Abstract
Overcrowding and poor-quality housing have a direct relationship to poor mental health, developmental delay, heart disease, and even short stature.
You have to call it an epidemic because it is increasing, and it is becoming not only more common, but more serious.
Megan Sandel, MD Department of Pediatrics, Boston University School of Medicine, on the link between inadequate housing and childhood asthma1
FOR MANY BREADWINNERS of low-income families, going home at the end of a long workday can be a challenge, but it is a challenge they look forward to from the moment they arrive at work. The battle might begin with stepping off site into a city block filled with diesel exhaust. Perhaps a hard worker straps into a car for a fight with congested traffic on the long commute home, constantly alert to each potential danger the modern roadways present.
Or maybe this breadwinner walks through the exhaust to a bus or subway platform littered with garbage, stepping over a foul-smelling river of leakage and spills that play host to germcarrying insects and vermin. There may be a tense wait for the push onto overcrowded public transportation, then a bumpy ride back to dark and dirty streets whose dimly lit corners conceal hidden threats and whose sidewalks are paved with broken glass and discarded, jagged-edged junk. Finally she’ll arrive at the comfort of home—a welcoming community, a loving family, and rooms and doors that close against the dangers of the outside world.
Home is where we want to feel safe. Access to a safe and comfortable “home,” as necessary shelter, a source of identification, and a place to rest and relax, is both a psychological and a physical necessity.2 Today's culture of fear and isolation have driven many families, particularly those living in crowded, urban environments, to seek safety and security behind the tightly closed doors of home.
DANGEROUS COMFORT
The physical and social makeup of the urban environment encourages this isolation. Corner markets make inexpensive junk food, liquor, soda, and cigarettes available close to home and at all hours. The amount of television being watched by each member of a family continues to increase, and what's more, individuals are sitting alone and sedentary, watching separate programs in separate rooms, eating from individual supersized bags of chips. Interaction, even among close-knit families, is discouraged.
The unfortunate reality is that home often harbors dangers of its own, and the tendency to isolate indoors is shown to have ill effects on family health. The connection between inadequate housing and poor health is increasingly well documented.3 Substandard and deteriorating housing contributes to a variety of ailments, from respiratory disease and neurological disorders to psychological and behavioral dysfunction. These often life-threatening ailments disproportionately affect children of color and children from low-income families.2
Significant research demonstrates the harmful association of asthma, neurological damage, malnutrition, stunted growth, accidents, and injury with household triggers like poor insulation, combustion appliances, cockroach and rodent infestation, dust mites, hyper- and hypothermia, unaffordable rent, and dangerous levels of lead in soil and household paint.4 Furthermore, the culture of isolation ensures that the persons who are most vulnerable to these diseases— infants, children, the elderly, the chronically ill, and the immunocompromised—are also those who spend the most time indoors and alone.
The temptations of “virtual living” can be too strong to resist. Use of personal computers, surfing the Web, Internet shopping, televiewing, telecommuting, telecommunicating, and teleliving are fast becoming the norm for those in the middle classes. Many see no reason to leave home. There is little, in an affluent urban environment, that can't be “ordered in”–from food to services to entertainment.
Those who can't afford these luxuries find virtual living through television (and the bombardment of advertisements that encourage sedentary consumerism). These, together with rising levels of malnutrition, contribute to a national epidemic of obesity, and the variety of chronic illnesses to which it contributes, exacerbating the crises of public health and housing (J. Harkness, unpublished data, 2001).
HOME SICK
The prevalence of childhood asthma is increasing at an alarming rate. Between 1982 and 1994, the number of children afflicted with this chronic respiratory disease increased 70%. Worse still, the number of asthma-related deaths among children increased 50%.5 Although environmental pollution, such as hazardous and toxic emissions and overall poor air quality, contributes greatly to this increase, the role that a harmful home environment plays in negative health outcomes is being taken more seriously.
In the case of asthma, environmental conservatives are quick to point to indoor triggers as being solely responsible for the marked increase in prevalence rates. Health advocates, both on a professional and a grassroots level, assert that both indoor and outdoor triggers are the culprits. Both triggers disproportionately affect poor children, children of color, and children living in inner-city environments.
Across the country, more than 5 million families—over 4 million children—are living in substandard housing that, despite its wretched state, they can barely afford.4 Inside many of these deteriorating houses and apartments are hosts of harmful biological and chemical contaminants that contribute to the growing asthma epidemic. Asthma triggers like mold, cockroaches and cockroach dust, mice and rats and their droppings, dust mites, carbon monoxide, and environmental tobacco smoke are all more prevalent in low-income and inner-city homes. Once again, the most vulnerable find themselves at greatest risk of harm.
