Abstract
Diagnosis of the etiologic agent of respiratory viral infection relies traditionally on culture or antigen detection. This pilot evaluation compared performance characteristics of the RT-PCR and electrospray ionization mass spectrometry (RT-PCR/ESI-MS) platform to conventional virologic methods for identifying multiple clinically relevant respiratory viruses in nasopharyngeal aspirates. The RT-PCR/ESI-MS respiratory virus surveillance kit was designed to detect respiratory syncytial virus, influenza A and B, parainfluenza types 1–4, adenoviridae types A–F, coronaviridae, human bocavirus, and human metapneumovirus. Patients (N = 192) attending an emergency department during the 2007–2008 respiratory season consented, and “excess” frozen archived nasopharyngeal aspirates were analysed; 46 were positive by conventional virology and 69 by RT-PCR/ESI-MS, among which there were six samples with multiple viral pathogens detected. The sensitivity and specificity of the assay were 89.1% and 80.3%, respectively. Additional viruses that were not identified by conventional virology assays were detected (4 human bocaviruses and 7 coronaviruses). Samples in which the RT-PCR/ESI-MS results disagreed with conventional virology were sent for analysis by a third method using a commercial RT-PCR-based assay, which can identify viruses not detectable by conventional virologic procedures. Time to first result of RT-PCR/ESI-MS was 8 h. RT-PCR/ESI-MS demonstrated capacity to detect respiratory viruses identifiable and unidentifiable by conventional methods rapidly.
Abbreviations: RT-PCR/ESI-MS, reverse transcription PCR and electrospray ionization mass spectrometry; SARS, severe acute respiratory syndrome
Keywords: Electrospray ionization mass spectrometry, Respiratory tract infections, Virus, Diagnosis, Surveillance
1. Introduction
Accurate and timely diagnosis of acute viral respiratory tract infections (RTIs), which is important for individual patients management decisions, as well as appropriate infection control, remains challenging both for clinicians and laboratorians (Mahony, 2008). Many clinical virology laboratories still rely on labour intensive or time-consuming diagnostic algorithms which incorporate antigen or culture-based methods (Mahony, 2008).
Molecular diagnostic assays hold great potential to impact infectious disease diagnosis and clinical management, particularly for viral infections, where conventional methods (i.e. antigen and culture based methods) do not provide timely or highly accurate results (Ratcliff et al., 2007). While many rapid nucleic acid amplification tests have been developed to identify individual virus (Liolios et al., 2001), the utility of molecular diagnostics in clinical settings may best be realized by single system diagnostic platforms that can simultaneously detect multiple pathogens (Liao et al., 2009, Pabbaraju et al., 2008, Raymond et al., 2009, Wu and Tang, 2009).
Electrospray ionization mass spectrometry following broad-range reverse transcription-PCR (RT-PCR/ESI-MS), one of the single system diagnostic platforms, that has the potential to not only detect rapidly but also identify and quantify multiple pathogens simultaneously. To date, studies with RT-PCR/EMI-MS have been restricted to the detection of individual respiratory bacteria or viruses [i.e. streptococcus (Ecker et al., 2005), coronavirus (SARS) (Sampath et al., 2005), adenovirus (Russell et al., 2006), and influenza viruses (Sampath et al., 2007)], or detailed characterization [e.g. resistance gene recognition (Ecker et al., 2006), genotyping of the organism (Ecker et al., 2005)]. The capacity of RT-PCR/EMI-MS for broad range, simultaneous and multiple pathogen detection with rapid turnaround may translate into a useful tool for clinicians in health care settings to aid in early diagnosis of respiratory tract infections.
This hospital-based pilot study was conducted over one season of respiratory infections to compare the performance characteristics of this RT-PCR/ESI-MS platform versus conventional virologic procedures, for identification of multiple clinically relevant respiratory viruses in nasopharyngeal aspirate samples collected from emergency department patients presenting with acute respiratory illnesses.
