Abstract
It is a known fact that cutaneous sarcoidosis is a great imitator in dermatology. We report three cases of cutaneous sarcoidosis without systemic involvement and with varied dermatologic presentation with regard to age and morphology. Lesions mimicked various common dermatologic conditions, causing great confusion for the diagnosis and posing problems for management. Awareness of these varied morphologic presentations is essential for the early diagnosis and management of the master mimicker - cutaneous sarcoidosis.
Keywords: Cutaneous sarcoidosis, granuloma, sarcoidosis
Introduction
Sarcoidosis is an idiopathic multisystem granulomatous disease that commonly involves the lungs, eyes, lymph nodes and skin. The disease usually begins at around 40 years of age and nearly two-thirds of the cases are females. Sarcoidosis confined to skin is quite uncommon as reported in literature, contrary to the latest scenario. Because lesions assume a vast array of morphologies, cutaneous sarcoidosis is known as one of the “great imitators” in dermatology. We report three cases of cutaneous sarcoidosis without systemic involvement with varied presentation with regard to age and morphologies. Lesions mimicked various other common dermatologic conditions.
Case Reports
Case 1
A 28-year-old female presented with a complaint of itchy skin lesions over the face and extremities. Initially, the lesions started on the elbow and leg, which was diagnosed as lichen planus and treated with topical steroid. There was no history of any systemic involvement. General physical and systemic examinations were normal.
Cutaneous examination revealed multiple, discrete, erythematous papules [Figure 1] along with flat-topped, violaceous papules and plaques, morphologically classical of lichen planus [Figure 2] lesions over the face, forearm, abdomen and leg. Oral and other mucosa was normal. Palms and soles were spared.
Figure 1.

Case 1 erythematous papules of sarcoidosis over face
Figure 2.

Case 1 violaceous lichenoid papules of sarcoidosis over elbow
Skin biopsy from the face and elbow lesion revealed classical noncaseating epithelioid cell granulomas of sarcoidal type involving the entire dermis [Figure 3]. Reticulum stain showed intact black reticulin fibers [Figure 4]. Routine hematologic and urine investigations were normal. Serum Angiotensin converting enzyme (ACE) titer was 80 U/L. Serum calcium, liver function tests (LFT), renal function tests (RFT), ultrasonogram (USG) abdomen and chest X-ray were normal
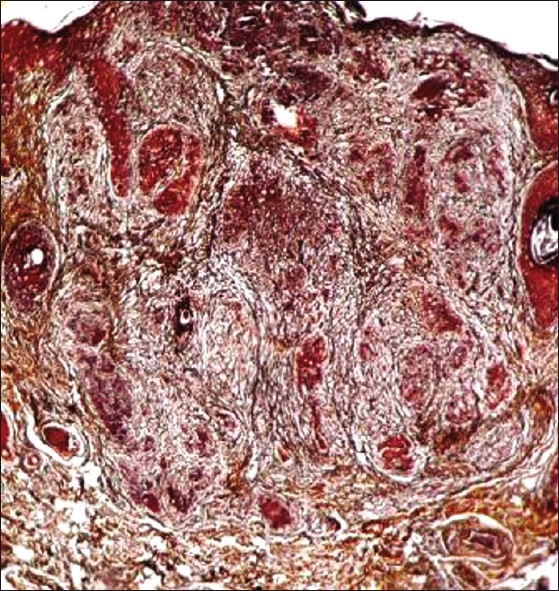
Figure 3.
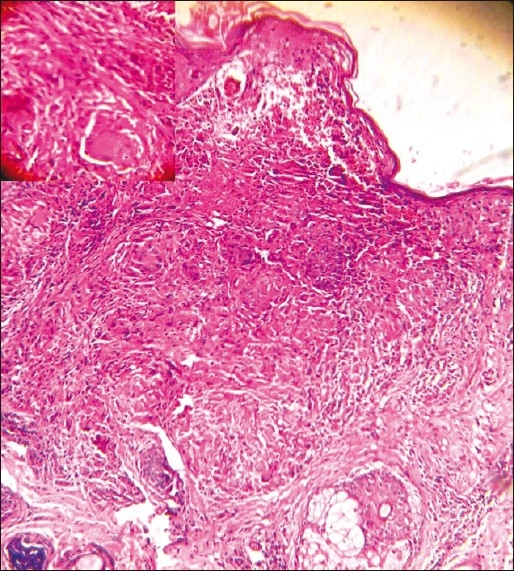
Case 1 H and E low power showing noncaseating granuloma extending till basal cell layer; (inset) high power showing epithelioid granuloma consisting of Langhan's giant cell
Figure 4.
