Abstract
Purpose
The aim of the study was to assess the role of residual hip dysplasia as a risk factor for osteoarthritis (OA) in developmental dysplasia of the hip (DDH).
Methods
Fifty-one patients (60 hips) with late-detected DDH were studied. Reduction had been performed at a mean age of 19 months (range 4–65 months). On radiographs at age 8–10 years, at skeletal maturity, and at long-term follow-up, femoral head coverage was assessed using the migration percentage (MP) and centre-edge (CE) angle. OA was diagnosed if the minimum joint space width of the upper part of the joint was <2.0 mm.
Results
The mean age at the last follow-up was 45 years (range 43–49 years) in patients who had not undergone total hip replacement (THR). Ten patients had developed OA and eight of them had undergone THR at a mean age of 40 years (range 32–47 years). There was a clear association between OA and residual hip dysplasia. At the last follow-up, 37 hips had normal CE angles (20° or higher) and OA had developed in only two of them (5%; 95% confidence interval [CI] 1–18%). Hip dysplasia without subluxation (CE angle 10–19°) was seen in 18 hips, of which 14 hips had good outcome and four had OA (22%; 95% CI 6–48%). Subluxation occurred in five hips, of which one had a good long-term outcome and four had OA (80%; 95% CI 28–99%). In patients without late reconstructive surgery, MP increased from the age of 10 years to skeletal maturity; thereafter, no significant change occurred. The CE angle did not change significantly between the age of 10 years and the last follow-up.
Conclusion
Hip dysplasia without subluxation has a relatively good long-term prognosis. Subluxation is a risk factor for osteoarthritis. Thus, children with MP above 33% and CE angle under 10° should be evaluated for reconstructive surgery in order to improve the long-term outcome.
Keywords: Developmental hip dislocation, Residual hip dysplasia, Long-term follow-up, Osteoarthritis of the hip
Introduction
Unsatisfactory development of the hip with residual dysplasia and reduced femoral head coverage has been reported in more than one-third of patients treated for late-detected developmental dysplasia of the hip (DDH) [1–3]. Although persistent acetabular dysplasia and subluxation are risk factors for the development of osteoarthritis (OA) later in life [4–7], there is no consensus with regard to the degree of dysplasia that is of clinical significance or how long a time it takes for OA to become clinically manifest. Another controversial question is to what degree residual dysplasia changes during long-term follow-up [2, 8].
Residual hip dysplasia can be corrected by pelvic and femoral osteotomies. The aim of these procedures is to avoid or postpone the development of later OA. Whereas the short-term and mid-term results of such procedures have been good [9], the long-term outcome shows a deterioration with time [10]. Therefore, to evaluate the indications for surgical treatment, long-term studies are necessary of unoperated patients showing the natural history and of patients who have undergone reconstructive surgery.
The aims of the present retrospective study were to:
Assess the role of residual hip dysplasia with and without subluxation as risk factors for the development of OA
Evaluate to what degree the radiographic indicators of hip dysplasia change during adolescence and adulthood
Patients and methods
A search through the diagnosis card index for the period 1961–1962 revealed 75 patients who had been treated for late-detected DDH in our department. Fifty-three patients formed a consecutive group with treatment commencement in 1961–1962. Treatment had been initiated during the period 1958–1960 in the remaining 22 patients and they had had additional admission for treatment during 1961–1962. The patients had no other congenital anomalies and they had not been previously treated in other hospitals. Before the present follow-up examination, four patients had died and two had been followed up to an age of <8 years. The remaining patients received a written request for a follow-up during 2005–2006. Fifty-two patients attended this long-term follow-up examination, whereas 17 patients, for various reasons, did not want to participate. Because the aim of the study was to assess the influence of residual hip dysplasia and subluxation on the incidence of OA, five hips with OA caused by marked deformities of the femoral head and neck due to severe avascular necrosis (three hips) or infection after acetabular shelf procedure (two hips) were not included. They represented both hips of one patient and one hip of each of three patients with bilateral affection.