In addition to home-based environmental hazard–related instances of childhood asthma and skin ailments such as eczema and alveolitis, lead poisoning continues to strike specific pockets of children at an alarming rate. Nationally, there has been a 77% decline in the prevalence of childhood lead poisoning over the past 15 years. This drop was predominantly due to the legislated termination of the use of leaded gasoline. Still, poor children and children of color, particularly those living in dilapidated, inner-city housing, continue to show dangerously high blood lead levels.
The lead found in dust, household paint, and the bare soil common in crawl spaces and tracked in from yards and poorly maintained parks contributes to the continuing crisis of childhood lead poisoning among the poor. Children in poor and inner-city communities and between the ages of 18 and 36 months are at greatest risk of lead poisoning. In fact, children from low-income families are 5 times more likely to have elevated blood lead levels.6 Lead poisoning can result in neurological damage, reduced IQ, hyperactivity, increased aggression, learning disabilities, and behavioral problems.6
It is no mere coincidence that the problems identifiably associated with childhood lead poisoning are also the problems associated with the education and safety of children and young people in inner-city communities. Lead poisoning doesn't come with the benefit of observable symptoms. Without proper screening, it can go undetected for the duration of an affected person's life. Unfortunately, the children and communities hardest hit by childhood lead poisoning are also those with limited access to health care.7
PRIMARY PREVENTION
Research also indicates that the type of housing in which low-income families reside adversely affects their health outcomes.8 Whether a family lives in owner-occupied housing, privately rented housing, or public housing has a significant relationship to their health. Not only are health outcomes affected in terms of childhood asthma and lead poisoning, but studies have shown that overcrowding in childhood homes can be connected to a variety of serious diseases later in life. Overcrowding and poor-quality housing have a direct relationship to poor mental health, developmental delay, heart disease, and even short stature.8
It's a much simpler task to identify the problems and connections between negative health outcomes and inadequate housing than it is to fix them. Lowincome families often don't have the resources or access to information to make their homes safer for themselves and their children. Public housing advocates decry the lack of funding to take care of even the most basic public health defects in the housing units to which low-income families are assigned.
Landlords, whether public or private, have a responsibility to provide housing that is free from water leaks, mold, roach and rodent infestation, and other harmful defects that give rise to asthma and lead poisoning. In the case of privately rented housing, the landlords themselves often lack the resources to adequately maintain their properties. Those who do have the necessary resources often lack the desire or initiative, refusing to use them until significant legal action has been taken against them.1 Poor and immigrant families are often afraid to complain, because living in substandard housing is better than being homeless. Too many families resign themselves to suffering in shame and watching their family's health deteriorate, with little hope for help.
MEETING THE DEMAND FOR ADEQUATE HOUSING
Grassroots groups and organizations across the country are gathering communities together to effect change in the health and housing outlook for poor families. Issues like access to adequate, affordable housing are at the forefront of the mission of some of these groups, while directly addressing the subsequent health issues that stem from lack of access is the focus of others. Increases in fair market housing costs in urban areas are far exceeding increases in income, particularly among low-income families.
Skyrocketing housing costs aren't limited to well-documented cities like New York, San Francisco, and Los Angeles. In areas that receive relatively little attention—like Salt Lake City, Utah, where housing costs have risen as much as 98.7% in the last decade9—fair market prices are forcing the average family to spend upward of 65% of their income on housing.
The acceptable standard for housing costs, approximately 30% of a household's income, can be a tough pill to swallow for low-income families. When families are forced not only to meet, but often to far exceed, standard spending on housing, other important needs suffer, such as food, health care, and insurance as well as family activities that provide exercise and emotional stability.
COMMUNITIES FIGHT BACK
In the United States and Europe, innovative efforts are being made at many levels to address the deteriorating social, physical, and psychological health of low-income families and individuals struggling with inadequate housing. These efforts include European experiments in social housing, international initiatives in public housing, and, in this country, Section 8 community housing initiatives and alternative nursing homes and senior living environments.
