertensive subjects. Indian J Psychiatry. 1983;25:260–3. [PMC free article] [PubMed] [Google Scholar]
- 87.Saldanha D, Goel DS, Rathee SP, Chawla ML. Personality profiles of coronary cases. Indian J Psychiatry. 1993;35:197–9. [PMC free article] [PubMed] [Google Scholar]
- 88.Pershad D, Verma SK, Wig NN, Wahi PL. Measures of neuroticism and prediction of psychiatric disturbances in patients awaiting cardiac surgery. Indian J Psychiatry. 1972;14:131–5. [Google Scholar]
- 89.Pestonjee DM, Bagchi R. Need patterns among coronary patients. Indian J Psychiatry. 1978;20:193–5. [Google Scholar]
- 90.Chatterjee AK, Dayal S. Concepts of “Cerebral Arteriosclerosis” and a Comparative Study with Duvadilan and Entodon. Indian J Psychiatry. 1965;7:160–6. [Google Scholar]
- 91.Srivastava ON, Singh G. Personality profile in neurodermatitis. Indian J Psychiatry. 1977;19:71–6. [Google Scholar]
- 92.Ayyar KS, Bagadia VN. A controlled study of psychosocial factors in neurodermatitis. Indian J Psychiatry. 1986;28:155–8. [PMC free article] [PubMed] [Google Scholar]
- 93.Chaudhury S, Das AL, John RT, Ramadasan P. Psychological factors in psoriasis. Indian J Psychiatry. 1998;40:295–9. [PMC free article] [PubMed] [Google Scholar]
- 94.Kulhara P, Marwaha R, Das K, Aga VM. Burden of care in patents of children suffering from haematological malignancies. Indian J Psychiatry. 1998;40:13–20. [PMC free article] [PubMed] [Google Scholar]
- 95.Kulhara P, Verma SC, Bambery P, Nehra R. Psychological aspects of haematological malignancies. Indian J Psychiatry. 1990;32:279–84. [PMC free article] [PubMed] [Google Scholar]
- 96.Wig NN. Psycho-social aspects of family planning. Indian J Psychiatry. 1968;10:29–35. [Google Scholar]
- 97.Sethi BB, Nathawat SS. Personality and family planning. Indian J Psychiatry. 1973;15:20–8. [PubMed] [Google Scholar]
- 98.Sawhney N, Nathawat SS, Sethi BB. A longitudinal study in family planning. Indian J Psychiatry. 1970;12:155–68. [Google Scholar]
- 99.Subramaniam G, Subramanian SK, Charles SX, Verghese A. Psychiatric aspects of hysterectomy. Indian J Psychiatry. 1982;24:75–9. [PMC free article] [PubMed] [Google Scholar]
- 100.Vyas JN, Rathore RS, Sharma P, Singhal AK. A study of psychiatric aspects of hysterectomy. Indian J Psychiatry. 1989;31:83–9. [PMC free article] [PubMed] [Google Scholar]
- 101.Bhatia MS, Kaur N, Bohra N, Goyal U. Psychiatric reactions in hysterectomy. Indian J Psychiatry. 1990;32:52–6. [PMC free article] [PubMed] [Google Scholar]
- 102.Thara R, Ramachandran V, Hassan M. Psychological aspects of infertility. Indian J Psychiatry. 1986;28:329–34. [PMC free article] [PubMed] [Google Scholar]
- 103.Sharma RG, Bhaskaran K. Attitude study of I.U.C.D cases from the psychiatric point of view. Indian J Psychiatry. 1968;10:12–6. [Google Scholar]
- 104.Prakash IJ, Murthy VN. Psychiatric morbidity and the menopause. Indian J Psychiatry. 1981;23:242–6. [PMC free article] [PubMed] [Google Scholar]
- 105.Wig NN, Kaur R, Paricha S, Devi PK. Psychological sequelae of medical termination of pregnancy. Indian J Psychiatry. 1978;20:254–61. [Google Scholar]
- 106.Upadhyaya M, Chaturvedi SK. A study of pre-menopausal psychiatric disorders. Indian J Psychiatry. 1988;30:173–6. [PMC free article] [PubMed] [Google Scholar]
- 107.Shah DK, Wig NN, Akhtar S. Status of post partum mental illnesses in psychiatric nosology: A Study of 102 Cases. Indian J Psychiatry. 1971;13:14–20. [Google Scholar]
