Introduction
Depression is associated with significantly poorer medical prognosis after acute coronary syndrome (ACS) [1,2]. Clinical trials of depression treatment in post-ACS patients have failed to improve event-free survival, and have for the most part shown only modest offsets in depression severity. Among the lessons learned from these efforts is that the intervention must be acceptable to trial participants [3]. The involvement of depressed medical patients in care decisions – e.g. between psychotherapy and pharmacotherapy [4] – enhances both patient engagement and treatment adherence [5,6], and results in significantly greater reductions in depression symptom severity and major depression incidence [7], as we have recently found with ACS patients as well [8]. The treatment preferences of post-ACS patients with elevated depressive symptoms, and correlates of these preferences, have not previously been examined.
In the observational Coronary Psychosocial Evaluation Study (COPES) [9], patients at 3 northeast university hospitals were queried at the time of ACS concerning their treatment preferences for emotional distress and problems coping with their ACS. Patients were ≥18 years old, spoke English or Spanish, and had scores <5 or ≥10 on the Beck Depression Inventory (BDI) [10] within 1 week after the ACS. Depression diagnosis was assessed by the Depression Interview and Structured Hamilton [11]. Only patients with a BDI score ≥10, that has previously been found to carry post-ACS prognostic significance [1], were included in the current analyses.
At baseline, patients were asked: (1) If your doctor advises you that you should either get counseling or take medication to help you cope, which one would you prefer? (2) Would you go to counseling, to talk about your emotions about your heart attack and coping with them, if it was offered without any costs for you? In addition, patients were questioned concerning their interest in talking about 3 common elements of the depression constellation: one's self, one's activities and one's relationships.
Differences in treatment preferences – medication versus counseling – according to sociodemographic and diagnostic characteristics were evaluated by χ2 and t test. Multivariate logistic modeling was used to calculate adjusted odds ratios and 95% confidence intervals. Answer options were coded into dichotomous categories for analyses regarding willingness to go to counseling (‘no’ or ‘probably not’ vs. ‘probably’ and ‘yes’) and analyses regarding interest in talking about specific topics (‘not at all’ or ‘very little’ vs. ‘somewhat’ or ‘a lot’).
Overall, 215 of 457 COPES patients had a BDI score ≥10, 143 of whom provided valid answers to the treatment preference questions. Those who did not were more likely to be Hispanic (14% vs. 26%, p = 0.03), and to have major depression (18% vs. 32%, p = 0.02). Of respondents, 63% (n = 90) had a BDI score of 10–16, and 37% (n = 53) had a BDI score >16; 33% (n = 47) met criteria for minor depression, and 18% (n = 26) for major depression; 55% (n = 78) were men, 14% (n = 20) Hispanic, 13% (n = 19) African American, and 78% (n = 112) Caucasian.
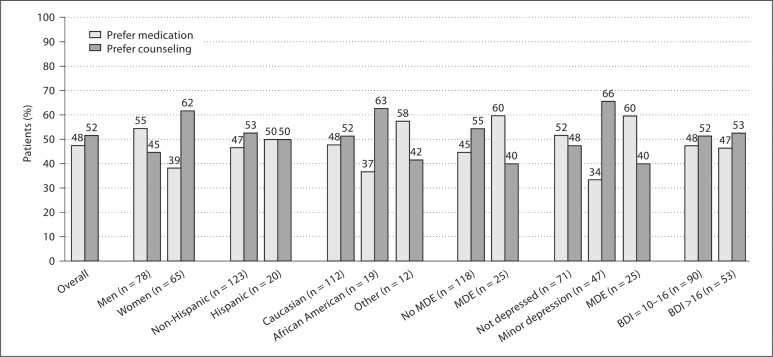
Fifty-two percent overall endorsed a preference for counseling; 66% with minor depression and 40% with major depression endorsed this preference (p = 0.061). More men versus women endorsed a preference for medication, and women for counseling (p = 0.047). This was the only significant factor in multivariate analyses (adjusted odds ratios = 2.06; 95% confidence intervals 1.04–4.10; fig. 1).
Fig. 1.
Patient preference for medication versus counseling: ‘If your doctor advises you that you should either get counseling or take medication to help you cope, which one would you prefer?’ MDE = Major depressive episode.
Fifty-nine percent of patients who had initially indicated a preference for medication said that they ‘would’ or ‘probably would’ go to counseling if it were offered for free. More patients with minor depression versus major depression indicated a willingness to utilize counseling if offered it at no cost (p = 0.061). In addition, more Hispanics than non-Hispanics indicated this willingness (p = 0.10). Patients who indicated a willingness to go to free counseling were slightly younger than patients who were unwilling (59.2 ± 12.7 years vs. 61.7 ± 15.7 years; p = 0.09). No other correlates emerged. In a logistic regression model, only initial patient preference was significant (adjusted odds ratios = 5.89; 95% confidence intervals 2.37–14.61).
