Abstract
Objectives. We assessed the influence of changes in primary care and hospital supply on rates of ambulatory care–sensitive (ACS) hospitalizations among adults in Brazil.
Methods. We aggregated data on nearly 60 million public sector hospitalizations between 1999 and 2007 to Brazil's 558 microregions. We modeled adult ACS hospitalization rates as a function of area-level socioeconomic factors, health services supply, Family Health Program (FHP) availability, and health needs by using dynamic panel estimation techniques to control for endogenous explanatory variables.
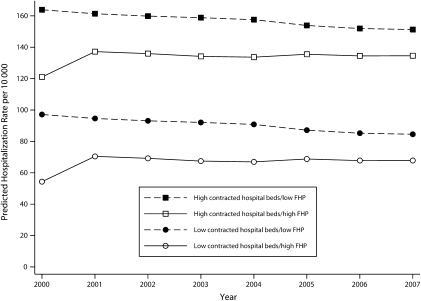
Results. The ACS hospitalization rates declined by more than 5% annually. When we controlled for other factors, FHP availability was associated with lower ACS hospitalization rates, whereas private or nonprofit hospital beds were associated with higher rates. Areas with highest predicted ACS hospitalization rates were those with the highest private or nonprofit hospital bed supply and with low (< 25%) FHP coverage. The lowest predicted rates were seen for areas with high (> 75%) FHP coverage and very few private or nonprofit hospital beds.
Conclusions. These results highlight the contribution of the FHP to improved health system performance and reflect the complexity of the health reform processes under way in Brazil.
Hospitalizations for ambulatory care–sensitive (ACS) conditions have been used to monitor health system performance in the United States and in several European countries.1–3 The idea behind the indicator is that hospitalizations for certain health problems represent a failure of the health system to provide access to good quality primary care, which should have detected the condition early in its progression, reduced its severity, or prevented the appearance of complications, thus obviating the need for hospitalization. Ambulatory care–sensitive hospitalization rates have been associated with primary care access and quality in several countries, including Australia, Canada, Spain, and the United States.4–9 However, these measures have rarely been used to study health system performance in low- and middle-income countries.
Several reasons exist for seeking a tool to assess primary care effectiveness at this time in Brazil. These reasons include the ongoing process of developing the national health system, which has been taking place since 1988.10 In addition, since 1994 the country has rolled out the Family Health Program (FHP) as a new, robust model of community-based primary health care explicitly designed to provide accessible, first-contact, comprehensive, and whole-person care that is coordinated with other health and social services and takes place within the context of families and communities. Each FHP team is multiprofessional and contains at least 1 physician, 1 nurse, 1 medical assistant, and 4 to 6 community health agents. Teams are organized by geographic regions and with a specific territory containing approximately 3500 people per team. The program enrolls the local population and uses local health data to plan health services and prevention efforts.11 All services and some medications are free of charge. By 2007, FHP access expanded in nearly every municipality and now reaches nearly 93 million people.
Concomitant changes have occurred in the Brazilian hospital sector. The government pays for about 80% of all hospitalizations, which consume nearly 70% of all national health expenditures.12 Hospital care in the national health system takes place in government-owned and operated facilities (about 36% of all hospitalizations), as well as in private (about 37%) and nonprofit (about 27%) hospitals that have been contracted by the federal government.13 Main reforms have included a decrease in the private or nonprofit to public sector hospital bed ratio, changes to the payment system, and introduction of new procedures covered by the national health system.
Our objective was to assess factors associated with ACS hospitalization rates in Brazil. Our main hypothesis was that the rapid scale-up of the FHP over the past decade in Brazil should have resulted in improved capacity for primary care to resolve common population health problems. There is some evidence of the impact of the program on mortality—especially among children.14,15 FHP effects on adult morbidity should be reflected in a decrease in ACS hospitalization rates, a hypothesis for which there is preliminary evidence, at least for some conditions.16 However, to our knowledge, no previous studies have assessed the role of the FHP in relation to other factors related to ACS hospitalization rates in the country.
