Abstract
Non-compaction cardiomyopathy is a recently recognized disorder, based on an arrest in endomyocardial morphogenesis. The disease is characterized by heart failure (both diastolic and systolic), systemic emboli and ventricular arrhythmias. The diagnosis is established by two-dimensional echocardiography. Isolated left ventricular non-compaction cardiomyopathy (IVNC) is an exceedingly rare congenital cardiomyopathy. Only a few cases of this condition have been reported. It is characterized by prominent and excessive trabeculation in a ventricular wall segment, with deep intertrabecular spaces perfused from the ventricular cavity. Echocardiographic findings are important clues for the diagnosis. We report a case of isolated non-compaction of the left ventricular myocardium presented with ventricular tachycardia.
Keywords: Isolated non-compaction cardiomyopathy, IVNC, non-compaction cardiomyopathy, ventricular tachycardia
INTRODUCTION
Non-compaction cardiomyopathy is a congenital pathological entity that can occur in isolated form or associated with other heart disease and often involves both ventricles. Non-compaction of ventricular myocardium is recently included in the 2006 classsification of cardiomyopathies as a genetic cardiomyopathy.
Isolated non-compaction cardiomyopathy is caused by a defect in cardiac morphogenesis resulting in an arrest of compaction of loose interwoven meshwork of myocardial fibers during intrauterine life, which results in severe systolic dysfunction as well as undue hypertrophy of the involved walls of the ventricles. Although the most frequent sites involved are left ventricular apex and inferior wall, involvement of other left ventricular walls and right ventricle has also been reported. The age of onset of symptoms ranges from infancy to the geriatric age.
Patients with isolated non-compaction cardiomyopathy have a high incidence of heart failure, arrhythmias, and thromboembolism. The most common presentation is congestive heart failure. Arrhythmias include atrial arrhythmias, ventricular tachycardia, and sudden cardiac death. A ratio of noncompacted to compacted myocardium greater than 3 and involvement of three or more segments are indicators of poor prognosis. Since the clinical manifestations are not sufficient to establish diagnosis, echocardiography is the diagnostic tool that makes it possible to document ventricular non-compaction and establish prognostic factors.
CASE PRESENTATION
A-25-year-old female presented to the emergency department with history of palpitations, sweating, syncope and breathlessness of sudden onset. There was history of intermittent similar episodes of breathlessness and palpitations over the last two years at rest. There was no history of drug intake or joint pain. There was no history of chest pain, hypertension or diabetes mellitus. The patient was previously diagnosed as hypertrophic cardiomyopathy by transthoracic echocardiography six months prior to admission. There was no history of significant medical illness.
On examination the pulse rate was 200 beats per minute, respiratory rate was 24 per minute, and blood pressure was 80/ 60 mmHg. The patient was immediately shifted to the coronary care unit for further management. The oxygen saturation (SpO2) was 77%. On auscultation, the heart sounds were soft and there was gallop rhythm with fine rales at bases of both lung fields. JVP was raised with mild hepatomegaly and mild pedal edema. Electrocardiogram showed sustained ventricular tachycardia with rate of 230/ minute. Chest X-ray showed an enlarged cardiac shadow and pulmonary congestion. Laboratory investigations: Hemoglobin was 11.4 gm%. The total WBC count was 7800 with normal differentiation. Renal and liver functions were within normal limits. Serum electrolytes (sodium, potassium, calcium and magnesium) were within normal range. Arterial blood gas analysis (ABGA) was suggestive of mild respiratory acidosis.
Hospital course: Ventricular tachycardia was treated with emergency electrical cardioversion. Considering the hemodynamic instability and life threatening arrhythmia with respiratory insufficiency, the patient was intubated and put on artificial ventilator. Supportive treatment was given in the form of inotrophic agents, antibiotics and proton pump inhibitors. After two hours, the patient was weaned from the ventilator and extubated.
After stabilization, the patient underwent transthoracic Doppler echocardiographic examination, with findings suggestive of isolated left ventricular non-compaction cardiomyopathy. The overall LVEF by Simpson's method was 55%. There was grade I diastolic dysfunction by Pulse Wave Doppler and tissue Doppler imaging. There was mild mitral regurgitation and mild tricuspid regurgitation. Pulmonary artery pressure (PAP) was normal (14.5 mmHg).
