Dear Sir,
We report the case of a 28-year-old housewife who presented with multiple painful non-healing skin ulcers on the legs. Over the preceding 6 years, she had developed progressive generalized weakness; along with progressive skin thickening, which was associated with Raynaud's phenomenon and bilateral asymmetrical polyarthritis. Progressive thickening and stiffening of skin started with swelling and puffiness of fingers, subsequently involving face and progressing proximally to involve the arm and trunk. She was diagnosed as suffering from systemic sclerosis and was on treatment for the same.
Since the last 8 months, she developed ulceration, which began as red, tender papulo-nodular lesion and sloughed out to giving rise to ulcerations. Examination revealed well-circumscribed ulcers (3 on left leg and 1 on right leg) with sharp, tender, irregular, crenated border and purulent granulating necrotic base [Figures 1 and 2], along with pseudo-clubbing and bilateral puffiness of fingers and ulceration at the knuckles and tip of the digits [Figure 3]. At presentation she also gave history of exertional dyspnea, heartburn and dysphagia; however, there was no history of chest pain, dryness of mouth, seizures or fetal loss. Patient was on nonsteroidal anti-inflammatory drugs (NSAIDs) and intermittent steroid therapy; and examination of respiratory, cardiovascular, neurological and reticulo-endothelial systems was unremarkable.
Figure 1.

Ulceration on the shin showing sharp, irregular, bluish, swollen margin with the floor covered with necrotic and purulent material
Figure 2.

Multiple ulceration on the dorsa of foot showing bluish irregular margin and covered with unhealthy granulation tissue with swollen toes
Figure 3.

Pseudo-clubbing and bilateral puffiness of fingers and ulceration at the knuckle
Punch biopsy of skin was taken from the edge of the ulcer, and it revealed intense inflammatory infiltrate arranged perivascularly and extending into the subcutis [Figure 4]. The dermis showed picture of vasculitis with fibrinoid necrosis of the wall of vessels, extravasation of RBCs and a picture of perivascular mixed lymphocytic and neutrophilic infiltrate [Figure 5]. There was no feature of granuloma formation, and periodic acid Schiff (PAS) stain showed no evidence of fungal element. The clinico-histopathological correlation established the ulcerations as pyoderma gangrenosum.
Figure 4.
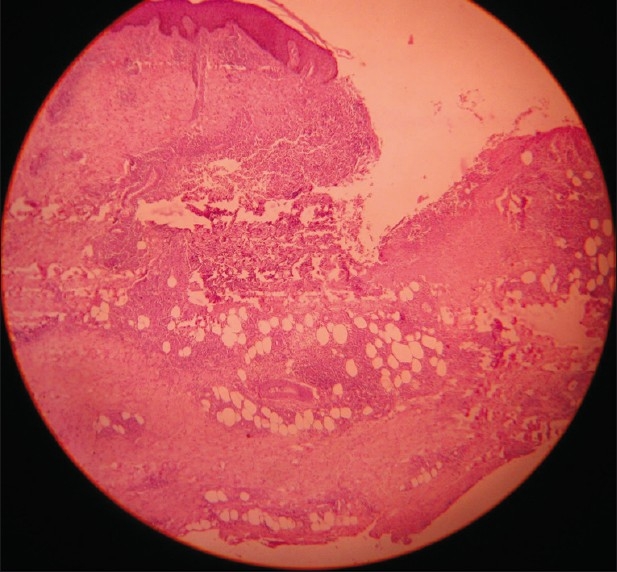
Histopathology taken from the margin of the ulcer showing necrotic debris at the edge of the ulcer with mixed inflammatory infiltrate consisting of polymorphonuclear leukocytes and mononuclear cells arranged around the debris, perivascular location, and extending into the subcutaneous tissue (H and E stain, ×100)
Figure 5.
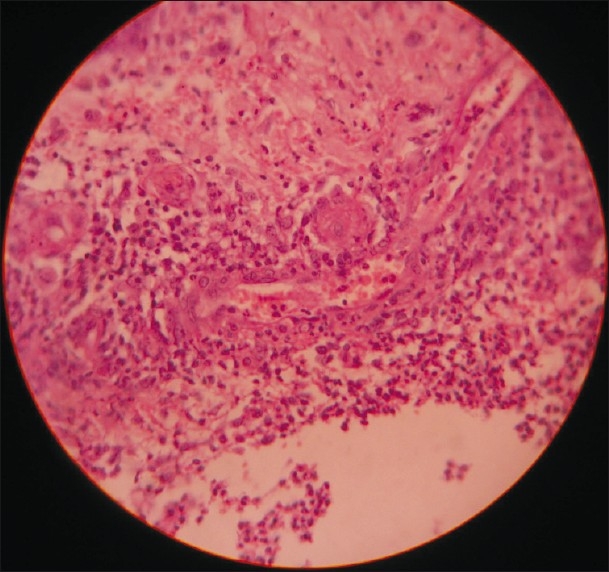
Dermis showing a blood vessel with dense perivascular infiltrate of mononuclear cells (lymphocytes and histiocytes) as well as polymorphonuclear leukocytes. Fibrinoid necrosis of the wall of the vessel is present along with swollen endothelium and extravasation of RBCs (H and E stain, ×400)
Since pyoderma gangrenosum is often associated with inflammatory bowel disease, sero-negative as well as seropositive arthritis, monoclonal gammopathy and myeloproliferative disorders,[1] the patient was investigated thoroughly. The baseline investigation showed Hb, 9 g/ dL; TLC, 6,400, N55, L32, E3, B0, M10; platelet count, 196,000/μL; ESR, 110 mm (first hour). Results of blood sugar (both fasting and post-glucose), renal and hepatic function tests were found to be within normal limits. HIV ELISA was negative; pulmonary function test showed moderate restrictive lung disease; and mild left ventricular diastolic dysfunction was detected in echocardiography.
The connective tissue profile was remarkable, with anti-nuclear factor, >1:640; creatine kinase, 220 units/L (normal range, 22-269); and positive rheumatoid factor and CRP. Anti-ds-DNA, anti-topoisomarase, anticentromere antibodies were within normal range. Anti-U1RNP was done and was positive in very high titer (>1:1640).
The patient fully satisfied the diagnostic criteria for mixed connective tissue disorder (MCTD) — both Alarcon-Segoria criteria and Khan's criteria[2] — and was diagnosed to be a case of MCTD with pyoderma gangrenosum and Raynaud's phenomenon, and treatment was started with oral prednisolone, dapsone, Disease-modifying antirheumatic drug (DMARD) and nifedipine. The ulcer showed poor response to the treatment even after 2 months; so azathioprine (1 mg/kg/d) was started in place of dapsone, and other medicines were continued. On addition of azathioprine, she started showing dramatic improvement, and ulcers healed over the next 1 month [Figure 6].
Figure 6.