METHODS
We performed an ecological cross-sectional, time-series study, which pooled together 9 years (1999–2007) of cross-sections composed of all 558 Brazilian microregions for each year, for a maximum sample size of 5502 observations. Each microregion contains several of Brazil's 5564 municipalities (Brazil's smallest administrative unit) that have been grouped together to be geographically contiguous and homogeneous in terms of demography, agriculture, and transportation. Microregions were originally designed to contain at least 1 hospital within their border and to have a larger population than do individual municipalities, allowing for construction of more stable hospitalization rates over time.17
Data Source
Our principal data source was the hospitalization information system, a national administrative database used to register inpatient data in the Brazilian health system. These data include the specific condition at discharge (International Classification of Diseases, Tenth Revision [ICD-10]18 codes), patient information (age, sex, and municipality of residence), type of hospital, length of stay, and specific medical procedures performed. Each medical procedure was associated with a specific monetary amount, based on a national list that is used to pay hospitals on a prospective basis. We were thus able to link nearly 60 million hospitalizations since 1999 to information on Brazil′s municipalities and their respective microregions.19
As per other studies on ACS hospitalizations, we excluded hospitalizations related to birth, because they apply only to women, are not associated with illness, and have increased because of public policies promoting in-hospital births.20 We further limited our analysis to hospitalizations among adults, defined here as aged 20 years or older because they represent the largest proportion of hospitalizations in the country.21 We set a maximum age limit of 79 years because after a certain age it is difficult to determine whether any hospitalization was preventable and because identifying the underlying cause of the hospitalization becomes increasingly difficult with older patients.
Our earlier work defined and validated a list of ACS hospitalization conditions relevant to the epidemiological and health services environment in Brazil through systematic literature reviews, expert meetings, consultations with primary care professional organizations, and a period of open public comment on the proposed set of conditions.19 The final list (available as a supplement to the online version of this article at http://www.ajph.org) is similar to many international lists, but differs in its emphasis on conditions that can be managed in primary care (as opposed to any ambulatory care setting) and its inclusion of several infectious diseases not present on lists developed in richer countries.
The main exposure variables were the proportion, by year, of the population in the microregion with access to the FHP, and public and private or nonprofit hospital beds per 10 000 inhabitants. Confounding variables included inflation-adjusted per capita income, socioeconomic conditions (i.e., proportion of the population older than 15 years who were illiterate, proportion of households with access to clean [indoor] water and adequate sanitation), health service access (i.e., annual mean number of doctor visits per capita), and the proportion of individuals with private health insurance. We also adjusted for population health status by including a measure of premature mortality (all-cause mortality before the age of 65 years) divided into quintiles. Income and socioeconomic data were derived from the national census and from national population surveys.22–24 Health services and mortality data were from the Brazilian Ministry of Health's online data information systems.25,26 We based population data on recent intercensal estimates.27
Some independent variable data were missing for some years. We imputed missing data by using nonlinear interpolation methods that modeled within-municipality changes as a function of previous values at the municipal level and contemporaneous values at the state level. These techniques are described elsewhere.10 We then summed up all municipal-level values to the microregional level.