Thus, 51 patients with 60 affected hips were included in the present study. The study was approved by the Regional Committee of Medical Research Ethics. Informed consent was received from all of the patients. There were 45 girls (88%) and 6 boys, with a mean age at diagnosis of 16.3 months (range 3–62 months). Forty-seven hips had total dislocation and 13 had pronounced subluxation with femoral head coverage <50%. The treatment principles were preliminary traction followed by closed reduction under general anaesthesia and hip plaster spica for 6–9 months (the spica was changed every 3 months). Open reduction was necessary in three hips because closed reduction could not be achieved. The mean age at reduction was 18.7 months (range 4–65 months). As part of the initial treatment, early derotation osteotomy of the femur because of increased anteversion was performed within 3 years from the time of reduction in 28 patients (34 hips).
Because of residual subluxation, acetabular dysplasia or increased femoral anteversion, surgical intervention was performed later than 3 years after hip reduction in 22 patients (23 hips). The procedures were proximal femoral osteotomy, acetabular shelf operation according to Spitzy [11] and Salter pelvic osteotomy [9].
Radiographic evaluation
Conventional anteroposterior radiographs of the pelvis were taken with the patient in the supine position with the legs parallel, and it was aimed at avoiding rotation of the pelvis and hips. The following radiographs were used for measurements: those taken at the age of 8–10 years, those after skeletal maturity at the age of 15–20 years and the radiographs at the long-term follow-up. In addition, the radiographs prior to and about 1 year after the late surgical procedures were evaluated. The radiographic measurements were performed by one observer (paediatric orthopaedic surgeon) with more than 30 years experience in the evaluation of radiographs of hips in children and adults.
Two measurements were used for the assessment of subluxation and residual dysplasia. The migration percentage (MP) was measured according to Reimers [12]. If the MP is <33%, then the hip is located, and a range of 33–89% means subluxation. The centre-edge angle (CE angle) was measured according to Wiberg [4]. A CE angle <20° was classified as residual hip dysplasia.
The joint space width (JSW) was measured as the distance between the femoral head and the acetabular roof at three locations of the upper, weight-bearing part of the hip joint, according to Jacobsen and Sonne-Holm [13]. The minimum JSW was used for the diagnosis of OA. If the minimum JSW was outside the three standard locations, an additional measurement at the site of maximum narrowing was performed. OA was defined by a minimum JSW of <2.0 mm. Whereas radiographs in the standing position were used by Jacobsen and Sonne-Holm [13], supine radiographs were used in the present study. According to previous reports [14, 15], there is no significant differences according to patient positioning (standing or supine) in either the minimum JSW, CE angle or MP. Intra- and inter-observer studies of the radiographic parameters have shown satisfactory reproducibility and, thus, reliability of the present radiographic parameters [14, 16].
Statistics
Categorical data were analysed with Fisher’s exact test (OpenEpi, Version 2.3.1.). Otherwise, SPSS (version 16.0) was used for the statistics (SPSS Inc., Chicago, IL, USA). Taking into account that nine patients had bilateral affection, continuous radiographic data (MP and CE angle) were analysed with linear mixed models. Correlations were analysed with Pearson’s correlation coefficient. Differences were considered to be significant when the P-value was below 0.05.
Results
The mean follow-up period in patients who had not undergone total hip replacement (THR) was 44 years (range 42–47 years) and the average age at the most recent follow-up was 45 years (range 43–49 years). At the time of the last follow-up, OA had developed in ten hips and eight of these had undergone THR at a mean patient age of 40 years (range 32–47 years). There was a clear association (P < 0.001) between radiographic results at the last follow-up and OA as seen in the flowchart of the affected hips (Fig. 1). In hips without residual hip dysplasia (CE angle of 20° or higher), OA had occurred in only 2 out of 37 hips (5%; 95% confidence interval [CI] 1–18%). Dysplasia without subluxation (CE angle 10–19°), was seen in 18 hips, of which 14 hips had good outcome (Fig. 2) and four had OA (22%; 95% CI 6–48%). Subluxation was present in five hips (Fig. 3), of which four had OA (80%; 95% CI 28–99%). Hips with OA had significantly higher MP at the long-term follow-up than those without OA (30% vs. 22%; P = 0.001) and lower CE angle (13° vs. 24°; P < 0.001).
Fig. 1.
