Abstract
This report explores the level of detailed knowledge about the Tuskegee Syphilis Study (TSS) among 848 Blacks and Whites in three U.S. cities across an array of demographic variables. The Tuskegee Legacy Project (TLP) Questionnaire was used, which was designed to explore the willingness of minorities to participate in biomedical studies. A component of the TLP Questionnaire, the TSS Facts & Myths Quiz, consisting of seven yes/no factual questions, was used to establish respondents’ level of detailed knowledge on the TSS. Both Blacks and Whites had similar very low mean quiz score on the 7-point scale, with Blacks’ scores being slightly higher than Whites (1.2 vs. 0.9, p = .003). When analyzing the level of knowledge between racial groups by various demographic variables, several patterns emerged: (a) higher education levels were associated with higher levels of detailed knowledge and (b) for both Blacks and Whites, 30 to 59 years old knew the most about TSS compared with younger and older adult age groups. The findings show that much of the information that circulates in the Black and White communities about the TSS is false, often minimizing or understating the most egregious injustices that occurred. Health promotion and educational implications of these findings are offered and conclude that the findings should be used as a catalyst to explore local realities and sentiments regarding participation in biomedical research within the research philosophy and framework of community-based participatory research.
Keywords: Tuskegee Syphilis Study, detailed knowledge between racial groups, community-based participatory research, African American, biomedical research, minorities, Blacks, health promotion
Introduction
It is widely acknowledged that the U.S. Public Health Service Syphilis Study at Tuskegee, which was conducted over a 40-year period from 1932 to 1972, is the most infamous biomedical research study in U.S. history because of the research abuses that occurred in that study (Bates & Harris, 2004; Corbie-Smith, Thomas, Williams, & Moody-Ayers, 1999; Fletcher, 2000; Jones, 1981; Shavers, Lynch, & Burmeister, 2000). A total of 399 Black sharecroppers from Macon County, Alabama who had syphilis were studied to investigate the “untreated” progression of syphilis by researchers from the U.S. Public Health Service.
From 1972 (when the Tuskegee Syphilis Study [TSS] was made public in newspapers and terminated) to 2005, there were many published articles that discussed the “legacy of the TSS,” namely, that Blacks are more reluctant to participate in clinical trials and other research studies because of the abuses within the TSS. All these articles on the “legacy of the TSS” were written from a purely legal, historical, ethical, or access to care perspective (Benedek, 1978; Bouleware, Cooper, Ratner, LaVeist, & Powe, 2003; Brandon, Isaac, & LaVeist, 2005; Caplan, 1992; Corbie-Smith, 2004; Fairchild & Bayer, 1999; Gamble, 1993, 1997; Matthews, Sellergren, Manfredi, & Williams, 2002; Pressel, 2003; Rathore & Krumholz, 2003; Shavers-Hornaday, Lynch, Burmeister, & Torner, 1997; White, 2005), rather than being based on any empirical data. Two 2006 reports on this topic found only five studies that provided quantified data that compared Blacks and Whites on self-reported willingness to participation in research studies relative to the TSS and reported on the major limitations of these studies (Katz et al., 2006; McCallum, Arekere, Green, Katz, & Rivers, 2006).
Recently, several articles have been published from the Tuskegee Legacy Project, a study funded by the National Institute of Dental Craniofacial Research (NIDCR) at the National Institutes of Health (NIH) to primarily study the “legacy” from an empirical perspective. Five of these articles provide the first direct empirical data on this widely discussed “legacy” (Katz et al., 2006; Katz et al., 2007; Katz et al., 2009; Katz, Green, et al., 2008; Katz, Kegeles, et al., 2008). These articles report that (a) despite having greater fear of participating in research studies, Blacks were just as likely as Whites to self-report willingness to participate in biomedical research (Katz et al., 2006; Katz, Green, et al., 2008); (b) Blacks were two to three times more likely than Whites to be willing to participate in biomedical studies despite having heard of the TSS or the Presidential Apology (Katz, Kegeles, et al., 2008); and (c) that there was no support for the widely held notion of the “legacy” of the TSS that Blacks were more reluctant than Whites to participate in biomedical research because of their awareness of the TSS (Katz, Green, et al., 2008; Katz et al., 2009).
Whereas the latter cited paper focused on detailed knowledge of the TSS for the overall population as a whole and on the development of a classification schema for the openended responses, this report simply continues this line of investigation into detailed knowledge of the TSS. Specifically, this report (a) explores the level of detailed knowledge about the TSS in Blacks and Whites within specific strata of those demographic variables such as age, education, and income and (b) presents the health promotion and educational implications derived from those demographic analyses.
Method
The Tuskegee Legacy Projects (TLP) Questionnaire, the principal research instrument for this study, was developed between 1994 and 1997 by a multidisciplinary, multiuniversity research team within the Northeastern Minority Oral Health Research Center (NMOHRC), an NIDCR/NIH Regional Research Center for Minority Oral Health. The TLP Questionnaire concentrated on a range of issues related to the recruitment of minorities into biomedical studies and was administered, via random-digit dial telephone interviews, to adults in four U.S. cities: Tuskegee, AL; Birmingham, AL; Hartford, CT; and San Antonio, TX.
