Abstract
Objectives
To determine the lifetime risk of undergoing pelvic floor surgery in a cohort of UK parous women and the re-operation rates for pelvic floor surgery, time intervals for repeat surgery and independent risk factors for undergoing primary and repeat pelvic floor surgery.
Study design
A register linkage study.
Main outcome measures
The primary outcome was lifetime risk of parous women in the UK undergoing pelvic floor surgery for pelvic organ prolapse (POP), urinary incontinence (UI), and rectal prolapse or faecal incontinence (RP-FI). Secondary outcomes were re-operation rates and time interval of repeat surgery for POP/UI, and independent risk factors for undergoing primary and repeat pelvic floor surgery.
Results
34 631 women identified from the Aberdeen Maternity and Neonatal Database were linked with the Scottish Morbidity Records databases of NHS Scotland to assess relevant outcomes. The lifetime risk for women by age 80 years of undergoing any form of pelvic floor surgery was 12.2%. 2130 (6.2%) women had at least one pelvic floor surgery, of whom 407 (19%) had repeat operations. The median time intervals (IQR) between index and repeat UI and POP surgery were 2.80 (0.94–8.07) years and 3 (1.00–8.25) years, respectively. There is a reduced lifetime risk of pelvic floor surgery in women who had all deliveries by caesarean section (p<0.001) and those aged <20 years at first delivery (p=0.021). Women who sustained at least one perineal laceration (in the absence of a classified perineal tear) during delivery or who had at least one instrumental delivery with forceps use were at increased risk (p<0.001 and p=0.015, respectively).
Conclusions
Our study shows that in the UK more than one in 10 parous women will require at least one surgical procedure for pelvic floor disorders over their lifetime. The study also identifies independent risk and protective factors for pelvic floor surgery in parous women.
Article summary
Article focus
Lifetime risk of undergoing various types of pelvic floor surgery in a cohort of UK women.
Re-operation rates for various types of pelvic floor surgery and time intervals for repeat surgery.
Independent risk factors for undergoing primary and repeat pelvic floor surgery.
Key messages
The lifetime risk for women by age 80 years undergoing any form of pelvic floor surgery was 12.2%.
The re-operation rate for pelvic floor surgery was 19%.
There was a reduced lifetime risk of pelvic floor surgery in women who had all deliveries by caesarean section only and those aged <20 years at first delivery, while women who sustained at least one perineal laceration during delivery or who had at least one instrumental delivery with the use of forceps were at increased risk.
Strengths and limitations of this study
To our knowledge, this is the first study to report the lifetime risk for women in the UK of undergoing surgical treatment for pelvic floor dysfunction.
As the study represents the general population rather than a selected population, we are confident that our findings are generalisable to the UK or indeed any European population.
The Aberdeen Maternity and Neonatal Database and Scottish Morbidity Records (SMR) databases used in this study are subjected to quality control measures at regular intervals and there are numerous consistency checks in place to ensure the validity of data entry.
We were unable to link 27% of women with the SMR databases.
Introduction
Female pelvic floor disorders, such as urinary incontinence (UI) and pelvic organ prolapse (POP), are common and distressing conditions, particularly over the age of 40 years1 and are associated with a negative impact on a woman's social, physical and psychological well-being. However, the true prevalence of these disorders is difficult to determine. In this age group in the UK, approximately 6 million women (40%) have clinically significant UI symptoms, of whom 1 million (6.2%) are bothered by these symptoms and 2.2% find them socially disabling.2 UI has significant cost implications for the individual and the health services; in the UK it accounts for 0.3% of the NHS budget3 in addition to costs borne by the women.4 Similarly, POP is an increasingly prevalent condition, especially as the elderly population continues to increase in the UK.5
Conservative management is usually the first line of treatment. However, surgical treatment for UI/POP is common. Aparna et al6 reported that 18/10 000 women in the USA had undergone surgical treatment for POP in 2003, with rates rising with advancing age. In the UK, POP accounts for 20% of women on the waiting list for major gynaecological surgery and is the indication for 15% of hysterectomies.7 In England alone, 11 000 mid-urethral sling (MUS) procedures were performed for stress UI in 2009–2010.8 In 1997, Olsen et al9 in a widely quoted study showed that the lifetime risk for American women of undergoing a surgical operation for UI/POP by the age of 80 years was 11.1%. However, a recent study in Western Australia reported a significantly higher risk (19%) of POP surgery by the age of 85 years.10 Re-operation rates for UI/POP vary widely in the literature, ranging from 43–56% in tertiary referral centres11 12 to 17% in the general population.13
In the UK, the population is expected to increase from an estimated 61.4 million in 2008 to 71.6 million by 2033. Older age groups will increase the fastest, with the number of women over 75 years of age expected to almost double by 2033 (by 81% from 4.8 million to 8.7 million).14 The lifetime risk of surgically managed UI/POP has not been previously studied in a UK population despite its importance in medical services planning and health resources allocation.
Research questions
In this study we aimed to determine the lifetime risk of parous women undergoing primary or repeat pelvic floor surgery, that is surgical treatment for UI, POP and rectal prolapse or faecal incontinence (RP-FI) in a cohort of women representing the general population in the UK (primary outcome). We also aimed to determine re-operation rates for UI/POP, time intervals for repeat surgery and independent risk factors for undergoing primary and repeat UI/POP surgery (secondary outcomes).
Methods
Identification of the cohort
The Aberdeen Maternity and Neonatal Databank (AMND) (http://www.abdn.ac.uk/amnd) stores linked information on all obstetric related events occurring in women living in Aberdeen city and district since 1950 and currently contains data for 147 000 women. Consequently, it is possible to construct a complete reproductive history for each woman on the database. This database is therefore ideal for identifying a cohort of UK parous women, up to the age of 80 years, for linkage to hospital discharge data base (SMR01) in Scotland.
The Information and Services Division (ISD) is responsible for collating the morbidity returns from all NHS hospitals in Scotland. The Scottish Morbidity Records (SMR) 01/02 contain information on all outpatient/in-patient hospital admissions and discharges, with around 1 million new records added each year. A record linkage system is in place in Scotland using probability matching to link together general hospital discharge records, death registrations from the General Register Office for Scotland (GRO-S) and cancer registrations for individual patients. All these health related data sets are contemporaneously added to the system, which establishes a hospital career summary for individual patients in Scotland from 1975 to date. This linkage system therefore offers an ideal opportunity to assess the lifetime risk of POP and UI surgery in the cohort of women identified from the AMND.