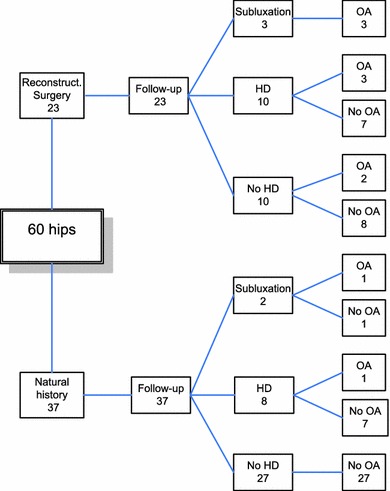
Flowchart of 60 hips, showing long-term outcome related to treatment and radiographic measurements. HD residual hip dysplasia, OA osteoarthritis
Fig. 2.
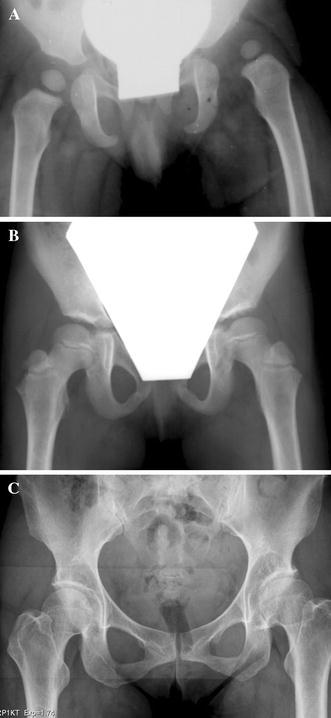
Radiographs of a girl with dislocation of her left hip. a Radiograph at the time of diagnosis at the age of 14 months. b Radiograph at the age of 9 years, showing acetabular dysplasia of the left hip with centre-edge (CE) angle 16° and migration percentage (MP) 25%. c Radiograph at the last follow-up at patient age 45 years, showing no osteoarthrosis in the left hip (CE angle 15° and MP 33%)
Fig. 3.
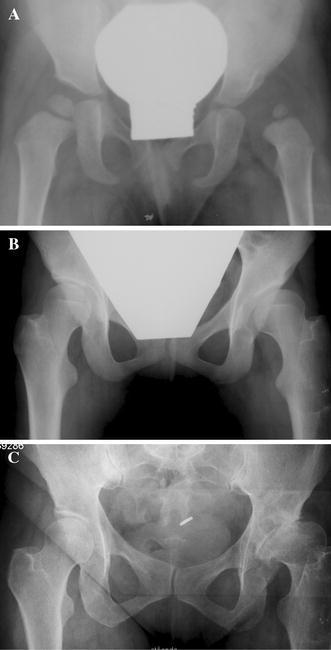
Radiographs of a girl with dislocation of her left hip. a Radiograph at the time of diagnosis at the age of 18 months. b Radiograph at skeletal maturity at the age of 15 years, showing subluxation of the left hip, with CE angle 8° and MP 38%. c Radiograph at the last follow-up at patient age 45 years, showing osteoarthrosis in the left subluxated hip (CE angle −1° and MP 45%)
The radiographic results did not significantly differ between hips without any type of surgery and those with early derotation osteotomy only. Thus, these 37 hips were combined and called the natural history group. Table 1 shows that the MP increased from age 8–10 years (18%) to skeletal maturity (25%; P < 0.001); thereafter, no significant change occurred. The mean CE angle was 23° at the age of 8–10 years and did not significantly change during the follow-up period. There was a clear association between the CE angle and the MP. At the final follow-up, the correlation coefficient was −0.93 (P < 0.001).
Table 1.
Radiographic measurements from age 8–10 years to 45 years; the results are mean (95% confidence interval)
| Patients | N | Migration percentage | CE angle | ||||
|---|---|---|---|---|---|---|---|
| 8–10 years | Maturity | Follow-up | 8–10 years | Maturity | Follow-up | ||
| Natural history | 37 | 18.1 (16–20) | 24.6 (22–26) | 22.7 (20–25) | 22.7 (20–25) | 23.5 (21–26) | 24.0 (22–26) |
| Late surgery | 23 | 22.3 (19–26) | 24.7 (21–29) | 24.2 (20–28) | 19.5 (16–23) | 20.6 (17–24) | 18.4 (15–22) |
| Osteoarthritis | 10 | 23.6 (17–31) | 28.6 (22–36) | 31.7 (24–39) | 17.7 (12–24) | 16.7 (11–23) | 12.1 (6–18) |
CE angle, centre-edge angle (°); N, number of hips; Natural history, hips with no late reconstructive surgery
Twenty-two patients (23 hips) underwent late reconstructive hip surgery at a mean age of 12 years (range 5–22 years). The indications for late surgical correction were residual subluxation in 17 hips, persisting acetabular dysplasia in seven and increased femoral anteversion or other reasons in three hips. Four patients were operated twice in the same hip. Proximal femoral osteotomy with varus and derotation was performed in 14 hips, acetabular shelf operation in 11 hips (combined with femoral osteotomy in two hips) and Salter type pelvic osteotomy in two hips. The mean preoperative MP was 33% and, 1 year postoperatively, it was 21%. The improvement in femoral head coverage was significantly better after the acetabular shelf procedures (mean 22%) than after femoral osteotomies (mean 5%; P < 0.001). Although femoral head coverage improved after reconstructive surgery in most of the patients, OA developed in 8 of 23 hips, which was significantly more frequent than in hips with no late surgery (P = 0.003).