A 2-layered structure of the left ventricular wall with an end-systolic ratio of the noncompacted to the compacted layer was >2. The segments involved in left ventricular non-compaction were the left ventricular (LV) apex. (LV) lateral wall, anterior wall and mid-ventricular areas. The direct blood flow was from the ventricular cavity into the deep intertrabecular recesses, as assessed by color Doppler echocardiography with six prominent trabaculae. There was severe concentric type LV hypertrophy (LVPW: 17.2 mm and IVSd: 17.1 mm).
Color Doppler was used to establish the continuity of flow between the chamber and the intertrabecular recesses and to evaluate the distribution of the prominent trabeculae in the left ventricle. There was no resting regional wall motion abnormality (RWMA), no vegetations, no clot and no pericardial effusion. The great arteries were normal. Interatrial septum (IAS) and interventricular septum (IVS) were intact. There were no associated cardiac abnormalities. [Figures 1–3].
Figure 1.
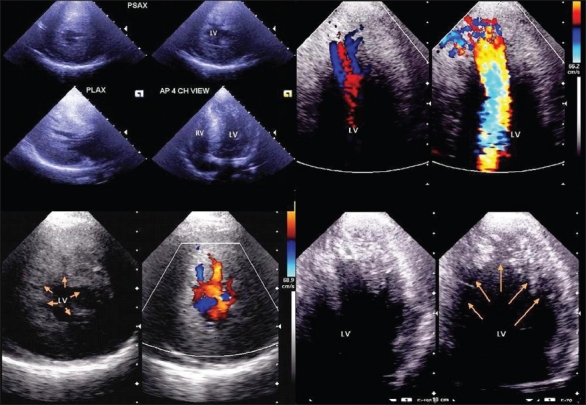
Transthoracic two-dimensional apical four chamber (AP-4-CH view), parasternal long axis (PLAX) and parasternal short axis (PSAX) images show, isolated non-compaction of left ventricle with multiple trabeculae and intertrabecular recesses in lateral, anterior walls, middle and apical portions of the septum and apex of the left ventricle with severe concentric left ventricular hypertrophy
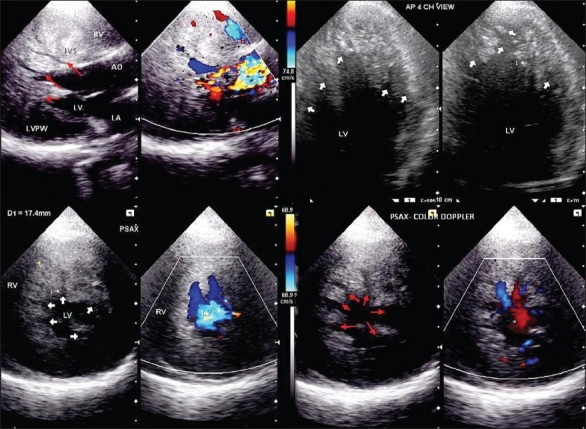
Figure 3.
Two-dimensional echocardiogram in apical four chamber zoom view (AP-4-CH view), parasternal long axis (PLAX) and parasternal short axis (PSAX) shows color Doppler images at the level of both ventricles that demonstrate the noncompacted:compacted wall ratio and how the color enters the intertrabecular recesses
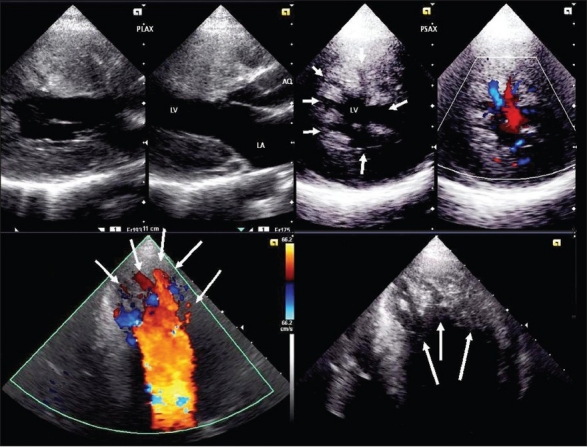
Figure 2.
