Abstract
Introduction. White Sponge Nevus (WSN) is a rare pathology with a pathogenesis on genetic basis, a benign course and a localization affecting the mucosal keratin.
WSN is usually a symptomless pathology: when pain is present, some authors reported reduction of symptoms by taking penicillin or oral tetracycline rinses, suggesting that a bacterial overinfection could be at the base of possible painful symptoms.
Case Report. We describe 2 patients affected by WSN, father and son: they presented two different oral diseases associated with an infection by Staphylococcus aureus. So, we have performed a careful oral hygiene to reduce infection in the oral cavity. In the following days we prescribed 2 rinses a day with a mouthwash containing chlorhexidine digluconate at two different percentages.
Discussion. Early diagnosis of this lesion is important, because it allows us to exclude other more serious diseases. In the most part of cases, WSN requires no treatment because of its benign and asymptomatic behaviour: up to now, no protocol of treatment for this condition was standardized. Even if WSN is a painless condition, sometime a correlated painful symptomatology was reported.
Conclusions. In our experience, we have achieved excellent results even with chlorhexidine digluconate rinses, considering that our treated cases were both infected by Staphylococcus aureus.
We hypothesize that the corrugated plaques and the altered texture of the mucosa create the right conditions for the colonization and the development of microbial species such as saprophytic bacteria or fungal species.
Keywords: White Sponge Nevus, Staphylococcus Aureus, Oral disease
Introduction
White Sponge Nevus (WSN) is a rare pathology with a pathogenesis on genetic basis, a benign course and a localization affecting the mucosal keratin.
The onset is usually during early infancy, often before 20 years, and there is no gender predilection. This mucosal alteration usually affects oral soft tissues, but it sometime involves vaginal and rectal mucosa. In literature, we can find that WSN is called also in several other ways, such as “nevus of Cannon”, “leukoderma exfoliativum mucosae oris”, “familial white folded mucosal dysplasia” and “hereditary leukokeratosis” 1.
The most recent studies indicate that a mutation in the helical domain of mucosal specific keratins, K4 and K132 could be responsible for the alteration of epithelial cells.
Lesions of WSN are easily recognized and clinically valuable: they appear as bilateral white spongy plaques, typically found on the buccal mucosa, and the patients refer no painful symptomatology. We can find these lesions in other common sites including the tongue, floor of the mouth, and alveolar mucosa 3,4.
Cytological features of this condition show that the nuclei are pyknotic. There are no aspects of malignant lesion and we have found no report of dysplasia in the literature. Other histological findings include intracellular edema of the spinous layer cells 5. However, intracellular edema is not pathognomonic for WSN; in fact, the same aspect is present in other lesions, such as the leukoedema which is quite similar to WSN, even if it shows no parakeratosis 6. When we manage a patient affected by WSN no treatment is required onto these lesions, except for a clinical condition of a plaque which extends onto the lip vermilion: in this kind of cases, we perform a surgical exeresis for aesthetic reasons 7.
Concerning the differential diagnosis, WSN is often confused with a form of chronic hyperplastic candidosis resistant to treatment; moreover, the surface of mucosa affected by WSN, which presents an irregular architecture, favors secondary infection by Candida 5.
WSN typically affects several individuals in a same family, further confirming its autosomal dominant heredity 8-9.
WSN is usually a symptomless pathology: when pain is present, some authors reported reduction of symptoms by taking penicillin10 or oral tetracycline rinses11, suggesting that a bacterial overinfection could be at the base of possible painful symptoms. However, almost all cases reported in the literature describe WSN as a benign condition that does not require any treatment.
We describe 2 patients affected by WSN, father and son: because they presented two different oral diseases associated with an infection by Staphylococcus aureus (SA), we hypothesized a relationship between WSN and Staphylococcus aureus infection.
Case Report
An 38 year-old Italian man came to the Department of Oral Hygiene and Periodontology at Calabrodental clinic in April 2011 for the evaluation of white bilateral corrugated plaques developed on the buccal mucosa and on the gingiva, these plaques were been present since he was 13 years-old. (Fig.1)
Fig 1.
a patient showing white bilateral corrugated plaques developed on the buccal mucosa and on the gingiva.
This clinical condition was investigated by another clinician who carried out a diagnosis of White Sponge Nevus, excluding so the other similar pathologies compatible with this clinical aspect.