2. Materials and methods
2.1. Study setting and population
Patients visiting the adult or paediatric emergency departments at a tertiary care inner-city hospital, between December 1, 2007 and May 31, 2008 were assessed for eligibility. All eligible patients, operationally defined as any patients with a suspected acute upper respiratory tract infection, in whom the emergency physicians ordered nasopharyngeal aspirate testing, were approached consecutively and recruited. Eligible patients were identified by dedicated study coordinators by the daily review of nasopharyngeal aspirate testing order lists from the emergency department, and sought informed consent (in person, for those who were still in the hospital, or by telephone, for those who were already discharged either from the emergency department or the inpatient setting). There were at least three separate attempts in different periods of different days to attempt contact and informed consent for potentially eligible subjects, which resulted in 30% participation rate. Clinical information was obtained by chart review to derive patient demographic variables, hospitalization related to the respiratory tract infection episode, and length of stay in the hospital in days if admitted. Samples were maintained by the clinical virology laboratory frozen at −80 °C, after standard virologic procedures were completed as part of their standard laboratory protocol. This study was approved by the Johns Hopkins University Institutional Review Board.
2.2. Reference standardized diagnostic tests in clinical virology laboratory
Nasopharyngeal aspirate tests (i.e. rapid immunochromatographic testing [Binax Now, Inverness, Bedford, UK] for influenza viruses and RSV during the respiratory season, direct fluorescent antibody testing [D3 ultra DFA respiratory virus ID kit, Diagnostic HYBRIDS, Athens, OH] and shell vial culture identification [R-mix too, Diagnostic HYBRIDS, Athens, OH] for adenovirus, influenza viruses, parainfluenza viruses and RSV, tube culture for adenovirus, influenza viruses, parainfluenza viruses, human MPV and RSV, HSV, CMV and enterovirus, and hemadsorption inhibition testing) were processed according to a standardized algorithm (Fig. 1 ) at this clinical virology laboratory for virologic identification. Routine PCR testing was not performed in the clinical virology laboratory.
Fig. 1.

Algorithm of clinical reference diagnostic test in clinical virology laboratory for respiratory samples. Diagnostic algorithm used in clinical virology laboratory to detect respiratory viruses mainly divided into respiratory season or non-respiratory season. Respiratory season defined as October to the following January (October to November for RSV, December to January for influenza). Immunochromatographic assays were used in respiratory season as the sole screening test for RSV and influenza, which will stop the testing algorithm if results are positive. Respiratory panel cocktail DFA tests serve for adenovirus, influenza A and B, parainfluenza types 1–3 and RSV, which will stop the testing algorithm if results are positive in non-respiratory season or for those screened negative by immunochromatographic assays in respiratory season as well. RSV, respiratory syncytial virus; PIV, parainfluenza virus; HSV, herpes simplex virus; CMV, cytomegalovirus; hMPV, human metapneumovirus; DFA, direct fluorescent antibody test; CPE, cytopathic effect; RBC, red blood cells.
2.3. Sample processing for RT-PCR/ESI-MS
Samples were processed for total nucleic acid extraction using the Thermo King-Fisher (Waltham, MA) robot according to an Ambion (ABI, Foster City, CA) MagMAX viral kit extraction protocol.
2.4. Reverse transcription PCR (RT-PCR)
All PCR wells are amplified under a one-step RT-PCR cycle protocol. This protocol was developed to support both RT-PCR and conventional PCR equally for primer pairs used. RT-PCR was performed in a 50 μL reaction mix consisting of 4 U of AmpliTaq Gold (Applied Biosystems, Foster City, CA); 20 mM Tris, pH 8.3; 75 mM KCl; 1.5 mM MgCl2; 0.4 M betaine; 800 mM mix of dATP, dGTP, dCTP, and dTTP (Bioline USA, Inc., Randolph, MA); 10 mM dithiothreitol; 100 ng sonicated polyA DNA (Sigma Corp., St. Louis, MO); 40 ng random hexamers (Invitrogen Corp., Carlsbad, CA); 1.2 U Superasin (Ambion Corp., Austin, TX); 400 ng T4-gene-32 protein (Roche Diagnostics Corp., Indianapolis, IN); 2 U Superscript III (Invitrogen Corp., Carlsbad, CA); 20 mM sorbitol (Sigma Corp.); and 250 nM of each primer. The following RT-PCR cycling conditions were used: 60 °C for 5 min, 4 °C for 10 min, 55 °C for 45 min, 95 °C for 10 min, followed by 8 cycles of 95 °C for 30 s, 48 °C for 30 s, and 72 °C for 30 s, with the 48 °C annealing temperature increasing 0.9 °C each cycle for reverse transcription. The PCR was then continued for 37 additional cycles of 95 °C for 15 s, 56 °C for 20 s, and 72 °C for 20 s. The RT-PCR cycle ended with a final extension of 2 min at 72 °C followed by a 4 °C hold.