Some groups are working through legislation. The Office of Native American Programs (ONAP), for instance, successfully lobbied for the 1996 Native American Housing Assistance and Self Determination Act (NAHASDA). NAHASDA is designed to guarantee federal housing assistance for indigenous tribes in a manner that recognizes and respects tribal sovereignty.10 ONAP's own Housing Resource Center works with individual tribes, researchers, businesses, nonprofits, and grassroots housing development groups to develop housing and promote economic growth on reservations and tribal lands.
San Diego's Lead-SALTA (Salud Ambiental Latínas Tomando Acción) Program, a project of the Environmental Health Coalition (EHC) Toxic-Free Neighborhoods Campaign, works to specifically address lead poisoning in its at-risk communities. Samples collected by the EHC found that over 80% of homes with children younger than 6 years exceeded both federal and state guidelines for lead content in at least one aspect.6 In San Diego County, 84% of children reported to have elevated blood lead levels are Latino. This is increasingly alarming when it is understood that not all at-risk children are being tested, and of those tested, not all cases of high lead levels are reported. In addition to assessing the problem, the Lead-SALTA Program is working to secure funds from California's increased tobacco tax to promote the health of children at risk.
Established research entities are working with inner-city communities to study the effects of inadequate housing and increase awareness of both the dangers and the steps that can be taken to make homes safer. Tufts University, Harvard University, and Boston University worked with community leaders to survey housing conditions and health in the Boston, Mass, area. The survey found high rates of hyperthermia, alternating with periods of excessive hypothermia, that led tenants to rely on gas ovens for warmth, increasing the levels of chemical contaminants in the home. These temperature variations, in addition to widespread mold, water damage, and pest infestation, coincided with extremely high rates of asthma, leading researchers to suggest a causal relationship.11
GETTING SPECIFIC
Some agencies are focusing on specific health outcomes, such as asthma, and directing their efforts at affecting positive change in that arena. The National Cooperative Inner-City Asthma Study (NCICAS) and the US Department of Housing and Urban Development (HUD) Roach Project are two such initiatives aimed at addressing asthma triggers both outdoors and in the home. The NCICAS found that 37% of children studied had cockroach allergies, while 50% of the children's bedrooms had dust containing excessively high levels of cockroach allergens.12 The HUD Roach Project works to assess the levels of cockroach allergen contamination in the home while working to set up safe systems of elimination and cleanup.
In New York City, the Harlem Hospital Center's Department of Pediatrics, the Harlem Children's Zone, Inc., and the Harlem Health Promotion Center are working together on the Harlem Children's Zone Asthma Initiative: From Home to School to Hospital. The Harlem Children's Zone Project is a 24-block area in Central Harlem that has been shown to have one of the highest rates of childhood asthma in the country. The groups are working together to study children from birth to 12 years of age, testing for asthma, linking the children with primary care providers and health insurance, and providing social, educational, environmental, and medical interventions both at home and in the school.
PUBLIC HEALTH AND SOCIAL JUSTICE
Other agencies are fighting on the local level for housing rights, using the impact of substandard housing on public health as a prime lobbying point to gain the increased attention and funding needed to address the problem. In Los Angeles, grassroots organizations like ACORN (Association of Community Organizations for Reform Now) and Housing LA are celebrating the local government's recent commitment to create a $100 million trust fund to build affordable housing. Even with such a large sum, much of it earmarked from tobacco settlement funds, the city will struggle to build enough housing. California's housing stock is the third oldest in the nation and is in serious need of attention. Housing experts estimate that 4000 additional housing units must be built each year just to meet the demand.13
The Community Environmental Health Resource Center (CEHRC) in Washington, DC, works with grassroots organizations engaged in the fight for social justice in low-income communities. The center's primary focus is empowering residents and increasing economic opportunities to address the environmental health hazards posed by substandard housing (including asthma, lead, carbon monoxide, and pesticides) that are faced by children and other vulnerable persons in low-income communities.14
Barely a year old, CEHRC (a project of the Alliance to End Childhood Lead Poisoning) trains community members in safe and effective tools for identifying the environmental hazards created by substandard housing. After documenting hazards, CEHRC targets the hardest hit communities and works with the private sector to train contractors and workers to control identified hazards. By working to target a number of environmental health hazards, CEHRC addresses the major negative health outcomes of childhood asthma and lead poisoning. It also takes on the less studied hazards that contribute to increased risk for chronic illnesses like cancer and heart disease as well as depression and poor mental health.
