Abstract
Background:
Hypopigmentary disorders are common group of dermatoses in pediatric age group.
Aim:
To study the frequency and patterns of hypopigmentary disorders in children.
Materials and Methods:
This study was a descriptive clinical study spanning over a period of 23 months. A total of 113 children (61 boys and 52 girls) were included in this study.
Results:
The frequency of hypopigmentary disorders among children was 3.28 per 1000 children attending the dermatology out patient department. The mean age of the children was 7.2 years. The mean of age of onset was 7.36 years. Most common hypopigmentary disorder in our study was pityriasis alba (24.7%), followed by vitiligo (20.4%), leprosy (11.5%), nevus depigmentosus (10.18%), and tinea versicolor (6.2%). Others were hypomelanosis of Ito (5), post-inflammatory hypopigmentation (5), pityriasis rosea (4), steroid-induced hypopigmentation (4), lichen sclerosus et atrophicus (3), pityriasis lichenoides chronica (3), lichen striatus (2), oculocutaneous albinism (2), tuberous sclerosis complex (2), pigmentary mosaicism (1), and Griscelli syndrome (1).
Conclusion:
Pityriasis alba, vitiligo, leprosy, nevus depigmentosus and tinea versicolor are the five most common hypopigmentary disorders in children.
Keywords: Hypopigmentary disorders, leprosy, nevus depigmentosus, pityriasis alba, tinea versicolor, vitiligo
Introduction
Skin color is an important visible sociocultural characteristic of an individual and any deviation from the normal pattern of pigmentation results in significant concerns. Pigmentary disorders are believed to be the commonest group of dermatoses in pediatric age group.[1] Pigmentary disorders in children are somewhat different from those in the adults in terms of etiology (pigmentary alterations due to genetic disorders are more commonly encountered in the children) and heightened parental concerns. This study was undertaken to find out the pattern of hypopigmentary disorders in children in our population.
Materials and Methods
This study was a descriptive study spanning over a period of 23 months, from August 2007 to June 2009. All children (up to 14 years of age) attending the Dermatology out patient department (OPD) at our Institution were screened for any cutaneous hypopigmentary lesions and those with any such lesion were included in the study after taking informed consent from the parents/guardians. A detailed clinical history was elicited with regard to patient's age, gender, age of onset, site, familial involvement, associated skin and systemic conditions. Detailed examination of the hypopigmentary lesion/lesions was done and findings were noted in terms of site, size, morphology of lesions, etc. General physical examination was done to see any associated cutaneous or systemic involvement and the relevant findings were recorded. Data were analyzed using descriptive statistical methods.
Results
A total of 113 children (61 boys and 52 girls) were included in this study. The frequency of hypopigmentary disorders among children attending the Dermatology OPD was 3.28 per 1000 children. The mean age of the children was 7.2 years. Most common age group was 6–10 years contributing to 34 out of 113 (30.0%) children, followed by 11–14 years contributing to 32 out of (28.1%). The mean of age of onset was 7.36 years. Eleven out of 113 (9.7%) children had onset at birth. The mean duration of the disorders was 1.64 years.
Most common hypopigmentary disorders in our study was pityriasis alba seen in 28 children (24.7%), followed by vitiligo in 23 (20.4%) children, leprosy in 13 (11.5%), nevus depigmentosus in 11 (10.18%), and tinea versicolor in 7 (6.2%) children [Table 1]. Face was the most common affected site in 55 (28.6%) children, followed by upper limb (23 children, 11.8%), lower limb (22 children, 11.3%), chest (20 children, 10.3%), back (18 children, 9.2%) and abdomen. Three children had generalized involvement [Figure 1].
Table 1.
Frequency of hypopigmentary disorders in different age groups
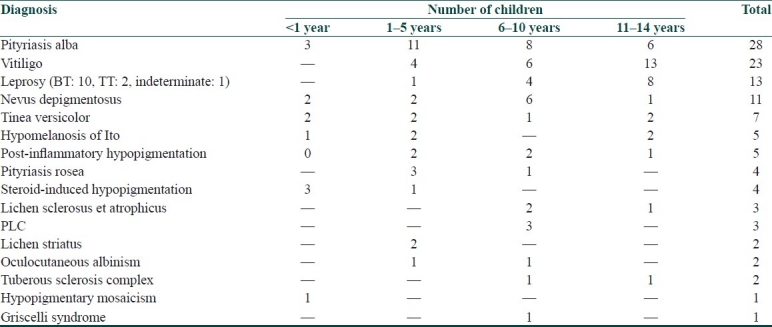
Figure 1.