2.5. Respiratory virus surveillance panel
The assay was performed using the Ibis T5000 respiratory virus surveillance II kit (Ibis Biosciences, Inc., Carlsbad, CA), which is designed to detect and subtype viruses from seven groups of “conventional viruses” (respiratory syncytial virus (RSV), influenza A and B, parainfluenza types 1–4, adenoviridae types A–F) and viruses that are not identifiable conventionally (coronaviridae, human bocavirus, and human metapneumovirus).
2.6. Mass spectrometry for base composition analysis and quantitation
RT-PCR products were analysed using the Ibis T5000 universal biosensor platform (Ibis Biosciences, Inc., Carlsbad, CA), which performs automated post-PCR desalting, ESI-MS signal acquisition, spectral analysis, and data reporting as described previously (Sampath et al., 2005). Briefly, steps were as follows: each PCR was desalted and purified using a weak anion exchange protocol as described elsewhere (Jiang and Hofstadler, 2003). Accurate mass (61 ppm), high-resolution (M/dM 100,000 FWHM) mass spectra were acquired for each sample using high-throughput ESI-MS protocols (Sampath et al., 2007). For each sample, approximately 1.5 μL of analyte solution was consumed during the 74-s spectral acquisition. Raw mass spectra were post-calibrated with an internal mass standard and deconvolved to monoisotopic molecular masses. Unambiguous base compositions were derived from the exact mass measurements of the complementary single-stranded oligonucleotides. The detailed information of the software used to interrogate amplicon mass and viruses identification was described elsewhere (Hofstadler et al., 2005). A calibrant consists of a specially designed nucleic acid sequence that similar to but distinguishable from any potential sequence were amplified in each well as the internal positive control. A negative control was implemented in each batch of processing with sterile viral transport media.
2.7. Evaluation of samples for which conventional virology and RT-PCR/ESI-MS did not agree
The clinical virology laboratory at this institution does not perform PCR tests routinely for all respiratory viruses. Accordingly, those samples for which clinical virology laboratory and RT-PCR/ESI-MS did not agree, and for which sufficient volume (200 μL) was available, were sent to Viracor (Lee's Summit, MO) for identification by another PCR-based platform (Luminex Respiratory Assay, Austin, TX) designed to detect all of viruses that the RT-PCR/ESI-MS could detect, except human bocavirus (Pabbaraju et al., 2008).
2.8. Throughput determination
Sample throughput determination with RT-PCR/ESI-MS included using one King/Fisher extraction robot, one JANUS automated dispensing robot, four Eppendorf thermocyclers simultaneously, and one T5000 clean-up and injection automation system.
2.9. Statistical analysis
For the primary analysis evaluating performance of RT-PCR/ESI-MS, conventional virology laboratory results were used as the reference standard. Fig. 2 describes the number of subjects, each of which had one nasopharyngeal aspirate sample evaluated. Also included in the figure is the number of ‘evaluable results’ operationally defined here for purposes of primary and secondary performance evaluation as the number of individual evaluable results which could be compared to one another, since each nasopharyngeal aspirate sample could yield test results (by culture or RT-PCR/MS-ESI) of ‘negative’, single positive, or multiple viral detections. In the secondary analysis, clinical virology laboratory results and the secondary (i.e. Luminex) PCR-based results were combined as the reference test. Samples containing viruses for which the clinical virology laboratory had no protocol available (i.e. bocavirus and coronavirus detection) were excluded from the primary analysis but included in the secondary analysis if the viral agent could be detected by the other (Luminex) RT-PCR-based method (i.e. all viruses except bocavirus). Confidence intervals for sensitivity, and specificity were based on exact binomial probabilities. Subgroup analysis was performed to detect any difference of performance among paediatric and adult patients.
Fig. 2.
