Abstract
The characteristics of dispositional mindfulness have rarely been explored in unhealthy populations. We sought to evaluate its association(s) with psychological morbidity and disease severity in 30 outpatients with implantable cardioverter defibrillators naïve to mindfulness training. We used the Five Facets of Mindfulness and the Hospital Anxiety and Depression Scale to measure dispositional mindfulness and anxiety/depression, respectively. Associations were estimated using linear regression models. Higher dispositional mindfulness was observed in patients with lower anxiety scores (β = − 1.10, CI: −1.71, −0.49) and no history of depression (β = − 7.95; CI: −14.31, −1.6) by univariate analysis. No associations were observed with disease severity or other covariates. In conclusion, psychological well-being and psychological morbidity, and not disease severity, appear to be associated with dispositional mindfulness in patients with implantable cardioverter defibrillators. Further research is needed to confirm these findings.
Keywords: dispositional mindfulness, cardiovascular disease, implantable cardioverter defibrillators, mindfulness training
Introduction
The practice of mindfulness has been central to Eastern philosophies for centuries. In these traditions, the cultivation of mindfulness is an important component of a path leading to a reduction of suffering and an increase in qualities such as compassion, equanimity, and wisdom. In Western medical settings, mindfulness practice has been shown to reduce anxiety, depression, sleep disturbance and a variety of physical symptoms in different medical conditions1 such as cancer,2–5 chronic pain,6, 7 anxiety disorders,8 rheumatoid arthritis9 and fibromyalgia,10 with an estimated effect size around 0.5.1, 11 When associated with cognitive behavioral therapy, mindfulness training reduces the rate of relapse/recurrence in major depression.12
While the current evidence for a beneficial role of mindfulness training on physical and psychological health has been fairly well established, very limited work has been done to investigate whether the ability to be mindful in everyday life13, 14 (i.e. “dispositional”, or “trait”, mindfulness) is associated with better psychological and physical well-being in individuals who were never exposed to formal mindfulness training. In fact, although dispositional mindfulness can be purposely cultivated and enhanced through mindfulness practice,15 it is not necessarily related to previous training.
Dispositional mindfulness has been linked with several personality and mood characteristics across diverse, generally healthy, populations. Negative correlations have been observed between dispositional mindfulness measured with the Mindful Attention Awareness Scale 13 and personality characteristics such as neuroticism (particularly with the facets of depression, self-consciousness, and angry hostility)13, 16, 17 and with self-reported aggressiveness and hostile attribution bias.18 An inverse relationship has been shown with depression and anxiety. 13 Similar associations have been documented by Baer and colleagues19, 20 and in a recent cross-sectional population-based study21 using the Five Facets of Mindfulness questionnaire.22
Finally, Shapiro and colleagues23 have shown that participants in a Mindfulness Based Stress Reduction program with higher levels of pre-training dispositional mindfulness had a better response to mindfulness training, with larger increases in mindfulness, subjective well-being, empathy, and hope, and a larger reduction in perceived stress.
The studies of dispositional mindfulness mentioned above, however, have all been conducted in healthy individuals, and the characteristics of dispositional mindfulness have rarely been explored in populations with chronic diseases. In patients with cancer, higher pre-intervention mindfulness levels were associated with lower mood disturbance and stress.13 The authors of this study noted that the baseline average mindfulness score in this group was higher than in other populations, and hypothesized that the experience of cancer may lead patients to reconsider their view of life, and to become more present-focused. Patients receiving an implantable cardioverter defibrillator (ICD) present some characteristics similar to those of cancer patients. ICD patients are facing a severe chronic disease and are, by definition, facing death, either because they are at risk of dying suddenly or because they survived a prior cardiac arrest. Thus, the purpose of this study was to evaluate the characteristics of dispositional mindfulness in a group of patients with severe cardiovascular disease who were naïve to mindfulness practices, and specifically whether mindfulness is associated with indicators of disease severity and with psychological morbidity and well-being.
Methods
This study was a cross-sectional analysis of baseline data collected from 30 patients enrolled in a pilot randomized controlled trial of a mindfulness-based intervention for patients undergoing an ICD procedure and/or who had ICD related events (shocks). The study was conducted at the university campus of the UMass Memorial Medical Center Worcester, MA. All consecutive candidates to an ICD related procedure were screened for study eligibility within a month of the procedure. Patients were eligible if they were 21 or older, able to understand and speak English, and had access to a telephone. Patients were excluded under the following conditions: inability/unwillingness to give informed consent, signs of cognitive impairment, New York Heart Association functional class >III or angina Canadian Cardiovascular Society class III and IV or otherwise clinically unstable, pending coronary by-pass or heart transplantation, co-morbid life threatening conditions, and ongoing severe depression or psychosis. Eligible patients received an interest survey and a letter inviting them to participate in the study. If the patient expressed interest, a screening visit was scheduled. After confirmation of study eligibility and informed consent was provided, patients completed a series of self-administered questionnaires.