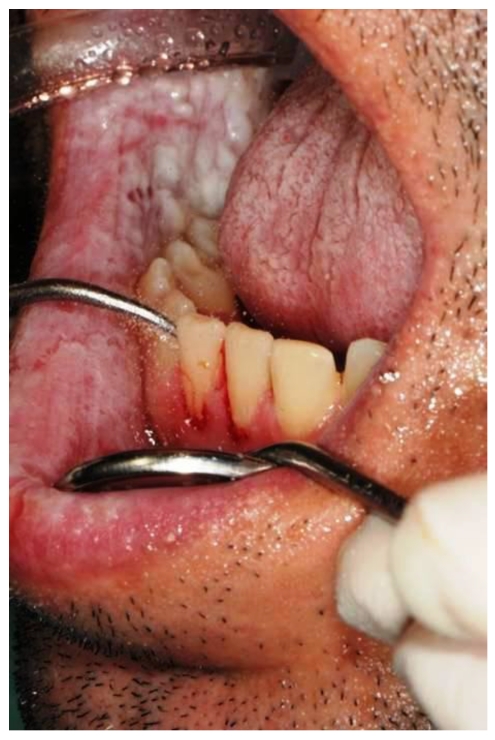
These plaques were always asymptomatic, however, from 2 months, the patient complained of burning symptoms that persisted throughout the day. So, he came at the clinic Calabrodental in order to alleviate these symptoms. After routine investigations, we prescribed an oral buffer to assess the possible presence of bacterial or fungal superinfection: the result was positive for Staphylococcus aureus which showed a susceptibility to methicillin. The analysis didn't evidenced the presence of Candida albicans or other fungal infections, so the painful symptomatology could be related to a poor oral hygiene and to the presence of the methicillin-resistant Staphylococcus aureus in the oral cavity of our patient. So, we have performed a careful oral hygiene to reduce infection in the oral cavity. (Fig.2)
Fig 2.
a careful oral hygiene performed to the patient affected by white sponge nevus.
In the following days we prescribed 2 rinses a day with a mouthwash containing chlorhexidine digluconate at 0.2%. We performed the follow-up after 7 days and the patient has reported the disappearance of pain. During the check we noted that the same plaques were developed on the oral mucosa of the son of our patient, so we wanted to document the case, after obtaining the written consent of the patient.
Our little patient showed an intraoral clinical condition very similar to father's, moreover, the patient was affected by a bilateral angular cheilitis. (Fig.3,4)
Fig 3.
the little son of our patient showing white plaques developed on the gingiva.
Fig 4.
a bilateral angular cheilitis caused by Staphylococcus aureus infection.
A buffer containing patient's saliva was submitted to a diagnostic oral microbiology laboratory: the microbiological analysis showed in the presence of Staphylococcus aureus sensitive to methicillin (MSSA) in the oral cavity of our young patient, while, no fungal infections was found.
2 rinses a day with mouthwash containing chlorhexidine digluconate at 0,12% was prescribed in order to decrease the bacteria and the occurrence of relapses of angular cheilitis.
Discussion
The aspect of WSN is not strongly pathognomonic. It's important to perform careful clinical and histological examinations to differentiate this benign condition from other potentially pre-malignant lesions as well as oral lichen planus, keratosis follicularis, candidiasis, lichenoid reactions and lupus erythematosus12.
Early diagnosis of this lesion is important, because it allows us to exclude other more serious diseases. In the most part of cases, WSN requires no treatment because of its benign and asymptomatic behaviour: up to now, no protocol of treatment for this condition was standardized 13. Even if WSN is a painless condition, sometime a correlated painful symptomatology was reported 5,10,11.
Antibiotic treatment with oral penicillin 10, ampicillin 5,11, and tetracycline has achieved a moderate success; some authors have also suggested the use of tetracycline mouthwashes. In our experience, we have achieved excellent results even with chlorhexidine digluconate rinses, considering that our treated cases were both infected by Staphylococcus aureus. WSN is not considered a bacterial disease; however, since antibiotic therapy is able to reduce the symptomatology occasionally occurred, it is possible that infections may play a role in the pathogenesis of this disease 14. Furthermore, the corrugated plaques and the altered texture of the mucosa create the right conditions for the colonization and the development of microbial species such as saprophytic bacteria or fungal species. In these 2 reported cases, the wide part of mucosa interested by the plaques of the WSN is a condition which promotes the grown of the Staphylococcus aureus 15.