To generate an anonymised study database of linked women up to 31 July 2010, records of parous women who were born between 1 January 1950 and 1 January 1968 identified on the AMND were linked by ISD to the SMR01 and the GRO-S death records using probability matching. The database contained information on episodes of diagnosis of and surgical treatment for pelvic floor disorders and the death records of women if available. The reproductive histories as recorded in the AMND database were extracted for these women.
Data available
A number of variables were considered as potential risk factors for undergoing pelvic floor surgery and were grouped as follows:
age of woman at first delivery: <20 years, 20–29 years or ≥30 years;
parity: 1, 2–4 or >4;
twin delivery;
mode of delivery: all spontaneous vaginal deliveries (SVD) or breech deliveries, all caesarean section (CS) deliveries, instrumental deliveries with at least one forceps delivery, instrumental deliveries but no forceps or a combination of SVD and CS;
time interval between deliveries: one delivery only, all intervals <2 years, all intervals ≥2 years or a mixture;
type of perineal wound sustained at delivery: intact perineum, all episiotomies, at least one third-degree tear or lacerations but no actual tears.
Reference groups were identified according to advice from a specialist urogynaecologist. The age of 80 years was chosen based on information from the Office for National Statistics (2009) showing that the life expectancy of women is 82 years in the UK and 80 years in Scotland.14
Statistical analysis
Cox regression was used to calculate the lifetime risk of pelvic floor surgery. Time was calculated from birth to date of operation (or censored at date of death/date of data extraction, as appropriate). The proportional hazards assumption for each covariate in each model was assessed using the log survival time versus the negative log of the survivor distribution function. Each covariate showed parallel curves, indicating the proportional hazards assumption was met. Unadjusted Cox regression models were carried out for the various risk factors mentioned above. The adjusted models were then implemented to identify independent risk factors for primary surgery for UI, POP or RP-FI. Time for these models was calculated from the date of first delivery to the date of operation (or censored appropriately). Sub-group analysis for women who had at least one operation was performed to calculate re-operation rates and logistic regression was used to determine any associations between the risk factors and repeat surgery. Logistic regression for repeat UI included type of primary operation as a potential risk factor.
Results
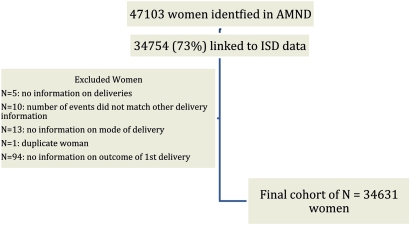
Of a total of 47 103 women identified in the AMND for initial linkage to the ISD database, 34 754 (73%) were linked. As 123 women were excluded, 34 631 women in the cohort were available for analysis (figure 1).
Figure 1.
Flow diagram of participants in the study. AMND, Aberdeen Maternity and Neonatal Database; ISD, Information and Services Division NHS Scotland.
Lifetime risk of pelvic floor surgery (UI, POP and/or RP-FI)
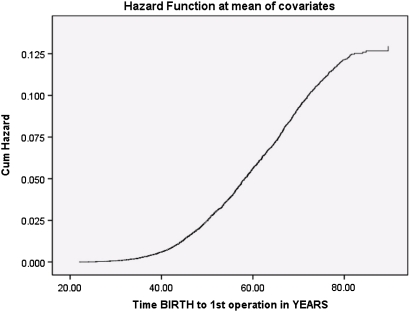
Within the cohort of women, 2130/34 631 (6.2%) had surgical treatment for UI, POP and/or RP-FI, 762 (2.2%) had an operation for UI, 1508 (4.4%) had a POP repair and 98 (0.3%) underwent an operation for RP-FI. The index surgery was for UI in 609 women (28.6%), POP in 1357 women (63.7%), combined UI and POP in 66 women (3.1%) and RP-FI in 78 women (3.7%). Figure 2 shows the cumulative hazard function for women for undergoing pelvic floor surgery with age. The lifetime distribution function can be calculated using this model. The probability of a woman undergoing pelvic floor surgery by age 80 was 0.115. Further analysis showed that the probability of undergoing UI surgery was 0.036, POP repair 0.091 and an operation for RP-FI 0.007.
Figure 2.
Plot of cumulative risk of surgery for pelvic floor disorders (POP/UI/RP-FI). Cum, cumulative; POP, pelvic organ prolapse; RP-FI, rectal prolapse or faecal incontinence; UI, urinary incontinence.
In other words, the lifetime risk for women for undergoing pelvic floor surgery by age 80, is 12.2%, while the lifetime risk of undergoing UI surgery is 3.6%, POP repair 9.5% and an operation for RP-FI 0.7%.
Risk factors for undergoing single pelvic floor surgery (UI, POP and/or RP-FI)
Table 1 shows the Cox regression model for each potential risk factor. There was a reduced risk of pelvic floor surgery if a woman had caesarean deliveries only (p<0.001), while the risk increased for women who sustained perineal lacerations in the absence of classified perineal tears (p<0.001). Body mass index (BMI) was considered to be an important risk factor, but was only available for 20 054 (58%) of the women. The same analysis in this subgroup including BMI, showed that women with increased BMI had an increased risk of pelvic floor surgery (p=0.007). With normal BMI as the reference group, the adjusted HRs (95% CI) for BMI were 0.60 (95% CI 0.34 to 1.06; p=0.078) for underweight, 1.22 (95% CI 1.06 to 1.41; p=0.007) for overweight and 0.94 (95% CI 0.72 to 1.22; p=0.63) for obesity.
Table 1.
