Abstract
Mental disorders impose a massive burden in the society. The National Mental Health Programme (NMHP) is being implemented by the Government of India to support state governments in providing mental health services in the country. India is facing shortage of qualified mental health manpower for District Mental Health Programme (DMHP) in particular and for the whole mental health sector in general. Recognizing this key constraint Government of India has formulated manpower development schemes under NMHP to address this issue. Under the scheme 11 centers of excellence in mental health, 120 PG departments in mental health specialties, upgradation of psychiatric wings of medical colleges, modernization of state-run mental hospitals will be supported. The expected outcome of the Manpower Development schemes is 104 psychiatrists, 416 clinical psychologists, 416 PSWs and 820 psychiatric nurses annually once these institutes/ departments are established. Together with other components such as DMHP with added services, Information, education and communication activities, NGO component, dedicated monitoring mechanism, research and training, this scheme has the potential to make a facelift of the mental health sector in the country which is essentially dependent on the availability and equitable distribution mental health manpower in the country.
Keywords: Development, India, manpower, NMHP, program, scheme
INTRODUCTION
Mental disorders are significant public health issue and pose a tremendous socioeconomic burden on community. Neuropsychiatric conditions have an aggregate point prevalence of about 10% for adult population.[1]
About 450 million people are estimated to be suffering from neuropsychiatric conditions worldwide. In 1990, mental and neurological disorders accounted for 10% of the total DALYs lost due to all diseases and injuries. This increased to 12% in the year 2000 and an analysis of trends indicates that the burden will further increase to 15% by the year 2020.[2]
The resources available to tackle the huge burden of these disorders are insufficient, inequitably distributed and inefficiently used, which leads to a treatment gap of more than 75% in many countries with low and lower-middle class incomes.[3] Poor awareness about symptoms of mental illness, myths and stigma related to it, lack of knowledge on the treatment availability and potential benefits of seeking treatment are important causes for the high-treatment gap.
In India, the prevalence estimates vary between 5.82[4] to 7.3%.[5] In terms of absolute number suffering from mental illnesses, the prevalence estimate throws up a huge number of about 7 crore persons.
The median number of psychiatrists in India is only 0.2 per 100,000 population compared to a global median of 1.2 per 100,000 population. Similarly, the figures for psychologists, social workers and nurses working for mental health is 0.03, 0.03 and 0.05 per 100,000 population compared to a global median of 0.60, 0.40 and 2.00 per 100,000 population, respectively.[6]
Growing awareness regarding the magnitude of mental health problems in the country, a flurry of health activities in the late 70s which included Alma Ata Declaration, the commitment to provide health to all by 2000, and the realization that mental health care was possible through the existing primary health care system led to the launch of National Mental Health Programme (NMHP) by the Government of India in 1982.[7]
NMHP strives to ensure availability and accessibility of minimum mental health care for all in the near foreseeable future, particularly to the most vulnerable sections of the population; to encourage mental health knowledge and skills in general health care and social development; to promote community participation in mental health service development and to stimulate self-help in the community.[7]
In line with the National Health Policy 2002, the objectives of the NMHP and global trend of community care of mentally ill, a field-tested model of community mental health care was adopted as District Mental Health Programme (DMHP) for NMHP.[8,9] This community-based mental health care at district level was initiated in four districts in 1996 and it was extended to 27 districts across 22 states/UTs in the ninth 5-year plan. NMHP was restrategized during the tenth 5-year plan to incorporate expansion of DMHP to 100 districts all over the country, modernization of state-run mental hospitals, upgradation of Psychiatry wings in the Government medical colleges/general hospitals, IEC activities, research and training in mental health for improving service delivery. By the end of the tenth 5-year plan, DMHP was extended to 110 districts, upgradation of psychiatric wings of 71 medical colleges/general hospitals and modernization of 23 mental hospitals was funded. The program showed an increased allocation from Rs. 280 million in ninth 5-year plan to Rs. 1900 million in tenth 5-year plan period which was later reduced to Rs.1390 million.[10]
A series of reviews, consultations and evaluations revealed areas of concern in program implementation. Some of these concerns are:
Non-availability of psychiatrists and other mental health professionals like psychiatric social workers and clinical psychologists in many states for manning DMHPs.
