Abstract
Background
The emergency department (ED) visit rate for older patients exceeds that of all age groups other than infants. The aging population will increase elder ED patient utilization to 35% to 60% of all visits. Older patients can have complex clinical presentations and be resource-intensive. Evidence indicates that emergency physicians fail to provide consistent high-quality care for elder ED patients, resulting in poor clinical outcomes.
Objectives
The objective was to develop a consensus document, “Geriatric Competencies for Emergency Medicine Residents,” by identified experts. This is a minimum set of behaviorally based performance standards that all residents should be able to demonstrate by completion of their residency training.
Methods
This consensus-based process utilized an inductive, qualitative, multiphase method to determine the minimum geriatric competencies needed by emergency medicine (EM) residents. Assessments of face validity and reliability were used throughout the project.
Results
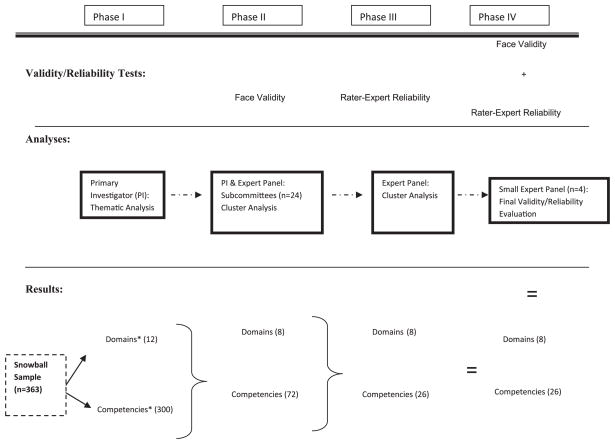
In Phase I, participants (n = 363) identified 12 domains and 300 potential competencies. In Phase II, an expert panel (n = 24) clustered the Phase I responses, resulting in eight domains and 72 competencies. In Phase III, the expert panel reduced the competencies to 26. In Phase IV, analysis of face validity and reliability yielded a 100% consensus for eight domains and 26 competencies. The domains identified were atypical presentation of disease; trauma, including falls; cognitive and behavioral disorders; emergent intervention modifications; medication management; transitions of care; pain management and palliative care; and effect of comorbid conditions.
Conclusions
The Geriatric Competencies for EM Residents is a consensus document that can form the basis for EM residency curricula and assessment to meet the demands of our aging population.
Keywords: geriatrics, emergency medicine residents, competency, consensus
The specialty of emergency medicine (EM) shoulders a great responsibility for the care of older adult patients in the United States. There were more than 17 million elder patient visits to emergency departments (EDs) in 2006, with visit rates exceeding those of all age groups other than infants.1 By 2030, the number of U.S. elders will almost double to 71 million, accounting for roughly 20% of the U.S. population.2 Older patients tend to have complex clinical presentations, and their care can be resource-intensive. Evidence indicates that emergency physicians (EPs) fail to provide consistent high-quality care for elder ED patients and that this results in poor clinical outcomes.3–10 Few EDs address the distinctive needs of older patients, and many do not have the necessary expertise, equipment, and policies in place to provide optimal care for this growing population.11,12 Older patients are often diagnostically challenging and quite ill, and their clinical presentations are often atypical or influenced by underlying comorbidities. In addition, older patients who present to the ED are a particularly challenging subgroup for the ED culture. They tend to be very time- and resource-intensive and have few safeguards in place for observation and care at home. As a consequence, they are admitted more often than their younger counterparts to the hospital and intensive care unit,13–15 although hospitalization has been shown to carry significant risk for this population.16,17
Despite this compelling need, there is little training for EPs in the unique clinical and psychosocial characteristics of older patients.18 In 1992, an American College of Emergency Physicians (ACEP) member survey found that practicing EPs considered it more difficult to manage elders compared with younger patients and that the time spent during residency training on geriatric EM was inadequate.19 When this survey was replicated in 2007, no improvement was identified.20
A 2008 Institute of Medicine (IOM) report details the crisis facing all segments of the health care workforce as the numbers of elders swell over the next 20 years.21 The IOM’s report recommends that “the geriatric competence of virtually all members of the health care workforce needs to be improved through significant enhancements in educational curricula and training programs, and then assessed through career-long demonstrations of this competence.”21 IOM recommendation number 4.2 goes on to state, “All licensure, certification and maintenance of certification for health care professionals should include demonstration of competence in the care of older adults as a criterion.”21
In October 2008, ACEP published a white paper detailing the multiple challenges that the surging “gray tsunami” will have on the practice of EM over the next two decades.22 ACEP’s primary recommendation to address these issues is education, particularly to 1) prioritize and provide support for the development of an enhanced geriatric core curriculum for resident training and 2) prioritize and support the development and dissemination of a body of core knowledge for practicing emergency clinicians similar to that for pediatrics and trauma.