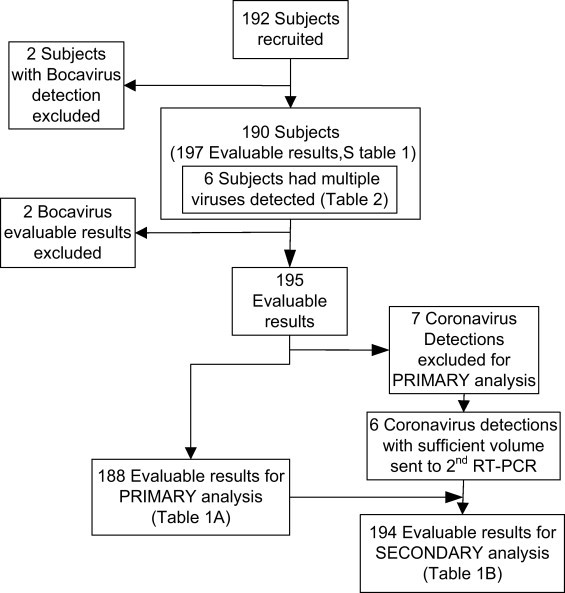
Flow diagram of recruitment and performance analysis process. Bocavirus that were not detectable in both clinical virology laboratory and secondary RT-PCR based platform were excluded (2 subjects with bocavirus only detection and 2 bocavirus detection). After excluding bocavirus and coronavirus detections that clinical virology laboratory had no protocol to detect, 188 were included in the primary performance analysis as in Table 3. Six coronavirus and 31 samples for which clinical virology laboratory and RT-PCR/ESI-MS did not agree with sufficient volume left were sent to secondary RT-PCR based assay for secondary analysis.
3. Results
During December 1, 2007 and June 30, 2008, 650 patients were eligible and 192 (29.5%) were recruited. Among those consented patients, most were younger than 18 years of age (n = 147, 76%), male (n = 95, 52%), African American (n = 95, 52%), and hospitalized (n = 116, 63%) (Supplementary Table 1). The most common reason for patients not participating in this study was inability to reach the subjects (e.g. wrong telephone numbers in registry, inability to connect the telephone call). The median storage time of nasopharyngeal aspirates was 7 months (range 5.5–11).
3.1. Primary analysis: performance of the RT-PCR/ESI-MS versus conventional virology
Of the 192 patients, there were 188 evaluable results for the primary analysis. Among 46 positive detections tested by the clinical virology laboratory, most were found by shell vial culture (n = 21, 46%), followed by immunochromatographic tests (n = 10, 22%), which detected 8 of 28 influenza viruses (28.6%) and 2 of 11 RSV (18.2%) isolated by viral culture. As described above, 4 bocaviruses were excluded (2 specimens with bocavirus only, and 2 bocavirus detections from samples, which had multiple detections), as well as 7 coronavirus only samples in primary analysis. After exclusions, the overall agreement between RT-PCR/ESI-MS with conventional virology was 82.4% (95% C.I.: 76.2–87.6%). Sensitivity and specificity were 89.1% and 80.3% (95% C.I.: 76.4–96.4, 72.7–86.5%, respectively (Table 1A)).
Table 1.
Overall performance of the RT-PCR/ESI-MS platform compared to conventional virology methods only for 190 subjects (A) and to both clinical virology and secondary RT-PCR based methods combined (B, N = 194).
| A | B | ||||
|---|---|---|---|---|---|
| Clinical virology reference tests (N = 188) |
Combineda reference tests (N = 194b) |
||||
| Positive | Negative | Positive | Negative | ||
| RT-PCR/ESI-MS | Positive | 41 | 28c | 62 | 15 |
| RVSII assay | Negative | 5d | 114 | 5 | 112 |
| Total | 46 | 142 | 67 | 127 | |
Raw sensitivity and specificity were 89.1% and 80.3% (95% C.I.: 76.4–96.4, 72.7–86.5%, respectively). Sensitivity and specificity in secondary analysis were 92.5% and 88.2% (95% C.I.: 83.4–97.5%, 81.2–93.2%, respectively). Samples from 190 subjects had one or more detection and sum to 195 total isolations.
Combined reference tests defined as combination of clinical virology reference tests and secondary RT-PCR based method.
Excludes one coronavirus detection with insufficient volume to send to the secondary PCR method.
Excludes seven coronavirus detections that were not confirmable with clinical virology reference tests.
Included one coronavirus detection that was detected by virology reference test as adenovirus.
Sensitivity of RT-PCR/ESI-MS for individual pathogens was as follows: 100% parainfluenza, 92.9% influenza viruses, 81.8% RSV, and 67% adenovirus (Table 2A). RT-PCR/ESI-MS successfully typed pathogens including 40 influenza A, one influenza B, four parainfluenza type 3 and one adenovirus type A, which were 100% matched to the findings of clinical virology, and six adenovirus type C adenovirus for which clinical virology laboratory had no protocol to type. RT-PCR/ESI–MS detected multiple virus detections in 6 samples (Table 3 ).
Table 2.