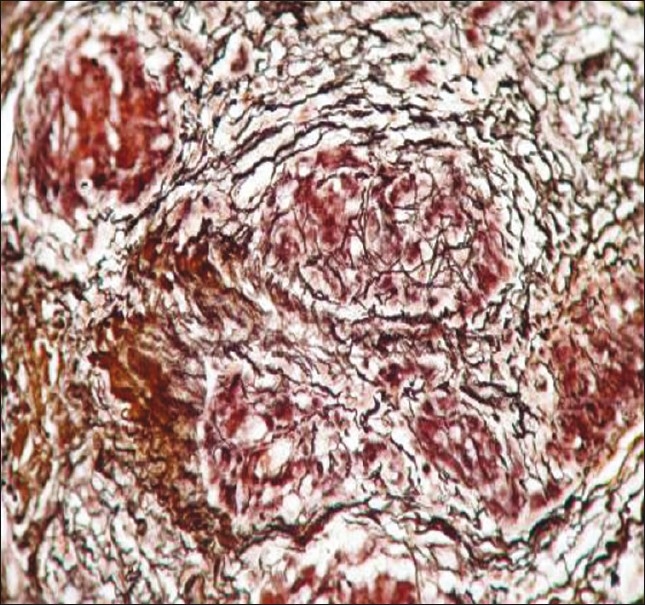
Case 1 reticulum stain showing intact black reticulin fibers
The patient was treated with hydroxy-chloroquine 200 mg bid for 3 months. The erythematous lesions started resolving but there was an increase in the number and size of the flat-topped, violaceous colored skin lesions. The repeat skin biopsy of these lesions revealed the classical histopathologic features of lichen planus, enabling us to come to the final diagnosis of cutaneous sarcoidosis and lichen planus overlap.
Lesions responded to oral prednisolone with a starting dose of 1 mg per kg body weight, tapered over a period of 5 weeks, with complete resolution without any recurrence for 6 months post-treatment.
Case 2
A 52-year-old female presented with multiple reddish skin lesions over the face and extremities of 1 year duration, which increase in size and number. It was associated with scaling. There was no history of itching or sudden exacerbation and remission with trauma, sunlight, stress, infection or medication. She had no history of joint pain or other systemic complaints. The case was treated as psoriasis with emollients and topical steroid by a few dermatologists and the patient presented to us since the lesions did not resolve.
On examination, multiple, well-defined, discrete and confluent erythematous papules and plaques with a few polycyclic lesions were seen over the extensor aspects of limbs, face, neck and scalp [Figures 5 and 6]. Lesions were covered with fine, powdery white, semi-adherent scales.
Figure 5.

Case 2 erythematous psoriasiform lesion of sarcoidosis over forearms
Figure 6.