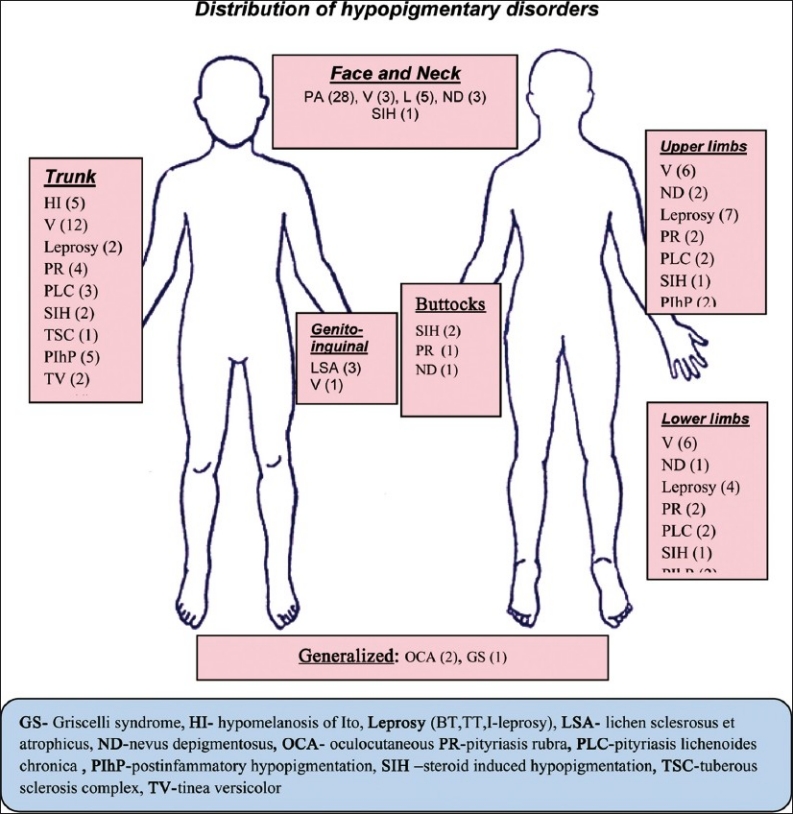
Sites of involvement of hypopigmentary lesions
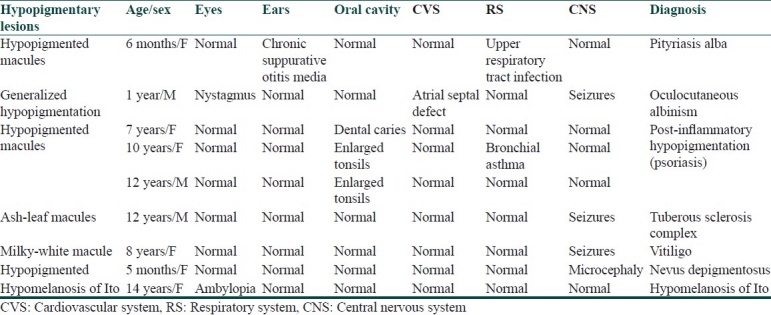
Parental consanguinity was present in 41 (36.2%) out of 113 children with hypopigmentary disorders. Second degree consanguinity was present in 29 (25.6%) children, and third degree consanguinity in 12 (10.6%) children. Family history was noted in four cases – one case of vitiligo had affected mother and sister, another case of vitiligo had affected grandfather, and two cases of BT leprosy had father having lepromatous leprosy. Delayed milestones were present in one child of oculocutaneous albinism. Some patients had associated systemic features as shown in Table 2.
Table 2.
Systemic involvement in hypopigmentary disorders in children
Discussion
According to Pinto and Bolognia, the most common disorders of hypopigmentation in children are pityriasis alba, vitiligo, nevus depigmentosus, and tinea versicolor.[2] In our study also, the most common hypopigmentary disorders were pityriasis alba, vitiligo, leprosy, nevus depigmentosus and tinea versicolor. Leprosy in children is common in leprosy endemic countries like India; thus, it has figured in the five most common disorders in children.
Sujatha et al.,[3] in their study of 200 cases of pityriasis alba, found majority (69%) of their cases below 15 years of age. Itching was noted in 17 patients. Personal history of atopy was noted in 34 (17%) patients. In our study, pityriasis alba lesions occurred in the age range of 5 months–14 years (mean of 6.3 years). Itching was present in three children. Three children had atopic diathesis.
Vitiligo occurs in about 1% of pediatric patients. Jaisankar et al.[4] reported an incidence of 0.72% (vitiligo was recorded in 90 children out of 346 cases of vitiligo). Vitiligo vulgaris was the commonest type followed by segmental, focal, acrofacial and mucosal vitiligo. They noticed family history of vitiligo in 3 (3.3%) children. In our study, vitiligo was seen in 23 children. Vitiligo vulgaris was seen in 11 (47.8%) cases, segmental vitiligo was seen in 8 children (34.7%), localized vitiligo in 2 girls, and lip-tip and lip vitiligo in one girl each. Two children had familial involvement.