The radiographic measurements at age 8–10 years, at skeletal maturity and at final follow-up for patients with late reconstructive surgery and for those with OA are are shown in Table 1. Neither the MP nor the CE angle changed during the follow-up period in patients with late reconstructive surgery. In patients with OA, the mean CE angle decreased and the MP increased from age 8–10 years to final follow-up, but the changes were not statistically significant (P = 0.102 and 0.062, respectively).
The clinical and radiographic data on each of the ten patients with OA are presented in Table 2. Eight of the hips had subluxation or acetabular dysplasia at skeletal maturity and at the last follow-up. One patient (no. 8) had a shelf operation at the age of 5 years, but the shelf was located too high and had no effect. After reoperation with shelf and femoral osteotomy at an age of 13 years, the femoral head coverage became normal, but, nevertheless, OA later developed. There was no significant difference in the mean age at THR between patients with subluxation (40.7 years) and those with residual dysplasia only (41.8 years).
Table 2.
Clinical and radiographic data of the ten patients with osteoarthritis
| N | Reconstructive surgery | MP | CE angle | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Type | Age | CE angle | 8–10 | 15–20 | F-up | 8–10 | 15–20 | F-up | ||
| Pre | Post | |||||||||
| 1 | FO | 21 | 24 | 27 | 19 | 15 | 19 | 20 | 27 | 22 |
| 2 | 18 | 28 | 32 | 24 | 19 | 15 | ||||
| 3 | Shelf | 7 | 8 | 16 | 24 | 46 | 41 | 16 | 2 | 0 |
| 4 | Salter | 11 | 11 | 11 | 34 | 44 | * | 9 | 3 | * |
| 5 | 30 | 36 | 41 | 12 | 15 | 8 | ||||
| 6 | FO | 11 | 12 | 13 | 30 | 38 | 45 | 12 | 8 | −1 |
| 7 | Shelf | 6 | 7 | 24 | 9 | 20 | 22 | 24 | 23 | 19 |
| 8 | Shelf + FO | 5 | 3 | 12 | ||||||
| Shelf + FO | 13 | 0 | 37 | 32 | 8 | 21 | 12 | 28 | 22 | |
| 9 | Shelf | 7 | 7 | 32 | 12 | 27 | 27 | 32 | 17 | 16 |
| 10 | FO | 16 | 25 | 25 | 28 | 24 | 28 | 16 | 25 | 16 |
N, patient number; MP, migration percentage (%); CE angle, centre-edge angle (°); 8–10, age 8–10 years; 15–20, age 15–20 years; F-up, final follow-up; pre, preoperative; post, 1 year postoperative; FO, varus femoral osteotomy; Shelf, acetabular shelf operation; Salter, Salter pelvic osteotomy; * (asterisk), preoperative radiograph prior to total hip replacement (THR) not available
Discussion
Previous studies have shown an association between residual hip dysplasia and OA [1, 4–6, 13]. Wiberg [4] followed 17 hips with acetabular dysplasia or subluxation and reported that all eventually developed OA. The age was related to the degree of pathology, as the mean age at diagnosis of OA in women was 41 years in hips with subluxation and 53 years in those with acetabular dysplasia without subluxation. Murphy et al. [7] studied 286 patients who had undergone unilateral THR because of OA secondary to hip dysplasia. At long-term follow-up, OA had developed in most of the contralateral hips and the mean CE angle in hips with OA was 7°, compared with 34° in hips without OA. No hip in the group without OA had a CE angle <16° or MP over 31%.