Recently, geriatrics-specific, competency-based consensus performance standards for medical students were created and disseminated by Leipzig et al.23 This was the first crucial development in medical education’s response to the IOM report. Leipzig and her colleagues demonstrated a way for graduate medical educators to advocate for new educational standards improving the care of older adults by applying the principles of competency-based training.
Competency-based training is the new standard for medical education. Over the past 10 years, the Accreditation Council for Graduate Medical Education (AC-GME) has moved from granting accreditation to residency programs based on their compliance with curricular and structural requirements, to a process where residencies are assessed on the actual accomplishments of their residents. Specifically, the ACGME requires that residents achieve measurable outcomes of performance and knowledge. This model shifts resident education to the demonstration of clinical competency in general (e.g., communication skills and professionalism) and discipline specific (e.g., medical knowledge) areas.24 Curricula and assessment are driven by the competencies, with the curricula describing how and where this learning occurs.
In this article, we describe the use of a consensus method to identify geriatric competencies for EM residents, a minimum set of behaviorally based performance standards that all residents should be able to demonstrate by completion of their residency training. All of the geriatric EM competencies begin with the phrase, “The graduating emergency medicine resident, in the context of a specific older patient scenario (real or simulated), must be able to …,” and then describes a specific behavior that the learner must demonstrate. This differs from a curriculum in an important way. While a topic area for learning is clearly described as in a curriculum, the desired outcome is not just didactic mastery of the topic area, but a defined behavior generated within that context.
We focus on EM resident education because residency programs train physicians to provide what becomes the standard of competent care to older adults. When these minimum geriatric competencies become the baseline for completion of residency training, the next step will be to assure that all practicing EPs achieve these competencies through continuing medical education and maintenance of certification.
METHODS
Process Overview and Timeline
Our primary objective was to develop a consensus document by identified experts on geriatric-based competencies for EM residents. This consensus process used an inductive qualitative research methodology to produce a consensus document.25 The phases are diagramed in Figure 1 and took place between February and December 2008 (Table 1). The Geriatric EM Competencies developed in this study expand, in a specialty-specific manner, the competencies developed for graduating medical students, by building on the medical student competencies the same way that residency training builds on medical school.23
Figure 1.
Phases. *Domains = broad general categories in the care of ED elders that encompass each competency; competencies = specific measurable behaviors that the EM resident must achieve.
Table 1.
Timeline for Consensus Process to Determine Geriatrics-related EM Resident Competencies
| Phase | Dates | Participants | Process | Results |
|---|---|---|---|---|
| I. Identify universe of potential content | Feb–May 2008 | Participant driven snowball sampling: selected members of: SAEM Geriatric Task Force SAEM Geriatric Interest Group ACEP Geriatric Section ENA Leadership Group EMRA CORD AGS (n = 363) |
PI conducted narrative inquiry using AAMC Medical Student Competencies and participants personal experiences as starting points | 12 domains: atypical presentations, emergent actions, trauma, falls, conditions causing morbidity, dementia and delirium, palliative care, transitions of care, medication problems, AMI stroke and sepsis, policies and procedures, geriatric syndromes. >300 competencies |
| II. Begin to narrow focus to essential domains and competencies | May–Oct 2008 | Expert panel (n = 24) | Specific subcommittees using online wiki and twice weekly expert panel conference calls | 8 domains 72 competencies |
| III. Consensus conference | Oct 26, 2008 | Expert panel (n = 24) | Face-to-face meeting | 8 domains 26 competencies |
| IV. Finalizing the document review for clarity and uniqueness | Nov–Dec 2008 | Smaller expert panel data analysts (n = 4) Expert panel (n = 24) |
Review for clarity and uniqueness (reliability and validity) Online wiki for agreement |
Domains finalized as most relevant to EM (Table 3) Consensus maintained |
Domains = broad general categories in the care of ED elders that encompass each competency; competency = specific measurable behavior that the EM resident must achieve.
AAMC = Association of American Medical Colleges; ACEP = American College of Emergency Physicians; AGS = American Geriatric Society; AMI = acute myocardial infarction; CORD = Council of Emergency Medicine Residency Directors; EMRA = Emergency Medicine Residents’ Association; ENA = Emergency Nurses Association; PI = primary investigator; SAEM = Society for Academic Emergency Medicine.