Conclusions
In all reported cases, the patients affected by WSN achieve a condition of clinical stability between 20 and 30 years, moreover, have never been described any malignant transformation of the interested mucosa16; however, if a Staphylococcus aureus infection is developing, there may be periods of exacerbation and remission of the symptoms: so we suggest to take care of the oral hygiene and to daily use a mouthwash containing chlorhexidine 0.05% in order to prevent the growth of most dangerous species of bacteria, especially the Staphylococcus aureus as we reported in our communication.
Authors' Contributions
MM and SB participated in the clinical and pharmacological management of the treated cases.
MT drafted the manuscript and revised the literature sources.
FI participated in the follow-up examinations.
All authors read and approved the final manuscript.
Consent Statement
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
References
- 1.Cannon AB. White sponge nevus of the mucosa (naevus spongiosus albus mucosae) Arch Dermatol Syphilol. 1935;31:365. [Google Scholar]
- 2.Woo S-B. Diseases of the oral mucosa. In: Mckee PH, et al., editors. Pathology of the Skin with Clinical Correlations. 3rd ed. Philadelphia: Elsevier Mosby; 2005. p. 387. [Google Scholar]
- 3.Frithiof L, Banoczy J. White sponge nevus (leukoedema exfoliativum mucosae oris): ultrastructural observations. Oral Surg. 1976;41:607. doi: 10.1016/0030-4220(76)90313-3. [DOI] [PubMed] [Google Scholar]
- 4.Jorgensen RJ, Levin S. White sponge nevus. Arch Dermatol. 1981;117:73. [PubMed] [Google Scholar]
- 5.Sadeghi EM, Witkop CJ. The presence of Candida albicans in hereditary benign intraepithelial dyskeratosis: an ultrastructural observation. Oral Surg Oral Med Oral Pathol. 1979;48:342–346. doi: 10.1016/0030-4220(79)90034-3. [DOI] [PubMed] [Google Scholar]
- 6.Jorgenson RJ, Levin LS. White sponge nevus. Arch Dermatol. 1981;117:73–76. [PubMed] [Google Scholar]
- 7.Yavazyilmaz E. et al. Oral-dental findings in dyskeratosis congenita. J Oral Pathol Med. 1992;21:280–284. doi: 10.1111/j.1600-0714.1992.tb01011.x. [DOI] [PubMed] [Google Scholar]
- 8.Martelli Jr H, Pereira SM, Rocha TM, Santos PLAN, Paula AMB, Bonan RF. White sponge nevus: report of a three-generation family. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;103:43–7. doi: 10.1016/j.tripleo.2006.05.029. [DOI] [PubMed] [Google Scholar]
- 9.López Jornet P. White sponge nevus: presentation of a new family. Pediatr Dermatol. 2008;25(1):116–7. doi: 10.1111/j.1525-1470.2007.00599.x. [DOI] [PubMed] [Google Scholar]
- 10.Alinovi A, Benoldi D, Pezzarossa E. White sponge nevus: successful treatment with penicillin. Acta Derm Venerol. 1983;63:83–5. [PubMed] [Google Scholar]
- 11.Lim J, Ng SK. Oral tetracycline rinse improves symptoms of white sponge nevus. J Am Acad Dermatol. 1992;26:1003–5. doi: 10.1016/s0190-9622(08)80340-4. [DOI] [PubMed] [Google Scholar]
- 12.Inchingolo F, Tatullo M, Abenavoli FM, Marrelli M, Inchingolo AD, Inchingolo AM, Dipalma G. Non-Hodgkin lymphoma affecting the tongue: unusual intra-oral location. Head Neck Oncol. 2011 Jan 4;3:1. doi: 10.1186/1758-3284-3-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sambucety OS, López PM, Prieto MAR, Gónzalez IR, Fernández MM. Lesiones blanquecinas en la mucosa oral. An Esp Pediatr. 2001;55:159–60. [PubMed] [Google Scholar]
- 14.McDonagh AJG. et al. White sponge naevus successfully treated with topical tetracycline. Clin Exp Dermatol. 1990;15:152. doi: 10.1111/j.1365-2230.1990.tb02056.x. [DOI] [PubMed] [Google Scholar]
- 15.Salgodo CO, Farr BM, Calfee DP. Community-acquired methicillin-resistant Staphylococcus aureus: a meta-analysis of prevalence and risk factors. Clin Infect Dis. 2003;36:131–9. doi: 10.1086/345436. [DOI] [PubMed] [Google Scholar]
- 16.Lamey PJ. et al. Oral White sponge naevus: response to antibiotic therapy. Clin Exp Dermatol. 1998;23:59. doi: 10.1046/j.1365-2230.1998.00325.x. [DOI] [PubMed] [Google Scholar]