Cox regression results for risks of undergoing pelvic floor surgery (POP, UI and/or RP-FI)
| Risk factor | All women (N=34 631) | No operation (N=32 501) | Operation (N=2130) | Unadjusted |
Adjusted |
||
| N (%) | N (%) | N (%) | HR (95% CI) | p Value | HR (95% CI) | p Value | |
| Mode of delivery | |||||||
| SVD/breech only | 21 210 (61.2%) | 19 776 (60.8%) | 1434 (67.3%) | 1.00 | |||
| CS only | 2551 (7.4%) | 2524 (7.8%) | 27 (1.3%) | 0.25 (0.16 to 0.36) | <0.001 | 0.27 (0.18 to 0.39) | <0.001 |
| Instrumental (at least one forceps) | 9022 (26.1%) | 8433 (25.9%) | 589 (27.7%) | 1.14 (1.03 to 1.26) | 0.007 | 1.13 (1.02 to 1.25) | 0.015 |
| Instrumental (at least one, but no forceps) | 663 (1.9%) | 639 (2.0%) | 24 (1.1%) | 1.42 (0.95 to 2.13) | 0.09 | 1.35 (0.90 to 2.02) | 0.15 |
| SVD+CS | 1185 (3.4%) | 1129 (3.5%) | 56 (2.6%) | 0.92 (0.70 to 1.20) | 0.53 | 0.89 (0.68 to 1.17) | 0.40 |
| Age at first delivery | |||||||
| Under 20 years | 5867 (16.9%) | 5510 (17.0%) | 357 (16.8%) | 0.88 (0.78 to 0.99) | 0.035 | 0.87 (0.78 to 0.98) | 0.021 |
| 20–29 years | 23 751 (68.6%) | 22 221 (68.4%) | 1530 (71.8%) | 1.00 | 1.00 | ||
| 30–49 years | 5013 (14.5%) | 4770 (14.7%) | 243 (11.4%) | 1.11 (0.97 to 1.28) | 0.12 | 1.34 (1.16 to 1.54) | <0.001 |
| Total number of deliveries | |||||||
| Single | 8699 (25.1%) | 8306 (25.6%) | 393 (18.5%) | 1.00 | 1.00 | ||
| 2–4 | 24 986 (72.1%) | 23 323 (71.8%) | 1663 (78.1%) | 1.41 (1.26 to 1.58) | <0.001 | 1.30 (1.16 to 1.46) | <0.001 |
| 5+ | 946 (2.7%) | 872 (2.7%) | 74 (3.5%) | 1.15 (0.90 to 1.48) | 0.27 | 1.10 (0.85 to 1.41) | 0.48 |
| Twins at some point | |||||||
| No | 34 148 (98.6%) | 32 044 (98.6%) | 2104 (98.8%) | 1.00 | |||
| Yes | 483 (1.4%) | 457 (1.4%) | 26 (1.2%) | 0.80 (0.54 to 1.17) | 0.25 | ||
| Time between deliveries | |||||||
| One delivery | 8699 (25.1%) | 8306 (25.6%) | 393 (18.5%) | 1.00 | |||
| All <2 years | 4151 (12.0%) | 3883 (11.9%) | 268 (12.6%) | 1.40 (1.19 to 1.63) | <0.001 | ||
| All ≥2 years | 16 510 (47.7%) | 15 463 (47.6%) | 1047 (49.2%) | 1.40 (1.24 to 1.57) | <0.001 | ||
| Mixture | 5271 (15.2%) | 4849 (14.9%) | 422 (19.8%) | 1.41 (1.23 to 1.62) | <0.001 | ||
| Type of perineal wound | |||||||
| No wound | 14 365 (41.5%) | 13 601 (41.8%) | 764 (35.9%) | 1.00 | 1.00 | ||
| All episiotomy | 9457 (27.3%) | 8852 (27.2%) | 605 (28.4%) | 1.19 (1.07 to 1.33) | 0.001 | 1.05 (0.94 to 1.18) | 0.37 |
| At least one third-degree tear | 162 (0.5%) | 150 (0.5%) | 12 (0.6%) | 1.99 (1.12 to 3.53) | 0.018 | 1.68 (0.95 to 2.97) | 0.076 |
| No perineal tears (lacerations only) | 10 647 (30.7%) | 9898 (30.5%) | 749 (35.2%) | 1.57 (1.41 to 1.73) | <0.001 | 1.36 (1.22 to 1.52) | <0.001 |
CS, caesarean section; POP, pelvic organ prolapse; RP-FI, rectal prolapse or faecal incontinence; SVD, spontaneous vaginal delivery; UI, urinary incontinence.
Subgroup analyses of independent risk factors for undergoing surgery for UI, POP or RP-FI separately are shown in tables 2–4. Undergoing at least one forceps delivery was an independent risk factor for requiring POP/RP-FI surgery but not for UI surgery. Similarly, sustaining a third-degree perineal tear was only a risk factor for a RP-FI operation. Delivering all siblings by CS was significantly protective against surgery for UI/POP but not RP-FI.
Table 2.
Cox regression results for risk factors for undergoing surgical treatment for UI
| Risk factor | No operation (N=32 501) | UI operation (N=762) | Unadjusted |
Adjusted |
||
| N (%) | N (%) | HR (95% CI) | p Value | HR (95% CI) | p Value | |
| Mode of delivery | ||||||
| SVD/breech only | 19 776 (60.8%) | 533 (69.9%) | 1.00 | 1.00 | ||
| CS only | 2524 (7.8%) | 18 (2.4%) | 0.40 (0.25 to 0.64) | <0.001 | 0.51 (0.32 to 0.83) | 0.007 |
| Instrumental (at least one forceps) | 8433 (25.9%) | 172 (22.6%) | 0.86 (0.72 to 1.02) | 0.08 | 0.86 (0.72 to 1.03) | 0.10 |
| Instrumental (at least one, but no forceps) | 639 (2.0%) | 12 (1.6%) | 1.72 (0.97 to 3.05) | 0.06 | 1.65 (0.93 to 2.94) | 0.09 |
| SVD+CS | 1129 (3.5%) | 27 (3.5%) | 1.12 (0.76 to 1.65) | 0.57 | 1.07 (0.73 to 1.58) | 0.72 |
| Age at first delivery | ||||||
| Under 20 years | 5510 (17.0%) | 182 (23.9%) | 1.28 (1.08 to 1.52) | 0.004 | 1.25 (1.05 to 1.48) | 0.011 |
| 20–29 years | 22 221 (68.4%) | 519 (68.1%) | 1.00 | 1.00 | ||
| 30–49 years | 4770 (14.7%) | 61 (8.0%) | 0.82 (0.63 to 1.07) | 0.14 | 1.00 (0.76 to 1.31) | 0.98 |
| Total number of deliveries | ||||||
| Single | 8306 (25.6%) | 126 (16.5%) | 1.00 | 1.00 | ||
| 2–4 | 23 323 (71.8%) | 614 (80.6%) | 1.63 (1.35 to 1.97) | <0.001 | 1.45 (1.18 to 1.77) | <0.001 |
| 5+ | 872 (2.7%) | 22 (2.9%) | 1.17 (0.74 to 1.84) | 0.51 | 0.98 (0.62 to 1.56) | 0.93 |
| Twins at some point | ||||||
| No | 32 044 (98.6%) | 754 (99.0%) | 1.00 | |||
| Yes | 457 (1.4%) | 8 (1.0%) | 0.70 (0.35 to 1.41) | 0.32 | ||
| Time between deliveries | ||||||
| One delivery | 8306 (25.6%) | 126 (16.5%) | 1.00 | |||
| All <2 years | 3883 (11.9%) | 97 (12.7%) | 1.57 (1.20 to 2.04) | 0.001 | ||
| All ≥2 years | 15 463 (47.6%) | 393 (51.6%) | 1.63 (1.33 to 1.99) | <0.001 | ||
| Mixture | 4849 (14.9%) | 146 (19.2%) | 1.59 (1.25 to 2.01) | <0.001 | ||
| Type of perineal wound | ||||||
| No wound | 13 601 (41.8%) | 265 (34.8%) | 1.00 | 1.00 | ||
| All episiotomy | 8852 (27.2%) | 239 (31.4%) | 1.32 (1.11 to 1.58) | 0.002 | 1.22 (1.01 to 1.46) | 0.035 |
| At least one third-degree tear | 150 (0.5%) | 2 (0.3%) | 0.90 (0.22 to 3.62) | 0.88 | 0.81 (0.20 to 3.24) | 0.76 |
| No perineal tears (lacerations only) | 9898 (30.5%) | 256 (33.6%) | 1.53 (1.29 to 1.82) | <0.001 | 1.31 (1.10 to 1.57) | 0.003 |
CS, caesarean section; SVD, spontaneous vaginal delivery; UI, urinary incontinence.