A snowball sample of participants and expert panel members initiated a four-phase process to gather the data (specific content that would become competencies). A snowball sample assembles a nonrandom population (in this case EPs and educators) with expertise in the topic at hand. The group is sampled on goal-directed topics and then asked to identify additional expert subjects for sampling until recommendations for further subjects are exhausted or repeated.26
A methodologic thematic analysis approach was used for this consensus document to establish the most appropriate geriatric EM competencies. All procedures were supported with institutional review board approval. The principal investigator (PI; TH) generated categories and themes, which were sequentially tested with the expert panel members for reliability and validity using Boyatzis’ method25 of rater-to-expert reliability. Rater–expert reliability is also known as category agreement with an expert. Specific other individuals who have authored previous research, discovered themes, and developed thematic codes are used to ensure consistency of judgment among viewers. Triangulated data sources were used. First, the PI’s documentation and wiki recording processes were used to compile the data and create a consistent source of information for the members of the expert panel, who served as coders.27,28 Additionally, both literature reviews and the undergraduate competencies were used to compare and contrast the recommended geriatric EM competencies.
Phase I: Identifying the Universe of Potential Content
In 2008, the PI was awarded a Brookdale Leadership in Aging Fellowship for the purpose of leading development of geriatric competencies in EM. She engaged leaders of the ACEP Geriatric Section, the American Geriatric Society (AGS) Council of Surgical and Related Specialty Societies, the American Medical Association (AMA) Impact in Aging Committee, the Council of Emergency Medicine Residency Directors (CORD), and the Society for Academic Emergency Medicine (SAEM) Geriatric Task Force in this process.
Snowball sampling was used to identify the largest possible number of individuals to consider those items important in the care of elder ED patients.29,30 The initial participants were identified based on publication history, position in stakeholder organizations, and participation in key interest groups. A total of 363 physician participants were identified and sampled by the PI using the above technique.
A narrative inquiry was used to gather the initial domains and competency themes.31 Domains are the broad general categories in the care of ED elders that encompass each competency, or specific measurable behavior, that the EM resident must achieve. Participants were asked to identify the important issues in the care of elders in the ED. The medical student competencies served to inform this conversation and as a template for the divisions into domains and competencies. Participants recalled real geriatric patient encounters and dissected the events in the care of those patients. The PI then categorized themes in the conversations into domains and competencies.
After the participants exhausted their suggestions for potential domains and competencies, they were asked who else might add valuable input to the process. The suggested individuals were then queried in an identical manner. The sampling ended when suggestions became redundant and those suggested as additional participants had already been queried. From these responses, thematic analyses yielded a total of 12 domains (Table 1) and over 300 potential competencies.
Phase II: Narrowing the Focus to Essential Competencies
The PI recruited a 24-member expert panel (see Data Supplement S1, available as supporting information in the online version of this paper) on the basis of their expertise in medical education, EM residency training, EM geriatric content, or general geriatric content. These individuals were selected to represent a wide spectrum of organizations, and represented 16 EM residency programs, dean’s offices, ACEP, AGS, AMA, CORD, the Emergency Medicine Residents Association (EMRA), the Residency Review Committee (RRC)-EM, and SAEM. One individual could represent more than one group. The expert panel also included leaders in the development of the Association of American Medical Colleges (AAMC) medical student geriatric competencies. It was anticipated that the professional standing and expertise of the members of the group, along with structured review of the evidence, would enhance acceptance of the recommendations by leaders in the field. The expert panel’s charge was to refine the domains and competencies identified to develop the consensus document.
This expert panel then broke up into subcommittees that tackled each of the broad domains and the series of related competencies. They were asked to limit the list to the smallest possible number of geriatric EM specific items pertaining to the behaviors that an EM resident would have to achieve to be minimally competent in the care of older adults in the ED. Specific guidelines (Table 2) were given to the subcommittees to assist in this cluster analysis process. Ultimately, the panel used an iterative process of refining the domains and competencies to the content that all agreed was essential to the practice of EM and absolutely necessary to assure competent care for older adults in the ED.
Table 2.
Guidelines for Competencies
| Each competency must be: |
|---|
|
The subcommittees worked through an interactive online “wiki” (accessible online workspace for asynchronous collaboration) discussing, researching, and refining the 300 potential competencies to 72 behavioral-based competencies. In addition, they reduced the domains from 12 to 8. An extensive literature review was conducted to inform the selections of the competency items and assure that the final items reflected the best clinical evidence available. The literature searches were begun by the PI and augmented substantially by each subcommittee, whose members often had significant expertise in the domain. Subcommittee work was facilitated by a series of biweekly expert panel conference calls between May and October 2008. Through this process some domains were unified or renamed, and others eliminated. Each of the subcommittees then submitted its list of competencies to the larger group in a wiki format in preparation for the consensus conference to evaluate the face validity of the competencies.