The selection of each of the four cities was based on the history of TSS, practical, regional, and demographic contributions the inclusion of each city would offer to the investigation. Tuskegee, AL, the epicenter of the infamous study, was chosen because of its historical significance. A similar rationale led to the selection of Birmingham, AL, the next closest major city. In addition to its proximity to Tuskegee, Birmingham was also chosen because of its demographic composition, which at the time of the investigation consisted primarily of Blacks (74.0%). Hartford, CT, was selected to allow for the consideration of regional cultural differences and because of demographic and economic similarities with Birmingham; its population, then, primarily consisted of Blacks and Hispanics (53.2% and 46.8%, respectively). When the survey was implemented, both Birmingham and Hartford were mid-sized cities (population 265,000 and 140,000, respectively), and both cities had similar poverty and unemployment rates among Black residents. Additionally, these cities were chosen because each had a major medical center and thus, the population was typical of a city where residents would likely be invited to participate in medical studies. The city of San Antonio was selected because it was identified as the city that would yield the highest rate of Mexican American participants, facilitating an intra-Hispanic group comparison with the large number of Puerto Ricans in Hartford. Additionally, it is also home to a major medical center.
The findings of this report were based on the data from three of the four cities (Tuskegee, Birmingham, and Hartford), as San Antonio data were excluded from this report on Black versus White respondents because there were only 16 Black participants in San Antonio. This study was approved by the Institutional Review Boards of the University of Connecticut Health Center and New York University.
The random-digit dial interviews for this study were administered by the Survey Research Unit of the University of Alabama at Birmingham between March 1999 and November 2000. The priority population was noninstitutionalized individuals 18 years or older living in households with working telephones in the targeted cities. This was based on a simple random sampling of telephone numbers using the three-digit telephone exchanges for those local calling areas with partial screening for nonworking or business numbers. Unresolved numbers were dropped after 20 attempts. A total of 13 interviewers were trained with full computer-assisted telephone interviewing technology and supervised at all times. Random electronic monitoring was also conducted a minimum of four times per month throughout the study.
Though the data that provide the basis for this analysis are nearly 10 years old, it remains relevant. A thorough literature search revealed no subsequent, or prior, investigation that explored the impact of TSS in similar detail. Thus, these data from the TLP continue to fill a gap in the literature and can still inform health disparity and public health investigators about future medical research and recruitment efforts in the Black community.
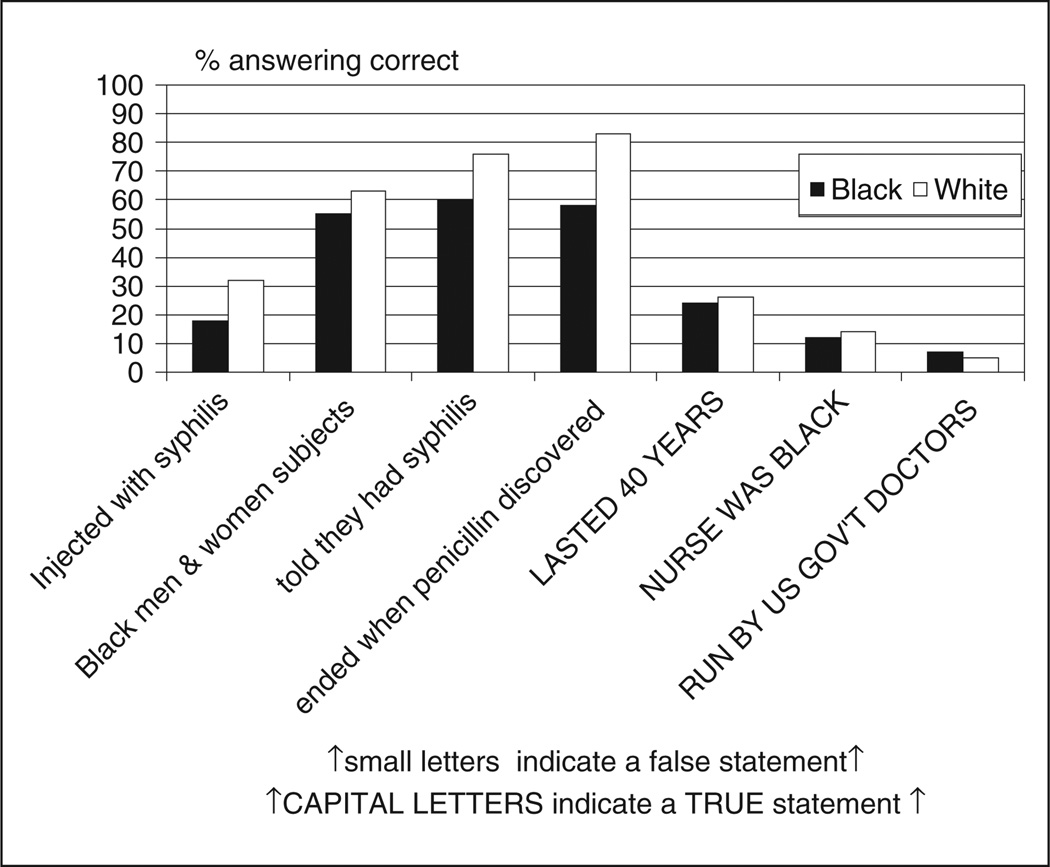
The TLP questionnaire contains 60 items, including demographic questions, in addition to the TSS Facts & Myths Quiz, which was used as the main approach to compare the level of detailed knowledge between Blacks and Whites. This quiz had seven yes/no factual questions about the TSS, identifying some of the major facts and myths associated with it. Table 1 lists the seven questions and explains which questions represent statements of fact or myth. A total TSS Facts & Myths score was calculated for each respondent based on assigning one point per correctly answered question to rate how much detailed knowledge a respondent possesses; hence, the range of possible scores for the TSS Facts & Myths Quiz was from 0 to 7. Figure 1 shows the unadjusted percents of those answering correctly for each question by race. An a priori categorization schema was created to assign participants into the four detailed knowledge categories based on quiz score ranging from “no knowledge” to “high knowledge,” as shown in Table 1. Two screening questions were used to identify those individuals who had heard about the TSS, and the TSS Facts & Myths Quiz items were only asked of that subset of respondents who indicated that they had, if in fact, heard of the TSS study. However, for all analysis in this report, respondents who indicated that they had not heard of the TSS were included in the “no knowledge” category since that is their appropriate categorization, and to omit them from the analyses would lead to a serious underestimation of the number and percentage of respondents in these communities who possessed no knowledge of the TSS. In a conservative methodological decision, all respondents who answered “don’t know/not sure” to the two lead-in questions on whether they had “ever heard of the TSS” (only n = 4 or 0.5% of the 848 respondents) were treated as missing values.