Performance of the RT-PCR/ESI-MS platform for individual pathogens compared to clinical virology methods only (A) and conventional virology with secondary RT-PCR based methods combined (B).
| Pathogens | A |
N = 188 |
B |
N = 194 |
||||
|---|---|---|---|---|---|---|---|---|
| TP | FP | FN | Raw sensitivity (%) | Raw specificity (%) | 2nd TP | 2nd analysis sensitivity (%) | 2nd analysis specificity (%) | |
| RSV | 9 | 10 | 2 | 81.8 | 94.4 | 15 | 88.2 | 97.7 |
| Parainfluenza | 4 | 0 | 0 | 100 | 100 | 4 | 100 | 100 |
| Influenza | 26 | 15 | 2 | 92.9 | 90.6 | 36 | 94.9 | 96.8 |
| Adenovirus | 2 | 4 | 1a | 67 | 97.8 | 3 | 75 | 98.4 |
| Coronavirusb | NA | NA | NA | NA | NA | 4 | 100 | 98.4 |
TP: true positive, RT-PCR/ESI-MS (+) and clinical virology (+).
FP: false positive, RT-PCR/ESI-MS (+) and clinical virology (−).
FN: false negative, RT-PCR/ESI-MS (−) and clinical virology (+).
2nd TP: secondary analysis true positive, RT-PCR/ESI-MS (+) and clinical virology (+) or secondary RT-PCR based method (+).
NA: not available.
One coronavirus isolation that detected by conventional virology reference test as adenovirus.
Excludes one coronavirus detection with insufficient volume to send to the secondary PCR method.
Table 3.
Findings from 6 subjects whom had multiple viruses detected by RT-PCR/ESI-MS platform.
| Subject ID | RT-PCR/ESI-MS | Clinical virology laboratory | 2nd RT-PCR based method |
|---|---|---|---|
| 895 | Adenovirus C, RSV, bocavirus | Negative | Negativea |
| 982 | Adenovirus, RSV | Negative | RSV |
| 984 | RSV, influenza A | RSV | RSV, influenza A |
| 986 | RSV, influenza A | Negative | RSV, influenza A |
| 1014 | Adenovirus C, coronavirus | Adenovirus | Adenovirus, coronavirus |
| 1027 | Influenza A, bocavirus | Influenza A | Influenza Aa |
RT-PCR/ESI-MS multiply detected nine more viruses in six samples. Among 13 detected viruses, three were also detected in clinical virology laboratory, and another four were confirmed by secondary RT-PCR based method.
Bocavirus was not detectable in secondary RT-PCR based method.
3.2. Secondary analysis: comparison of RT-PCR/ESI-MS with conventional virology and Luminex assay
Total evaluable results were 194 (Fig. 2). There were 33 evaluable results from the primary analysis where findings from the RT-PCR/ESI-MS disagreed with the clinical virology; 31 of these had sufficient volume, and together with 6 coronavirus positive specimens from RT-PCR/ESI-MS (no protocol by clinical virology laboratory) were sent for evaluation by the secondary PCR-based method (Luminex, total 37 samples). Twenty-one of 37 (57%) RT-PCR/ESI-MS results were confirmed by Luminex, including 17 conventional viruses detections (10 influenza A, 6 RSV, 1 adenovirus) and 4 coronavirus detections (not detectable by conventional clinical virology). The overall agreement, sensitivity and specificity, after secondary analysis of available samples were 89.7% (95% C.I.: 84.5–93.6%), 92.4% (95% C.I.: 83.2–97.5%) and 89.0% (95% C.I.: 82.2–93.8%), respectively (Table 1B). The results for individual pathogens shown in Table 2B. Accuracy of RT-PCR/ESI-MS did not differ significantly between adult and paediatric patients.
3.3. Throughput
Time to first result from sample preparation to detection of RT-PCR/ESI-MS was 8 h:1 h of DNA/RNA extraction, 4 h of RT-PCR, and 3 h of processing in ESI-MS. Estimated throughput of RT-PCR/ESI-MS was 300 samples with 2 technicians working 8 h.
4. Discussion
This hospital-based pilot study was designed to describe the preliminary performance of a novel RT-PCR/ESI-MS platform versus the current diagnostic algorithm used in the clinical virology laboratory in clinical specimens. The findings demonstrate that the assay has high throughput and was able to detect simultaneously and type multiple clinically relevant respiratory pathogens in nasopharyngeal aspirates from patients with suspected viral infections with 82.4% accuracy, compared to conventional clinical virology laboratory testing. This study also shows that pathogens not detectable by conventional clinical virology methods could be detected successfully by the RT-PCR/ESI-MS platform.