Table 3.
Cox regression results for risk factors for undergoing surgical treatment for POP
| Risk factor | No operation (N=32 501) | POP operation (N=1508) | Unadjusted |
Adjusted |
||
| N (%) | N (%) | HR (95% CI) | p Value | HR (95% CI) | p Value | |
| Mode of delivery | ||||||
| SVD/breech only | 19 776 (60.8%) | 1021 (67.7%) | 1.00 | 1.00 | ||
| CS only | 2524 (7.8%) | 7 (0.5%) | 0.09 (0.04 to 0.19) | <0.001 | 0.10 (0.05 to 0.21) | <0.001 |
| Instrumental (at least one forceps) | 8433 (25.9%) | 430 (28.5%) | 1.20 (1.07 to 1.34) | 0.002 | 1.19 (1.05 to 1.33) | 0.004 |
| Instrumental (at least one, but no forceps) | 639 (2.0%) | 16 (1.1%) | 1.41 (0.86 to 2.32) | 0.17 | 1.34 (0.82 to 2.21) | 0.25 |
| SVD+CS | 1129 (3.5%) | 34 (2.3%) | 0.80 (0.57 to 1.13) | 0.20 | 0.79 (0.56 to 1.12) | 0.18 |
| Age at first delivery | ||||||
| Under 20 years | 5510 (17.0%) | 221 (14.7%) | 0.77 (0.67 to 0.89) | <0.001 | 0.76 (0.66 to 0.89) | <0.001 |
| 20–29 years | 22 221 (68.4%) | 1100 (72.9%) | 1.00 | 1.00 | ||
| 30–49 years | 4770 (14.7%) | 187 (12.4%) | 1.20 (1.02 to 1.40) | 0.023 | 1.48 (1.26 to 1.73) | <0.001 |
| Total number of deliveries | ||||||
| Single | 8306 (25.6%) | 285 (18.9%) | 1.00 | 1.00 | ||
| 2–4 | 23 323 (71.8%) | 1171 (77.7%) | 1.38 (1.21 to 1.57) | <0.001 | 1.25 (1.09 to 1.44) | 0.001 |
| 5+ | 872 (2.7%) | 52 (3.4%) | 1.08 (0.80 to 1.45) | 0.61 | 1.04 (0.77 to 1.41) | 0.81 |
| Twins at some point | ||||||
| No | 32 044 (98.6%) | 1489 (98.7%) | 1.00 | |||
| Yes | 457 (1.4%) | 19 (1.3%) | 0.81 (0.52 to 1.28) | 0.37 | ||
| Time between deliveries | ||||||
| One delivery | 8306 (25.6%) | 285 (18.9%) | 1.00 | |||
| All <2 years | 3883 (11.9%) | 196 (13.0%) | 1.42 (1.18 to 1.70) | <0.001 | ||
| All ≥2 years | 15 463 (47.6%) | 727 (48.2%) | 1.35 (1.18 to 1.55) | <0.001 | ||
| Mixture | 4849 (14.9%) | 300 (19.9%) | 1.37 (1.16 to 1.61) | <0.001 | ||
| Type of perineal wound | ||||||
| No wound | 13 601 (41.8%) | 527 (34.9%) | 1.00 | 1.00 | ||
| All episiotomy | 8852 (27.2%) | 412 (27.3%) | 1.19 (1.04 to 1.35) | 0.009 | 1.03 (0.90 to 1.17) | 0.70 |
| At least one third-degree tear | 150 (0.5%) | 6 (0.4%) | 1.50 (0.67 to 3.34) | 0.33 | 1.23 (0.55 to 2.76) | 0.61 |
| No perineal tears (lacerations only) | 9898 (30.5%) | 563 (37.3%) | 1.73 (1.53 to 1.94) | <0.001 | 1.50 (1.32 to 1.70) | <0.001 |
CS, caesarean section; POP, pelvic organ prolapse; SVD, spontaneous vaginal delivery.
Table 4.