- 108.Bhat VK, Srivastava ON, Gauba S, Prakash A. Personality characteristics of patients attending the Gynaecology outpatients of a general hospital. Indian J Psychiatry. 1977;19:77–81. [Google Scholar]
- 109.Verghese A. The syndrome of premenstrual psychosis. Indian J Psychiatry. 1963;5:160–3. [Google Scholar]
- 110.Dash S, Dash B. A comparative study of accepters and rejecters of psychiatric referrals for medical termination of pregnancy. Indian J Psychiatry. 1979;21:149–52. [Google Scholar]
- 111.Sood M, Sood AL. Depression in pregnancy and post-partum period. Indian J Psychiatry. 2003;45:48–51. [PMC free article] [PubMed] [Google Scholar]
- 112.John J, Seethalakshmi, Charles SX, Verghese A. Psychiatric disturbance during the postpartum period: A prospective study. Indian J Psychiatry. 1977;19:40–3. [Google Scholar]
- 113.Dube KC. Incidence of psychoses after childbirth. Indian J Psychiatry. 1952;3:129–32. [Google Scholar]
- 114.Sharma RG, Bhaskaran K. Religious attitudes towards family planning. Indian J Psychiatry. 1970;12:48–57. [Google Scholar]
- 115.Abhyankar RR, Bagadia VN. A psychiatric study of metropathia haemorrhagica. Indian J Psychiatry. 1979;21:328–31. [Google Scholar]
- 116.Rao AV. Vasectomy as a family planning procedure: Some psychiatric aspects. Indian J Psychiatry. 1968;10:198–202. [Google Scholar]
- 117.Wig NN, Singh S, Sahasi G, Isaac P. Psychiatric symptoms following vasectomy. Indian J Psychiatry. 1970;12:169–76. [PubMed] [Google Scholar]
- 118.Takrani LB. Untoward psychological effects of sterlization. Indian J Psychiatry. 1968;10:17–21. [Google Scholar]
- 119.Sabhesan S, Arumugham R, Natarajan M. Clinical indices of head injury and memory impairment. Indian J Psychiatry. 1990;3:313–7. [PMC free article] [PubMed] [Google Scholar]
- 120.Agnihotri BR, Teja JS, Prabhu GG, Virmani V. A study of psychiatric, psychological and social disturbances in epileptics. Indian J Psychiatry. 1972;14:171–82. [Google Scholar]
- 121.Bagadia VN, Jeste DV, Charegaonkar AS, Pradhan PV, Shah LP. A psycho-social study of 180 cases of epilepsy. Indian J Psychiatry. 1973;15:391–401. [Google Scholar]
- 122.Sikdar AK, Kar SK. Some observations on behaviour of epileptics. Indian J Psychiatry. 1972;14:162–70. [Google Scholar]
- 123.Shukla GD, Katiyar SC. Psychiatric disorders in children with temporal lobe epilepsy: A controlled investigation. Indian J Psychiatry. 1981;23:62–5. [PMC free article] [PubMed] [Google Scholar]
- 124.Mishra BP, Mahajan R, Dhanuka A, Narang RL. Neuro-psychological profile of epilepsy on Luria-Nebraska neuropsychological battery. Indian J Psychiatry. 2002;44:53–6. [PMC free article] [PubMed] [Google Scholar]
- 125.Jacob R, Kumar SM, Rajkumar R, Palaniappan V. A study to assess depression, its correlates and suicidal behavior in epilepsy. Indian J Psychiatry. 2001;44:161–4. [PMC free article] [PubMed] [Google Scholar]
- 126.Rao VA, Mahendran N, Gopalakrishnan C, Reddy K, Prabhakar ER, Swaminathnan R, et al. One hundred female burns cases: A study in suicidology. Indian J Psychiatry. 1989;31:43–50. [PMC free article] [PubMed] [Google Scholar]
- 127.Prasad CE, Krishnamurthy K, Murthy KJ. Psychiatric disorders in patients receiving anti-tuberculosis drugs. Indian J Psychiatry. 1985;27:311–4. [PMC free article] [PubMed] [Google Scholar]
- 128.Mathau JP, Ravindran P, Joshi P, Sundaram P. Psychiatric morbidity in pulmonary tuberculosis: A clinical study. Indian J Psychiatry. 1981;23:66–8. [PMC free article] [PubMed] [Google Scholar]