Advantages of the RT-PCR/ESI-MS platform over conventional testing include rapid turnaround, capacity to detect multiple respiratory pathogens simultaneously with high throughput, and provision of more detailed pathogen characterization (i.e. semi-quantitation, typing, and subtyping of species). The commonly used diagnostic methods in less well-equipped clinical virology laboratories are culture-based, which may take days to yield results, are labour-intensive and costly (Anzueto and Niederman, 2003). Although some rapid antigen tests offer faster detection times for individual pathogen, clinical utility is limited, as the pathogenic agent is usually not known a priori, and these tests have sub-optimal sensitivity and specificity (Ginocchio, 2007). As demonstrated in this study that the rapid antigen tests detected only small proportions of influenza and RSV in clinical specimens, the sub-optimal sensitivity restricts the wider utilization of these rapid tests in clinical settings. Compared to diagnostic algorithms used commonly in hospitals (Fig. 1), the RT-PCR/ESI-MS platform provides a more straightforward approach for identification of clinically relevant respiratory viruses and may serve as a diagnostic adjunct ultimately.
Data demonstrating capacity of RT-PCR/ESI-MS platform to type and subtype, while not shown here, comes from a pilot study by our group in which 26 of 29 novel H1N1 influenza A viruses detections were confirmed by additional state laboratory testing using the Centers for Disease Control and Prevention novel H1N1 influenza A PCR typing method, supporting a role for this platform for surveillance in clinical or public health settings (Gaydos, 2010). Viral load quantitation capacity of the assay, not detailed here, was being performed in a separate pilot study from this group demonstrating that readouts of viral genome copy/well by RT-PCR/ESI-MS correlate positively with the type of detection method employed by clinical virology (Chen et al., 2008).
Methods for evaluating the performance of novel assays, which are potentially more “accurate” than the current reference tests, remain controversial. Some researchers employ other similar assays (i.e. secondary PCR based assay) to confirm findings from the novel assays discordant with conventional culture or rapid antigen test (Liolios et al., 2001, Pabbaraju et al., 2008), while others propose using adjunctive clinical data as reference (Doring et al., 2008). Although this retrospective study design did not permit detailed clinical data collection for reference, the secondary analysis was performed using a secondary PCR assay. However, the secondary PCR assay itself is still not perfect in diagnosing every type of respiratory virus in clinical samples. As a result, two of four adenovirus detections, for which the Luminex assay had poor sensitivity to detect (Pabbaraju et al., 2008), were not able to be confirmed in this study and may have underestimated the performance of RT-PCR/ESI-MS platform for adenoviruses.
In the subgroup analysis, differences were not found in the performance characteristics of the platform among different clinical subgroups of the study population as hypothesized, which could be due to small sample size of this pilot. However, specimens from the clinical virology laboratory negative groups were found to contain significantly lower viral load in the RT-PCR/ESI-MS platform compared to the positive group (data not presented), which could be explained by the better sensitivity of the nucleic acid amplification tests (Mahony, 2008). Further studies to confirm performance among patients with different demographic characteristics, are merited.
The current study has several important limitations. Although the optimal design to determine whether the candidate assay performs potentially better than the “gold standard” is to have a third confirmatory test done for every sample, the limited volume of the excess nasopharyngeal aspirate samples, precluded this type of detailed evaluation. Accordingly, readers should be cautioned to interpret results of the secondary analysis carefully, since they could be overestimating performance of the assay (Hadgu et al., 2005). Because of the same reason, specimens with bocavirus detected by RT-PCR/ESI-MS could not be confirmed. Another limitation is that RT-PCR/ESI-MS testing on excess nasopharyngeal aspirate samples was performed several months after initial clinical samples were obtained and tested by clinical virology. Although the effect of length of storage of nasopharyngeal aspirates has been shown to be minimal within 2 months (Ward et al., 2004), another study suggests nucleic acid degradation may be associated the −70 °C storage (Frisbie et al., 2004), and the impact of longer periods of storage remains unknown. Furthermore, the majority of the study population was comprised of paediatric patients (<18 years of age), which limits generalizability of the findings to the adult population. Future validation of the performance of the RT-PCR/ESI-MS platform on adult population is necessary. Lastly, this Ibis T5000 respiratory virus surveillance II kit was not designed to detect rhinovirus, one of the most prevalent respiratory viruses. However, a modified respiratory virus surveillance kit is under development to include rhinovirus, the accuracy and reliability of this type of platform merits further studies using prospective clinical respiratory specimens.