Most of the competencies that were eliminated represented good medicine that was likely to be encountered by EM residents in many adult, not necessarily geriatric, patients or that were process and systems issues out of the control of residents. For example, the statement “To search for anticoagulation and reverse any coagulopathy in patients with significant trauma” was one of the initial competencies. Although more elder patients are anticoagulated than are patients in younger age groups,32 it is always good medicine to search for anticoagulation and reverse coagulopathy in trauma. Therefore, this was not considered to meet the geriatric-specific guideline. Competencies were included when they occur in all adults, but there are special considerations in older patients. For example, medication management in older adults requires special attention to age-related changes in drug metabolism and response, requiring dosage modification and avoiding the use of certain drugs. Older adults in hospice care are covered by specific Medicare guidelines that are not applicable to younger adults. Finally, outcomes of some ED practices have worse outcomes in geriatric patients, such as the likelihood of developing a pressure ulcer from lying for a long time on a backboard or ED stretcher.
If a competency was specific to geriatric care but not a resident-specific task, it was also dropped. For example, “To expedite imaging in elders who are back boarded and with cervical collars in order to decrease iatrogenic pressure ulcerations” is elder specific.33 However, this is an operations or policy issue. While residents can sometimes effect and expedite the workup of such patients, assuring that this occurs systematically is not under resident control, and therefore this did not make the final list of competencies.
Phase III: Consensus Conference
The next refinement of domains and competencies was achieved in a formal face-to-face meeting. The expert panel convened at a day-long meeting in Chicago on October 26, 2008. Its mandate was to review the list of 72 competencies developed by the subcommittees and come to consensus on a final list of essential competencies. Using audience response software (Turning Technologies, LLC, Youngstown, OH), each competency was presented and participants rated each as must include, should include, or do not need to include, a method of rater–expert internal reliability.25
After debates about feasibility and educational and clinical appropriateness, eight domains and 26 competencies emerged. The domains were atypical presentation of disease; trauma, including falls; cognitive and behavioral disorders; emergent intervention modifications; medication management; transitions of care; pain management and palliative care; and effect of comorbid conditions. A final consensus-based recommendation to accept or reject each competency was made by the entire group. At the end of the meeting, unanimous consensus was reached that these 26 competencies constituted the essential knowledge and skills that all EM residents must achieve prior to finishing their training.
Phase IV: Finalizing the Competencies
Once the final 26 competencies were established by the consensus conference, a subgroup of four expert panel members tested the domains and competencies for reliability and validity to ensure the clarity and uniqueness of the language and consistency of form and substance. The subgroup evaluated each competency for face validity—that the content of the competency clearly fit with the concept of the domain. In addition, reliability (100%) was tested with a rater–expert coder process.34 The group assured that each competency was behaviorally based and had a reasonable behavioral measure embedded within it.
To improve the validity of the competencies, the data were triangulated using both a literature review and the AMC medical student competencies. The literature review consisted of the PI and experts gathering relevant literature to clarify the significance of issues and topics for each domain. The undergraduate competencies were used to compare the recommended EM competencies to the minimum criteria established by the consensus for undergraduate geriatric competency. The final consensus document of minimum geriatric competencies for EM residents was circulated to the whole expert panel for review and was unanimously approved (see Table 3).
Table 3.
Geriatric EM Resident Domains and Competencies
|
The graduating EM resident, in the context of a specific older patient scenario (real or simulated), must be able to: | |
|---|---|
| Domain | Competency |
| I. Atypical presentation of disease |
|
| II. Trauma including falls |
|
| III. Cognitive and behavioral disorders |
|
| IV. Emergency intervention modifications |
|
| V. Medication management |
|
| VI. Transitions of care |
|
| VIII. Effect of comorbid conditions |
|
NSAID = nonsteroidal anti-inflammatory drug; PCP = primary care provider.
DISCUSSION
This article describes the iterative process of consensus development used to identify the essential knowledge and skills residents need, in addition to core EM training, to give competent care to elders in the ED. The results of this inductive, qualitative consensus process highlight the issues that EM education and geriatric experts believe EM residents should have the ability to recognize, anticipate, and act on to assure the quality and safety of care received by elders in the emergency setting. With clear guidelines, experts identified eight domains and 26 competencies.