Leprosy in children can be an indicator of disease prevalence in the general population and its detection helps in determining the disease transmissibility. Kumar et al.,[5] in their study, recorded the frequency of leprosy in children at 4.5% (61 out of 1360 new cases of leprosy) – most common type was borderline tuberculoid leprosy (78.7%) followed by borderline lepromatous leprosy (8.2%), indeterminate leprosy (6.6%), lepromatous leprosy (4.9%) and pure neuritic leprosy (1.6%). In our study, borderline tuberculoid leprosy was the commonest type followed by tuberculoid (TT) leprosy, and indeterminate leprosy. Ulnar neuritis with claw hand was seen in one child. History of contact with lepromatous leprosy patients (father) was present in two children with BT leprosy (paucibacillary), which is consistent with the finding of Swain et al.,[6] who noted that 57% cases of leprosy in children occurred from household contact with their father having lepromatous leprosy.
In Jena et al.'s study[7] of pityriasis versicolor in 271 children, majority of children were aged 8–12 years (31.7%), but 10 infants were also affected. Face was the most affected site (39%) and extensive involvement was seen in 45 (16.6%) children with lesions on the back and shoulder. In our study, tinea versicolor was seen in seven children. Five children had lesions on the face, and the remaining two children had lesions on the chest, back and upper limb. Medial canthi of both eyes were involved in two infants, which was a unique finding in our study.
We noted lichen sclerosus et atrophicus in three boys who presented to us with depigmentation of foreskin of penis and phimosis. Pityriasis lichenoides chronica (PLC) may subside leaving behind hypopigmentation like we noted in three children in our study. Lesions of PLC were seen on the face, trunk, upper limb, thighs, and buttock. The hypopigmented macules in our patients were interspersed between typical papules of PLC.
Pigmentary mosaicism is characterized by hypo- or hyperpigmented lesions along the lines of Blaschko.[8] In our study, hypopigmentary cutaneous mosaicism was seen in a 1-year-old boy. The lesion was well-defined, bizarre, roughly linear hypopigmentation with irregular margins unilaterally distributed over the right side of lower abdomen, inguinal region and over the lower limb. No history of delayed milestones was obtained. Other dermatological or systemic examinations were normal.
In our study, Griscelli syndrome was seen in an 8-year- old girl who had generalized hypopigmentation of skin since birth. There was no developmental delay or familial involvement. Later, the skin color turned bronze tan over photo-exposed areas.
Footnotes
Source of Support: Nil
Conflict of Interest: Nil.
References
- 1.Toossi P, Nabai L, Alaee Z, Ahmadi H, Saatee S. Prevalence of skin diseases and cutaneous manifestations among Iranian children.A survey of 1417 children. Arch Dermatol. 2007;143:115–6. doi: 10.1001/archderm.143.1.115. [DOI] [PubMed] [Google Scholar]
- 2.Pinto FJ, Bolognia JL. Disorders of hypopigmentation in children. Pediatr Clin North Am. 1991;38:991–1017. doi: 10.1016/s0031-3955(16)38164-0. [DOI] [PubMed] [Google Scholar]
- 3.Vinod S, Singh G, Dash K, Grover S. Clinico-epidemiological study of pityriasis alba. Indian J Dermatol Venereol Leprol. 2002;68:338–40. [PubMed] [Google Scholar]
- 4.Jaisankar TJ, Baruah MC, Garg BR. Vitiligo in children. Int J Dermatol. 1992;31:621–3. doi: 10.1111/j.1365-4362.1992.tb03978.x. [DOI] [PubMed] [Google Scholar]
- 5.Kumar B, Rani R, Kaur I. Childhood leprosy in Chandigarh: clinicohistopathological correlation. Int J Leprol. 2000;68:330–1. [PubMed] [Google Scholar]
- 6.Swain JP, Mishra S, Jena S. Prevalence of leprosy among household contacts of leprosy cases in Western Orissa. Indian J Lepr. 2004;76:19–29. [PubMed] [Google Scholar]
- 7.Jena DK, Sengupta S, Dwari BC, Ram MK. Pityriasis versicolor in the pediatric age group. Indian J Dermatol Venereol Leprol. 2005;71:259–61. doi: 10.4103/0378-6323.16618. [DOI] [PubMed] [Google Scholar]
- 8.Paller AS, Mancini AJ. 3rd ed. Philadelphia: Elsevier Saunders; 2006. Hurwitz Clinical Pediatric Dermatology; pp. 265–98. [Google Scholar]