Cox regression results for risk factors for undergoing surgical treatment for RP-FI
| Risk factor | No operation (N=32 501) | RP or FI operation (N=1508) | Unadjusted |
Adjusted |
||
| N (%) | N (%) | HR (95% CI) | p Value | HR (95% CI) | p Value | |
| Mode of delivery | ||||||
| SVD/breech only | 19 776 (60.8%) | 56 (57.1%) | 1.00 | 1.00 | ||
| CS only | 2524 (7.8%) | 2 (2.0%) | 0.45 (0.11 to 1.84) | 0.26 | 0.41 (0.10 to 1.71) | 0.22 |
| Instrumental (at least one forceps) | 8433 (25.9%) | 37 (37.8%) | 1.90 (1.25 to 2.88) | 0.003 | 1.81 (1.18 to 2.77) | 0.007 |
| Instrumental (at least one, but no forceps) | 639 (2.0%) | 1 (1.0%) | 1.39 (0.19 to 10.1) | 0.75 | 1.35 (0.18 to 9.87) | 0.77 |
| SVD+CS | 1129 (3.5%) | 2 (2.0%) | 0.83 (0.20 to 3.40) | 0.79 | 0.83 (0.20 to 3.39) | 0.79 |
| Age at first delivery | ||||||
| Under 20 years | 5510 (17.0%) | 14 (14.3%) | 0.77 (0.43 to 1.36) | 0.36 | ||
| 20–29 years | 22 221 (68.4%) | 73 (74.5%) | 1.00 | |||
| 30–49 years | 4770 (14.7%) | 11 (11.2%) | 0.97 (0.52 to 1.83) | 0.93 | ||
| Total number of deliveries | ||||||
| Single | 8306 (25.6%) | 16 (16.3%) | 1.00 | |||
| 2–4 | 23 323 (71.8%) | 77 (78.6%) | 1.65 (0.96 to 2.83) | 0.067 | ||
| 5+ | 872 (2.7%) | 5 (5.1%) | 1.86 (0.68 to 5.09) | 0.23 | ||
| Twins at some point | ||||||
| No | 32 044 (98.6%) | 96 (98.0%) | 1.00 | |||
| Yes | 457 (1.4%) | 2 (2.0%) | 1.32 (0.33 to 5.34) | 0.70 | ||
| Time between deliveries | ||||||
| One delivery | 8306 (25.6%) | 16 (16.3%) | 1.00 | |||
| All <2 years | 3883 (11.9%) | 8 (8.2%) | 1.05 (0.45 to 2.45) | 0.91 | ||
| All ≥2 years | 15 463 (47.6%) | 54 (55.1%) | 1.82 (1.04 to 3.19) | 0.035 | ||
| Mixture | 4849 (14.9%) | 20 (20.4%) | 1.66 (0.86 to 3.21) | 0.13 | ||
| Type of perineal wound | ||||||
| No wound | 13 601 (41.8%) | 43 (43.9%) | 1.00 | 1.00 | ||
| All episiotomy | 8852 (27.2%) | 26 (26.5%) | 0.98 (0.60 to 1.60) | 0.94 | 0.80 (0.48 to 1.33) | 0.40 |
| At least one third-degree tear | 150 (0.5%) | 7 (7.1%) | 21.8 (9.72 to 48.7) | <0.001 | 16.9 (7.44 to 38.3) | <0.001 |
| No perineal tears (lacerations only) | 9898 (30.5%) | 22 (22.4%) | 0.83 (0.49 to 1.38) | 0.47 | 0.76 (0.45 to 1.29) | 0.31 |
CS, caesarean section; RP-FI, rectal prolapse or faecal incontinence; SVD, spontaneous vaginal delivery.
Re-operation rate for UI and/or POP
Four hundred and seven women had more than one operation for UI/POP, giving a re-operation rate of 19%. Two hundred and thirty-eight women had at least one repeat POP operation with a re-operation rate of 15.8% and a median (IQR) of 3.0 (1.00–8.25) years between the index and repeat surgery. Sixty-seven women had at least one repeat UI surgery, giving a re-operation rate of 8.8%. The median (IQR) time between the index and repeat UI surgery was 2.80 (0.94–8.07) years. The median time interval for repeat UI surgery varied according to the type of index operation ranging from 0.93 (0.27–2.49) years for mid-urethral slings to 4.20 (1.73–8.38) years for retropubic abdominal procedures.
Risk factors for re-operation for UI/POP
The re-operation rate for UI was 3.2% (11/342) in the MUS group, 10.7% (34/319) in the abdominal retropubic surgery group, 17.5% (14/80) in the anterior colporraphy group and 50% (5/10) in the peri-urethral injectables group. Table 5 shows the independent risk factors for re-operation for UI. Using the abdominal retropubic group as the reference group, women undergoing MUS had a significantly lower risk of repeat UI surgery.
Table 5.
Results of logistic regression for risk of re-operation for UI
| Risk factor | UI operation |
Unadjusted analysis |
Adjusted analysis |
|||
| One (N=695) | >1 (N=67) | OR (95% CI) | p Value | OR (95% CI) | p Value | |
| Type of first UI surgery | ||||||
| Abdominal retropubic procedures | 285 (41.0%) | 34 (50.7%) | 1.00 | 1.00 | ||
| Mid-urethral slings | 331 (47.6%) | 11 (16.4%) | 0.28 (0.14 to 0.56) | <0.001 | 0.30 (0.15 to 0.60) | 0.001 |
| Anterior colporrhapy | 66 (99.5%) | 14 (20.9%) | 1.78 (0.90 to 3.50) | 0.096 | 1.92 (0.97 to 3.82) | 0.063 |
| Peri-urethral injectables | 5 (0.7%) | 5 (7.5%) | 8.38 (2.31 to 30.4) | 0.001 | 9.05 (2.42 to 33.8) | 0.001 |
| Repair of uro-genital fistulae | 8 (1.2%) | 3 (4.5%) | 3.14 (0.80 to 12.4) | 0.102 | 2.50 (0.58 to 10.8) | 0.22 |
| Mode of delivery | ||||||
| SVD only | 488 (700.2%) | 45 (67.2%) | 1.00 | |||
| CS only | 16 (2.3%) | 2 (3.0%) | 1.36 (0.30 to 6.08) | 0.69 | ||
| At least one forceps | 158 (22.7%) | 14 (20.9%) | 0.96 (0.51 to 1.80) | 0.90 | ||
| At least one instrumental but no forceps | 9 (1.3%) | 3 (4.5%) | 3.62 (0.95 to 13.8) | 0.06 | ||
| SVD+CS | 24 (3.5%) | 3 (4.5%) | 1.36 (0.39 to 4.68) | 0.63 | ||
| Age at first delivery | ||||||
| Under 20 years | 166 (23.9%) | 16 (23.9%) | 0.93 (0.51 to 1.67) | 0.80 | ||
| 20–29 years | 470 (67.6%) | 49 (73.1%) | 1.00 | |||
| 30–49 years | 59 (8.5%) | 2 (3.0%) | 0.33 (0.08 to 1.37) | 0.13 | ||
| Total number of deliveries | ||||||
| One | 116 (16.7%) | 10 (14.9%) | 1.00 | |||
| 2–4 | 558 (80.3%) | 56 (83.6%) | 1.16 (0.58 to 2.35) | 0.67 | ||
| 5+ | 21 (3.0%) | 1 (1.5%) | 0.55 (0.07 to 4.55) | 0.58 | ||
| Occurrence of twins | ||||||
| No | 687 (98.8%) | 67 (100%) | ||||
| Yes | 8 (1.2%) | 0 (0%) | ||||
| Time between deliveries | ||||||
| One delivery | 116 (16.7%) | 10 (14.9%) | 1.00 | |||
| All <2 years | 89 (12.8%) | 8 (11.9%) | 1.04 (0.40 to 2.75) | 0.93 | ||
| All ≥2 years | 354 (19.6%) | 10 (14.9%) | 1.28 (0.62 to 2.64) | 0.51 | ||
| Mixture | 136 (19.6%) | 10 (14.9%) | 0.85 (0.34 to 2.12) | 0.73 | ||
| Type of perineal wound | ||||||
| No wound | 239 (34.4%) | 26 (38.8%) | 1.00 | 1.00 | ||
| All episiotomy | 211 (30.4%) | 28 (41.8%) | 1.22 (0.69 to 2.15) | 0.49 | 1.22 (0.68 to 2.19) | 0.51 |
| At least one third-degree tear | 1 (0.1%) | 1 (1.5%) | 9.19 (0.56 to 151) | 0.12 | 4.83 (0.25 to 92.8) | 0.30 |
| No perineal tears (lacerations only) | 244 (35.1%) | 12 (17.9%) | 0.45 (0.22 to 0.92) | 0.028 | 0.46 (0.22 to 0.95) | 0.037 |
CS, caesarean section; SVD, spontaneous vaginal delivery; UI, urinary incontinence.