5. Conclusion
In conclusion, the innovative RT-PCR/ESI-MS technology could detect most viruses identified by conventional virology methods rapidly and accurately, and allowed identification of mixed pathogens in clinical specimens. Detection of conventional viruses missed by the clinical virology algorithm, and unconventional viruses required additional confirmatory testing to further evaluate performance characteristics of this assay. The RT-PCR/ESI-MS method is a promising diagnostic platform for rapid identification of conventional and unconventional viruses and merits further prospective evaluation.
Acknowledgement
Financial support for this study in part was provided by Ibis Biosciences, who also provided diagnostic kits and participated in data interpretation.
Footnotes
Grant numbers and sources of support: Drs. Gaydos and Rothman are supported in part by NIAID 2U54AI057168.
The results of this work in part were previously presented at the 48th Annual ICAAC/IDSA 46th Annual Meeting, Washington, DC, October 12–16, 2008.
Supplementary data associated with this article can be found, in the online version, at doi:10.1016/j.jviromet.2011.01.007.
Appendix A. Supplementary data
References
- Anzueto A., Niederman M.S. Diagnosis and treatment of rhinovirus respiratory infections. Chest. 2003;123:1664–1672. doi: 10.1378/chest.123.5.1664. [DOI] [PubMed] [Google Scholar]
- Chen K., Hardick A., Blyn L.B., Sampath R., Melton R., Matthews H., Valsamakis A., Wehrlin J., Rothman R., Gaydos C.A. IDSA/ICAAC; Washington, DC: 2008. PCR and Electrospray Ionization Mass Spectrometry (PCR/ESI-MS) for Identifying Viral Respiratory Infections. October 25–28. [Google Scholar]
- Doring G., Unertl K., Heininger A. Validation criteria for nucleic acid amplification techniques for bacterial infections. Clin. Chem. Lab. Med. 2008;46:909–918. doi: 10.1515/CCLM.2008.152. [DOI] [PubMed] [Google Scholar]
- Ecker D.J., Sampath R., Blyn L.B., Eshoo M.W., Ivy C., Ecker J.A., Libby B., Samant V., Sannes-Lowery K.A., Melton R.E., Russell K., Freed N., Barrozo C., Wu J., Rudnick K., Desai A., Moradi E., Knize D.J., Robbins D.W., Hannis J.C., Harrell P.M., Massire C., Hall T.A., Jiang Y., Ranken R., Drader J.J., White N., McNeil J.A., Crooke S.T., Hofstadler S.A. Rapid identification and strain-typing of respiratory pathogens for epidemic surveillance. Proc. Natl. Acad. Sci. U.S.A. 2005;102:8012–8017. doi: 10.1073/pnas.0409920102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ecker J.A., Massire C., Hall T.A., Ranken R., Pennella T.T., Agasino Ivy C., Blyn L.B., Hofstadler S.A., Endy T.P., Scott P.T., Lindler L., Hamilton T., Gaddy C., Snow K., Pe M., Fishbain J., Craft D., Deye G., Riddell S., Milstrey E., Petruccelli B., Brisse S., Harpin V., Schink A., Ecker D.J., Sampath R., Eshoo M.W. Identification of Acinetobacter species and genotyping of Acinetobacter baumannii by multilocus PCR and mass spectrometry. J. Clin. Microbiol. 2006;44:2921–2932. doi: 10.1128/JCM.00619-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frisbie B., Tang Y.W., Griffin M., Poehling K., Wright P.F., Holland K., Edwards K.M. Surveillance of childhood influenza virus infection: what is the best diagnostic method to use for archival samples? J. Clin. Microbiol. 2004;42:1181–1184. doi: 10.1128/JCM.42.3.1181-1184.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gaydos C. XII International Symposium on Respiratory Viral Infections. 2010. PLEX-ID: a new technology for identification of influenza and other respiratory viruses. [Google Scholar]
- Ginocchio C.C. Detection of respiratory viruses using non-molecular based methods. J. Clin. Virol. 2007;1(40 (Suppl.)):S11–S14. doi: 10.1016/S1386-6532(07)70004-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hadgu A., Dendukuri N., Hilden J. Evaluation of nucleic acid amplification tests in the absence of a perfect gold-standard test: a review of the statistical and epidemiologic issues. Epidemiology. 2005;16:604–612. doi: 10.1097/01.ede.0000173042.07579.17. [DOI] [PubMed] [Google Scholar]