- 129.Sreedhar KP. Manifest anxiety in bronchial asthma. Indian J Psychiatry. 1989;31:311–4. [PMC free article] [PubMed] [Google Scholar]
- 130.Ramachandran V, Thiruvengadam KV, Zackria MG. Parental loss and emotional factors in bronchial asthma. Indian J Psychiatry. 1977;19:44–7. [Google Scholar]
- 131.Chakraborty A, Banerji G, Sandal B. Depressive reaction in children following short fever: An original report. Indian J Psychiatry. 1977;19:83–8. [Google Scholar]
- 132.Chatterjee RN, Nandi DN, Banerjee G, Sen B, Mukherjee A, Banerjee G. The social and psychological correlates of leprosy. Indian J Psychiatry. 1989;31:315–8. [PMC free article] [PubMed] [Google Scholar]
- 133.Verma KK, Gautam S. Effect of Rehabilitation on the prevalence of psychiatric morbidity among leprosy patients. Indian J Psychiatry. 1994;36:183–6. [PMC free article] [PubMed] [Google Scholar]
- 134.Chaturvedi SK. Psychiatric aspects of renal transplantation. Indian J Psychiatry. 1985;27:77–81. [PMC free article] [PubMed] [Google Scholar]
- 135.Kuruvilla K, Mohan Rao M, Johny KV. Psychiatric aspects of renal transplantion-1: Some observations on recipients. Indian J Psychiatry. 1975;17:26–32. [Google Scholar]
- 136.Kurvilla K, Pandey AP, Shastry JC. Psychiatric aspects of renal transplantation observations on donors. Indian J Psychiatry. 1979;21:155–8. [Google Scholar]
- 137.Guha P, De A, Ghosal M. Behavior profile of children with nephrotic syndrome. Indian J Psychiatry. 2009;51:122–6. doi: 10.4103/0019-5545.49452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Pawar AA, Rathod J, Chaudhury S, Saxena SK, Saldanha D, Ryali VS, et al. Cognitive and emotional effects of renal transplantation. Indian J Psychiatry. 2006;48:21–6. doi: 10.4103/0019-5545.31614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Haroon EA. Psychiatric disturbances following stroke. Indian J Psychiatry. 1986;28:335–41. [PMC free article] [PubMed] [Google Scholar]
- 140.Kar N, John SP. Site of Stroke: Correlation with cognitive deficits, symptoms of anxiety and depression, and quality of life. Indian J Psychiatry. 2003;45:218–20. [PMC free article] [PubMed] [Google Scholar]
- 141.Purandare N. Prevention of dementia: Role of vascular risk factors and cerebral emboli. Indian J Psychiatry. 2009;51:39–43. [PMC free article] [PubMed] [Google Scholar]
- 142.Kumar R, Datta S, Jayaseelan L, Gnanmuthu C, Kuruvilla K. The psychiatric aspects of Wilson's disease - A study from a neurology unit. Indian J Psychiatry. 1996;38:208–11. [PMC free article] [PubMed] [Google Scholar]
- 143.Menawat AS, Purohit DR, Joshi CK. Prevalence of psychiatric morbidity in acute intermittent porphyria. Indian J Psychiatry. 1979;21:58–9. [Google Scholar]
- 144.Narayanan HS, Mohan KS, Jayasimha N, Sridhara Rama Rao BS. A clinical and biochemical study of the mucopolysaccharidoses. Indian J Psychiatry. 1987;29:123–6. [PMC free article] [PubMed] [Google Scholar]
- 145.Narayanan HS, Mohan KS, Jayasimha N, Sridhara Rama Rao BS. Some Paradoxical observations noted in the prevalence of Hurler's and Hunter's syndrome. Indian J Psychiatry. 1987;29:169–70. [PMC free article] [PubMed] [Google Scholar]
- 146.Narayanan HS, Sridhara Rama Rao BS, Rao MP, Subbarishna DK. Clinical and genetic studies in cases of phenylketonuria (PKU) and a report of Follow up after dietary therapy. Indian J Psychiatry. 1988;30:123–7. [PMC free article] [PubMed] [Google Scholar]
- 147.Pandey RS, Swamy HS, Sreenivas KN, John CJ. Depression in Wilson's disease. Indian J Psychiatry. 1981;23:82–5. [PMC free article] [PubMed] [Google Scholar]