Post-treatment photograph after 1 month of azathioprine therapy showing healed ulceration on the dorsa of foot leaving behind a cribriform scar
Pyoderma gangrenosum is a rare destructive, necrotizing, noninfective, non-neoplastic dermatosis, which ranks among the group of neutrophilic dermatoses characterized by rich dermal infiltrate of mature polymorphonuclear cells. Diagnosis of pyoderma gangrenosum is mostly clinical, and histopathology is only corroborative. Recently it has been classified into four distinctive clinical variants: ulcerative, pustular, bullous and vegetative.[3] The ulcerative variant is the most frequent clinical type, with the lower legs being the most commonly affected.[4] The ulcerative form begins as a papular lesion and undergoes necrosis, resulting in an ulcer, as in our case.
Though pyoderma gangrenosum is reported with several other systemic diseases,[1] the PubMed search gathered only one entry of MCTD associated with pyoderma gangrenosum in literature from all over the world.[5] MCTD is an overlap syndrome generally associated with high titer of autoantibodies to U1RNP. Early in the course of the disease, most patients complain of early fatigability; poorly defined myalgias, arthralgias and Raynaud's phenomenon; and often, swollen hands, as in the present case. With the progress of time, overlap features of systemic sclerosis, systemic lupus erythematosus (SLE), rheumatoid arthritis and polymyositis develop in various combinations. High index of suspicion regarding underlying systemic disorder prompted us to undertake the battery of investigations in the present case, and MCTD was diagnosed before it could manifest in its full-blown form.
Treatment of pyoderma gangrenosum always presents a challenge, and there is a long list of agents, including systemic steroids, dapsone, clofazimine, methotrexate, minocycline, tacrolimus, thalidomide, cyclosporine, which are being tried with varied success.[3] The present case was unresponsive to systemic steroid and dapsone; and only when azathioprine (1 mg/kg/d) was added, the patient showed dramatic improvement, highlighting the role of azathioprine in the management of pyoderma gangrenosum.
References
- 1.Wolff K, Stingl G. Pyoderma gangrenosum. In: Freedberg IR, Eisen AZ, Wolff K, Austen FK, Goldsmith LA, Katz SA, editors. Fitzpatrick's Dermatology in General Medicine. 6th ed. New York: Mc Graw Hill Publications; 2003. pp. 969–76. [Google Scholar]
- 2.Bennett RM. Mixed Connective Tissue Disease and Other Overlap Syndromes. In: Harris DE, Budd CR, Genovese CM, Firestein SG, Sargent SJ, Sledge BC, editors. Kelly's Textbook of Rheumatology. 7th ed. Philadelphia: Elsevier Saunders; 2005. pp. 1258–78. [Google Scholar]
- 3.Powell FC, O’Kane M. Management of pyoderma gangrenosum. Dermatol Clin. 2002;20:347–55. doi: 10.1016/s0733-8635(01)00029-8. [DOI] [PubMed] [Google Scholar]
- 4.Mlika RB, Riahi I, Fenniche S, Mokni M, Dhaoui MR, Dess N, Dhahri AB, Mokhtar I. Pyoderma gangrenosum: a report of 21 cases. Int J Dermatol. 2002;41:65–8. doi: 10.1046/j.1365-4362.2002.01329.x. [DOI] [PubMed] [Google Scholar]
- 5.Malaviya, Moudi Al-Mutairi AN, Francis I, Sawabn S, Hussein AYT. Sharp's Syndrome (Mixed Connective Tissue Disease) With Extensive Inflammatory Panniculitis Complicated with Pyoderma Gangrenosum – A Case Report. J Indian Rheumatol Assoc. 2003;11:45–50. http://medind.nic.in/jaa/t03/i2/jaat03i2p45.pdf . [Google Scholar]