Table 1.
Questions of the Detailed Knowledge and Categories of the Knowledge Scores for the Tuskegee Syphilis Study
Questions of the detailed knowledge regarding Tuskegee Syphilis Studya
|
Categories of the knowledge scores:
|
Statements in capital letters indicate a true statement.
Figure 1.
The percentage of respondents by race who gave correct answers to the seven items on the Tuskegee Syphilis Study (TSS) Facts & Myths Quiz among those who “had heard” of the TSS (n = 565)
The statistical analysis was designed to determine if Blacks and Whites differed from each other on the detailed knowledge levels of the TSS. First, unadjusted bivariate chi-squared analyses were performed to examine the frequency distributions. Analyses of covariance (ANCOVA) was followed to test a model with race/ethnicity (Blacks vs. Whites) as the independent variable and mean detailed knowledge scores as the dependent variable, adjusting for age, gender, education, and income, as well as city of residence. The statistical significance levels for all analyses used an alpha level set at ≤.05 and were conducted using either SPSS version 15.0 or SAS version 9.0 data analysis software.
Results
The TLP Questionnaire was administered to 1,133 adult Blacks, Puerto Rican Hispanics, Mexican American Hispanics, and Whites in four city/county areas: Birmingham/Jefferson County, AL; Tuskegee/Macon County, AL; Hartford/Hartford County, CT; and San Antonio/Bexar County, TX. Response rates from each city were 70%, 65%, 49%, and 50%, respectively. Of the 1,133 individuals who participated in the four-city TLP survey, the responses of all 848 Black and White respondents from Birmingham, AL, Tuskegee, AL, and Hartford, CT formed the basis for this analysis.
Table 2 shows the mean values or percentage of frequency distributions for each demographic variable listed by race. The only statistically significant differences by race for personal demographic characteristics were education and income, with Whites having more education and higher income than Blacks. Table 2 also shows the percentage of respondents who reported awareness of the TSS and adjusted mean TSS Facts & Myths Quiz scores for each racial group. Although the mean scores for each racial group was low on the 0- to 7-point scale, Blacks did have a slightly higher adjusted mean quiz score than did Whites (1.2 vs. 0.9, p = .003).
Table 2.
Demographic Characteristics by Race, Age, Gender, Education, Income Level, and Cities for the 848 Black and White Respondents
| Blacks (n = 337) | Whites (n = 511) | |
|---|---|---|
| Age in years (mean ± SD) | 49.0 ± 16.4 | 54.1 ± 16.7 |
| Gender (%); p = .765 | ||
| Male | 51.9 | 50.9 |
| Education level (%); p = .000 | ||