Assessments
Mindfulness scores
Baseline and post-intervention mindfulness scores were measured using the Five Facets of Mindfulness questionnaire,19,22 a self-report measure of mindfulness derived from a factor analysis of questionnaires measuring mindfulness in daily life. To reduce patient burden we used a shortened version consisting of 15 items, each rated on a Likert scale ranging from one (never or very rarely true) to five (very often or always true), with total scores ranging from zero to 75.
Study covariates
Information was collected on demographic characteristics (age, gender, income, marital status, education and ethnicity) and on other variables that may affect dispositional mindfulness such as previous history of anxiety and depression and related prescriptions; baseline anxiety and depression scores; disease-related characteristics such as ejection fraction, New York Heart Association functional class and history of cardiac arrest; use of other (non mindfulness-based) alternative therapies during the previous month; and physical activity. Demographic information, functional class, ejection fraction (obtained from the most recent echocardiogram or ventriculogram) and other clinical information were collected from the electronic version of the medical record. Anxiety and depression scores were each measured using the Hospital Anxiety and Depression Scale,24, 25 a 14-items self-administered questionnaire with two sub-scales measuring anxiety and depression, with higher scores indicating greater psychological morbidity. Since in cardiac patients symptoms of the underlying cardiac disease maybe similar to those resulting from the somatic manifestations of anxiety and depression, we chose the Hospital Anxiety and Depression Scale because it focuses on cognitive symptoms instead of physical symptoms. Its validity has been confirmed in both hospital settings and primary care,26–28 and a correlation between 0.6–0.8 has been reported between this scale and the Beck Depression Inventory and the State-Trait Anxiety Inventory. Information about the use of complementary/alternative therapies and physical activity during the previous month was collected through self-administered questionnaires.
Statistical analysis
A preliminary analysis was conducted to determine the variability and distribution of mindfulness scores, to evaluate the appropriateness of the model’s assumptions, and to assess correlations between covariates to avoid collinearity in the multivariate model. Variables were checked for missing data and distribution, if continuous; for counts, if categorical. Loess curves were used to examine and test linear vs. non-linear associations. Age, ejection fraction, time from ICD implantation, anxiety and mindfulness scores were treated as continuous variables. Sex, race, financial status, marital status, education, use of antidepressant and anxiolytics, previous history of anxiety and depression, psychotropic and anti-arrhythmic therapy, type of ICD implanted (bi-ventricular vs. ventricular), prior shocks, history of cardiac arrest or severe cardiac arrhythmia, New York Heart Association class, physical exercise and use of other complementary therapies in the previous month were treated as categorical variables. Spearman’s rho was estimated to evaluate correlations between mindfulness scores and continuous variables. Mean baseline mindfulness scores were compared across categories of non-continuous variables using T test; Kruskal-Wallis was used when the assumption of constant variance was not met. The association between mindfulness scores and the different variables was estimated in univariate linear regression models. Variables associated with the mindfulness scores with p≤0.10 were then included in a multivariate linear regression model. Results are presented as beta coefficient (with confidence intervals). P values <0.05 were considered significant. All statistical analyses were performed using STATA 10 statistical software (StataCorp, LP; College Station, TX, 2007).
Results
Baseline data from 30 patients were available for this analysis. The baseline demographic and clinical characteristics of the study sample are presented in Table 1. The average age at enrollment was 63.1 years (range: 46–78). Study participants were mostly males (70%), white-non Hispanic (90.0%) and married or in a committed relationship (70%). Sixty percent had less than a college degree and 30% reported that it was somewhat hard to very hard to provide for basics such as heating, food or health insurance. The most common diagnosis was coronary heart disease; cardiac function was usually compromised with a mean ejection fraction of 0.31 (normal: >0.50); 80% of participants were in functional class II or III. Twenty-three percent of patients had experienced a previous severe arrhythmia or cardiac arrest, and 20% had experienced a recent ICD shock. Twenty-three percent were currently receiving anxiolytics and 26.7 % were on anti-depressants, while 20% and 26.7% had a prior history of anxiety and depression, respectively. Four patients (13.3%) reported to have used other integrative/alternative treatments such as expressive writing (2), reflexology (1), or meditation (1) during the previous month. The mean mindfulness score was 57.3 (SD 8.2, range: 38–75).
Table 1.