Of the 106 patients who had indicated a willingness to go to counseling, the vast majority indicated an interest in talking about how they feel about themselves, their recreational activities, and their relationships. More non-Hispanics than Hispanics endorsed an interest in talking about their recreational activities (90% vs. 72%, p = 0.06) or their relationships (90% vs. 67%, p = 0.01). There were no other demographic differences in these interests, nor were they related to depression status.
Overall, an essentially equal number of patients with a prognostically significant level of post-ACS depression endorsed a preference for counseling and for medication. Of those who endorsed a preference for medication, over half stated that they would utilize counseling if offered it at no cost. While stated preferences do not necessarily translate to real choices [12], the importance of matching treatment to patients’ preference is highlighted by the overall success of the COPES Intervention Trial [8], along with recent research showing more rapid improvement in depression symptoms among matched versus unmatched treatment recipients [13,14]. These findings indicate the need for future clinical trials of post-ACS depression treatment to devise an intervention that accommodates participants’ treatment preferences, while providing for obstacles such as distance and travel (e.g. by providing treatment via phone or internet).
The preference for counseling among women is consistent with previous research [15]. The importance of this finding is underlined by 2 large depression treatment trials – neither of which utilized patient preference – that reported a trend towards harm for women in the treatment arm [16,17], though for the most part these trials utilized counseling alone. In contrast to others which found older individuals resisted medication [12,15], age did not affect preference for counseling versus medication. Similarly, while other trials have found African Americans less likely than Caucasians to use counseling [18], this was not the case here; education also had no effect.
Limitations include: the small sample size, exacerbated by the third who did not answer preference questions, and the relatively small number of individuals with major depression, though the percent observed was consistent with prior post-ACS depression studies. In addition, the sample was not geographically representative, and preferences stated may differ by location. Significant differences in preferences due to demographic characteristics might have emerged with larger representation. Also the question regarding treatment preference did not provide for a preference for neither counseling nor medication, or for both, or for an assessment of how insurance status affects preference, though the question concerning free counseling implies an effect for such coverage. Nonetheless, the findings of the current study, which are consistent with the findings of recent trials of depression treatment for medical populations [7,12,14,15,19,20] remain to be implemented and tested in large trials.
Acknowledgement
This work was supported by grants HC-25197, HL-076857, HL-084034, and HL-088117, from the National Heart, Lung, and Blood Institute, Bethesda, Md., USA.
References
- 1.Barth J, Schumacher M, Herrmann-Lingen C. Depression as a risk factor for mortality in patients with coronary heart disease: a meta-analysis. Psychosom Med. 2004;66:802–813. doi: 10.1097/01.psy.0000146332.53619.b2. [DOI] [PubMed] [Google Scholar]
- 2.Van Melle JP, de Jonge P, Spijkerman TA, Tijssen JG, Ormel J, van Veldhuisen DJ, van den Brink RH, van den Berg MP. Prognostic association of depression following myocardial infarction with mortality and cardiovascular events: a meta-analysis. Psychosom Med. 2004;66:814–822. doi: 10.1097/01.psy.0000146294.82810.9c. [DOI] [PubMed] [Google Scholar]
- 3.Burg MM, Czajkowski S, ENRICHD Clinical Trial: Lessons learned; in Allan R, Scheidt S (eds): Heart and Mind: The Practice of Cardiac Psychology, ed 2. Washington: American Psychological Association, in press.