| <High school | 21.7 | 13.1 |
| High school graduate | 60.4 | 51.9 |
| College graduate or higher | 17.9 | 35.0 |
| Income level (%); p = .000 | ||
| <$20,000 | 42.7 | 21.9 |
| $20,000–74,999 | 52.2 | 56.8 |
| ≥$75,000 | 5.1 | 21.3 |
| Location (%); p = .003 | ||
| Hartford | 37.7 | 43.4 |
| Tuskegee | 31.5 | 36.0 |
| Birmingham | 30.9 | 20.5 |
| Reported awareness of Tuskegee Syphilis Study (%) | 75.0 | 60.0 |
| Adjusted mean detailed knowledge score; p = .0027 | 1.16 | 0.86 |
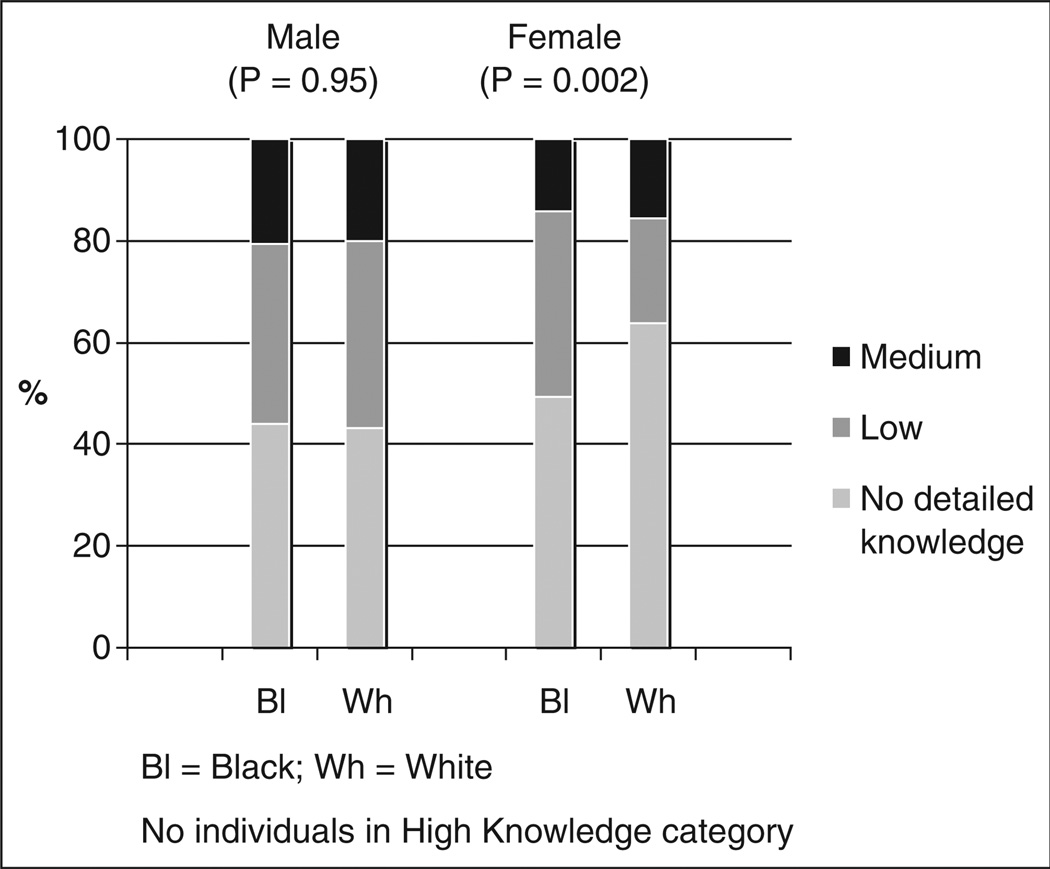
Level of detailed knowledge was examined by race and demographic characteristic. First, it should be noted that no respondents were categorized as having “high knowledge” in any race or demographic characteristic group, as no respondents had >5 correct answers to the Fact & Myth Quiz. Figure 2 shows the unadjusted distribution of the detailed knowledge levels between Blacks and Whites by gender. Overall, males, as compared with females, showed a slightly higher level of knowledge (fewer in “no detailed knowledge” category, and more in the “medium detailed knowledge” category), but these observed differences were not statistically significant. However, the largest observed (and only statistically significant) difference, as seen in Figure 2, was that Black females showed higher levels of detailed knowledge than White females; almost two thirds of White females (63.7%) had no detailed knowledge of TSS compared with just under half (49.4%) for Black females (p = .002).
Figure 2.
Distribution of detailed knowledge scores by race: males versus females (n = 848)
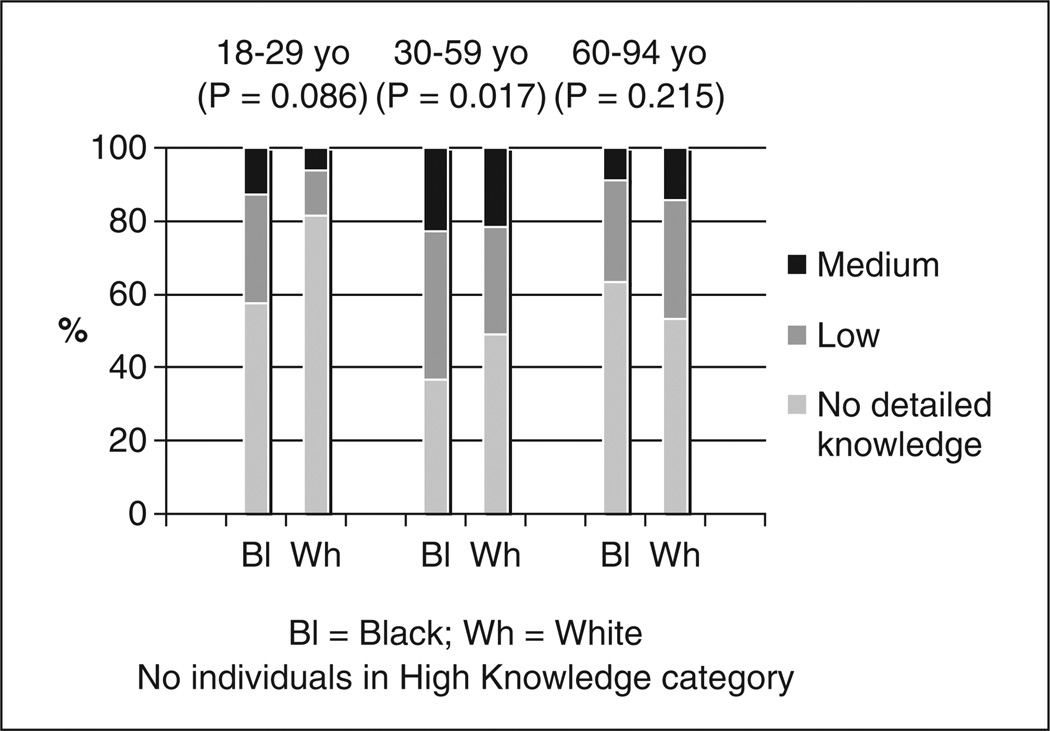
The unadjusted distribution of the detailed knowledge levels between Blacks and Whites across the three age groups is shown in Figure 3. Overall, the middle-aged adults (30–59 years old) had the highest level of detailed knowledge with more than 50% of Blacks and Whites categorized as having low or medium detailed knowledge. On the other hand, the reverse was observed for the other two age groups; that is, the majority of younger adults (18–29 years old) and of older adults (60–94 years old) were categorized as having “no detailed knowledge” of the TSS, irrespective of race. As for differences between races, the biggest observed difference was between younger adults where Blacks were twice as likely as Whites to have low or moderate levels of detailed knowledge about the TSS (~40% vs. ~20%, p = .09). This finding of higher detailed knowledge in Blacks than in Whites, albeit much more muted and at a lower overall level of detailed knowledge was also observed in middle-aged adults (p = .02), but this trend, still muted, was reversed in the 60- to 94-year-olds (p = .22).