Baseline characteristics of the study sample
| N (%) or mean (SD)* | |
|---|---|
| Total sample | 30 (100) |
| Age (mean, SD) | 63.1 (10.3) |
| Males | 21(70) |
| Females | 9 (30) |
| White-non Hispanic | 27 (90.0) |
| High School | 7 (23.3) |
| Some college | 11 (36.7) |
| College graduate | 4 (13.3) |
| Post graduate | 8 (26.7) |
| Married or in committed relationship | 21 (70.0) |
| Separated/divorced/single | 9 (30.0) |
| Not at all hard to pay for basics† | 21 (70.0) |
| Somewhat hard | 4 (13.3) |
| Very hard | 5 (16.7) |
| Coronary heart disease | 16 (53.3) |
| Idiopathic dilated cardiomyopathy | 6 (20.0) |
| Other | 8 (26.7) |
| Previous cardiac arrest or severe cardiac arrhythmia | 7 (23.3) |
| Previous ICD shocks/storms | 6 (20.0) |
| Months from ICD procedure median (25th–75th percentile) | 1.43 (0.3, 14.2) |
| Bi-ventricular ICD | 21 (70) |
| Ejection fraction (mean, SD) | 0.31 (0.1) |
| New York Heart Association class | |
| I | 7 (23.3) |
| II | 16 (53.4) |
| III | 7 (23.3) |
| Beta-blockers | 26 (86.7) |
| Anti-arrhythmics | 6 (20.0) |
| Anxiolytics | 7 (23.3) |
| Anti-depressants | 8 (26.7) |
| Exercise at least 30’ once a week during past month | 6 (20) |
| Used integrative medicine treatments‡ during previous month | 4 (13.3) |
| FFM§ scores (mean, SD) | 57.3 (8.2) |
| History of anxiety | 6 (20.0) |
| History of depression | 8(26.7) |
Values are n (%) unless otherwise indicated
Food, housing, medical care and heating
Expressive writing, reflexology, or meditation (non-mindfulness)
FFM= Five Facets of Mindfulness
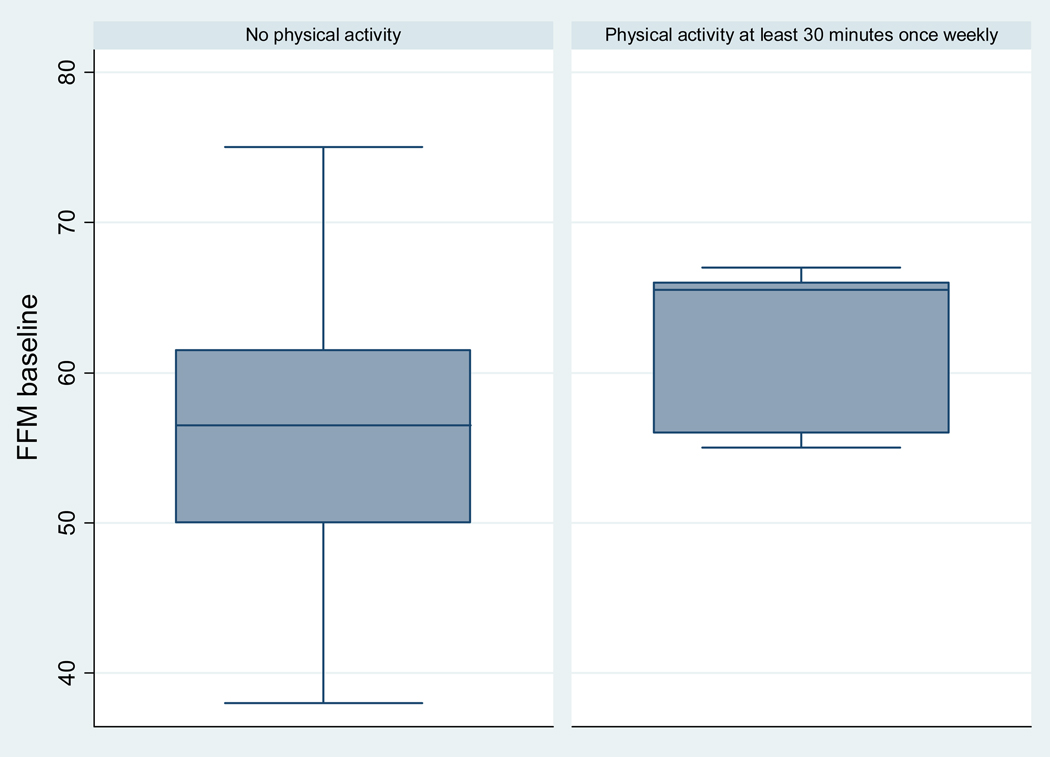
Table 2 shows the mean baseline mindfulness scores by different clinical characteristics. Scores did not differ by demographic characteristics, prior shocks or history of cardiac arrest, and cardiac diagnosis. Mindfulness scores were higher in patients with a bi-ventricular ICD (p=0.057). Likewise, mindfulness scores were higher in patients with no history of depression (p=0.016) or anxiety, as well as in patients not taking antidepressants or anxiolytics. Finally, patients reporting to exercise at least for 30 minutes once a week during the previous month had higher mindfulness scores vs. those not exercising (Figure 1). Mindfulness scores were significantly and inversely correlated with baseline anxiety (Spearman rho: − 0.57, p=0.0005) and depression scores (Spearman rho: −0.37, p=0.04), while there was no association with age (Spearman rho: 0.09, p=0.61), ejection fraction (Spearman rho: −0.06, p=0.73) and time since ICD procedure (Spearman rho: 0.13, p=0.50).