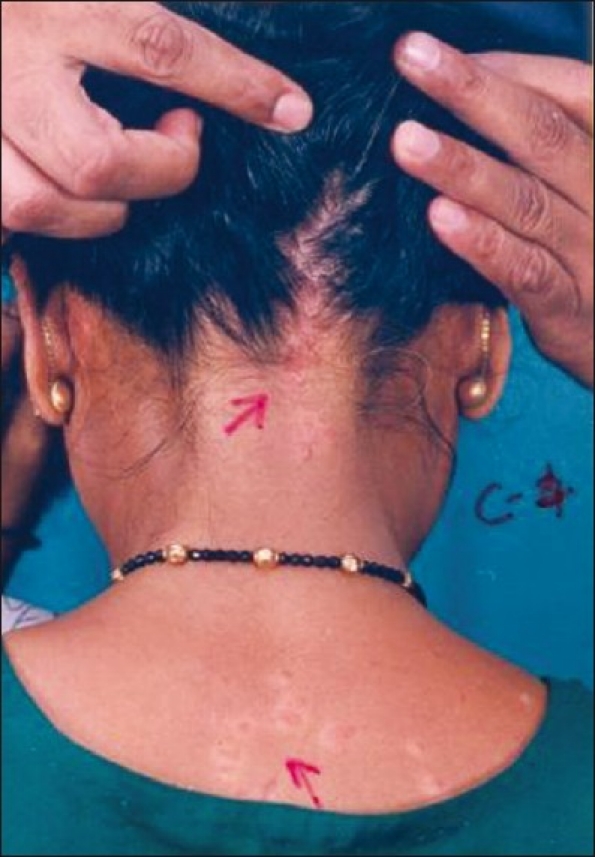
Case 2 erythematous papules and plaques with scales of sarcoidosis over neck, back and scalp
The morphology of the lesions was classical of psoriatic lesions, but Auspitz sign was negative. Mucosa and nails were normal. Systemic examination was unremarkable. At this stage, the skin biopsy revealed epithelioid cell, noncaseating, naked granulomas, mainly in the mid and lower dermis, with multinucleate giant cells and sparse lymphocytic infiltrate [Figure 7]. Reticulum stain showed intact network of reticulin fibers [Figure 8].
Figure 7.
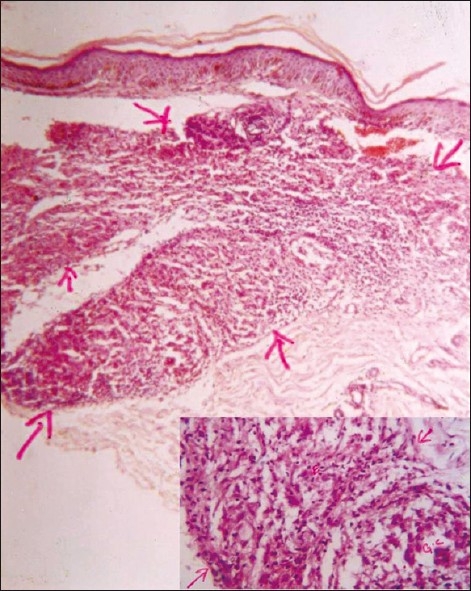
Case 2 H and E low power showing noncaseating granuloma; (inset) high power showing epithelioid granuloma consisting of langhans giant cell, epithelioid cell and sparse lymphocytes
Figure 8.
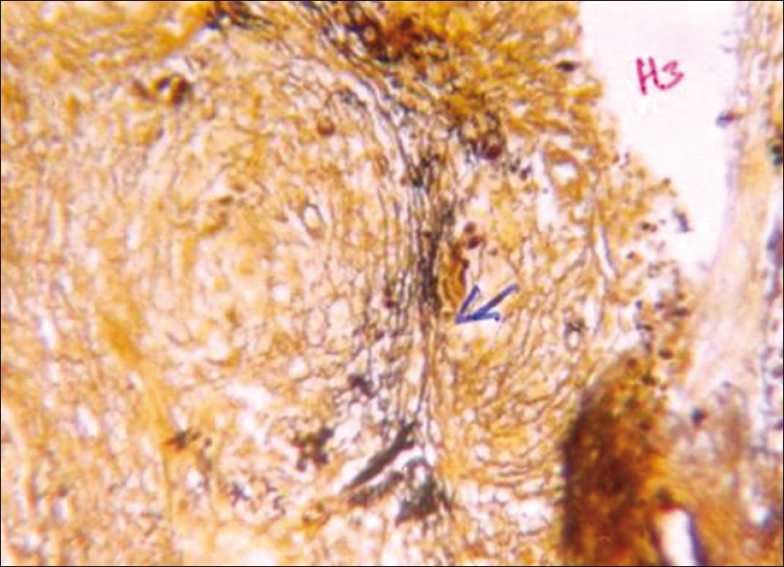
Case 2 reticulum stain showing intact black reticulin fibers
Routine blood and urine tests along with serum calcium, ACE levels, USG abdomen and chest X-ray were normal. A final diagnosis of psoriasiform cutaneous sarcoidosis was made.
The patient was treated with hydroxyl-chloroquin 200 mg orally bid, combined with a short course of low-dose oral prednisolone initially for the first 3 weeks only. The lesions started resolving after 1 month of initiating the treatment; however, the patient was lost for follow-up later.