Long-term studies of patients previously treated for late-detected DDH have confirmed that residual subluxation is an important risk factor for later OA [2, 8]. Hartofilakidis et al. [17] followed the natural history of patients with subluxation (42 hips) who had not received any previous treatment. All hips except two had undergone THR by the final follow-up, and the mean age at surgery was 51 years. In the present study 4 out of 5 hips with subluxation at maturity developed OA during 45 years of follow-up. Since subluxation clearly leads to OA, such hips should be considered for corrective surgery during childhood or adolescence. Acetabular osteotomy with or without femoral osteotomy to correct femoral anteversion or increased valgus are reasonable treatment alternatives.
Compared with subluxation, the association between residual dysplasia and OA is weaker. Cooperman et al. [6] followed 20 patients (32 hips) with acetabular dysplasia but without subluxation. Almost all of the patients developed OA. Their results differed from those of Wiberg [4], because there was no clear relationship between the grade of dysplasia (CE angle) and the age at occurrence of OA. Since nine of their patients were OA-free at the age of 50–60 years, they concluded that acetabular dysplasia leads to OA, but the process may take decades to show evidence. Hartofilakidis et al. [17] found a mean age at medium-degree OA of 44 years (range 34–50 years) in individuals with acetabular dysplasia who had not had any previous treatment and a mean age of 55 years (range 34–75 years) at severe grade of OA. Thus, the patients have to be followed at least until over the age of 40 years to provide reliable data on the prevalence of OA.
The present results showed that 14 out of 18 hips with CE angle between 10° and 20° did not develop OA during 45 years of follow-up. Even if the remaining hips developed OA, this might also have occurred if they had undergone surgery. Thus, reconstructive surgery in asymptomatic hips with CE angles in the range 10° to 19° is barely indicated. Whether or not symptomatic hips in this range should be recommended for surgery is a difficult evaluation because long-term studies to prove the effect are lacking. Although very good results after pelvic osteotomy was reported at 10–15 years postoperatively [9], the results deteriorated with longer follow-up and, at patient age 43 years, the survival rate (hips without THR) was only 54% [10]. The present results showed that reconstructive surgery is not a guarantee for good long-term outcome, since 8 out of 23 hips with such surgery developed OA. Newer pelvic osteotomy techniques will probably improve the results of reconstructive surgery but, so far, follow-up beyond 20 years is lacking [18].
Already in 1939, Wiberg [4] pointed out that a certain arbitrariness characterises the determination of whether or not an acetabulum is normal. He described the CE angle and considered a CE angle above 25° as normal, angles below 20° as abnormal and angles in the range 20–25° as “borderline”. The limit of 20° has been used in most later studies [5, 6], as well as in the present study. In a cross-sectional survey of 4,151 individuals in Copenhagen, Jacobsen and Sonne-Holm [13] found a mean CE angle for women and men combined of 34.6° (standard deviation [SD] 7.7). The lower limit of normalcy, defined as mean −2SD, was 19.2°. This supports that 20° is an appropriate lower limit of the normal range. A few studies have used 25° as the lower limit [19, 20], which is hardly adequate because many normal hips will then be included in the pathologic group and the prevalence of hip dysplasia will be too high.
Wiberg [4] did not use the CE angle to distinguish between mere dysplasia and subluxation. He recommended an interrupted Shenton’s line as the sign of subluxation. Shenton’s line has also been used by others, but some allowed a 5-mm discrepancy as the border of subluxation [6, 13], whereas others used a 10-mm discrepancy [21]. Scoles et al. [22] regarded Shenton’s line difficult to measure in children and found the measurements not to be accurate. Measurement of the femoral head coverage is probably a more reliable criterion than Shenton’s line in the distinction between subluxation and mere acetabular dysplasia.