Table 6 shows the unadjusted ORs for the different risk factors for repeat POP operation. Only women aged 30–49 years at first delivery were less likely to have a re-operation for POP. Seventy-two of 814 women underwent repeat anterior repair at some point with a re-operation rate for the anterior compartment of 8.8%. Similarly, 57/775 women underwent a repeat posterior repair with a re-operation rate of 7.4% for the posterior compartment. For those women whose initial POP operation was in the anterior or posterior compartment, the median (IQR) time interval for repeat surgery was 3 years (1, 9.25) and 4 years1 9 for those women whose initial POP operation was in the anterior and posterior compartments respectively.
Table 6.
Results of logistic regression for risk of re-operation for POP repair
| Risk factor | POP operation |
Unadjusted |
||
| One (N=1270) | >1 (N=238) | OR (95% CI) | p Value | |
| Mode of delivery | ||||
| SVD only | 857 (67.5%) | 164 (68.9%) | 1.00 | |
| CS only | 7 (0.6%) | 0 (0%) | ||
| At least one forceps | 365 (28.7%) | 65 (27.3%) | 0.93 (0.68 to 1.27) | 0.65 |
| At least one instrumental, but no forceps | 15 (1.2%) | 1 (0.4%) | 0.35 (0.05 to 2.66) | 0.31 |
| SVD+CS | 26 (2.0%) | 8 (3.4%) | 1.61 (0.72 to 3.61) | 0.25 |
| Age at first delivery | ||||
| Under 20 years | 174 (13.7%) | 47 (19.7%) | 1.44 (1.00 to 2.06) | 0.049 |
| 20–29 years | 926 (72.9%) | 174 (73.1%) | 1.00 | |
| 30–49 years | 170 (13.4%) | 17 (7.1%) | 0.53 (0.31 to 0.90) | 0.018 |
| Total number of deliveries | ||||
| One | 246 (19.4%) | 39 (16.4%) | 1.00 | |
| 2–4 | 978 (77.0%) | 193 (81.1%) | 1.25 (0.86 to 1.81) | 0.25 |
| 5+ | 46 (3.6%) | 6 (2.5%) | 0.82 (0.33 to 2.06) | 0.68 |
| Occurrence of twins | ||||
| No | 1254 (98.7%) | 235 (98.7%) | 1.00 | |
| Yes | 16 (1.3%) | 3 (1.3%) | 1.00 (0.29 to 3.46) | 0.99 |
| Time between deliveries | ||||
| One delivery | 246 (19.4%) | 39 (16.4%) | 1.00 | |
| All <2 years | 167 (13.1%) | 29 (12.2%) | 1.10 (0.65 to 1.84) | 0.73 |
| All ≥2 years | 608 (47.9%) | 119 (50.0%) | 1.24 (0.84 to 1.83) | 0.29 |
| Mixture | 249 (19.6%) | 51 (21.4%) | 1.29 (0.82 to 2.03) | 0.27 |
| Type of perineal wound | ||||
| No wound | 442 (34.8%) | 85 (35.7%) | 1.00 | |
| All episiotomy | 361 (28.4%) | 51 (21.4%) | 0.74 (0.51 to 1.07) | 0.11 |
| At least one third-degree tear | 5 (0.4%) | 1 (0.4%) | 1.04 (0.12 to 9.01) | 0.97 |
| No perineal tears (lacerations only) | 462 (36.4%) | 101 (42.4%) | 1.14 (0.83 to 1.56) | 0.43 |
CS, caesarean section; POP, pelvic organ prolapse; SVD, spontaneous vaginal delivery.
Discussion
In this large longitudinal epidemiological study, we have established that the lifetime risk for parous women in a UK population of undergoing a single pelvic floor surgery (UI/POP/RP-FI) was 12.2% by the age of 80 years. Olsen et al9 reported an 11.1% lifetime risk for women of undergoing a single operation for UI/POP by the age of 80 years. Their results were echoed by Fialkow et al15 in 2008, who showed a comparable 11.8% lifetime risk of UI/POP surgery in a similar cohort of American women. The latter two studies were limited because they sampled health maintenance organisations. Therefore the results may not be applicable to European or wider US populations, since generalisability is poor as a result of the exclusion of large groups, such as the elderly, socially disabled, those of lower social class and individuals with chronic illness. Furthermore, both study designs were cross-sectional and therefore had a limited follow-up period. Our study is a longitudinal retrospective study spanning the lifetime of a group of women representing the general population in the UK. We chose 80 years as our age limit as it represents the average life-span of women in the UK.14 The population in Aberdeen city and district is predominantly Caucasian, but there are a number of ethnic minority communities including those of Asian, African and Eastern Europe origin, and therefore is deemed to be quite representative of the general UK population.