The domains reflect three types of content. The first are core geriatrics concepts such as the atypical presentation of disease, recognition and treatment of cognitive and behavioral disorders, and the complexities of medication management. Elders simply present differently from younger adults. Myocardial infarctions often present with dyspnea or dizziness, not chest pain; a perforated viscous presents without abdominal tenderness; subdural hematomas without acute neurologic changes; and injury with occult shock.35–37 However, these subtle presentations are not really atypical for elders, they are just different from what is typical for younger adults. EM residents need to learn the typical presentations for the countless elders they will see in their practices.
The second content area includes core EM concerns such as trauma and emergent interventions. Trauma is a key part of the EM curriculum, and falls are the most prevalent type of geriatric trauma.35 Yet understanding how to care for elders who have fallen, and how to prevent future falls, is not a standard part of residents’ training. Emergent intervention modifications include adapting treatments and monitoring to maximize benefit and minimize harm in elders. Modifications include recognizing that, in general, age alone should not be the deciding factor on whether to treat, and that for older adults, the need for care like bladder catheterization or spinal immobilization needs to be regularly reevaluated because the benefit may decrease while the likelihood of harm increases.38
The third content area involves adapting fundamental principles within geriatrics to the specifics of the emergency patient. These include concerns about transitions of care (the tradeoff in care and safety between going home and hospitalization), pain management and palliative care (the tradeoff between the ED need for rapid pain management and the geriatric mantra of “start low, go slow” for medications), and anticipating the effect of comorbid conditions on the patient’s episode of illness. EPs must recognize that many elders are physiologically frail and that stress on one system can soon lead to deterioration in another. For example, an elder who comes to the ED with a gastrointestinal hemorrhage is at risk for myocardial ischemia. Residents need to anticipate what other organ systems are at risk and take appropriate preventive measures.
The Model of the Clinical Practice of Emergency Medicine is designed as the core foundation document for future medical school and residency curricula.39 The geriatric competencies are meant to complement the Model, taking those broad overarching principles and identifying the specific behaviors that assure quality care for geriatric patients. The competencies are intended to inform the curriculum and assessments needed for residents to gain the knowledge and skills to demonstrate these behaviors.
Defining the geriatric EM competencies is just a first step toward achieving desired norms of practice for older adults seen in the ED. Despite the “calls to action” from ACEP and the IOM, the interest of CORD leadership, and the ACGME mandate to move to competency-based education, there are multiple barriers to actually achieving this goal. One is that most faculty did not receive training in geriatric EM, making it less likely that they will be comfortable teaching the competencies to their residents. At the request of CORD, an educational “tool box” is being developed to provide curricular materials that residency programs can use to facilitate implementing geriatric EM teaching and assessment. The tool box of teaching and assessment resources for the geriatric EM competencies, being developed by members of the expert panel and others, will serve as a content repository for educational material that supports the teaching of each competency and for faculty development. These educational materials will be organized under the eight domains and include relevant articles, PowerPoint presentations, Web-based interactive clinical cases, pocket cards, and suggested assessment tools. The tool box will also include resources that can be used for asynchronous learning outside of the conference setting. Assessment tools are being developed, including written tests, case simulations, interactive Web-based cases, and other materials to facilitate the measurement of residents’ performance of the competencies. The tool box also provides links between each geriatric competency and the corresponding ACGME core competency it demonstrates. In this way the geriatric competencies can be used to demonstrate active compliance with ACGME and RRC mandates. An example of such a tool box exists in the Portal of Geriatric Online Education (http://www.pogoe.org), sponsored by the Donald W. Reynolds Foundation, where the AAMC medical student geriatric competencies are being linked to teaching and assessment products accessible on the Web site.
Implementing effective models of education in an overcrowded residency curriculum is a challenge to all programs. According to several theoretical models of education, such as Miller’s Triangle,40 and the six steps identified by Davis et al.,41 learners must progress through specific stages to achieve competence. Each step is necessary for the next, and the steps build on one another toward the final goal of consistently improved patient outcomes. Receptive attitudes are necessary to allow suitable intake of knowledge, knowledge must be used to develop skills, skills must be used to result in appropriate actions, actions must achieve desired outcomes, and all of these must be taken up in norms of practice for overall improvement to result. Definition of minimum competency targets is a necessary prerequisite for implementing any of these steps well. There are several ways that viable implementation can be achieved using these models. Currently a pilot is under way at five EM residency programs to evaluate one method for teaching the geriatric EM competencies. Attitudes toward the care of older adults, knowledge, and skill acquisition in EM residents will be measured as outcomes using a written knowledge assessment as well as chart review. Impact on norms of practice will not be measured, but can be expected, and progress will be further aided as additional residency programs adopt these competencies.