Lack of delegation of power for procuring medicines and recruiting staff under the program at the district level.
The program was focused on catering mostly to severely mentally ill and many important issues like suicide prevention, workplace stress management, adolescent mental health and college counseling services which could benefit larger section of society and were not covered under DMHP thus making these important services inaccessible to the community.
Low level of community participation.
Lack of regular and dedicated monitoring and facilitating mechanism.
Lack of detailed operational guidelines for implementation of the schemes.
Lack of co-ordination between Department of Medical Education and Health Department at the State level lead to delays in implementation of DMHPs.
Some states were not able to take over the funding of DMHP activities after the completion of 5 years.
The foremost area of concern facing the program and mental health scene in the country is the shortage of skilled mental health professionals in the country.[11]
As against an estimated requirement of 11,500 psychiatrists, 17,250 clinical psychologists, 23,000 psychiatric social workers and 3000 psychiatric nurses only approximately 3000 psychiatrists, 500 clinical psychologists, 400 PSWs and 900 psychiatric nurses are available at present. The estimated figure is calculated using a norm of one psychiatrist per 100,000 population, 1.5 clinical psychologist per 100,000 population, two psychiatric social workers per 100,000 population and one psychiatric nurse per 10 psychiatric beds.[12] The existing training infrastructure in the country producesapproximately 320 psychiatrists, 50 clinical psychologists, 25 PSWs and 185 psychiatric nurses per year.[10]
Manpower development schemes in mental health for the 11th 5-year plan
To address the shortage of qualified mental health professionals it was thought necessary to have dedicated manpower development schemes in addition to continuing with the community care approach adopted under DMHP. These schemes are aimed at increasing the PG training capacity in the mental health specialties of psychiatry, clinical psychology, PSW and psychiatric nursing. The PG courses identified specifically to be supported under the scheme are MD/DPM/DNB in psychiatry, Diploma in psychiatric nursing, M.Phil. in clinical psychology and PSW. Ph.D in clinical psychology and PSW and M.Sc. in psychiatric nursing has been excluded from the scheme as they are of longer duration and usually candidates after completing these degrees go into teaching rather than into field-based programs. To support the expansion of DMHP and implement Manpower Development Schemes the allocation for NMHP during the 11th 5-year plan period has been raised to Rs. 10,000 million up from Rs. 1390 million in the last plan period. The schemes approved for addressing the Manpower concerns in mental health are as follows:
Centers of excellence in mental health
Also known as scheme A, this scheme aims at establishing centers of excellence in the field of mental health by upgrading and strengthening identified existing mental health hospitals/institutes for addressing the acute manpower gap and providing state of the art mental health care facilities during the current 5-year plan period. These institutes will focus on production of quality manpower in mental health with primary aim to fulfill manpower needs of the NMHP.
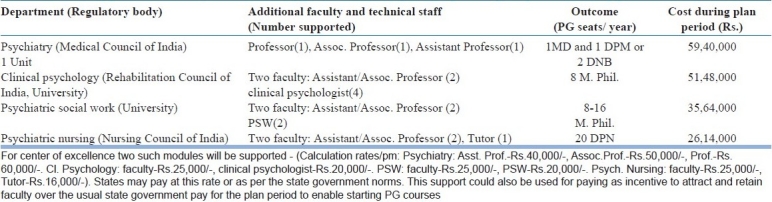
The support under the program would cover capital work (Academic block, Library, Hostel, Lab., Supportive departments, Lecture theatres, etc.), equipments and furnishing, support for induction and retention of additional faculty for the current plan period. Preference would be given to centers where the state government shows commitment for faculty and other recurring and necessary expenditure. This support for additional faculty could also be used for paying as incentive to attract and retain new faculty over the usual state government pay for the plan period to enable starting PG courses. Under support for engaging additional faculty, cost for two units of psychiatry, four faculty posts of clinical psychology, eight non-faculty posts of clinical psychology, four faculty posts of PSW, four non-faculty posts of PSW, two faculty posts of psychiatric nursing, one non-faculty post of psychiatric nursing has been provided at a competitive rate [Table 1].