- 148.Virman V, Devi GM, Sawhney BB. Psychiatric symptoms in organic brain disease. Indian J Psychiatry. 1967;9:41–8. [Google Scholar]
- 149.Shukla GD, Srivastava RP. Pre-operative anxiety and its management in dentistry. Indian J Psychiatry. 1981;23:254–5. [PMC free article] [PubMed] [Google Scholar]
- 150.Singh MV, Anand NK, Dhingra DG, Gupta S. Intelligence in relation to duration of protein calorie malnutrition. Indian J Psychiatry. 1977;19:52–4. [Google Scholar]
- 151.Galgali RB, Rao S, Ashok MV, Appaya P, Srinivasan K. Psychiatric diagnosis of self poisoning cases: A general hospital study. Indian J Psychiatry. 1998;40:254–9. [PMC free article] [PubMed] [Google Scholar]
- 152.Pillai KV. Psychological influence on erythrocyte sedimentation rate. Indian J Psychiatry. 1962;4:46–9. [Google Scholar]
- 153.Somasundaram O, Vaidyalingam M. Tuberous Sclerosis- A report of 12 Cases. Indian J Psychiatry. 1966;8:311–25. [Google Scholar]
- 154.Chaudhury S, Dinker NL, Sharma AK. Psychophysiological evaluation of leg fracture patients. Indian J Psychiatry. 1998;40:46–9. [PMC free article] [PubMed] [Google Scholar]
- 155.Bhojak MM, Nathawat SS. Body image, hopelessness and personality dimensions in lower limb amputees. Indian J Psychiatry. 1988;30:161–5. [PMC free article] [PubMed] [Google Scholar]
- 156.Mall CP, Trivedi JK, Mishra US, Sharma VP, Dalal PK, Katiyar M, et al. Psychiatric Sequelae of Amputation: I Immediate Effects. Indian J Psychiatry. 1997;39:313–7. [PMC free article] [PubMed] [Google Scholar]
- 157.Srivastava S, Trivedi JK, Mall CP, Mishra US, Sharma VP, Dalal PK, et al. Psychosocial aspects of Amputation. Indian J Psychiatry. 1997;39:247–50. [PMC free article] [PubMed] [Google Scholar]
- 158.Trivedi JK, Mall CP, Mishra US, Sharma VP, Dalal PK, Katiyar M, et al. Psychiatric Sequelae of Amputation: II Long Term Effects. Indian J Psychiatry. 1997;39:318–23. [PMC free article] [PubMed] [Google Scholar]
- 159.Khurana P, Sharma PS, Avasthi A. Prevalence of Delirium in Geriatric Hospitalized General Medical Population. Indian J Psychiatry. 2002;44:41–6. [PMC free article] [PubMed] [Google Scholar]
- 160.Khurana P, Sharma PS, Avasthi A. Risk factors in delirious geriatric general medical patients. Indian J Psychiatry. 2002;44:266–72. [PMC free article] [PubMed] [Google Scholar]
- 161.Sabhesan S, Natarajan M. Post traumatic hyperactive delirium. Indian J Psychiatry. 1990;32:309–12. [PMC free article] [PubMed] [Google Scholar]
- 162.Dutta KS. Personality and peptic ulcer. Indian J Psychiatry. 1978;20:244–6. [Google Scholar]
- 163.Arun P, Vyas JN, Rai RR, Kanwal K, Sushil CS. Psychological and sociodemographic correlates of the Irritable Bowel Syndrome. Indian J Psychiatry. 1993;35:193–6. [PMC free article] [PubMed] [Google Scholar]
- 164.Chakraborty PK, Shah AV, Parikh NK. Psychiatric factors in ulcerative colitis. Indian J Psychiatry. 1983;25:219–22. [PMC free article] [PubMed] [Google Scholar]
- 165.Rajagopalan M, Kurian G, John JK. Psychological aspects of irritable bowel syndrome. Indian J Psychiatry. 1996;38:217–24. [PMC free article] [PubMed] [Google Scholar]
- 166.Shulka GD, Mishra DN, Agarwal AK. Non-organic dyspepsia: A controlled psychosomatic study. Indian J Psychiatry. 1982;24:280–3. [PMC free article] [PubMed] [Google Scholar]
- 167.Vishnar A, Ghulam R, Mittal RK. Non ulcer dyspepsia and its correlation with life stress, anxiety and depression. Indian J Psychiatry. 1999;41:88–93. [PMC free article] [PubMed] [Google Scholar]