The geriatric EM competencies herald a new era for EM residency programs. With this tool we have identified critical topic areas with its own set of minimum behaviorally measurable performance standards. With such tools, resident educators can seize new opportunities to drive specialty content. The competencies can serve as evidence of a program’s advancement in step with the ACGME Outcomes Project, because each competency ties to several of the core competences. The geriatric EM competencies can serve as a report card for mastery and eventually assure the public that our residents are prepared for the predictable challenges of caring for the upcoming tidal wave of older adults.
CONCLUSIONS
We describe the expert consensus development of the document Geriatric Competencies for EM Residents. We utilized snowball sampling, literature review, prior consensus documents, consensus panels, expert advice, and principles of inductive, qualitative, multiphased research to create a minimum set of competencies for the care of older adults that EM residents would be expected to achieve during residency. The consensus document is written in behavior-based language so that it can serve as the basis for competency-based geriatrics EM curriculum and assessment tools to measure resident attainment of the competent behavior it defines. These competencies define the minimum set of behaviors that EM residents need to demonstrate to ensure that they are able to care for our nation’s rapidly growing and complex older patient population.
Pilot work is now under way to examine the effect of dissemination of these competencies to five selected EM residency programs. The pilot evaluation will focus on changes in knowledge through pre- and postdidactic testing, attitudes through surveys, and behavior through retrospective chart review of selected documentation points.
These competencies are a start at defining physician behavior that can improve quality of care for older adults in EM. They are resident-focused, although many apply to all practicing physicians. Future work on competencies for attending physicians will build on these, but could also address systems changes needed to improve care for geriatric ED patients. Having residents achieve these competencies is a first step at ensuring better outcomes for older adults receiving emergency care.
Supplementary Material
Expert panel.
Acknowledgments
The authors acknowledge the inspirational mentorship of Dr. Linda Emanuel, the Buehler Professor of Geriatric Medicine and Director of the Buehler Center on Aging at Northwestern’s Feinberg School of Medicine; Dr. Rosanne Leipzig, Gerald and May Ellen Ritter Professor and Vice Chair, Education, Brookdale Department of Geriatrics and Adult Development, Mount Sinai School of Medicine; and Dr. Gary Strange, Professor and Chair, Department of Emergency Medicine, University of Illinois, Chicago. This project would not be possible without the dedication and expertise of the entire expert panel who worked tirelessly for the cause of improving care for our nation’s elders. Finally, the authors thank all who participated in the snowball sampling: your ideas carried us forward.
This work was primarily funded by a grant from the Brookdale Foundation, through the Brookdale Leadership in Aging Fellowship. The authors thank them for their generous support and advocacy for geriatric care. Additional support was provided by the American Medical Association through underwriting the conference calls, consensus conference, and support of the Mount Sinai School of Medicine and the Portal of Geriatric Online Education.
References
- 1.Pitts SR, Niska RW, Xu J, Burt CW. [Accessed Dec 2, 2009];National Hospital Ambulatory Medical Care Survey: 2006 Emergency Department Summary. Available at: http://www.cdc.gov/nchs/data/nhsr/nhsr007.pdf. [PubMed]
- 2.Roberts DC, McKay MP, Shaffer A. Increasing rates of emergency department visits for elderly patients in the United States, 1993 to 2003. Ann Emerg Med. 2008;51:769–74. doi: 10.1016/j.annemergmed.2007.09.011. [DOI] [PubMed] [Google Scholar]