Case 3
A 15 year-old boy from kolar gold fields, Karnataka, presented with multiple asymptomatic lesions of 6 months duration over the face. There was no history of fever, joint pain, cough weight loss, joint pains, eye complaints or any other systemic complaints. Past and family history was not contributory. There was no significant drug history. General physical and systemic examinations were normal.
Dermatologic examination revealed multiple skin colored to reddish-brown, translucent papules, measuring 2-5 mm, on the cheeks, nose, upper lip, chin and forehead [Figure 9]. Lesions were non-tender. Palms, soles, hair, nail and mucosal areas were uninvolved. Ophthalmologic examination was normal. Differential diagnosis of acne, histoid Hansen's disease, and trichoepithelioma were considered and investigated further.
Figure 9.

Papular lesions on face of case 3; (inset) grouped papules over chin
Investigations revealed raised serum ACE (118 U/L) level, negative Mantoux test, and LFT, serum calcium, serum creatinine and blood urea were normal. Venereal disease research laboratory test (VDRL) was nonreactive; skin slit smear for acid fast bacilli was negative. Radiologic examination of chest, hands and feet, ultrasound abdomen and lung function tests revealed no abnormality.
Skin biopsy revealed noncaseating granulomas involving the full thickness of the dermis. The granulomas predominantly composed of epithelioid cells, with few Langhan's giant cells and sparse lymphocytic infiltrate (naked granulomas) [Figure 10]. Reticulum stain showed intact reticulin fibers [Figure 11]. Special stains for acid fast bacilli (AFB), LD bodies, fungi and calcium were negative.
Figure 10.
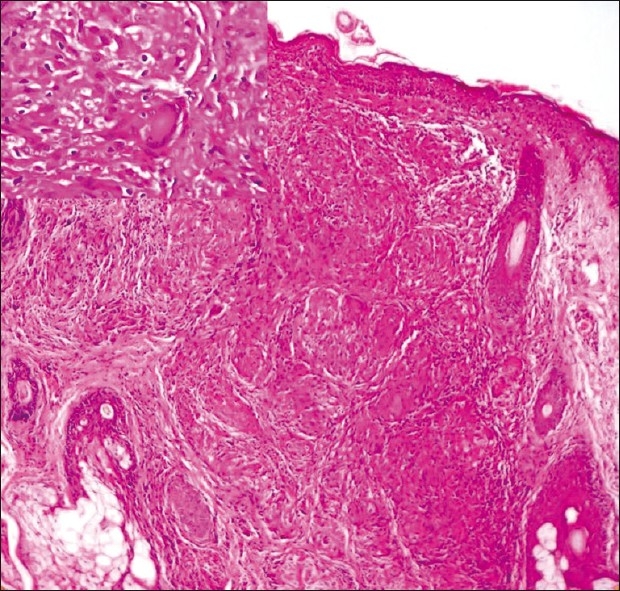
Case 3 H and E low power showing noncaseating granuloma; (inset) high power showing epithelioid granuloma consisting of giant cell, epithelioid cell and sparse lymphocytes
Figure 11.
Case 3 special stain low power showing intact black reticulin fibers
The patient was treated with hydroxychloroquine 200 mg OD and topical fluticasone. The patient responded with near- complete resolution at the end of 4 months treatment [Figure 12].
Figure 12.

Case 3 resolution of lesion after 4 months of treatment
Discussion
Sarcoidosis commonly affects the lungs, lymph nodes, liver, eyes, bones and skin. Hutchinson recorded the first case in 1865, but first unequivocal case of sarcoidosis in English literature was reported by Boeck in 1899.[1] First case in India was reported by Rajam et al. in 1957.
It occurs worldwide with the highest prevalence in Scandinavia and the prevalence was 20/100,000 in 1975 but recent report says it to be 64/100,000.[2] Only 300 cases of sarcoidosis were reported in our country till 1986 but a recent report says there is an increased prevalence.[3]
The authors are of the strong opinion that this increase in incidence is because of increased awareness about the not so uncommon occurrence of sarcoidosis in India in the recent times. Missed diagnosis due to lack of clinical suspicion, better understanding and newer investigative modalities have also contributed.