Table 2.
Mean values of FFM scores by baseline characteristic
| Variables | FFM score | P value* | |
|---|---|---|---|
| Sex | Male | 58.2 (6.7) | 0.365 |
| Female | 55.2 (10.7) | ||
| Education | High School | 56.4 (6.9) | 0.920† |
| Some college | 57.1 (8.5) | ||
| College graduate | 60.0 (10.9) | ||
| Post graduate | 57.1 (8.9) | ||
| Marital status | Married or in committed relationship | 57.6 (7.9) | 0.776 |
| Separated/divorced/single | 56.6 (9.4) | ||
| Financial status | Not at all hard to pay for basics‡ | 57.1 (8.7) | 0.837† |
| Somewhat hard | 59.5 (7.0) | ||
| Very hard | 56.2 (8.4) | ||
| Diagnosis | Coronary heart disease | 59.3 (6.55) | 0.390† |
| Idiopathic dilated cardiomyopathy | 55.8 (11.0) | ||
| Other | 54.6 (9.1) | ||
| Previous cardiac arrest | yes | 58.0 (10.5) | 0.810 |
| no | 57.1 (7.7) | ||
| Previous shocks | yes | 58.6 (7.7) | 0.664 |
| no | 57.0 (8.5) | ||
| Type of ICD | Bi-ventricular | 59.2 (7.1) | 0.057 |
| Single chamber | 53.0 (9.4) | ||
| NYHA class | I | 53.6 (9.4) | 0.360† |
| II | 58.0 (7.0) | ||
| III | 59.6 (9.6) | ||
| History of depression | Yes | 51.5 (8.3) | 0.016 |
| No | 59.5 (7.2) | ||
| History of anxiety | Yes | 52.8 (10.5) | 0.136 |
| no | 58.5 (7.4) | ||
| Antidepressants | yes | 54.3 (10.2) | 0.221 |
| no | 58.5 (7.3) | ||
| Anxiolytics | yes | 53.9 (7.9) | 0.206 |
| no | 58.4 (8.2) | ||
| Exercise at least 30’ once a week during past month | yes | 62.5 (5.5) | 0.084 |
| no | 56.0 (8.3) | ||
| Used integrative medicine treatments during previous month | yes | 53.5 (6.8) | 0.338 |
| no | 57.9 (8.5) |
Values are means (SD)
T-test unless otherwise indicated
ANOVA (analysis of variance)
Food, housing, medical care and heating
Figure 1.
Mean mindfulness scores by physical activity condition (at least 30 minutes once a week)
FFM= Five Facets of Mindfulness score
Consistent with the above results, in univariate linear regression models (Table 3), baseline mindfulness scores were significantly and inversely associated with baseline anxiety scores (p=0.001), with a previous diagnosis of depression (p=0.016); and positively associated with type of ICD implanted (bi-ventricular vs. single chamber, p=0.057). Baseline mindfulness scores were not associated with age, gender, race/ethnicity, marital status, education, financial status, smoking, EF, previous cardiovascular procedures, previous cardiac arrest or severe arrhythmia, cardiac diagnosis, time from ICD procedure, previous ICD shocks, current use of anti-arrhythmics or beta-blockers, and use of other complementary/alternative therapies during the past month. There was a positive, non-significant, association between mindfulness scores and exercise, and New York Heart Association class, and an inverse relationship between mindfulness scores and history of anxiety and baseline depression scores.
Table 3.