Figure 3.
Distribution of detailed knowledge scores by race: young adults versus middle-aged adults versus older adults (n = 848)
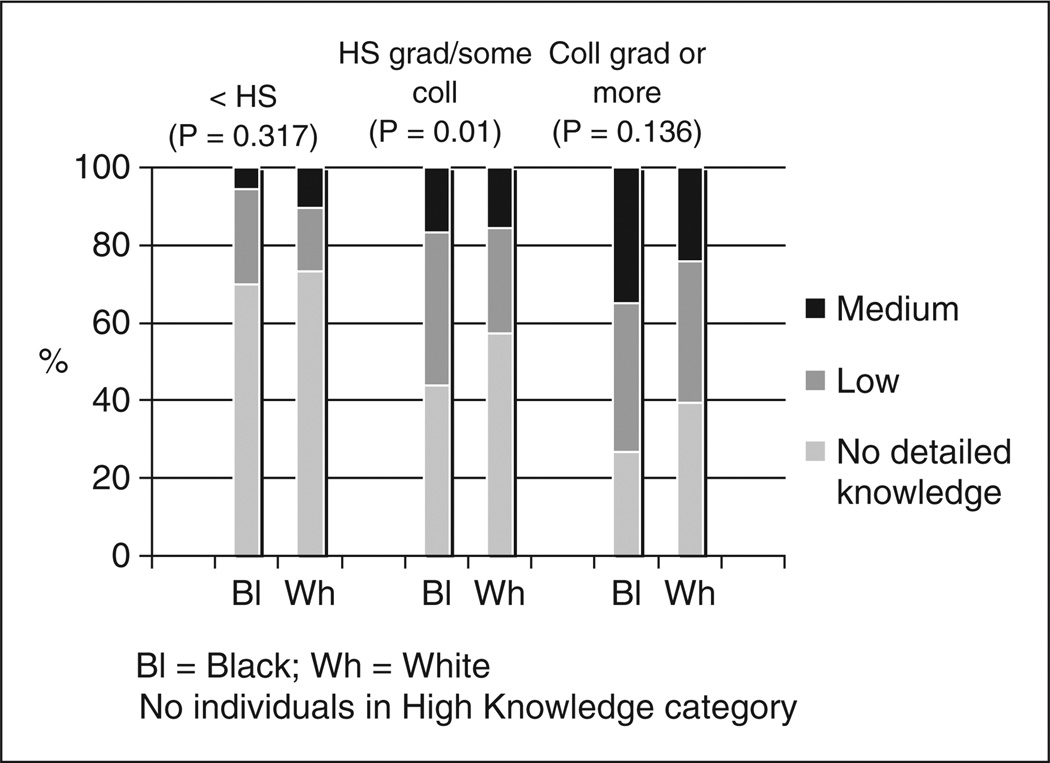
When analyzed by education level (see Figure 4), three observations are evident. First, the higher the educational level, the greater the detailed knowledge about the TSS, albeit not at a statistically significant level (p = .14), irrespective of race. Second, the overall pattern by race across educational levels was that Blacks consistently had a slightly higher level of detailed knowledge than Whites. Last, the only statistically significant finding on detailed knowledge about the TSS between Blacks and Whites was found in the moderate educational level category (i.e., the group who were high school graduates or had some college) with Blacks more likely to have low or medium detailed knowledge scores than Whites (56.3% vs. 42.7%, p = .01).
Figure 4.
Distribution of detailed knowledge scores by race: low versus moderate versus high educational levels (n = 848)
While the analyses between Blacks and Whites by income level revealed no statistically significant differences, the trends for income level were the same as found for educational level. It was found that although Blacks indicated a higher level of detailed knowledge overall for each level of income (<$20,000; $20,000–74,999; and ≥$75,000), the majority of both Blacks and Whites were in the “no detailed knowledge” category for each of the three income levels.
Discussion
It has been a long-held belief (i.e., the oft-referred to “legacy of the Tuskegee Syphilis Study”) that many people in the Black community have heard of the Tuskegee Syphilis Study, and, because of their knowledge of the study, their levels of participation in research studies has historically been lower compared with other populations (Bates & Harris, 2004; Corbie-Smith et al., 1999; Shavers et al., 2000). In the absence of any specific supporting data prior to 2006, this widely held belief appears to have been based solely on either anecdotal information or just a “gut feeling.” Only since 2006 have published studies directly assessed this long-held belief about this “legacy” of the TSS, with all four publications from the two surveys (one in 1999–2000 and one in 2003) reporting no detectable differences observed in the likelihood of participating in biomedical studies between racial and ethnic groups and no relationship between knowledge of the TSS and willingness to participate in biomedical research for either Blacks or Whites (Katz et al., 2006; Katz et al., 2007; Katz et al., 2009; Katz, Green, et al., 2008).