- 3.Chin MH, Jin L, Karrison TG, et al. Older patients’ health related quality of life around an episode of emergency illness. Ann Emerg Med. 1999;34:595–603. doi: 10.1016/s0196-0644(99)70161-7. [DOI] [PubMed] [Google Scholar]
- 4.Denman SJ, Ettinger WH, Zarkin BA, Coon PJ, Casani JA. Short-term outcomes of elderly patients discharged from an emergency department. J Am Geriatr Soc. 1989;37:939–43. doi: 10.1111/j.1532-5415.1989.tb07278.x. [DOI] [PubMed] [Google Scholar]
- 5.Friedmann PD, Jin L, Karrison TG, et al. Early revisit, hospitalization, or death among older persons discharged from the ED. Am J Emerg Med. 2001;19:125–9. doi: 10.1053/ajem.2001.21321. [DOI] [PubMed] [Google Scholar]
- 6.Krumholz HM, Radford MJ, Wang Y, Chen J, Marciniak TA. Early beta-blocker therapy for acute myocardial infarction in elderly patients. Ann Intern Med. 1999;131:648–54. doi: 10.7326/0003-4819-131-9-199911020-00003. [DOI] [PubMed] [Google Scholar]
- 7.Lee PY, Alexander KP, Hammill BG, Pasquali SK, Peterson ED. Representation of elderly persons and women in published randomized trials of acute coronary syndromes. JAMA. 2001;286:708–13. doi: 10.1001/jama.286.6.708. [DOI] [PubMed] [Google Scholar]
- 8.Magid DJ, Masoudi FA, Vinson DR, et al. Older emergency department patients with acute myocardial infarction receive lower quality of care than younger patients. Ann Emerg Med. 2005;46:14–21. doi: 10.1016/j.annemergmed.2004.12.012. [DOI] [PubMed] [Google Scholar]
- 9.Wilber ST. Altered mental status in older emergency department patients. Emerg Med Clin North Am. 2006;24:299–316. doi: 10.1016/j.emc.2006.01.011. [DOI] [PubMed] [Google Scholar]
- 10.Rathore SS, Mehta RH, Wang Y, Radford MJ, Krumholz HM. Effects of age on the quality of care provided to older patients with acute myocardial infarction. Am J Med. 2003;114:307–15. doi: 10.1016/s0002-9343(02)01531-0. [DOI] [PubMed] [Google Scholar]
- 11.Hwang U, Morrison RS. The geriatric emergency department. J Am Geriatr Soc. 2007;55:1873–6. doi: 10.1111/j.1532-5415.2007.01400.x. [DOI] [PubMed] [Google Scholar]
- 12.Wilber ST, Gerson LW, Terrell KM, et al. Geriatric emergency medicine and the 2006 Institute of Medicine reports from the Committee on the Future of Emergency Care in the U.S. Health System. Acad Emerg Med. 2006;13:1345–51. doi: 10.1197/j.aem.2006.09.050. [DOI] [PubMed] [Google Scholar]
- 13.Singal BM, Hedges JR, Rousseau EW, et al. Geriatric patient emergency visits. Part I: comparison of visits by geriatric and younger patients. Ann Emerg Med. 1992;21:802–7. doi: 10.1016/s0196-0644(05)81025-x. [DOI] [PubMed] [Google Scholar]
- 14.Strange GR, Chen EH. Use of emergency departments by elder patients: a five-year follow-up study. Acad Emerg Med. 1998;5:1157–62. doi: 10.1111/j.1553-2712.1998.tb02688.x. [DOI] [PubMed] [Google Scholar]
- 15.Strange GR, Chen EH, Sanders AB. Use of emergency departments by elderly patients: projections from a multicenter data base. Ann Emerg Med. 1992;21:819–24. doi: 10.1016/s0196-0644(05)81028-5. [DOI] [PubMed] [Google Scholar]
- 16.Fernandez HM, Callahan KE, Likourezos A, Leipzig RM. House staff member awareness of older inpatients’ risks for hazards of hospitalization. Arch Intern Med. 2008;168:390–6. doi: 10.1001/archinternmed.2007.87. [DOI] [PubMed] [Google Scholar]
- 17.Horwitz LI, Meredith T, Schuur JD, Shah NR, Kulkarni RG, Jeng GY. Dropping the baton: a qualitative analysis of failures during the transition from emergency department to inpatient care. Ann Emerg Med. 2009;53:701–10. doi: 10.1016/j.annemergmed.2008.05.007. [DOI] [PubMed] [Google Scholar]
- 18.Institute of Medicine Committee on the Future of Emergency Care in the U.S. Health System. Emergency Medical Services at the Crossroads. Washington, DC: National Academies Press; 2006. [Google Scholar]
- 19.McNamara RM, Rousseau EW, Sanders AB. Geriatric emergency medicine: a survey of practicing emergency physicians. Ann Emerg Med. 1992;21:796–801. doi: 10.1016/s0196-0644(05)81024-8. [DOI] [PubMed] [Google Scholar]
- 20.Carpenter CR, Lewis LM, Caterino JM, Wilber S, Scheatzle M, Fiorello A. Emergency physician geriatric education: an update of the 1992 Geriatric Task force survey. Has anything changed? [abstract] Ann Emerg Med. 2008;52(4 Suppl 1):S156. [Google Scholar]