Univariate and multivariate associations with FFM scores
| Unadjusted Coefficient (95% CI) |
P value | Adjusted Coefficient (95% CI) |
P value | |
|---|---|---|---|---|
| Covariate | ||||
| Baseline HADS anxiety scores | − 1.10 (−1.71, −0.49) | 0.001 | − 0.77 (−1.55, 0.02) | 0.054 |
| Previous depression (yes vs. no) | − 7.95 (−14.31, −1.6) | 0.016 | − 3.14 (−10.21, 3.93) | 0.369 |
| Bi-ventricular vs. single chamber ICD | 6.19 (−0.19, 12.57) | 0.057 | 4.03 (−1.87, 9.92) | 0.172 |
| Exercise* 30 minutes once a week (yes vs. no) | 5.51 (−1.22, 12.24) | 0.10 | 1.96 (−5.08, 9.0) | 0.571 |
F (4, 25) = 4.44; Prob > F = 0.0076 ; R-squared = 0.4152 (multivariate model)
Walking or golfing
FFM= Five Facets of Mindfulness; HADS=Hospital Anxiety and Depression Scale; ICD=implantable cardioverter defibrillator
Next, a multivariate model was generated including all the variables that were associated with the outcome with p≤0.10 in univariate models (Table 3). Psychological variables were highly correlated and in order to avoid collinearity, only covariates showing the strongest associations with the outcome in univariate models were included. In the multivariate model, no variable appeared to be independently statistically significantly associated with mindfulness scores (p=0.054 for the association between anxiety and mindfulness scores).
Discussion
In this group of patients with severe cardiovascular disease and depressed heart function who underwent ICD implantation or received recent shocks, dispositional mindfulness was inversely associated with a previous diagnosis of depression and current anxiety symptoms. Associations with other psychological variables (i.e. use of antidepressants and anxiolytics, previous anxiety, current depression scores), although not reaching statistical significance, were in the expected direction, i.e. they were inversely associated with dispositional mindfulness, supporting the hypothesis of an inverse association between dispositional mindfulness and negative mind states, in agreement with other studies. 13, 17, 20–22 Dispositional mindfulness was inversely associated with not only self-reported current anxiety and depression scores, that could be dependent on current circumstances such as the ICD procedure and the recent hospitalization, but also with a prior diagnosis of anxiety and depression.
In univariate models, patients with more severe cardiovascular symptoms tended to show higher dispositional mindfulness, as indicated by the increased mindfulness scores in patients with higher functional class and in those receiving a biventricular ICD. Biventricular ICDs are usually implanted in patients with more severe heart failure symptoms (i.e. patients having an ejection fraction less than or equal to 35%, a QRS duration greater than or equal to 0.12 seconds, sinus rhythm and New York Heart Association functional class III or IV).29–31 Two hypotheses can be made to explain this finding. First, since ICD patients are usually educated by their providers to pay attention to physical symptoms (such as chest pain, palpitations or shortness of breath) that may signal a worsening of their conditions, they may learn to be more conscious of physical sensations and, in general, to pay more attention to what unfolds in the present. Alternatively, patients may have become more aware of the value of their lives and learned to appreciate the present similarly to what was reported in a study of cancer patients. Higher psychological and interpersonal growth has been reported in survivors of stem cells-transplantation compared to healthy volunteers.32
Dispositional mindfulness was not associated with a history of previous shocks and cardiac arrest; namely, in this group of patients exposure to conditions close to a “near-death” experience did not result in an increased attitude to be mindful in everyday life. However, the study was not powered to detect this association and the number of patients with a history of shocks (6/30) or who received an ICD following a cardiac arrest (7/30) was low.
Finally, one interesting preliminary finding is worth mentioning. Mindfulness scores were higher in patients who exercised at least once a week compared to patients who did not (62.5, SD 5.5 vs. 56.0, SD 8.3, p=0.08; Figure 1). Physical exercise in the form of light yoga exercises is a component of the Mindfulness Based Stress Reduction (MBSR) program,6, 33 the most popular and world renowned mindfulness-based intervention. Self reported yoga practice has been associated with positive changes in mindfulness during MBSR training.34 If physical activity is positively associated with mindfulness levels, it might contribute to the increase in mindfulness observed at the end of such training, which in turn may mediate its beneficial effects on psychological and physical well-being.15, 35, 36 An alternative explanation is that these patients may have paid close attention (been mindful) to their bodily sensations while they were exercising because of the underlying heart conditions. However, this association was of borderline statistical significance, and it deserves further investigation in larger populations.
The most notable strength of this preliminary study is that this is the first study describing the characteristics of dispositional mindfulness in patients with severe cardiovascular disease. Second, the study sample was selected from a “real life” diverse population of consecutive candidates to ICD procedures and/or with ICD shocks, thus very different from the highly educated, high socio-economic status, and mostly female population usually accessing mind-body programs.37 However, there are also several limitations. First, because of the small sample size, this study was not powered to detect associations with less frequent events such as previous cardiac arrest or shocks, and to examine associations with the specific facets of mindfulness measured by the Five Facets of Mindfulness questionnaire. Second, we studied a highly selected population and the study findings cannot be generalized to patients with other diseases. Third, although the study was proposed to all consecutive ICD candidates, it cannot be excluded that only highly motivated participants joined the study and that due to social desirability or other factors they may be more prone to report higher or different levels of mindfulness compared to patients that did not participate. Fourth, dispositional mindfulness was self-reported. This is a common limitation of studies assessing the effect of mindfulness training. In fact, despite recent evidence that mindfulness is an important mediator of the effect of mindfulness interventions on anxiety and other psychological outcomes, 15, 35, 36 adequate definitions of mindfulness are often not provided, and when provided, they are either inconsistent or overlapping across studies.38 Objective criteria for the measurement of mindfulness are currently unavailable and although several self-report instruments were developed to measure this construct,13, 19, 20, 39, 40 correlations across different scales are modest,41 further complicating the comparison of results across studies. It is likely that the meaning of some items in mindfulness inventories (including the one used for this study) may have a quite different meaning in mindfulness-trained subjects and in patients such as the ones enrolled in this study, who were never exposed to mindfulness training.38
Finally, since this was a cross-sectional analysis, the direction of the association could not be established, i.e. whether enhanced dispositional mindfulness leads to an improved emotional well-being or if the mind’s absorption in the powerful struggles and emotions accompanying anxiety and depression is limiting its natural capacity of attending to the present.