Femoral head coverage, or the acetabulum-head index as it was originally called by Heyman and Herndon [23], is an easy and reproducible measurement [24]. Heyman and Herndon [23] reported a mean coverage of 90% and considered 70% to be the lower limit of the normal range, corresponding to 30% of the femoral head outside the acetabulum. Reimers [12] used the term “migration percentage” for the same measurement and recommended 33% as the limit of subluxation. In the Copenhagen study, 25% was used as the cut-off value between normal hips and hip dysplasia [13]. Eklöf et al. [25] found a 98th percentile of 24% in normal adolescents. Thus, it is reasonable to use 25% as the upper normal limit of MP and 33% as the limit between dysplasia and subluxation. There is a close relationship between the CE angle and the MP, as shown in this study. MP values above 33% correspond well with CE angles of <10°, which supports this cut-off value to be used for subluxation. Although this may be disputed, a cut-off of 10° is suitable to distinguish between slight to moderate dysplasia (CE 10–19°) and more severe dysplasia, especially in hips without marked enlargement of the femoral head.
Do the CE angle and MP change with patient age? Angliss et al. [2] found that the femoral head congruency worsened over time from 2 to 33 years after reduction. There were 30 hips graded as acetabular dysplasia at the age of 5 years, which had subluxated at final review and two that had dislocated. A trend towards deterioration with time was noted by Malvitz and Weinstein [8], but the change was not significant. In the present study, the natural history in hips without late reconstructive surgery showed a moderate increase in MP from age 8–10 years to skeletal maturity and no change later, whereas the CE angle did not change significantly during the whole period. In hips that developed OA, there was a decrease in head coverage from age 8–10 years to the last follow-up, but the change was relatively small, since the CE angle decreased by only 5°. This indicates that hips with normal head coverage during childhood and at skeletal maturity rarely deteriorate. In hips with residual dysplasia and subluxation, however, a decrease in head coverage may occur during long-term follow-up and contributes to the worse prognosis in these hips.
Conclusion and significance
Hip dysplasia without subluxation has a relatively good prognosis and hardly needs surgical correction. Subluxation is a clear risk factor of osteoarthritis (OA). Children and adolescents with migration percentage (MP) above 33% and centre-edge (CE) angle under 10° should be evaluated for surgery in order to improve femoral head coverage and, hopefully, avoid long-term OA.
References
- 1.Albinana J, Dolan LA, Spratt KF, Morcuende J, Meyer MD, Weinstein SL. Acetabular dysplasia after treatment for developmental dysplasia of the hip. Implications for secondary procedures. J Bone Joint Surg Br. 2004;86:876–886. doi: 10.1302/0301-620X.86B6.14441. [DOI] [PubMed] [Google Scholar]
- 2.Angliss R, Fujii G, Pickvance E, Wainwright AM, Benson MKD. Surgical treatment of late developmental displacement of the hip. Results after 33 years. J Bone Joint Surg Br. 2005;87:384–394. doi: 10.1302/0301-620X.87B3.15247. [DOI] [PubMed] [Google Scholar]
- 3.Terjesen T, Halvorsen V. Long-term results after closed reduction of late-detected hip dislocation: 60 patients followed up to skeletal maturity. Acta Orthop. 2007;78:236–246. doi: 10.1080/17453670710013744. [DOI] [PubMed] [Google Scholar]
- 4.Wiberg G. Studies on dysplastic acetabula and congenital subluxation of the hip joint. Acta Chir Scand. 1939;83(Suppl 58):7–135. [Google Scholar]
- 5.Stulberg SD, Harris WH (1974) Acetabular dysplasia and development of osteoarthritis of the hip. In: Harris WH (ed) The hip. Proceedings of the Second Open Scientific Meeting of the Hip Society. Mosby, St. Louis, MO, pp 82–93
- 6.Cooperman DR, Wallensten R, Stulberg SD. Acetabular dysplasia in the adult. Clin Orthop Relat Res. 1983;175:79–85. [PubMed] [Google Scholar]