- 168.Amruthraj B, Mishra H, Kumaraiah V. Autogenic therapy in tension headache. Indian J Psychiaty. 1987;29:239–42. [PMC free article] [PubMed] [Google Scholar]
- 169.Mehta M. Effects of relaxation therapy in management of muscular contraction headache in executives. Indian J Psychiatry. 1983;25:144–7. [PMC free article] [PubMed] [Google Scholar]
- 170.Rangaswami K. Personality and clinical manifestations of tension headache. Indian J Psychiatry. 1982;24:66–9. [PMC free article] [PubMed] [Google Scholar]
- 171.Wig NN. Psychogenic Headache. Indian J Psychiatry. 1964;6:18–21. [Google Scholar]
- 172.Sharma H, Shah S. Psychiatric comorbidity of headache in a medical relief camp in a rural area. Indian J Psychiatry. 2006;48:185–8. doi: 10.4103/0019-5545.31583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Kachhwaha SS, Chadda VS, Singhwal AK, Bhardwaj P. Psychiatric morbidity in patients with chronic abdominal pain. Indian J Psychiatry. 1994;36:170–2. [PMC free article] [PubMed] [Google Scholar]
- 174.Varma VK, Chaturvedi SK, Chari P. Sociodemographic study of patients with chronic pain. Indian J Psychiatry. 1986;28:119–25. [PMC free article] [PubMed] [Google Scholar]
- 175.Varma VK, Chaturvedi SK, Malhotra A, Chari P. Psychiatric aspects of chronic intractable pain. Indian J Psychiatry. 1983;25:173–9. [PMC free article] [PubMed] [Google Scholar]
- 176.Agarwal P, Khastgir U, Bhatia MS, Bohra N, Malik SC. Psychological profile of females with chronic pelvic pain. Indian J Psychiatry. 1996;38:212–6. [PMC free article] [PubMed] [Google Scholar]
- 177.Mehta BC, Bagadia VN, Vardhachari KS, Vahia NS. Subacute Progressive Encephalitis. Indian J Psychiatry. 1959;1:183–91. [Google Scholar]
- 178.Deo VR. Post-Influenzal Psychosis. Indian J Psychiatry. 1958;5:19–21. [Google Scholar]
- 179.Chaudhury S, Chakraborty PK, Gurunadh VS, Ratha P. Psychological reactions to cataract surgery with intraocular lens implantation. Indian J Psychiatry. 1995;37:165–8. [PMC free article] [PubMed] [Google Scholar]
- 180.Rajsekar K, Rajsekar YL, Chaturvedi SK. Psycho Ophthalmology: The interface between psychiatry and ophthalmology. Indian J Psychiatry. 1999;41:186–96. [PMC free article] [PubMed] [Google Scholar]
- 181.Narayanan HS, Keshavan MS, Ramakrishna M. Changing psychiatric manifestations of neurosyphilis over a period of 23 years. Indian J Psychiatry. 1980;22:94–6. [PMC free article] [PubMed] [Google Scholar]
- 182.Somasundaram O. Syphilis and mental deficiency. Indian J Psychiatry. 1967;9:137–44. [Google Scholar]
- 183.Verghese A, John S. Some observations on the clinical features of general paresis of insane. Indian J Psychiatry. 1972;14:137–42. [Google Scholar]
- 184.Varma LP. The incidence and clinical features of General Paresis. Indian J Psychiatry. 1952;3:141–63. [Google Scholar]
- 185.Varma LP. General paresis II: Diagnosis and course. Indian J Psychiatry. 1952;3:259–87. [Google Scholar]
- 186.Varma LP. General paresis III: Its prognosis. Indian J Psychiatry. 1952;3:345–64. [Google Scholar]
- 187.Varma VK, Chaturvedi SK, Malhotra A, Chari P. Psychiatric symptoms in patients with non-organic chronic intractable pain. Indian J Med Res. 1991;94:60–3. [PubMed] [Google Scholar]
- 188.Chandra PS, Chaturvedi SK. Cultural variations in attitudes toward menstruation. Can J Psychiatry. 1992;37:196–8. doi: 10.1177/070674379203700310. [DOI] [PubMed] [Google Scholar]