- 4.Hegel MT, Imming J, Cyr-Provost M, Hitchcock NP, Arean P, Unutzer J. Role of allied behavioral health professionals in a collaborative stepped care treatment model for depression in primary care: project IMPACT. Fam Syst Health. 2002;20:265–277. [Google Scholar]
- 5.Benbassat J, Pilpel D, Tidhar M. Patients' preferences for participation in clinical decision making: a review of published surveys. Behav Med. 1998;24:81–88. doi: 10.1080/08964289809596384. [DOI] [PubMed] [Google Scholar]
- 6.Patel SR, Bakken S. Preferences for participation in decision making among ethnically diverse patients with anxiety and depression. Community Ment Health J. 2010 doi: 10.1007/s10597-010-9323-3. E-pub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Unützer J, Katon W, Callahan CW, Williams JW, Hunkeler E, Harpole L, Hoffing M, Della Penna RD, Noel PH, Lin EH, Arean PA, Hegel MT, Tang L, Belin TR, Oishi S, Langston C, IMPACT Investigators Collaborative care management of late-life depression in the primary care setting: a randomized controlled trial. JAMA. 2002;288:2836–2845. doi: 10.1001/jama.288.22.2836. [DOI] [PubMed] [Google Scholar]
- 8.Davidson KW, Rieckmann N, Clemow L, Schwartz JE, Shimbo D, Medina V, Albanese G, Kronish IM, Hegel M, Burg MM. Enhanced depression care for acute coronary syndrome patients with persistent depressive symptoms. Coronary Psychosocial Evaluation Studies (COPES) randomized controlled trial. Arch Intern Med. 2010;170:1–9. doi: 10.1001/archinternmed.2010.29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Davidson KA, Burg MM, Kronish IM, Shimbo D, Dettenborn L, Mehran R, Vorchheimer D, Clemow L, Schwartz JE, Lesperance F, Rieckmann N. Association of anhedonia with recurrent major adverse cardiac events and mortality 1 year after acute coronary syndrome. Arch Gen Psychiatry. 2010;67:480–488. doi: 10.1001/archgenpsychiatry.2010.36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Arch Gen Psychiatry. 1961;4:561–571. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- 11.Freedland KE, Skala JA, Carney RM, Raczynski JM, Taylor CB, Mendes de Leon CF, Ironson G, Youngblood ME, Krishnan KR, Veith RC. The Depression Interview and Structured Hamilton (DISH): rationale, development, characteristics, and clinical validity. Psychosom Med. 2002;64:897–905. doi: 10.1097/01.psy.0000028826.64279.29. [DOI] [PubMed] [Google Scholar]
- 12.Gum AM, Arean PA, Hunkeler E, Tang L, Katon W, Hitchcock P, Steffens DC, Dickens J, Unutzer J. Depression treatment preferences in older primary care patients. Gerontologist. 2006;46:14–22. doi: 10.1093/geront/46.1.14. [DOI] [PubMed] [Google Scholar]
- 13.Iacoviello BM, McCarthy KS, Marrett MS, Rynn M, Gallop R, Barber JP. Treatment preferences affect the therapeutic alliance: implications for randomized controlled trials. J Consult Clin Psychol. 2007;75:194–198. doi: 10.1037/0022-006X.75.1.194. [DOI] [PubMed] [Google Scholar]
- 14.Lin P, Campbell DG, Chaney EF, Liu CF, Heagerty P, Felker BL, Hedrick SC. The effect of patient preference on depression treatment in primary care. Ann Behav Med. 2005;30:164–173. doi: 10.1207/s15324796abm3002_9. [DOI] [PubMed] [Google Scholar]
- 15.Dwight-Johnson M, Sherbourne CD, Liao D, Wells KB. Treatment preferences among depressed primary care patients. J Gen Intern Med. 2006;21:146–151. doi: 10.1046/j.1525-1497.2000.08035.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Berkman LF, Blumenthal J, Burg M, Carney RM, Catellier D, Cowan MJ, Czajkowski SM, DeBusk R, Hosking J, Jaffe A, Kaufmann PG, Mitchell P, Norman J, Powell LH, Raczynski JM, Schneiderman N, ENRICHD Investigators Effects of treating depression and low perceived social support on clinical events after myocardial infarction: the Enhancing Recovery in Coronary Heart Disease Patients (ENRICHD) Randomized Trial. JAMA. 2003;289:3106–3116. doi: 10.1001/jama.289.23.3106. [DOI] [PubMed] [Google Scholar]
- 17.Frasure-Smith N, Lesperance F, Prince RH, Verrier P, Garbe R, Juneau M, Wolfson C, Bourassa MG. Randomized trial of home-based psychosocial nursing intervention for patients recovering from myocardial infarction. Lancet. 1997;350:473–479. doi: 10.1016/S0140-6736(97)02142-9. [DOI] [PubMed] [Google Scholar]
- 18.Joo JH, Morales KH, de Vries HF, Gallo JJ. Disparity in use of psychotherapy offered in primary care between older African American and white adults: results from a practice based depression intervention trial. J Am Geriatr Soc. 2010;58:154–160. doi: 10.1111/j.1532-5415.2009.02623.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Katon WJ, von Korff M, Lin EH, Simon G, Ludman E, Russo J, Ciechanowski P, Walker E, Bush T. The Pathways Study: a randomized trial of collaborative care in patients with diabetes and depression. Arch Gen Psychiatry. 2004;61:1042–1049. doi: 10.1001/archpsyc.61.10.1042. [DOI] [PubMed] [Google Scholar]
- 20.Lin EH, Katon W, Von Korff M, Tang L, Williams JW, Jr, Kroenke K, Hunkeler E, Harpole L, Hegel M, Arean P, Hoffing M, Della Penna R, Langston C, Unützer J, IMPACT Investigators Effect of improving depression care on pain and functional outcomes among older adults with arthritis: a randomized controlled trial. JAMA. 2003;290:2428–2429. doi: 10.1001/jama.290.18.2428. [DOI] [PubMed] [Google Scholar]