A COMMUNITY IN CRISIS
Working in concert to address multiple issues at once is becoming a top priority as more communities face health crises of epidemic proportions in areas directly related to substandard housing. Cleveland, Ohio, found itself dealing with a double dose of trouble when studies showed that the prevalence of asthma, the most common chronic childhood disease, had increased by more than 100% in 20 years. Additionally, childhood lead poisoning had become a crisis among Cleveland's children. In 1998, 34% of children in Cleveland were found to have elevated blood lead levels, compared with 5% nationally.15
Rather than stretch the capacity of already meager resources, the Cleveland Housing Network and the Cleveland Department of Public Health's Lead-Safe Housing Program decided to coordinate their efforts with the Lead+ Asthma Project, a joint program targeting the 2 deadliest environmental health hazards facing local children. The Lead+Asthma Project combined asthma trigger control intervention with existing lead poisoning prevention programs to conduct parent education, hazard assessment, and environmental intervention.18
The project is based on the understanding that both asthma and lead poisoning are related to substandard housing, that both disproportionately affect poor and inner-city children and children of color, that the role of caregivers is critical to the success of programs addressing either problem, and that strategies to address both problems must focus on reducing moisture and dust contamination. Additionally, similarities were found in the number of children affected, the nature and immediacy of the impairments, and the strength of the evidence of direct correlation between negative health outcomes and substandard housing.
Cleveland's environmental health crisis also attracted the attention of the Center for Community Action for Primary Prevention (CCAPP), in Columbia, Maryland. Working together with Environmental Health Watch of Cleveland, CCAPP has begun the Cleveland Better Start Pilot Project. Identifying childhood asthma and lead poisoning as contributors to children's school performance, absenteeism, and ability to learn and participate in a full range of activities, the project focuses on pregnant women and infants in an effort to prevent exposure to lead hazards and asthma triggers before harm is done.
Once lead poisoning has taken place, the harm cannot be reversed. Similarly, asthma, once contracted, is a lifelong health concern. Both the Lead+Asthma Project and the Cleveland Better Start Pilot Project focus on primary prevention in high-risk communities, screening children, and providing access to appropriate health care to address the problem while also providing support and training to health care professionals so that they may best address the situation.
AT RISK IN RURAL AMERICA
Although urban areas are receiving increased attention and funding to address the health concerns associated with substandard housing, poor children in rural areas are also affected. In the Appalachian region of southeast Ohio, the Rural Action Development Corporation is entering its 20th year of working to train the community regarding issues of economic and environmental justice. The area's feast-or-famine economic cycle, based on its reliance on extraction-based industry, has led to unemployment, widespread poverty, illiteracy, ill health, and family instability.19
Rural Action works with grassroots organizations, citizens groups, and individuals to improve the environmental and economic outlook of the community. Its HealthCorps utilizes AmeriCorps volunteers and Rural Action staffers to face environmental health hazards head-on by integrating the entire community into the effort. The Self-Help Home Repair Program hires local labor and materials purchased from local suppliers to perform emergency home repairs for low-income families while increasing local economic activity and community stability.
EFFECTING CHANGE FROM WITHIN
The focus on multi-issue approaches to home-based hazards, particularly in low-income and inner-city families and among families of color, is gaining agency in communities across the country. One of the most promising aspects of the many grassroots efforts to address home-based environmental health hazards is the focus on increasing community awareness of both the concerns and the methods of reducing risk.
Alerting parents and caregivers to the harmful effects of environmental tobacco smoke on children is one thing. Giving them tools they can use to prevent those hazards in the spirit of harm reduction is another. Because not all caregivers are going to give up smoking, suggesting alternatives—such as smoking outdoors or closing off a separate space for smoking so that children are not directly exposed to the smoke—is an important way that organizations, healthcare providers, and research teams can work to assure positive results in even the most challenging of environments.
Similarly, great strides are being made in integrated pest management to fight insect and rodent infestation, which remains a serious problem for both urban and rural at-risk families. It is important, however, that the community have access to information detailing not only what to fight but how to fight it. While insect and rodent infestation is a main trigger for asthma and a host of other ailments, the pesticides being used—and often misused—to fight infestation can contribute to the hazardous environment.
Although more and more research on the immediate health outcomes posed by home-based environmental hazards is being conducted, precious little is understood about the long-term health outcomes. What is known is that even the smallest positive change in health outcomes can have a large effect on the community.3 While the studies continue, support for grassroots efforts is essential to the struggle to address and eliminate the environmental hazards posed by substandard and inadequate housing.