- 189.Chandra PS, Venkatasubramanian G, Thomas T. Infanticidal ideas and infanticidal behavior in Indian women with severe postpartum psychiatric disorders. J Nerv Ment Dis. 2002;190:457–61. doi: 10.1097/00005053-200207000-00006. [DOI] [PubMed] [Google Scholar]
- 190.Chaturvedi SK, Chandra PS. Sociocultural aspects of menstrual attitudes and premenstrual experiences in India. Soc Sci Med. 1991;32:349–51. doi: 10.1016/0277-9536(91)90114-r. [DOI] [PubMed] [Google Scholar]
- 191.Chaturvedi SK, Chandra PS, Issac MK, Sudarshan CY, Beena MB, Sarmukkadam SB, et al. Premenstrual experiences: The four profiles and factorial patterns. J Psychosom Obstet Gynaecol. 1993;14:223–35. doi: 10.3109/01674829309084444. [DOI] [PubMed] [Google Scholar]
- 192.Chaturvedi SK, Chandra PS, Prema SV, Issac MK, Sudarshan CY, Beena MB, et al. Detection of psychiatric morbidity in gynecology patients by two brief screening methods. J Psychosom Obstet Gynaecol. 1994;15:53–8. doi: 10.3109/01674829409025629. [DOI] [PubMed] [Google Scholar]
- 193.Chaturvedi SK, Chandra PS, Gururaj G, Pandian RD, Beena MB. Suicidal ideas during premenstrual phase. J Affect Disord. 1995;34:193–9. doi: 10.1016/0165-0327(95)00017-h. [DOI] [PubMed] [Google Scholar]
- 194.Babu GN, Subbakrishna DK, Chandra PS. Prevalence and correlates of suicidality among Indian women with post-partum psychosis in an inpatient setting. Aust N Z J Psychiatry. 2008;42:976–80. doi: 10.1080/00048670802415384. [DOI] [PubMed] [Google Scholar]
- 195.Varma D, Chandra PS, Thomas T, Carey MP. Intimate partner violence and sexual coercion among pregnant women in India: Relationship with depression and post-traumatic stress disorder. J Affect Disord. 2007;102:227–35. doi: 10.1016/j.jad.2006.09.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Chandra PS, Satyanarayana VA, Satishchandra P, Satish KS, Kumar M. Do men and women with HIV differ in their quality of life? A study from south India. AIDS Behav. 2009;13:110–7. doi: 10.1007/s10461-008-9434-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Chandra PS, Gandhi C, Satishchandra P, Kamat A, Desai A, Ravi V, et al. Quality of life in HIV subtype C infection among asymptomatic subjects and its association with CD4 counts and viral loads—A study from South India. Qual Life Res. 2006;15:1597–605. doi: 10.1007/s11136-006-9001-7. [DOI] [PubMed] [Google Scholar]
- 198.Chandra PS, Deepthivarma S, Jairam KR, Thomas T. Relationship of psychological morbidity and quality of life to illness-related disclosure among HIV-infected persons. J Psychosom Res. 2003;54:199–203. doi: 10.1016/s0022-3999(02)00567-6. [DOI] [PubMed] [Google Scholar]
- 199.Mattoo SK, Handa S, Kaur I, Gupta N, Malhotra R. Psychiatric morbidity in vitiligo: Prevalence and correlates in India. J Eur Acad Dermatol Venereol. 2002;16:573–8. doi: 10.1046/j.1468-3083.2002.00590.x. [DOI] [PubMed] [Google Scholar]
- 200.Mattoo SK, Handa S, Kaur I, Gupta N, Malhotra R. Psychiatric morbidity in vitiligo and psoriasis: A comparative study from India. J Dermatol. 2001;28:424–32. doi: 10.1111/j.1346-8138.2001.tb00004.x. [DOI] [PubMed] [Google Scholar]
- 201.Raval A, Dhanaraj E, Bhansali A, Grover S, Tiwari P. Prevalence and determinants of depression in type 2 diabetes patients in a tertiary care centre. Indian J Med Res. 2010;132:195–200. [PubMed] [Google Scholar]
- 202.Avasthi A, Grover S, Bhansali A, Das RJ, Gupta N, Sharan P, et al. Erectile Dysfunction in Diabetes Mellitus leads to Poor Quality of life. Int Rev Psychiatry. 2011;23:93–9. doi: 10.3109/09540261.2010.545987. [DOI] [PubMed] [Google Scholar]