Data Analysis
The available data were present for each year from 1999 (the year the Brazilian government switched to the ICD-10 coding scheme) to 2007. The model to be estimated was as follows:
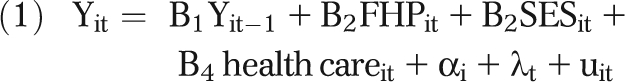 |
where Yit is the ACS hospitalization rate for microregion i in year t, Yit-1 is a lagged dependent variable reflecting the fact that the previous year's hospitalization rate is a significant predictor of contemporary rates, FHP is the percentage of the population with access to the FHP, SES is the socioeconomic conditions in each microregion in each year, health care represents the supply of health services, and uit is the error. The time-specific effect, λt, is equivalent to a dummy variable for each year and captures national-level policy changes, and other technologic and economic trends that affect all microregions. The fixed effect, αi, captures all unobserved, time-invariant factors, such as persistent geographical and historical differences between microregions, that might affect hospitalization rates.28
We used a linear dynamic panel data method to estimate the model.29,30 This approach was based on first-differencing the previously mentioned regression equation and used lagged dependent variables as well as past, present, and future values of independent variables as instruments for the lagged dependent variable on the right-hand side.31,32 The technique also allowed us to address the problem of endogeneity of the FHP and other independent variables by using the appropriate lags as instruments for the FHP and other independent variables in the same way that the model estimated lagged dependent variables.29 This dynamic panel model method therefore allowed a means of obtaining consistent parameter estimates while controlling for unobserved time-invariant factors, autocorrelation, and endogenous explanatory variables.33
To develop a valid model, the total number of instruments was limited to the shortest number of lags possible and the validity of instruments was tested with a Sargan test of over-identifying restrictions.34 Then we tested first- and second-order serial correlation in the first-differenced residuals by using the Arellano-Bond m1 and m2 statistics, respectively. We based the final choice of models on the significance of the coefficients for the lagged dependent variables, the Arellano-Bond tests, and the Sargan test. The most appropriate model treated all control variables, except income per capita, as endogenous. Dependent variables with 1-, 2-, or 3-year lags were included in each model and varied by outcome, on the basis of their statistical significance and the results of the tests described previously.
Finally, we compared results of our final models for ACS hospitalization rates with the sum of hospitalizations for all other conditions (non–ACS hospitalization). We predicted that primary care supply should not be associated with these outcomes, but that measures of hospital supply should be, if the mechanisms driving hospital decision-making regarding admissions processes are similar regardless of type of condition requiring hospital admission.
RESULTS
Table 1 shows the number of hospitalizations and government expenditures on these hospitalizations from 1999 to 2007. The total number of hospitalizations increased by about 2%, and hospitalizations for ACS conditions decreased by nearly 17%. Hospitalizations for all other (non–ACS) conditions increased by nearly 10% during this time, resulting in a 5% decrease in the share of all hospitalizations that were considered ACS to about a quarter of all hospitalizations in 2007.
TABLE 1.
Ambulatory Care–Sensitive Hospitalizations in Relation to Other Hospitalizations and Related Expenditures for Adults Aged 20 to 79 Years: Brazil, 1999–2007
| Public-Sector Hospitalizationsa |
Government Expenditures on Hospitalizationsb |
|||||||||
| Year | Total No., Millions | No. of ACS Hospitalizations, Millions | No. of Non-ACS Hospitalizations, Millions | ACS Hospitalizations per Total, % | Total Hospitalizations, Millions of Reaisa | ACS Hospitalizations, Millions of Reais | Non-ACS Hospitalizations, Millions of Reais | ACS Hospitalizations per Total, % | ACS Hospitalization Average Expenditure, Reais | Non-ACS Hospitalization Average Expenditure, Reais |
| 1999 | 6.52 | 1.92 | 4.60 | 29.47 | 2886.95 | 654.03 | 2232.92 | 22.65 | 340.64 | 485.42 |
| 2000 | 6.66 | 1.90 | 4.76 | 28.53 | 2690.82 | 609.60 | 2081.22 | 22.65 | 320.84 | 437.23 |
| 2001 | 6.59 | 1.87 | 4.72 | 28.35 | 2897.75 | 656.67 | 2241.09 | 22.66 | 351.16 | 474.81 |
| 2002 | 6.79 | 1.83 | 4.96 | 27.01 | 2893.58 | 617.23 | 2276.35 | 21.33 | 337.29 | 458.94 |
| 2003 | 6.80 | 1.78 | 5.02 | 26.19 | 3330.93 | 677.35 | 2653.58 | 20.34 | 380.53 | 528.60 |
| 2004 | 6.74 | 1.75 | 5.00 | 25.89 | 3424.33 | 704.64 | 2719.69 | 20.58 | 402.65 | 543.94 |
| 2005 | 6.62 | 1.67 | 4.95 | 25.19 | 4033.20 | 838.28 | 3194.91 | 20.78 | 501.96 | 645.44 |
| 2006 | 6.62 | 1.64 | 4.98 | 24.83 | 3895.80 | 785.27 | 3110.54 | 20.16 | 478.82 | 624.61 |
| 2007 | 6.63 | 1.60 | 5.03 | 24.09 | 4141.95 | 820.17 | 3321.78 | 19.80 | 512.61 | 660.39 |
| Difference 1999 to 2007 | 0.12 | −0.32 | 0.44 | −5.38 | 1255.00 | 166.143 | 1088.86 | −2.85 | 171.97 | 174.98 |
| Change, % | 1.8 | −16.8 | 9.57 | … | 43.47 | 25.40 | 48.76 | … | 50.48 | 36.05 |
Note. ACS = ambulatory care–sensitive. Ellipses indicate that data were not available.