Transthoracic two-dimensional echocardiogram in apical four chamber (AP-4-CH view), parasternal short axis (PSAX) and parasternal long axis (PLAX) shows deep trabeculae and intertrabecular recesses in the lateral, anterior walls, middle and apical portions of the septum and apex of the left ventricle
The patient was put on amiodarone and diuretic treatment. After seven days of hospitalization the patient was discharged and advised to continue amiodarone, ACE inhibitors and diuretic. The prognosis, complications, and need of cardioverter-defibrillation implantation was explained to the patient. We also advised echocardiography screening of first relatives considering the familial association of IVNC.
DISCUSSION
The incidence of non-compaction cardiomyopathy is estimated as 0.05% in adults. Non-compaction of the left ventricular myocardium is the result of an arrest in compaction of myocardial fibers during embryogenesis. It is most frequently observed in the left ventricle but the right ventricle can also be affected.[1] The disorder is diagnosed by two-dimensional echocardiography or magnetic resonance imaging, showing large prominent trabeculations and deep intertrabecular recesses, in which flow can be observed. In addition, the two-layered wall structure (thin compacted epicardium and thick, non-compacted endocardium) is essential for the diagnosis.[1]
Nilda et al, in their study quoted a prevalence of noncompacted cardiomyopathy as 4/10,000/5 years. While 77% of patients were in functional class I/II, the remaining 33% manifested frank congestive heart failure. Ventricular arrhythmias (premature ventricular contractions and short runs of ventricular tachycardia) were documented in more than a third of the patients.[2]
Jenni et al.[3] established four morphologic criteria for echocardiographic diagnosis that allow accurate differentiation from other forms of left ventricular hypertrophy. Echocardiography has been shown to be the method of choice in diagnosis of IVNC. The diagnostic criteria can be summarized as: 1) appearance of at least four prominent trabeculations and deep intertrabecular recesses; 2) appearance of blood flow from the ventricular cavity into the intertrabecular recesses as visualized by color Doppler imaging; 3) the segments of noncompacted myocardium mainly involve the apex and the inferior-mid and lateral-mid of the left ventricular wall and typically show a two-layered structure with an endsystolic ratio greater than two between the noncompacted subendocardial layer and the compacted subepicardial layer; 4) absence of coexisting cardiac abnormalities. Similarly, the patient in our case report had left ventricular non-compaction involving the left ventricle (LV) apex, LV lateral wall, anterior wall and mid-ventricular areas. The direct blood flow was from the ventricular cavity into the deep intertrabecular recesses, as seen by color Doppler echocardiography with six prominent trabeculae.
In the study by Nilda et al[2] ventricular non-compaction was an isolated finding in 74% of cases. Noncompacted ventricular myocardium involved only the left ventricle in 62% of the patients and both ventricles in 38%. The presence of ventricular non-compaction in more than three segments was associated with a functional class greater than II and ventricular arrhythmia. In their study, Holter monitoring showed premature ventricular contractions in 32% and sustained ventricular tachycardia in 7.5%. Similarly in our patient, the patient had more than three segments involved with noncompacton on echocardiography with episode of sustained ventricular tachycardia.[3]
Ritter M et al[4] in his nine-year echocardiographic study of 37,555 subjects, identified only 17 cases of IVNC in adult subjects (14 men and 3 women, 18 to 71 years of age). Although the diagnosis of IVNC in an adult population is often delayed because of similarities with more frequently diagnosed conditions, two-dimensional echocardiography will facilitate the diagnosis of IVNC in this subset of patients. Because of the high incidence of heart failure, ventricular arrhythmias, and embolization in adults with IVNC, early diagnosis is important. The patient in our case report was previously diagnosed as hypertrophic cardiomyopathy. Aragona P et al[5] also stated that non-compaction of the left ventricular myocardium is an uncommon finding and remains frequently overlooked and screening with echocardiography of first relatives is recommended, because of its familial association.
Khan IA et al[6] stated that the end-stage congestive heart failure is managed with heart transplantation and potential life-threatening ventricular tachyarrhythmias with an implantable cardioverter defibrillator. Prognosis is poor and the common causes of death are intractable heart failure and sudden cardiac death. Coppola G et al[7] stated that Isolated non-compaction of the ventricular myocardium (INVM) is often associated with systolic dysfunction and ventricular dilatation. The incidence of malignant ventricular arrhythmias in as many as 47% of the patients and sudden cardiac death in almost 50% of them supported our decision to implant cardioverter-defibrillator. Okçün Baniş et al,[8] described a case of isolated non-compaction of the ventricular myocardium in a 20-year-old man who presented initially with ventricular tachycardia similar to our case report.