- 203.Srinivasan K, Joseph W. A study of lifetime prevalence of anxiety and depressive disorders in patients presenting with chest pain to emergency medicine. Gen Hosp Psychiatry. 2004;26:470–4. doi: 10.1016/j.genhosppsych.2004.06.001. [DOI] [PubMed] [Google Scholar]
- 204.Mattoo SK, Bhansali AK, Gupta N, Grover S, Malhotra R. Psychosocial morbidity in Cushing disease: A study from India. Endocrine. 2009;35:306–11. doi: 10.1007/s12020-009-9182-2. [DOI] [PubMed] [Google Scholar]
- 205.Nehra R, Grover S, Bhansali A, Khehra N. Effect of corrective surgery on neurocognitive functions in endogenous cushing syndrome. Endocrinologist. 2009;19:205–7. [Google Scholar]
- 206.Mattoo SK, Bhansali AK, Gupta N, Grover S, Malhotra R. Psychosocial morbidity in acromegaly: A study from India. Endocrine. 2008;34:17–22. doi: 10.1007/s12020-008-9112-8. [DOI] [PubMed] [Google Scholar]
- 207.Grover S, Kumar V, Chakrabarti S. Comparative efficacy study of Haloperidol, Olanzapine and Risperidone in delirium. J Psychosom Res. 2011;71:277–81. doi: 10.1016/j.jpsychores.2011.01.019. [DOI] [PubMed] [Google Scholar]
- 208.Grover S, Chakrabarti S, Shah R, Kumar V. A factor analytic study of the Delirium Rating Scale-Revised-98 in untreated patients with delirium. J Psychosom Res. 2011;70:473–478. doi: 10.1016/j.jpsychores.2010.11.007. [DOI] [PubMed] [Google Scholar]
- 209.George C, Nair JS, Ebenezer JA, Gangadharan A, Christudas A, Gnanaseelan LK, et al. Validation of the Intensive Care Delirium Screening Checklist in nonintubated intensive care unit patients in a resource-poor medical intensive care setting in South India. J Crit Care. 2011 doi: 10.1016/j.jcrc.2010.11.002. [DOI] [PubMed] [Google Scholar]
- 210.Shyamsundar G, Raghuthaman G, Rajkumar AP, Jacob KS. Validation of memorial delirium assessment scale. J Crit Care. 2009;24:530–4. doi: 10.1016/j.jcrc.2008.12.016. [DOI] [PubMed] [Google Scholar]
- 211.Avasthi A, Varma SC, Kulhara P, Nehra R, Grover S, Sharma S. Diagnosis of common mental disorders by using PRIME-MD Patient Health Questionnaire. Indian J Med Res. 2008;127:159–64. [PubMed] [Google Scholar]
- 212.Sharma P, Avasthi A, Chakrabarti S, Varma S. Depression among hospitalized medically ill patients: A two-stage screening study. J Affect Disord. 2002;70:205–9. doi: 10.1016/s0165-0327(01)00311-1. [DOI] [PubMed] [Google Scholar]
- 213.Das PP, Grover S, Avasthi A, Chakrabarti S, Malhotra S, Kumar S. Intentional self-harm seen in psychiatric referrals in a tertiary care hospital. Indian J Psychiatry. 2008;50:187–91. doi: 10.4103/0019-5545.43633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214.Mohandas E, Sam PJ, Grover S. Physical illnesses in psychiatric disorders. In: Avasthi A, Mohandas E, Gautam S, Grover S, editors. Physical Health of Mentally ill. Indian Psychiatric Society; 2010. pp. 9–16. [Google Scholar]
- 215.Ingle GK, Nath A. Geriatric Health in India: Concerns and Solutions. Indian J Community Med. 2008;33:214–8. doi: 10.4103/0970-0218.43225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216.Chadda RK, Shome S. Psychiatric aspects of clinical practice in general hospitals: A survey of non-psychiatric clinicians. Indian J Psychiatry. 1996;38:86–93. [PMC free article] [PubMed] [Google Scholar]
- 217.Gupta R, Narang RL. Psychiatric training and its practice: A survey of 86 practitioners. Indian J Psychiatry. 1987;29:349–52. [PMC free article] [PubMed] [Google Scholar]