The goal of this report was to examine the detailed knowledge about the TSS data from the first of those two surveys at a deeper level (i.e., a stratified analysis by age, gender, education, and income within racial groups) rather than just as a sample-of-the-whole, adjusted for those demographic variables within racial groups or just analyzing detailed knowledge and its impact on willingness to participate, as was done in those prior publications (Katz et al., 2006; Katz, Green, et al., 2008). Detailed knowledge was estimated by totaling the correct answers for each question on the TSS Facts & Myths Quiz, which gave the best measure of detailed knowledge. The most salient of the findings from this more detailed stratified analysis was the lack of detailed knowledge of the TSS within both Blacks and Whites. Out of the seven most common facts associated with the study, Black respondents, on average, gave slightly more than one correct answer (1.2) whereas White respondents gave less than one correct answer on average (0.9). The adjusted mean is reported because adjusted results show usefulness related to a long-term, more detached “controlled scientific understanding” of the factors that affect any observed differences across race/ethnicity (Katz, Claudio, et al., 2008). Though stratified bivariate analysis did indicate that although specific demographic subgroups had differing knowledge of the TSS, most participants regardless of race knew very few factual details about the TSS.
With approximately 75% of Blacks and 60% of Whites in this study self-reporting awareness of TSS (i.e., they self-reported having heard of the TSS), one might have expected to find higher levels of detailed knowledge about the TSS event. However, our findings suggest that although many people, both Black and White, are aware of the TSS (i.e., they have heard of the TSS) a much smaller subset appear to know any factual details about the TSS, and even in that subset very few knew more than one factually correct detail. Given that the TSS is rarely, if ever, used as a rationale to explain the participation of Whites in biomedical research, then the question is can these findings meaningfully contribute to discussions of the impact of TSS on the Black community, as it is frequently cited as the reason for the underrepresentation of Blacks in biomedical research as well as for the broader mistrust of health care and health care providers.
It is clear that information about the TSS has circulated in the Black community, as 3 out of every 4 Black participants in this TLP study indicated that they had heard of the study. However, much of this information that is shared must be factually incorrect based on the findings of this study. Interestingly enough, this does not imply that the misinformation vilifies biomedical research; on the contrary, some of the misinformation—as reported by the respondents—misses or covers up some of the most egregious injustices that actually occurred in the TSS. For example, as reported previously on this TLP study, which examines in more detail the correct responses for each question (Katz, Green, et al, 2008), Blacks were significantly more likely than Whites to misstate that the subjects in the TSS were “told that they had syphilis” and that the study “ended when penicillin” became available. Additionally, though the majority of respondents, both Blacks and Whites (this latter fact for Whites previously unreported and unknown) believed that the men were injected with syphilis, they also believed that the doctors involved in the study were not affiliated with the government. Thus, misinformation can potentially add to and distract from the potency and poignancy of the TSS. Whether information about TSS is fact or myth, it appears that it is shared in the Black community at an extremely high frequency, and the simple reality of exchange speaks to the social power of the study.
The most obvious or simplest solution to the misinformation would be to go into communities and correct the misinformation about the TSS. This would certainly lead to increasing the knowledge levels of community members. However, this approach of merely educating the community about the accurate details of the TSS would miss a very important strategy of addressing more localized issues of distrust and skepticism. In other words, the broader scope of these findings may not lie in how accurate the circulation of details of the study are, but rather in how this misinformation has potential to be a powerful and influential cause of distrust and skepticism about local experiences and stories in the community. This local distrust and skepticism may have an effect on health behavior and biomedical research participation rates more than merely having inaccurate knowledge of TSS. Developing strategies that would allow for the exchange of information about the TSS between researchers and the community would be warranted. Therefore, education in the form of simply offering the facts of the TSS or simply seeking to debunk myths associated with the study is not enough to dispel real and perceived injustices formed in the Black community.
The most effective approach to the health promotion use of these findings would focus on education that explores local realities and sentiments regarding medical research and try to understand how these local perceptions relate to the TSS. Community members would give insight on the local knowledge around trust and skepticism about research studies or research institutions. This would be the basis for a collaborative effort between the community and the researchers to collectively address information about the TSS and local issues that have an impact on trust and skepticism. This approach to community education parallels well with the research philosophy behind “community-based participatory research” (CBPR), which involves having community representation in research protocols and projects from start to finish (Brownson, Baker, & Novick, 1999; Israel, Schulz, Parker, & Becker, 1998; Levine et al., 1992; Schulz et al., 1999; Wolff & Maurana, 2001). This approach to research allows for the voice of the community to be represented with regards to research being done on communities of interest. This also allows for the community to provide their perceptions, thoughts, and needs, and for participation in planning and evaluation. Through CBPR efforts, community members are also able to develop trust and rapport with the researchers, which can be used to break down barriers between the community and research entities (Agency for Healthcare Research and Quality, 2009; Christopher, Watts, McCormick, & Young, 2008; Sapienza, Corbie-Smith, Keim, & Fleischman, 2007). CBPR is a tool that can be used to help evaluate the knowledge base of the community and to address long held beliefs of the community as it is related to major issues in the Black community. By having researchers and the community working closer together, an exchange of knowledge can take place, which strengthens the work overall.