In conclusion, current psychological well-being and prior psychological morbidity, and not indicators of disease severity such as prior cardiac arrest or shocks, appear to be more strongly associated with dispositional mindfulness in patients with ICDs who did not receive previous mindfulness training. Further research in larger populations is needed to confirm these finding, which may help shed further light on the mechanism of the beneficial effects of mindfulness training on health outcomes.
Acknowledgements
This study was partially supported by a grant of the National Center of Complementary and Alternative Medicine (F32AT005048).
We want to thank Mary Stanley, MS, NP and Karen Rose, MS, NP for their help with recruitment.
Footnotes
Authors’ contributions
Elena Salmoirago-Blotcher designed the study, collected the data, conducted the data analysis and wrote the manuscript draft; Sybil Crawford provided statistical advice and revised the manuscript; James Carmody contributed to the study design, the interpretation of the data and revised the manuscript; Ira Ockene and Lawrence Rosenthal contributed to the study conception and revised the manuscript. All authors approved the final version of the manuscript for publication.
Conflicting interests: none reported
Ethical approval: The study protocol and all study materials were approved by the Committee for the Protection of Human Subjects at the University of Massachusetts Medical School (Docket H-13078).
REFERENCES
- 1.Grossman P, Niemann L, Schmidt S, Walach H. Mindfulness-based stress reduction and health benefits: A meta-analysis. J Psychosom Res. 2004;57(1):35–43. doi: 10.1016/S0022-3999(03)00573-7. [DOI] [PubMed] [Google Scholar]
- 2.Speca M, Carlson LE, Goodey E, Angen M. A Randomized, wait-list controlled clinical trial: the effect of a mindfulness meditation-based stress reduction program on mood and symptoms of stress in cancer outpatients. Psychosom Med. 2000;62(5):613–622. doi: 10.1097/00006842-200009000-00004. [DOI] [PubMed] [Google Scholar]
- 3.Carlson LE, Garland SN. Impact of Mindfulness-Based Stress Reduction (MBSR) on sleep, mood, stress and fatigue symptoms in cancer outpatients. Int J Behav Med. 2005;12(4):278–285. doi: 10.1207/s15327558ijbm1204_9. [DOI] [PubMed] [Google Scholar]
- 4.Carlson LE, Speca M, Faris P, Patel KD. One year pre-post intervention follow-up of psychological, immune, endocrine and blood pressure outcomes of mindfulness-based stress reduction (MBSR) in breast and prostate cancer outpatients. Brain Behav Immun. 2007;21(8):1038–1049. doi: 10.1016/j.bbi.2007.04.002. [DOI] [PubMed] [Google Scholar]
- 5.Saxe GA, Hebert JR, Carmody JF, et al. Can diet in conjunction with stress reduction affect the rate of increase in prostate specific antigen after biochemical recurrence of prostate cancer? J Urol. 2001;166(6):2202–2207. [PubMed] [Google Scholar]
- 6.Kabat-Zinn J. An outpatient program in behavioral medicine for chronic pain patients based on the practice of mindfulness meditation: theoretical considerations and preliminary results. Gen Hosp Psychiatry. 1982;4(1):33–47. doi: 10.1016/0163-8343(82)90026-3. [DOI] [PubMed] [Google Scholar]
- 7.Plews-Ogan M, Owens JE, Goodman M, et al. Brief report: A pilot study evaluating Mindfulness-Based Stress Reduction and massage for the management of chronic pain. J Gen Intern Med. 2005;20(12):1136–1138. doi: 10.1111/j.1525-1497.2005.0247.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kabat-Zinn J, Massion AO, Kristeller J, et al. Effectiveness of a meditation-based stress reduction program in the treatment of anxiety disorders. Am J Psychiatry. 1992;149(7):936–943. doi: 10.1176/ajp.149.7.936. [DOI] [PubMed] [Google Scholar]
- 9.Pradhan E, Baumgarten M, Langenberg P, et al. Effect of Mindfulness-Based Stress Reduction in rheumatoid arthritis patients. Arthritis Rheum. 2007;57(7):1134–1142. doi: 10.1002/art.23010. [DOI] [PubMed] [Google Scholar]