In a study of 238 patients affected by non-compaction, Fazio G et al,[9] only 11 patients had documented ventricular tachycardia, which was sustained in two cases and non-sustained in nine.
CONCLUSIONS
In conclusion, a high index of suspicion for non-compaction is necessary as the condition may lead to serious heart failure, thrombo-embolic events, ventricular tachyarrythmias or death. Early recognition of non-compaction may give better follow-up and management of patients with this condition.
Non-compacted cardiomyopathy is a congenital malformation that can occur as an isolated entity or associated with other pathologies of the heart and can often involve both ventricles. A ratio of noncompacted:compacted wall greater than 3 and involvement of three or more segments are signs of poor prognosis associated with greater clinical deterioration (functional class III/IV) and ventricular arrhythmias.
The clinical picture does not provide sufficiently specific evidence to establish the diagnosis. Echocardiography is the diagnostic cornerstone. Treatment should be directed towards prevention and management of heart failure, ventricular arrhythmias and prevention of thromboembolic events. The long-term prognosis of non-compaction cardiomyopathy is poor.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Maron BJ, Towbin JA, Thiene G, Antzelevich C, Corrado D, Arnett D, et al. AHA Scientific Statement.Contemporary Definition and Classification of the Cardiomyopathies. Circulation. 2006;113:1807–16. doi: 10.1161/CIRCULATIONAHA.106.174287. [DOI] [PubMed] [Google Scholar]
- 2.Jenni R, Oechnlin E, Schneider J, Jost CA, Kaufman PA. Echocardiographic and pathoanatomical characteristics of isolated left ventricular non-compaction: A step towards classification as a distinct cardiomyopathy. Heart. 2001;86:666–71. doi: 10.1136/heart.86.6.666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Espinola-Zavaleta N, Soto ME, Castellanos LM, Játiva-Chávez S, Keirns C. Non-compacted cardiomyopathy: Clinical-echocardiographic study. Cardiovasc Ultrasound. 2006;4:35. doi: 10.1186/1476-7120-4-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ritter M, Oechslin E, Sutsch G, Attenhofer C, Schnider J, Jenni R. Isolated non-compaction of the myocardium in adults. Mayo Clin Proc. 1997;72:26–31. doi: 10.4065/72.1.26. [DOI] [PubMed] [Google Scholar]
- 5.Aragona P, Badano LP, Pacileo G, Pino GP, Sinagra G, Zachara E. Isolated left ventricular non-compaction. Ital Heart J Suppl. 2005;6:649–59. [PubMed] [Google Scholar]
- 6.Khan IA, Biddle WP, Najeed SA, Abdul-Aziz S, Mehta NJ, Salaria V, et al. Isolated non-compaction cardiomyopathy presenting with paroxysmal supraventricular tachycardia–case report and literature review. Angiology. 2003;54:243–50. doi: 10.1177/000331970305400216. [DOI] [PubMed] [Google Scholar]
- 7.Coppola G, Guttilla D, Corrado E, Falletta C, Marrone G, Farulla RA, et al. ICD implantation in non-compaction of the left ventricular myocardium: A case report. Pacing Clin Electrophysiol. 2009;32:1092–5. doi: 10.1111/j.1540-8159.2009.02443.x. [DOI] [PubMed] [Google Scholar]
- 8.Okçün Baniş, Tekin A, Oz B, Küçükoğlu MS. Isolated ventricular non-compaction. Acta Cardiol. 2004;59:183–5. doi: 10.2143/AC.59.2.2005174. [DOI] [PubMed] [Google Scholar]
- 9.Fazio G, Corrado G, Zachara E, Rapezzi C, Sulafa AK, Sutera L. Ventricular tachycardia in non-compaction of left ventricle: Is this a frequent complication.? Pacing Clin Electrophysiol. 2007;30:544–6. doi: 10.1111/j.1540-8159.2007.00706.x. [DOI] [PubMed] [Google Scholar]