Unlike previous studies, we calculated the lifetime risk of surgical treatment of various pelvic floor disorders separately. The lifetime risk of women of undergoing a single UI operation in our study was 3.6%. The MRC Leicestershire study2 showed that 33.6% of the population in the UK above the age of 40 years describe UI symptoms, but only 6.2% report these symptoms as bothersome. A recent French study showed similar findings with a 29% prevalence of female UI, although only 9% sought medical help.16 Conservative measures such as pelvic floor muscle training (PFMT) can be quite successful in the management of 50–60% of women with UI,17 while surgical treatment is usually second line treatment. Therefore the lifetime risk reported in our study is likely to be a true reflection of current clinical practice.
Our study showed that the lifetime risk of women undergoing a single POP surgery was 9.5%, which was almost 50% lower than the risk for women in Western Australia. In 2010, Smith et al10 reported on their cross-sectional study of the general female population in Western Australia conducted between 2001 and 2005, and calculated a higher lifetime risk of POP surgery of 19% by the age of 85 years. It is difficult to explain the disparity in the results between both general population-based studies. The difference in design, that is, longitudinal versus cross-sectional, is unlikely to be a major influence. In a European study, Hove et al18 assessed the entire population of a small town in the Netherlands and reported that 40% of women aged 45–85 years had POP ≥stage II on examination, but only 12% of the women were symptomatic. We therefore believe that, with the current concept of only treating symptomatic and/or severe prolapse and knowing that a percentage of women will opt for conservative measures such as vaginal pessaries, the lifetime surgical risk reported in our study is likely to be more representative of clinical practice in the UK and European countries.
The re-operation rate for UI/POP in our study was 19% and was comparable with the 17% reported by Denman et al13 in a 10-year follow-up prospective study. The re-operation rate in the latter study increased to 21% after adjustment for missing women in the follow-up. Olsen et al9 reported a re-operation rate of 29% for UI/ POP within 5 years in their cross-sectional study. It is important to note that 50% of their population were smokers (current/former) and over 20% had chronic lung disease which may have contributed to their higher re-operation rates. In our study, the re-operation rates for UI and POP were 8.8% and 15.8%, respectively; these were comparable to the 8% and 13% re-operation rates for UI and POP, respectively, reported by Clark et al19 in their 5-year prospective study. Similarly, Fialkow et al15 showed an 8.6% re-operation rate for UI over 8 years in a retrospective cohort study. The POP re-operation rates were not hugely different for the anterior and posterior compartments. Similar results were reported by Clark et al19 who found 5-year re-operation rates for the anterior and posterior compartments of 8% and 11%, respectively, with higher re-operation rates (15% vs 12%, respectively) if associated with apical prolapse.
In our study, exclusive delivery by CS compared to only SVD was found to be protective against pelvic floor surgery for each of UI, POP and RP-FI (≈60%). This protective effect was not seen if a woman had a mixture of caesarean and vaginal deliveries. A single forceps delivery significantly increased the risk of surgery for POP and/or RP-FI but not for UI. Similar results were reported by MacArthur et al20 in their 12-year prospective study and Larsson et al21 in their nested case–control study. In our study, having two to four deliveries was an independent risk factor for POP/UI surgery compared to a single delivery. A Dutch group previously showed having two or three deliveries was a risk factor for the development of POP; interestingly the risk was not further increased if parity was >3.5 Conversely, MacArthur et al20 found parity ≥4 to be a risk factor for UI. The latter two studies assessed risk factors for the development of symptomatic UI/POP rather than risk factors for undergoing surgical treatment. It is evident from our data that increased parity and vaginal forceps deliveries are risk factors for the development of UI/POP that warrant surgical management. As expected, sustaining a third-degree perineal tear was a risk factor for undergoing RP-FI surgery. Episiotomy was not found to be protective.
Analysis of potential risk factors for re-operation for UI/POP did not reveal specific independent risk factors, except for delayed age at first delivery (30–49 years), which seems to be of little clinical significance. These results were in agreement with other studies in the literature,9 13 15 all of which failed to detect independent risk factors for repeat UI/POP surgery. However, it was evident that women undergoing MUS had a significantly reduced risk of re-operation for UI when compared to abdominal retropubic surgery. It can be argued that MUS have not been used in surgical practice for as long as abdominal retropubic procedures and therefore the detected reduced risk may be subject to bias. However, the finding that the median time interval for repeat UI surgery was 1 year following MUS compared to 4 years following retropubic abdominal procedures indicates that repeat surgery following MUS is likely to have been captured within the time frame of this study. Conversely, peri-urethral injections were associated with a significantly higher risk of repeat UI surgery. Fialkow et al15 have previously reported a reduced risk of repeat UI surgery following Burch colposuspension compared to traditional slings.
Strengths and limitations
To our knowledge, this is the first study to report the lifetime risk for women in the UK of undergoing surgical treatment for UI/POP/RP-FI.
The cohort was large and there was a long duration of follow-up.
As the study represents the general population rather than a selected population, we are confident that our findings are generalisable to the UK or indeed any European population.
Aberdeen city and district had a relatively stable population over the last century, minimising loss to follow-up.
The AMND and SMR databases used in this study are subjected to quality control measures at regular intervals and there are numerous consistency checks in place to ensure the validity of data entry.
Good quality data relating to both exposure (AMND) and outcomes (SMR) added strength and validity to the findings.
However, our study had a number of limitations:
Information was missing on smoking and BMI in a large proportion of women.
We were unable to link 27% of the women with the SMR databases. There are a number of possible reasons for this:
Failure to match the health records for these women with the data available on the AMND.
These women are alive and have moved away from Scotland.
These women may have undergone further treatment on private basis.
In the latter two situations, their hospital admissions would not be recorded by the ISD in Scotland. As migration is highly correlated with socio-economic status, we cannot rule out selection bias resulting from this.
There is also a possibility, albeit small, of misclassification bias resulting from incorrect linkage due to error in probability matching.
Clinical and research implications
We believe our results provide essential information for policy makers in the UK and Europe regarding healthcare planning, resource allocation and staff training. Increased BMI and forceps deliveries were independent risk factors for undergoing surgery for pelvic floor disorders, both of which are potentially avoidable. Exclusive delivery by CS was found to be protective against pelvic floor surgery, although not 100% so. Other risks associated with delivery by CS should be taken into consideration when making decisions regarding mode of delivery.
Conclusion
Our study reveals that more than one in 10 parous women in the UK, over their lifetime, will require at least one surgical procedure for pelvic floor dysfunction, with 19% requiring more than one procedure. Independent risk factors for pelvic floor surgery were forceps delivery and delayed initial childbearing. Protective factors included early initial delivery and delivery exclusively by CS. This information is essential for clinicians, patients and policy makers regarding counselling, decision making and the allocation of healthcare resources.