- 21.Institute of Medicine Committee on the Future Health Care Workforce for Older Americans. Retooling for an Aging America: Building the Health Care Workforce. Washington, DC: The National Academies Press; 2008. [PubMed] [Google Scholar]
- 22.Fitzgerald RT. The Future of Geriatric Care in Our Nation’s Emergency Departments: Impact and Implications. Dallas, TX: American College of Emergency Physicians; 2008. [Google Scholar]
- 23.Leipzig RM, Granville L, Simpson D, Anderson MB, Sauvigne K, Soriano RP. Keeping granny safe on July 1: a consensus on minimum geriatrics competencies for graduating medical students. Acad Med. 2009;84:604–10. doi: 10.1097/ACM.0b013e31819fab70. [DOI] [PubMed] [Google Scholar]
- 24.Chapman DM, Hayden S, Sanders AB, et al. Integrating the Accreditation Council for Graduate Medical Education core competencies into the model of the clinical practice of emergency medicine. Ann Emerg Med. 2004;43:756–69. doi: 10.1016/j.annemergmed.2003.12.022. [DOI] [PubMed] [Google Scholar]
- 25.Boyatzis RE. Thematic Analysis and Code Development: Transforming Qualitative Information. Thousand Oaks, CA: Sage Publications; 1998. [Google Scholar]
- 26.Goodman LA. Snowball sampling. Ann Math Stat. 1961;32:148–70. [Google Scholar]
- 27.Holsti OR. Content analysis. In: Lindsey G, Aronson E, editors. Handbook of Social Psychology. Reading, MA: Addison-Wesley; 1968. [Google Scholar]
- 28.Smith CP. Managerial Competence: The Key to Excellence. Dubuque, IA: Kendall/Hunt; 1992. [Google Scholar]
- 29.Heckathorn DD. Collective samples and compliance norms: a formal theory of group mediated social control. Am Sociol Rev. 1990;55:366–84. [Google Scholar]
- 30.Heckathorn DD. Respondent-driven sampling: a new approach to the study of hidden populations. Social Problems. 1997;44:174–99. [Google Scholar]
- 31.Marshall C, Rossman GB. Designing Qualitative Research. 3. Thousand Oaks, CA: Sage Publications; 1999. [Google Scholar]
- 32.Hutten BA, Lensing AW, Kraaijenhagen RA, Prins MH. Safety of treatment with oral anticoagulants in the elderly: a systematic review. Drugs Aging. 1999;14:303–12. doi: 10.2165/00002512-199914040-00005. [DOI] [PubMed] [Google Scholar]
- 33.Ackland HM, Cooper DJ, Malham GM, Kossmann T. Factors predicting cervical collar related decubitus ulceration in major trauma patients. Spine. 2007;32:423–8. doi: 10.1097/01.brs.0000255096.52871.4e. [DOI] [PubMed] [Google Scholar]
- 34.Anastas JW, MacDonald ML. Research Design for Social Work and the Human Services. New York, NY: Lexington Books; 1994. [Google Scholar]
- 35.Callaway DW, Wolfe R. Geriatric trauma. Emerg Med Clin North Am. 2007;25:837–60. doi: 10.1016/j.emc.2007.06.005. [DOI] [PubMed] [Google Scholar]
- 36.Majeski J, Durst GG. Geriatric acute perforated appendicitis: atypical symptoms lead to a difficult diagnosis. South Med J. 1998;91:669–71. doi: 10.1097/00007611-199807000-00014. [DOI] [PubMed] [Google Scholar]
- 37.Muller RT, Gould LA, Betzu R, Vacek T, Pradeep V. Painless myocardial infarction in the elderly. Am Heart J. 1990;119:202–4. doi: 10.1016/s0002-8703(05)80106-1. [DOI] [PubMed] [Google Scholar]
- 38.Alter DA, Manuel DG, Gunraj N, Anderson G, Naylor CD, Laupacis A. Age, risk-benefit trade-offs, and the projected benefits of evidence-based therapy. Am J Med. 2004;116:540–5. doi: 10.1016/j.amjmed.2003.10.039. [DOI] [PubMed] [Google Scholar]
- 39.Thomas HA, Beeson MS, Binder LS, et al. [Accessed Dec 2, 2009];Model of the Clinical Practice of Emergency Medicine from the American College of Emergency Physicians and Society for Academic Emergency Medicine and American Board of Emergency Medicine. 2007 Available at: https://www.abem.org/public/_Rainbow/Documents/2007%20EM%20Model.pdf.
- 40.Miller GE. The assessment of clinical skills/competence/performance. Acad Med. 1990;65:S63–7. doi: 10.1097/00001888-199009000-00045. [DOI] [PubMed] [Google Scholar]
- 41.Davis DA, Thomson MA, Oxman AD, Haynes RB. Changing physician performance: a systematic review of the effect of continuing medical education strategies. JAMA. 1995;274:700–5. doi: 10.1001/jama.274.9.700. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Expert panel.