Table 1.
Support for faculty – Critical support for meeting the regulatory requirement support for one module
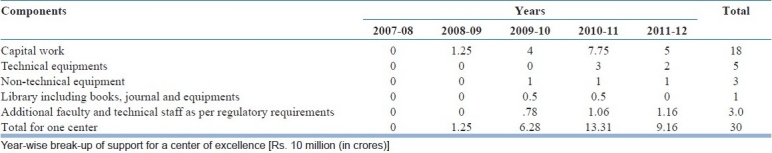
Budgetary support under the scheme is up to Rs. 300 million per center which will be need-based and assessed by a team of experts. [Table 2] The proposal for availing the scheme has to be routed through the state governments and must include a definite plan with timelines for initiating/ increasing PG courses in psychiatry, clinical psychology, PSW and psychiatric nursing.
Table 2.
Centres of excellence in mental health
It is planned to establish at least 11 centers of excellence in mental health under the scheme during the current plan period. This would result in increase in at least 44 PG seats in psychiatry, 176 M.Phil. seats in clinical psychology and PSW each and 220 seats in diploma in psychiatric nursing. Thus, a total of 616 qualified mental health professionals would be produced from these centers annually after they are established. After the current plan period, the concerned state governments is to take over the entire funding of these centers. Total budgetary allocation under this scheme is Rs. 3381.21 million.The centers which are being supported under this scheme are Institute of Mental Health-Hyderabad, Hospital for Mental Health-Ahmedabad, Institute for Mental Health and Hospital-Agra, Mental Health Institute-Cuttack,Institute of Psychiatry-Kolkata, Government Medical College-Chandigarh, State Mental Health Institute-Rohtak, Psychiatric Diseases Hospital- Srinagar, Institute of Mental health and Neurosciences (IMHANS)-Kozhikode, Institute of Human Behaviour & Allied Sciences-Delhi. One more center is awaiting the commitment of the concerned state government to avail grant under the scheme. A recent review of progress of the upgradation work of the centers of excellence in mental health funded under this scheme has revealed that the pace of work is slow and needs to be speeded up so that it is complete within the plan period.
Scheme for manpower development in mental health
Also known as scheme B, this scheme aims at development of PG training capacity on low input and high-output pattern. Vis-a-vis the scheme A this scheme is more cost-effective and would cover far more institutes. Under this scheme Government Medical Colleges/Government General Hospitals/state-run mental health institutes would also be supported for starting PG courses or increasing the intake capacity for PG training in mental health specialties. The support would involve limited amount of physical work for establishing/improving department in specialties’ of mental health (psychiatry, clinical psychology, PSW and psychiatric nursing), equipments, tools and basic infrastructure (hostel, library, department, etc.), support for engaging additional faculty. It is planned to support setting up/strengthening of 30 units of psychiatry, 30 departments of clinical psychology, 30 departments of PSW and 30 departments of psychiatric nursing during the plan period. The financial support will extend from up to Rs.5.1 million for each psychiatric nursing department to up to Rs. 10 million for each PG department of psychiatry [Table 3].
Table 3.
Cost of establishing/strengthening training departments in mental health (scheme B)
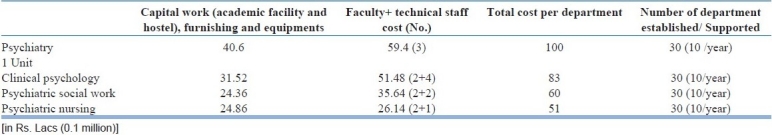
This scheme is expected to generate about 60 psychiatrists, 240 clinical psychologists, 240 PSWs and 600 psychiatric nurses per year. The support under this scheme is approved for the current plan period and it is expected that the concerned state government will take over the additional infrastructure at the end of the period. The proposal should have definite timelines for starting/increasing training seats in mental health specialties’. Total budgetary allocation under this scheme is Rs. 700 million. A total of 23 PG departments have been funded under this scheme and about 100 more PG departments could be taken up for upgradation in the plan period. The scheme provides a golden opportunity for initiating PG courses as well as increasing PG seats in mental health specialties.