Supplementary Material
Footnotes
To cite: Abdel-fattah M, Familusi A, Fielding S, et al. Primary and repeat surgical treatment for female pelvic organ prolapse and incontinence in parous women in the UK: a register linkage study. BMJ Open 2011;1:e000206. doi:10.1136/bmjopen-2011-000206
Funding: This research was funded by an NHS Grampian Endowment grant for data linkage and administrative work. The University of Aberdeen acted as sponsors for this research project, but the findings and their interpretation in this study are the authors' own. All authors were employed by the University of Aberdeen at the time of conducting this research.
Competing interests: None.
Ethics approval: This research proposal was approved by the Steering Committee of the Aberdeen Maternity and Neonatal Databank and the Privacy Advisory Committee of the Information and Services Division NHS Scotland.
Contributors: MAF conceived the research idea, wrote the first draft of the paper and was responsible for the clinical interpretation of the findings. AF facilitated data linkage, cleaned the linked data and conducted initial analyses. SF conducted and supervised all statistical analyses. JF conducted initial literature searches. SB gave methodological support in the designing of the study and extraction and linkage of data. All authors contributed to the writing of the final draft of the paper. MAF is the guarantor of this paper.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: Data tables and summaries are available from corresponding author at m.abdelfattah@abdn.ac.uk.
References
- 1.National Institute for Health and Clinical Excellence (NICE) and National Collaborating Centre for Women's and Children's Health Urinary Incontinence; The Management Of Urinary Incontinence In Women. London: Royal College of Obstetricians and Gynaecologists Press, 2006 [Google Scholar]
- 2.Perry S, Shaw C, Assassa P, et al. An epidemiological study to establish the prevalence of urinary symptoms and felt need in the community: the Leicestershire MRC Incontinence Study. Leicestershire MRC Incontinence Study Team. J Public Health Med 2000;22:427–34 [DOI] [PubMed] [Google Scholar]
- 3.Turner DA, Shaw C, McGrother CW, et al. ; MRC Incontinence Team The cost of clinically significant urinary storage symptoms for community dwelling adults in the UK. BJU Int 2004;93:1246–52 [DOI] [PubMed] [Google Scholar]
- 4.Papanicolaou S, Pons ME, Hampei C, et al. Medical resource utilisation and cost of care for women seeking treatment for urinary incontinence in an outpatient setting: examples from three countries participating in the PURE study. Maturitas 2005;52(Suppl 2):S35–47 [DOI] [PubMed] [Google Scholar]
- 5.Hove M, Pool-Goudzwaard A, Eijkemans M, et al. The prevalence of pelvic organ prolapse symptoms and signs and their relation with bladder and bowel disorders in a general female population. Int Urogynecol J 2009;20:1037–45 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Aparna D, Kohli SN, Rajan SS, et al. The age distribution, rates, and types of surgery for pelvic organ prolapse in USA. Int Urogynecol J 2008;19:421–8 [DOI] [PubMed] [Google Scholar]
- 7.Carlson KJ, Nicholos DH, Schiff I. Indications for hysterectomy. N Engl J Med 1993;328:856–60 [DOI] [PubMed] [Google Scholar]
- 8.Jacklin C, Ducket J. Analytic model comparing the cost utility of TVT versus duloxetine in women with urinary stress incontinence. Int Urogynecol J 2010;21:977–84 [DOI] [PubMed] [Google Scholar]
- 9.Olsen AL, Smith VJ, Bergstrom JO, et al. Epidemiology of surgically managed pelvic organ prolapse and urinary incontinence. Obstet Gynecol 1997;89:501–6 [DOI] [PubMed] [Google Scholar]
- 10.Smith F, Holman CD, Moorin RE, et al. Lifetime risk of undergoing surgery for pelvic organ prolapse. Obstet Gynaec 2010;116:1096–100 [DOI] [PubMed] [Google Scholar]
- 11.Wiskind AK, Creighton SM, Stanton SL. The incidence of genital prolapse after the Burch colposuspension. Am J Obstet Gynecol 1992;167:399–405 [DOI] [PubMed] [Google Scholar]
- 12.Kjolhede P, Noren B, Ryden G. Prediction of genital prolapse after Burch colposuspension. Acta Obstet Gynecol Scand 1996;75:849–54 [DOI] [PubMed] [Google Scholar]
- 13.Denman MA, Gregory WT, Boyles SH, et al. Reoperation 10 years after surgically managed pelvic organ prolapse and urinary incontinence. Am J Obstet Gynecol 2008;198:555.e1–5 [DOI] [PubMed] [Google Scholar]
- 14.Office of National Statistics. 2009. http://www.statistics.gov.uk
- 15.Fialkow MF, Newton KM, Lentz GM, et al. Lifetime risk of surgical management for pelvic organ prolapse or urinary incontinence. Int Urogynecol J 2008;19:437–40 [DOI] [PubMed] [Google Scholar]
- 16.Lasserre A, Pelat C, Guéroult V, et al. Urinary incontinence in french women: prevalence, risk factors and impact on quality of life. Eur Urol 2009;56:177–83 [DOI] [PubMed] [Google Scholar]
- 17.Imamura M, Abrams P, Bain C, et al. Systematic review and economic modelling of the effectiveness and cost effectiveness of non-surgical treatments for women with stress urinary incontinence. Health Technol Assess 2010;14:1–188 iii-iv. [DOI] [PubMed] [Google Scholar]
- 18.Hove M, Bloembergen H, Vierhout M, et al. Distribution of pelvic organ prolapse (POP) in the general population. Int Congr Ser 2005;1279:383–6 [Google Scholar]
- 19.Clark AL, Gregory T, Smith VJ, et al. Epidemiologic evaluation of reoperation for surgically treated pelvic organ prolapse and urinary incontinence. Am J Obstet Gynecol 2003;189:1261–7 [DOI] [PubMed] [Google Scholar]
- 20.MacArthur C, Glazener C, Lancashire R, et al. ; On behalf of the ProLong study group Exclusive caesarean section delivery and subsequent urinary and faecal incontinence: a 12-year longitudinal study. BJOG 2011;118:1001–7 [DOI] [PubMed] [Google Scholar]
- 21.Larsson C, Källen K, Andolf E. Cesarean section and risk of pelvic organ prolapse: a nested case-control study. Am J Obstet Gynecol 2009;200:243.e1–4 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.