Conclusion
If the accurate details of the TSS are used as a platform to discuss potential medical mistrust in the Black community and the local and national events that support mistrust (including the need for using a healthy skepticism to “filter” incoming information for truths vs. misstatements), it opens up a line of dialogue or exchange with the community that may be used as a means to discuss some of the realities and benefits of participation in biomedical research. As all the reports of surveys assessing willingness of Blacks to participate in biomedical research have reported a similar willingness between Blacks and Whites (Brown & Topcu, 2003; Green, Maisiak, & Wang, 1997; Katz et al., 2006; Katz et al., 2007; Sengupta et al., 2000; Shavers et al., 2000), these educational sessions may be an opportunity to facilitate the exchange of information that could lead to the operationalization of this willingness, as willingness is but one component that determines actual participation. The conversations, within the context of CBPR, can be used to develop a better understanding of how to create strategies that will increase minority participation in clinical trials and research studies that are sensitive to the culture of the community.
The TSS has been used for so long as a marker in history, one often presumed to explain why Blacks are very skeptical of researchers and of the overall health care system. This presumed widely held belief in the Black community is “to not trust either researchers or the medical community” because of what happened within the TSS. The TSS has consequently become used as a metaphor for distrust in the Black community of the research and medical community. From our findings, these beliefs, as strongly held as they may be, are not based on detailed factual knowledge of the TSS in the Black community. Although it is not known whether the effect of having detailed knowledge would, in fact, exacerbate or ameliorate these widely held ‘beliefs on distrust’ within the Black community, this now documented lack of detailed knowledge does “open the door” for community-based health promotion education activities.
Researchers, public health practitioners, health educators, and other health-related professionals who work and participate deeply within the Black community, have the opportunity to use our findings on low detailed knowledge to revisit discussions around the TSS. Revisiting the facts of the TSS and using it as an educational tool for discussing past and future research benefits and challenges would be a good starting point.
Acknowledgments
Funding
The authors disclosed receipt of the following financial support for the research and/or authorship of this article:
This work was supported by the New York University Oral Cancer Research on Adult and Adolescent Health Promotion Center [NIDCR/NIH Grant U54 DE 14257] and by the Northeastern Minority Oral Health Research Center (NIDCR/NIH Grant P50 DE10592).
Footnotes
Declaration of Conflicting Interests
The authors declared no conflicts of interest with respect to the authorship and/or publication of this article.
References
- Agency for Healthcare Research and Quality. AHRQ activities using community-based participatory research to address health care disparities. Rockville, MD: Author; 2009. (AHRQ Publication No. 09-P012). Retrieved from http://www.ahrq.gov/research/cbprbrief.htm. [Google Scholar]
- Bates BR, Harris TM. The Tuskegee study of untreated syphilis and public perceptions of biomedical research: A focus group study. Journal of National Medical Association. 2004;96:1051–1064. [PMC free article] [PubMed] [Google Scholar]
- Benedek TG. The Tuskegee study of syphilis: Analysis of moral versus methodological aspects. Journal of Chronic Diseases. 1978;31:35–50. doi: 10.1016/0021-9681(78)90079-6. [DOI] [PubMed] [Google Scholar]
- Bouleware LE, Cooper LA, Ratner LE, LaVeist TA, Powe NR. Race and trust in the health care system. Public Health Reports. 2003;118:358–365. doi: 10.1016/S0033-3549(04)50262-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brandon DT, Isaac LA, LaVeist TA. The legacy of Tuskegee and trust ill medical care: Is Tuskegee responsible for race differences in mistrust of medical care? Journal of the National Medical Association. 2005;97:951–956. [PMC free article] [PubMed] [Google Scholar]
- Brown DR, Topcu M. Willingness to participate in clinical treatment research among older African Americans and whites. Gerontologist. 2003;43:62–72. doi: 10.1093/geront/43.1.62. [DOI] [PubMed] [Google Scholar]
- Brownson R, Baker E, Novick L. Community-based prevention: Programs that work. Gaithersburg, MD: Aspen; 1999. [Google Scholar]
- Caplan AL. Twenty years after. The legacy of the Tuskegee Syphilis Study. When evil intrudes. Hastings Center Report. 1992;22(6):29–32. [PubMed] [Google Scholar]
- Christopher S, Watts V, McCormick AKHG, Young S. Building and maintaining trust in a community-based participatory research partnership. American Journal of Public Health. 2008;98:1398–1406. doi: 10.2105/AJPH.2007.125757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corbie-Smith G, Thomas SB, Williams MV, Moody-Ayers S. Attitudes and beliefs of African Americans toward participation in medical research. Journal of General Internal Medicine. 1999;14:537–546. doi: 10.1046/j.1525-1497.1999.07048.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corbie-Smith GM. Minority recruitment and participation in health research. North Carolina Medical Journal. 2004;6:385–387. [PubMed] [Google Scholar]
- Fairchild AL, Bayer R. Uses and abuses of Tuskegee. Science. 1999;284:919–921. doi: 10.1126/science.284.5416.919. [DOI] [PubMed] [Google Scholar]
- Fletcher JC. Tuskegee syphilis study legacy committee report of 1996, CDC workshop at Tuskegee University. In: Reverby SM, editor. Tuskegee’s truths: Rethinking the Tuskegee syphilis study. Chapel Hill: University of North Carolina Press; 2000. pp. 559–566. [Google Scholar]