- 10.Sephton S, Salmon P, Weissbecker I, et al. Mindfulness meditation alleviates depressive symptoms in women with fibromyalgia: Results of a randomized clinical trial. Arthritis Rheum. 2007;57(1):77–85. doi: 10.1002/art.22478. [DOI] [PubMed] [Google Scholar]
- 11.Bohlmeijer E, Prenger R, Taal E, Cuijpers P. The effects of Mindfulness-Based Stress Reduction therapy on mental health of adults with a chronic medical disease: a meta-analysis. J Psychosom Res. 2010;68(6):539–544. doi: 10.1016/j.jpsychores.2009.10.005. [DOI] [PubMed] [Google Scholar]
- 12.Teasdale JD, Segal ZV, Williams JMG et al. Prevention of relapse/recurrence in major depression by mindfulness-based cognitive therapy. J Consult Clin Psychol. 2000;68(4):615–623. doi: 10.1037//0022-006x.68.4.615. [DOI] [PubMed] [Google Scholar]
- 13.Brown KW, Ryan RM. The benefits of being present: mindfulness and its role in psychological well-being. J Pers Soc Psychol. 2003;84(4):822–848. doi: 10.1037/0022-3514.84.4.822. [DOI] [PubMed] [Google Scholar]
- 14.Kabat-Zinn J. Mindfulness-based interventions in context: past, present, and future. Clinical Psychology: Science and Practice. 2003;10(2):144–156. [Google Scholar]
- 15.Carmody J, Baer R. Relationships between mindfulness practice and levels of mindfulness, medical and psychological symptoms and well-being in a mindfulness-based stress reduction program. J Behav Med. 2008;31(1):23–33. doi: 10.1007/s10865-007-9130-7. [DOI] [PubMed] [Google Scholar]
- 16.Thompson BL, Waltz J. Everyday mindfulness and mindfulness meditation: Overlapping constructs or not? Personality and Individual Differences. 2007;43(7):1875–1885. [Google Scholar]
- 17.Carlson LE, Brown KW. Validation of the Mindful Attention Awareness Scale in a cancer population. J Psychosom Res. 2005;58(1):29–33. doi: 10.1016/j.jpsychores.2004.04.366. [DOI] [PubMed] [Google Scholar]
- 18.Heppner WL, Kernis MH, Lakey CE, et al. Mindfulness as a means of reducing aggressive behavior: dispositional and situational evidence. Aggress Behav. 2008;34(5):486–496. doi: 10.1002/ab.20258. [DOI] [PubMed] [Google Scholar]
- 19.Baer RA, Smith GT, Hopkins J, et al. Using self-report assessment methods to explore facets of mindfulness. Assessment. 2006;13(1):27–45. doi: 10.1177/1073191105283504. [DOI] [PubMed] [Google Scholar]
- 20.Baer RA, Smith GT, Allen KB. Assessment of mindfulness by self-report: the Kentucky inventory of mindfulness skills. Assessment. 2004;11(3):191–206. doi: 10.1177/1073191104268029. [DOI] [PubMed] [Google Scholar]
- 21.Branstrom R, Duncan LG, Moskowitz JT. The association between dispositional mindfulness, psychological well-being, and perceived health in a Swedish population-based sample. [Published online ahead of print: April 26 2010] Br J Health Psychol. 2010 doi: 10.1348/135910710X501683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Baer RA, Smith GT, Lykins E, et al. Construct validity of the Five Facet Mindfulness Questionnaire in meditating and non-meditating samples. Assessment. 2008;15(3):329–342. doi: 10.1177/1073191107313003. [DOI] [PubMed] [Google Scholar]
- 23.Shapiro SL, Brown KW, Thoresen C, Plante TG. The moderation of Mindfulness-Based Stress Reduction effects by trait mindfulness: Results from a randomized controlled trial. J Clin Psychol. 2011;67(3):267–277. doi: 10.1002/jclp.20761. [DOI] [PubMed] [Google Scholar]
- 24.Zigmond A, Snaith R. The Hospital Anxiety and Depression Scale. Acta Psychiatr Scand. 1983;67(6):361–370. doi: 10.1111/j.1600-0447.1983.tb09716.x. [DOI] [PubMed] [Google Scholar]
- 25.Snaith RP. The Hospital Anxiety and Depression Scale. Health Qual Life Outcomes. 2003;1(1):29. doi: 10.1186/1477-7525-1-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bjelland I, Dahl AA, Haug TT, Neckelmann D. The validity of the Hospital Anxiety and Depression Scale: An updated literature review. J Psychosom Res. 2002;52(2):69–77. doi: 10.1016/s0022-3999(01)00296-3. [DOI] [PubMed] [Google Scholar]