In patients with systemic disease, the skin is involved in 20-35% of cases.[3] However; cutaneous lesions are the sole manifestation of sarcoidosis in approximately 10% of patients.[2]
Among the numerous reported morphologic presentations are papules, micropapules, plaques, subcutaneous nodules, scar sarcoidosis, lupus pernio, erythema nodosum, ulcer and alopecia.[4] Multiple other cutaneous morphologies are possible; many are quite rare, although the incidence is difficult to determine.
Papules of sarcoidosis may be of various colors, including red, reddish-brown, violaceous, translucent, or hyperpigmented.[5] Because of this varied color, it mimics many common conditions including violaceous color of lichen planus. Sarcoid lesions are asymptomatic but approximately 10-15% may itch.[2] Case 1 is rare example where lesions exhibited violaceous color which was associated with pruritus and the histopathology of the differently colored lesions was different (lichen planus and sarcoidosis). Rare presentations like follicular, verrucous, ichthyosiform, hypomelanotic, and annular lesions have also been described.[6] Psoriasiform lesions have been very rarely reported, as described by Burgoyne et al.[7] Case 2 was an example for psoriasiform variety and initially treated as psoriasis.
The disease usually begins at around 40 years of age and nearly two-thirds of the cases are females.[8] Cutaneous sarcoidosis has been reported rarely from India[9] and incidence in children is much lesser.[9,10] Also, in all these reports, lesions of skin were associated with some forms of systemic involvement. Sarcoidosis in children with lesion confined to the face mimics many common skin conditions. The age of onset in case 3 of this report is 14 years, which is rare as per the existing reports.
Conclusion
Sarcoidosis is a great imitator of other dermatologic diseases because the cutaneous manifestations are quite variable and occur in both localized as well as generalized forms. Greater awareness about the not so rare occurrence of sarcoidosis and its varied manifestations mimicking the most common dermatologic conditions like psoriasis (as in case 2) and its association with common conditions like lichen planus (as in case 1) will help prevent misdiagnosis of sarcoidosis and helps in appropriate therapy.
Footnotes
Source of Support: Nil
Conflict of Interest: Nil.
References
- 1.Moschella SL, Crepley TG. Diseases of the mononuclear phagocytic system. In: Fletcher J, editor. Moschella and Hurley Dermatology. 3rd ed. Philadelphia: Saunders; 1992. pp. 1064–75. [Google Scholar]
- 2.Sarcoidosis . Andrews’ diseases of the skin. In: James WD, Berger TG, Elston DM, editors. 10th ed. Canada: Saunders elsevier; 2006. pp. 708–14. [Google Scholar]
- 3.Gupta SK. Sarcoidosis in India: The past, present and the future. Lung India. 1987;5:101–5. [Google Scholar]
- 4.Mohanty R, Singh SN, Bhattamishra AB. Cutaneous sarcoidosis without systemic manifestations. Indian J Dermatol. 2009;54:80–2. [Google Scholar]
- 5.Katta R. Cutaneous sarcoidosis: A dermatologic masquerader. Am Fam Physician. 2002;65:1581–4. [PubMed] [Google Scholar]
- 6.Fujii K, Okamoto H, Onuki M, Horio T. Recurrent follicular and lichenoid papules of sarcoidosis. Eur J Dermatol. 2000;10:303–5. [PubMed] [Google Scholar]
- 7.Burgoyne JS, Wood MG. Psoriasiform sarcoidosis. Arch Dermatol. 1972;106:896–8. [PubMed] [Google Scholar]
- 8.Mahajan VK, Sharma NL, Sharma RC, Sharma VC. Cutaneous sarcoidosis: Clinical profile of 23 Indian patients. Indian J Dermatol Venereal Leprol. 2007;73:16–21. doi: 10.4103/0378-6323.30645. [DOI] [PubMed] [Google Scholar]
- 9.Rajam RV, Vishwanathan GS, Rangaiah PN, Misra RS, Saxena P, Indira U. et al.Sarcoidosis-a short review with a case report. Indian Dermatol Venereol Leprol. 1957;23:97–135. [Google Scholar]
- 10.Ghorpade A, Ramanan C. Cutaneous sarcoidosis. Indian J Dermatol Venereol Leprol. 1996;62:171–2. [PubMed] [Google Scholar]