- Hofstadler S.A. S.R., Blyn L.B., Eshoo M.W., Hall T.A. TIGER: the universal biosensor. Int. J. Mass Spectrom. 2005;242:23–41. [Google Scholar]
- Jiang Y., Hofstadler S.A. A highly efficient and automated method of purifying and desalting PCR products for analysis by electrospray ionization mass spectrometry. Anal. Biochem. 2003;316:50–57. doi: 10.1016/s0003-2697(03)00024-1. [DOI] [PubMed] [Google Scholar]
- Liao R.S., Tomalty L.L., Majury A., Zoutman D.E. Comparison of viral isolation and multiplex real-time reverse transcription-PCR for confirmation of respiratory syncytial virus and influenza virus detection by antigen immunoassays. J. Clin. Microbiol. 2009;47:527–532. doi: 10.1128/JCM.01213-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liolios L., Jenney A., Spelman D., Kotsimbos T., Catton M., Wesselingh S. Comparison of a multiplex reverse transcription-PCR-enzyme hybridization assay with conventional viral culture and immunofluorescence techniques for the detection of seven viral respiratory pathogens. J. Clin. Microbiol. 2001;39:2779–2783. doi: 10.1128/JCM.39.8.2779-2783.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mahony J.B. Detection of respiratory viruses by molecular methods. Clin. Microbiol. Rev. 2008;21:716–747. doi: 10.1128/CMR.00037-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pabbaraju K., Tokaryk K.L., Wong S., Fox J.D. Comparison of the Luminex xTAG respiratory viral panel with in-house nucleic acid amplification tests for diagnosis of respiratory virus infections. J. Clin. Microbiol. 2008;46:3056–3062. doi: 10.1128/JCM.00878-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ratcliff R.M., Chang G., Kok T., Sloots T.P. Molecular diagnosis of medical viruses. Curr. Issues Mol. Biol. 2007;9:87–102. [PubMed] [Google Scholar]
- Raymond F., Carbonneau J., Boucher N., Robitaille L., Boisvert S., Wu W.K., De Serres G., Boivin G., Corbeil J. Comparison of automated microarray detection with real-time PCR assays for detection of respiratory viruses in specimens obtained from children. J. Clin. Microbiol. 2009;47:743–750. doi: 10.1128/JCM.01297-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Russell K.L., Broderick M.P., Franklin S.E., Blyn L.B., Freed N.E., Moradi E., Ecker D.J., Kammerer P.E., Osuna M.A., Kajon A.E., Morn C.B., Ryan M.A. Transmission dynamics and prospective environmental sampling of adenovirus in a military recruit setting. J. Infect. Dis. 2006;194:877–885. doi: 10.1086/507426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sampath R., Hofstadler S.A., Blyn L.B., Eshoo M.W., Hall T.A., Massire C., Levene H.M., Hannis J.C., Harrell P.M., Neuman B., Buchmeier M.J., Jiang Y., Ranken R., Drader J.J., Samant V., Griffey R.H., McNeil J.A., Crooke S.T., Ecker D.J. Rapid identification of emerging pathogens: coronavirus. Emerg. Infect. Dis. 2005;11:373–379. doi: 10.3201/eid1103.040629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sampath R., Russell K.L., Massire C., Eshoo M.W., Harpin V., Blyn L.B., Melton R., Ivy C., Pennella T., Li F., Levene H., Hall T.A., Libby B., Fan N., Walcott D.J., Ranken R., Pear M., Schink A., Gutierrez J., Drader J., Moore D., Metzgar D., Addington L., Rothman R., Gaydos C.A., Yang S., St. George K., Fuschino M.E., Dean A.B., Stallknecht D.E., Goekjian G., Yingst S., Monteville M., Saad M.D., Whitehouse C.A., Baldwin C., Rudnick K.H., Hofstadler S.A., Lemon S.M., Ecker D.J. Global surveillance of emerging Influenza virus genotypes by mass spectrometry. PLoS One. 2007;2:e489. doi: 10.1371/journal.pone.0000489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ward C.L., Dempsey M.H., Ring C.J., Kempson R.E., Zhang L., Gor D., Snowden B.W., Tisdale M. Design and performance testing of quantitative real time PCR assays for influenza A and B viral load measurement. J. Clin. Virol. 2004;29:179–188. doi: 10.1016/S1386-6532(03)00122-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu W., Tang Y.W. Emerging molecular assays for detection and characterization of respiratory viruses. Clin. Lab. Med. 2009;29:673–693. doi: 10.1016/j.cll.2009.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