- 27.Herrmann C. International experiences with the Hospital Anxiety and Depression Scale--a review of validation data and clinical results. J Psychosom Res. 1997;42(1):17–41. doi: 10.1016/s0022-3999(96)00216-4. [DOI] [PubMed] [Google Scholar]
- 28.Spinhoven P, Ormel J, Sloekers PP, et al. A validation study of the Hospital Anxiety and Depression Scale (HADS) in different groups of Dutch subjects. Psychol Med. 1997;27(2):363–370. doi: 10.1017/s0033291796004382. [DOI] [PubMed] [Google Scholar]
- 29.Epstein AE, DiMarco JP, Ellenbogen KA, et al. ACC/AHA/HRS 2008 guidelines for device-based therapy of cardiac rhythm abnormalities: A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the ACC/AHA/NASPE 2002 Guideline Update for Implantation of Cardiac Pacemakers and Antiarrhythmia Devices) developed in collaboration with the American Association for Thoracic Surgery and Society of Thoracic Surgeons. J Am Coll Cardiol. 2008;51(21):e1–e62. doi: 10.1016/j.jacc.2008.02.032. [DOI] [PubMed] [Google Scholar]
- 30.Abraham WT, Fisher WG, Smith AL, et al. Cardiac resynchronization in chronic heart failure. N Engl J Med. 2002;346(24):1845–1853. doi: 10.1056/NEJMoa013168. [DOI] [PubMed] [Google Scholar]
- 31.Cleland JG, Daubert JC, Erdmann E, et al. The effect of cardiac resynchronization on morbidity and mortality in heart failure. N Engl J Med. 2005;352(15):1539–1549. doi: 10.1056/NEJMoa050496. [DOI] [PubMed] [Google Scholar]
- 32.Andrykowski MA, Bishop MM, Hahn EA, et al. Long-term health-related quality of life, growth, and spiritual well-being after hematopoietic stem-cell transplantation. J Clin Oncol. 2005;23(3):599–608. doi: 10.1200/JCO.2005.03.189. [DOI] [PubMed] [Google Scholar]
- 33.Kabat-Zinn J. Full catastrophe living: using the wisdom of your body and mind to face stress, pain, and illness. New York: Dell Publishing; 1990. [Google Scholar]
- 34.Carmody J, Baer RA. Relationships between mindfulness practice and levels of mindfulness, medical and psychological symptoms and well-being in a mindfulness-based stress reduction program. J Behav Med. 2008;31(1):23–33. doi: 10.1007/s10865-007-9130-7. [DOI] [PubMed] [Google Scholar]
- 35.Nyklícek I, Kuijpers K. Effects of Mindfulness-Based Stress Reduction intervention on psychological well-being and quality of life: is increased mindfulness indeed the mechanism? Ann Behav Med. 2008;35(3):331–340. doi: 10.1007/s12160-008-9030-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Branstrom R, Kvillemo P, Brandberg Y, Moskowitz JT. Self-report mindfulness as a mediator of psychological well-being in a stress reduction intervention for cancer patients-a randomized study. Ann Behav Med. 2010;39(2):151–161. doi: 10.1007/s12160-010-9168-6. [DOI] [PubMed] [Google Scholar]
- 37.Yeh GY, Davis RB, Phillips RS. Use of complementary therapies in patients with cardiovascular disease. Am J Cardiol. 2006;98(5):673–680. doi: 10.1016/j.amjcard.2006.03.051. [DOI] [PubMed] [Google Scholar]
- 38.Grossman P. On measuring mindfulness in psychosomatic and psychological research. J Psychosom Res. 2008;64(4):405–408. doi: 10.1016/j.jpsychores.2008.02.001. [DOI] [PubMed] [Google Scholar]
- 39.Lau M, Bishop SR, Segal ZV, et al. The Toronto Mindfulness Scale: Development and validation. J Clin Psychol. 62(12):1445–1467. doi: 10.1002/jclp.20326. [DOI] [PubMed] [Google Scholar]
- 40.Walach H, Buchheld N, Buttenmüller V, et al. Measuring mindfulness--the Freiburg Mindfulness Inventory (FMI) Personality and Individual Differences. 2006;40(8):1543–1555. [Google Scholar]
- 41.Carmody J, Reed G, Kristeller J, Merriam P. Mindfulness, spirituality, and health-related symptoms. J Psychosom Res. 2008;64(4):393–403. doi: 10.1016/j.jpsychores.2007.06.015. [DOI] [PubMed] [Google Scholar]