Spill over activities of 10th 5-year plan
Spill over activities of 10th 5-year plan comprises two schemes viz. upgradation of psychiatric wings of Government Medical Colleges/ General Hospitals and modernization of state-run mental hospitals. Total allocation during the plan period is Rs. 580.3 million.
Upgradation of psychiatric wings of Government Medical Colleges/General Hospitals
Every medical college should ideally have a Department of Psychiatry with minimum of three faculty members and inpatient facilities of about 30 beds as per the norms laid down by the Medical Council of India. There should be outpatient facilities, as well as facilities for providing various forms of therapy including electroconvulsive therapy. In addition to psychiatrists, clinical psychologists, psychiatric social workers and psychiatric nurses are essential for an ideal psychiatric department in a medical college. Out of the existing medical colleges in the country, approximately one-third of them did not have adequate psychiatric services.
Looking at the huge manpower gap in the psychiatry and concerned disciplines, this scheme was adopted for upgradation of the UG and PG training in psychiatry in medical colleges. It is sought to upgrade the psychiatry wings by supporting:
Provision for independent psychiatry department in medical colleges where they did not exist
Upgradation of existing psychiatry services including provision of inpatient services, with necessary equipment; provision of trained manpower
The department of psychiatry to be responsible for implementing and providing support for execution of NMHP/DMHP
Facilities to train psychiatric social workers and nurses; provision for accreditation and licensing for health professionals
Provision of enhancing capacity of existing central/state-governmental institutes/colleges to train manpower.
Under this scheme one-time grant will be provided to the psychiatry departments of Government Medical Colleges which have not been funded earlier under NMHP. Some of the deserving areas, where there is no well-established Government Medical colleges, Government General hospitals/district hospitals could be funded for establishment of a psychiatry wing. The grant to be provided would cover non-recurring expenditure of up to Rs. 5 million per college for upgradation of facilities and equipments. Preference would be given to medical colleges/hospitals planning to start/increase PG seats (MD/DPM/DNB) in psychiatry.
Modernization of state-run mental hospitals
There are 43 state-run mental hospitals in the country. Out of them 29 mental hospitals have been funded for modernization and some still remain to be modernized. A one-time grant of up to Rs. 30 million per mental hospital would be provided to mental hospitals based upon submission of firmed up proposal under NMHP through the concerned state government for modernization of facilities and equipments from custodial to a modern therapeutic setup.
CONCLUSION
NMHP was launched in 1982 with very comprehensive objectives which stand true even today. National Health Policy 2002 recognised and incorporated the objectives and strategies of NMHP. DMHP was launched in 1996 with an aim to achieve the objectives of NMHP. DMHP was expanded and more components were added to make it more comprehensive. Eleventh plan period focuses on consolidation of achievements made under NMHP and seeks to address the biggest barrier in development of mental health services by addressing the manpower shortage in mental health. The strategy of upgrading psychiatric centers with into centers of excellence will address the manpower shortage to some extent and at the same time develop infrastructure for effective implementation of NMHP in their regions and make the concerned region self-sufficient in quality mental health care. The scheme B which is slated to give a better outcome in terms of increase in PG training seats in mental health as compared to scheme A focuses on the quantity of mental health human resource. Establishment of 120 PG departments as planned in the scheme will lead to spread of mental health training to many centers and increase the level of care available in addition to address the manpower shortage for the program and the country. Expansion of DMHP services along with manpower development will lead to creation of posts of mental health specialists in districts as well as in mental health institutions availing support under manpower development schemes.