- 7.Murphy SB, Ganz R, Müller ME. The prognosis in untreated dysplasia of the hip. A study of radiographic factors that predict the outcome. J Bone Joint Surg Am. 1995;77:985–989. doi: 10.2106/00004623-199507000-00002. [DOI] [PubMed] [Google Scholar]
- 8.Malvitz TA, Weinstein SL. Closed reduction for congenital dysplasia of the hip. Functional and radiographic results after an average of thirty years. J Bone Joint Surg Am. 1994;76:1777–1792. doi: 10.2106/00004623-199412000-00004. [DOI] [PubMed] [Google Scholar]
- 9.Salter RB, Dubos JP. The first fifteen year’s personal experience with innominate osteotomy in the treatment of congenital dislocation and subluxation of the hip. Clin Orthop Relat Res. 1974;98:72–103. doi: 10.1097/00003086-197401000-00009. [DOI] [PubMed] [Google Scholar]
- 10.Thomas SR, Wedge JH, Salter RB. Outcome at forty-five years after open reduction and innominate osteotomy for late-presenting developmental dislocation of the hip. J Bone Joint Surg Am. 2007;89:2341–2350. doi: 10.2106/JBJS.F.00857. [DOI] [PubMed] [Google Scholar]
- 11.Spitzy H. Künstliche pfannendachbildung. Z Orthop. 1924;43:284–294. [Google Scholar]
- 12.Reimers J (1980) The stability of the hip in children: a radiological study of the results of muscle surgery in cerebral palsy. Acta Orthop Scand 51(Suppl 184):4–91 [DOI] [PubMed]
- 13.Jacobsen S, Sonne-Holm S. Hip dysplasia: a significant risk factor for the development of hip osteoarthritis. A cross-sectional survey. Rheumatology (Oxford) 2005;44:211–218. doi: 10.1093/rheumtology/keh436. [DOI] [PubMed] [Google Scholar]
- 14.Terjesen T, Gunderson RB (2011) Reliability of radiographic parameters in adults with hip dysplasia. Skel Radiol (accepted for publication) [DOI] [PubMed]
- 15.Troelsen A, Jacobsen S, Rømer L, Søballe K. Weightbearing anteroposterior pelvic radiographs are recommended in DDH assessment. Clin Orthop Relat Res. 2008;466:813–819. doi: 10.1007/s11999-008-0156-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Troelsen A, Rømer L, Kring S, Elmengaard B, Søballe K. Assessment of hip dysplasia and osteoarthritis: variability of different methods. Acta Radiol. 2010;51:187–193. doi: 10.3109/02841850903447086. [DOI] [PubMed] [Google Scholar]
- 17.Hartofilakidis G, Karachalios T, Stamos KG. Epidemiology, demographics, and natural history of congenital hip disease in adults. Orthopedics. 2000;23:823–827. doi: 10.3928/0147-7447-20000801-16. [DOI] [PubMed] [Google Scholar]
- 18.Steppacher SD, Tannast M, Ganz R, Siebenrock KA. Mean 20-year followup of Bernese periacetabular osteotomy. Clin Orthop Relat Res. 2008;466:1633–1644. doi: 10.1007/s11999-008-0242-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Goker B, Sancak A, Haznedaroglu S. Radiographic hip osteoarthritis and acetabular dysplasia in Turkish men and women. Rheumatol Int. 2005;25:419–422. doi: 10.1007/s00296-004-0473-x. [DOI] [PubMed] [Google Scholar]
- 20.Reijman M, Hazes JMW, Pols HAP, Koes BW, Bierma-Zeinstra SMA. Acetabular dysplasia predicts incident osteoarthritis of the hip: the Rotterdam study. Arthritis Rheum. 2005;52:787–793. doi: 10.1002/art.20886. [DOI] [PubMed] [Google Scholar]
- 21.Hasegawa Y, Iwata H, Mizuno M, Genda E, Sato S, Miura T. The natural course of osteoarthritis of the hip due to subluxation or acetabular dysplasia. Arch Orthop Trauma Surg. 1992;111:187–191. doi: 10.1007/BF00571474. [DOI] [PubMed] [Google Scholar]
- 22.Scoles PV, Boyd A, Jones PK. Roentgenographic parameters of the normal infant hip. J Pediatr Orthop. 1987;7:656–663. doi: 10.1097/01241398-198707060-00005. [DOI] [PubMed] [Google Scholar]
- 23.Heyman CH, Herndon CH. Legg–Perthes disease; a method for the measurement of the roentgenographic result. J Bone Joint Surg Am. 1950;32:767–778. [PubMed] [Google Scholar]
- 24.Wiig O, Terjesen T, Svenningsen S. Inter-observer reliability of radiographic classifications and measurements in the assessment of Perthes’ disease. Acta Ortop Scand. 2002;73:523–530. doi: 10.1080/000164702321022794. [DOI] [PubMed] [Google Scholar]
- 25.Eklöf O, Ringertz H, Samuelsson L. The percentage of migration as indicator of femoral head position. Acta Radiol. 1988;29:363–366. doi: 10.1177/028418518802900320. [DOI] [PubMed] [Google Scholar]