- Gamble VN. A legacy of distrust: African Americans and medical research. American Journal of Preventive Medicine. 1993;9(6 Suppl):35–38. [PubMed] [Google Scholar]
- Gamble VN. The Tuskegee syphilis study and women’s health. Journal of the American Medical Women’s Association. 1997;52:195–196. [PubMed] [Google Scholar]
- Green BL, Maisiak R, Wang MQ. Participation in health education, health promotion, and health research by African Americans: Effects of the Tuskegee syphilis experiment. Journal of Health Education. 1997;28:196–201. [Google Scholar]
- Israel B, Schulz A, Parker E, Becker A. Review of community-based research: Assessing partnership approaches to improve public health. Annual Review of Public Health. 1998;19:173–202. doi: 10.1146/annurev.publhealth.19.1.173. [DOI] [PubMed] [Google Scholar]
- Jones JH. Bad blood: The Tuskegee syphilis experiment. New York, NY: Free Press; 1981. [Google Scholar]
- Katz RV, Claudio C, Kressin NR, Green BL, Wang MQ, Russell SL. Willingness to participate in cancer screenings: Blacks vs. Whites vs. Puerto Rican Hispanics. Cancer Control. 2008;15:334–343. doi: 10.1177/107327480801500408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Katz RV, Green BL, Kressin NR, Claudio C, Wang MQ, Russell SL. Willingness of minorities to participate in biomedical studies: Confirmatory findings from a follow-up study using the Tuskegee legacy project questionnaire. Journal of the National Medical Association. 2007;99:1050–1062. [PMC free article] [PubMed] [Google Scholar]
- Katz RV, Green BL, Kressin NR, Kegeles SS, Wang MQ, James SA, McCallum JM. The legacy of the Tuskegee syphilis study: Assessing its impact on willingness to participate in biomedical research studies. Journal of Health Care for the Poor and Underserved. 2008;19:1168–1180. doi: 10.1353/hpu.0.0067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Katz RV, Green BL, Kressin NR, Kegeles SS, Wang MQ, James SA, Russell SL. Exploring the “legacy” of the Tuskegee syphilis study: A follow-up study from the Tuskegee legacy project. Journal of the National Medical Association. 2009;101:179–183. doi: 10.1016/s0027-9684(15)30833-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Katz RV, Kegeles SS, Kressin NR, Green BL, Wang MQ, James SA, Claudio C. The Tuskegee legacy project: Willingness of minorities to participate in biomedical research. Journal of Health Care for the Poor and Underserved. 2006;17:698–715. doi: 10.1353/hpu.2006.0126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Katz RV, Kegeles SS, Kressin NR, James SA, Green BL, Wang MQ, Claudio C. Awareness of the USPHS syphilis study at Tuskegee and the U.S. presidential apology and their influence on minority participation in biomedical research. American Journal of Public Health. 2008;98:1137–1147. doi: 10.2105/AJPH.2006.100131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levine DM, Becker DM, Bone LR, Stillman FA, Tuggle MB, II, Prentice M, Filippeli J. A partnership with minority populations: A community model of effectiveness research. Ethnicity & Disease. 1992;2:296–305. [PubMed] [Google Scholar]
- Matthews AK, Sellergren SA, Manfredi C, Williams M. Factors influencing medical information seeking among African American cancer patients. Journal of Health Communication. 2002;7:205–219. doi: 10.1080/10810730290088094. [DOI] [PubMed] [Google Scholar]
- McCallum JM, Arekere DM, Green BL, Katz RV, Rivers BM. Awareness and knowledge of the U.S. Public Health Service syphilis study at Tuskegee: Implications for biomedical research. Journal of Health Care for the Poor and Underserved. 2006;17:716–733. doi: 10.1353/hpu.2006.0130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pressel DM. Nuremberg and Tuskegee: Lessons for contemporary American medicine. Journal of the National Medical Association. 2003;95:1216–1225. [PMC free article] [PubMed] [Google Scholar]
- Rathore SS, Krumholz HM. Race, ethnic group, and clinical research. British Medical Journal. 2003;327:763–764. doi: 10.1136/bmj.327.7418.763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sapienza JN, Corbie-Smith G, Keim S, Fleischman AR. Community engagement in epidemiological research. Ambulatory Pediatrics. 2007;7:247–252. doi: 10.1016/j.ambp.2007.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schulz A, Parker E, Israel B, Becker A, Maciak B, Hollis R. Conducting a participatory community-based survey. In: Brownson R, Baker E, Novick L, editors. Community-based prevention programs that work. Gaithersburg, MD: Aspen; 1999. pp. 84–104. [Google Scholar]
- Sengupta S, Strauss RP, DeVellis R, Quinn SC, DeVellis B, Ware WB. Factors affecting African-American participation in AIDS research. Journal of Acquired Immune Deficiency Syndromes. 2000;24:275–284. doi: 10.1097/00126334-200007010-00014. [DOI] [PubMed] [Google Scholar]
- Shavers VL, Lynch CF, Burmeister LF. Knowledge of the Tuskegee study and its impact on willingness to participate in medical research studies. Journal of the National Medical Association. 2000;92:563–572. [PMC free article] [PubMed] [Google Scholar]
- Shavers-Hornaday VL, Lynch CF, Burmeister LF, Torner JC. Why are African Americans under-represented in medical research studies? Impediments to participation. Ethnicity & Health. 1997;2:31–45. doi: 10.1080/13557858.1997.9961813. [DOI] [PubMed] [Google Scholar]
- White RM. Misinformation and misbeliefs in the Tuskegee study of untreated syphilis fuel mistrust in the healthcare system. Journal of the National Medical Association. 2005;97:1566–1573. [PMC free article] [PubMed] [Google Scholar]
- Wolff M, Maurana C. Building effective community academic partnerships to improve health: A qualitative study of perspectives from communities. Academic Medicine. 2001;76:166–172. doi: 10.1097/00001888-200102000-00016. [DOI] [PubMed] [Google Scholar]