Upgradation of psychiatric wings of government medical colleges will improve the UG as well as PG training facility in mental health leading ultimately to start of more PG training course in psychiatry. Many colleges have already availed of this grant and established full-fledged psychiatric ward, OPD and department. This has changed the perception of psychiatry as a discipline in patients and health professionals alike. Modernization of state-run mental hospitals which began in 2004 has improved the infrastructure and level of care of many custodial hospitals and many of these are now coming forward to avail grant under manpower development schemes to rise to a further higher level of services and care. These schemes are an opportunity to improve the mental health facilities and he departments and institutes which have not availed of this grant should avail of it at the earliest.
Slow work of projects funded under manpower development schemes and a luke warm response in taking up scheme B of manpower development scheme points towards dearth of leadership in mental health sector in the country and the danger of continuing with business as usual. To truely implement these schemes and achieve the scheme objectives it will require a vision to transform the mental health institutes/departments. Being the most knowledgeable about mental health it is the prime responsibility of the senior mental health professionals who are heading their departments to foster and spread the vision among all stakeholders in their area to develop their departments into a modern multidisciplinary teaching institutions.
Other issues like stigma, NGO participation, innovative pilot schemes, research, training in subspecialty areas, dedicated monitoring mechanism, support for statutory bodies in mental health, integration with other development sectors, preventive and promotive mental health services under DMHP are also being taken up earnestly. Together these developments have a potential to change the face of mental health in India and give us an opportunity to bring mental health from the shadows of darkness into sunshine.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Murray CJ, Lopez AD. Progress and directions in refining the global burden of disease approach: A response to Williams. Health Econ. 2000;9:69–82. doi: 10.1002/(sici)1099-1050(200001)9:1<69::aid-hec493>3.0.co;2-i. [DOI] [PubMed] [Google Scholar]
- 2.Mental Health: New Understanding, New Hope. Geneva: World Health Organization; 2001. The World health report; pp. 19–45. [Google Scholar]
- 3.mhGAP: Mental Health Gap Action Programme: Scaling up care for mental, neurological and substance use disorders. Geneva: World Health Organization; 2008. [PubMed] [Google Scholar]
- 4.Reddy MV, Chandrasekhar CR. Prevalence of mental and behavioural disorders in India: A meta-analysis. Indian J Psychiatry. 1998;40:149–57. [PMC free article] [PubMed] [Google Scholar]
- 5.Ganguli HC. Epidemiological finding on prevalence of mental disorders in India. Indian J Psychiatry. 2000;42:14–20. [PMC free article] [PubMed] [Google Scholar]
- 6.Mental Health Atlas. Geneva: World Health Organization; 2005. World Health Organization. [Google Scholar]
- 7.National Mental Health Programme for India. New Delhi: Ministry of Health and Family Welfare, Government of India; 1982. Directorate General of Health Services (DGHS) [Google Scholar]
- 8.Community Mental Health News. 11 and 12. Bangalore: NIMHANS; 1988. Apr-Sep. pp. 2–16. [Google Scholar]
- 9.National Mental Health Program: A Progress Report (1982-1990) Directorate General of Health Services, Ministry of Health and Family Welfare. 1990 [Google Scholar]
- 10.Salhan RN, Sinha SK, Kaur J. Asia Australia Community Mental Health Development Project, Asia Australia Mental Health. Melbourne: 2008. Country Report-India. [Google Scholar]
- 11.Kaur J, Sinha SK. Health Programme series 14, National Institute of Health and Family Welfare. New Delhi: 2008. National Mental Health Programme. [Google Scholar]
- 12.Goel DS, Agarwal SP, Ichhpujani RL, Shrivastava S. Mental Health 2003: The Indian Scene. In: Agarwal SP, Goel DS, Ichhpujani RL, Salhan RN, Shrivastava S, editors. Mental Health: An Indian Perspective, 1946–2003. New Delhi: Directorate General of Health Services; 2004. pp. 3–24. [Google Scholar]