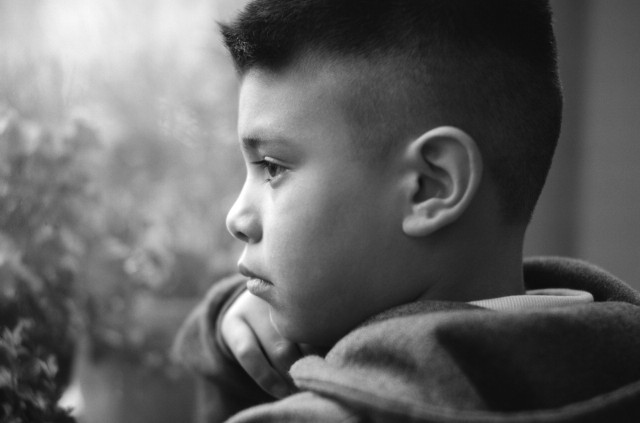
Figure 1.

Chidren who live in insecure urban areas may not be any safer indoors. Asthma can be triggered by allergens in the indoor environment; lead poisoning can be caused by dust from old paint and dirt tracked into the house.
Figure 2.

Harlem Children's Zone, Inc led a successful effort to convert this 159-unit apartment building in Harlem, on 118th Street, from New York City ownership to tenant ownership in October 2000.
Peer Reviewed
References
- 1.WBUR Web site. Rachel Gotbaum interview with Megan Sandel on WBUR. July 10, 2000. Available at: http://www.publicbroadcasting.net/wbur/news.newsmain?action=article&ARTICLE_ID=41278. Accessed December 18, 2001.
- 2.Fullilove MT, Fullilove RE. What's housing got to do with it? Am J Public Health. 2000;90:183–184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Thomson H, Petticrew M, Morrison D. Health effects of housing improvement: systematic review of intervention studies. BMJ. 2001;323:187–190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sharfstein J, Sandel M, Kahn R, Bauchner H. Is child health at risk while families wait for housing vouchers? Am J Public Health. 2001;91: 1191–1192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Environmental Health Watch Web site. Asthma. Available at: http://www.ehw.org/asthma/asth_home1.htm. Accessed January 15, 2002.
- 6.Environmental Health Coalition. EHC study reveals housing health horrors. San Diego Earth Times. April 2001. Available at: http://www.sdearthtimes.com/et0401/et0401s17.html. Accessed January 15, 2002.
- 7.Brown MJ, Gardner J, Sargent JD, Swartz K, Hu H, Timperi R. The effectiveness of housing policies in reducing children's lead exposure. Am J Public Health. 2001;91:621–624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gordon D, Pantazis C, Heslop P. Poor housing and health: the long term health consequences of housing deprivation during childhood. School for Policy Studies, University of Bristol. Available at http://www.hel.fi/tietokeskus/tutkimuksia/enhr2000/ws13/ws13_gordon.pdf. Accessed November 8, 2001.
- 9.Verma N, Mangum G, Cookson C. Poverty in Utah 2000: A Snapshot of Income, Housing, Health, and Welfare Issues in Utah. 2nd ed. Salt Lake City, Utah: Utah Issues Center for Research and Action; 2001.
- 10.NAHASDA Web site. Available at: http://www-domino.hud.gov/IHP/newhome.nsf?OpenDatabase. Accessed November 8, 2001.
- 11.Brugge D. Grassroots epidemiology in public housing [comment]. Harvard Health Rev [serial online]. Fall 2000. Available at: http://www.hsph.harvard.edu/review/comment.html. Accessed April 5, 2002.
- 12.Environmental Health Watch Web site. Asthma/Healthy House: HUD Roach Project. Available at: http://www.ehw.org/asthma/asth_HUDroach_sum.htm. Accessed January 15, 2002.
- 13.Stewart JY. Hahn plans trust fund for affordable housing. Los Angeles Times. January 17, 2002:B1.
- 14.CEHRC Web site. Available at www.aeclp.org/cehrc.html. Accessed January 10, 2002.
- 15.Environmental Health Watch Web site. Asthma/lead poisoning: A Better Start Project. Available at: http://www.ehw.org/Lead/LEAD_Better_Start1.htm. Accessed January 15, 2002.
- 16.Environmental Health Watch Web site. Asthma/lead: Lead+Asthma Project. Available at: http://www.ehw.org/Asthma/ASTH_Lead+Asthma3.htm. Accessed January 15, 2002.
- 17.Concern, Inc. Sustainability in Action. Trimble, Ohio: Rural Action; 1997: 79–80.