Excluded hospitalizations related to births. Included all hospitalizations in public and private and nonprofit contracted hospitals reimbursed by the federal government.
Inflation-adjusted and expressed in 1999 constant Brazilian reais.
Inflation-adjusted expenditures for all hospitalizations increased by 43% to a total of 4.1 billion Brazilian reais (slightly less than US $2 billion) during this period. Total expenditures for ACS conditions increased by about a quarter, which was less than the increase for other conditions (49%), and which resulted in a 2.8% reduction in the share of expenditures going to ACS hospitalizations in 2007. The average expenditure per ACS hospitalization increased by about 50% to 512 Brazilian reais, and the average expenditure per non–ACS hospitalization increased by 36% to 660 Brazilian reais.
Table 2 presents descriptive data on study variables. Mean income per capita rose slightly over time, and other improvements in markers of living conditions included increased percentage of houses with indoor water and reduced illiteracy rates. The FHP expanded coverage from 13% to about 64% of the Brazilian population, and the average yearly number of medical consultations per capita increased nearly 6-fold. The total number of hospital beds shrank overall, primarily because of a large reduction in the private–nonprofit sector, accompanied by an 11% increase of hospital beds in the public sector. The number of families with private health insurance also increased.
TABLE 2.
Variables in Study of the Influence of Primary Care and Hospital Supply on Ambulatory Care–Sensitive Hospitalizations Among Adults, Mean Values and Changes Over Time: Brazilian Microregions, 1999–2007
| Variable | 1999, Mean (SD) | 2007, Mean (SD) | Change 1999–2007, Difference (Total % Change) | Mean Annual % Change 1999–2007a |
| Income per capita, reais | 109.67 (140.60) | 206.10 (276.49) | 96.43*** (87.93) | … |
| Clean water, % of households | 10.11 (8.83) | 11.25 (9.26) | 1.14*** (11.28) | … |
| Illiteracy, % of population > 15 y | 3.39 (3.65) | 2.47 (2.55) | −0.91*** (−26.84) | … |
| Family Health Program, % of population | 12.97 (15.73) | 64.50 (25.03) | 51.53*** (397.30) | … |
| Hospital beds, per 10 000 | ||||
| Public hospital | 7.69 (8.87) | 8.55 (7.57) | 0.86** (11.18) | … |
| Private or nonprofit hospital | 21.57 (18.86) | 7.77 (9.65) | −13.80*** (−63.98) | … |
| Private health insurance, % of population | 7.00 (9.20) | 8.46 (9.60) | 1.46*** (20.86) | … |
| Medical consultations, per capita | 0.25 (0.10) | 1.72 (0.64) | 1.47*** (588.00) | … |
| Premature mortality,b per 100 000 | ||||
| Male | 57.14 (19.02) | 51.72 (12.93) | −5.42*** (−9.49) | … |
| Female | 31.93 (11.26) | 26.84 (8.02) | −5.09*** (−15.94) | … |
| ACS hospitalizationsc | ||||
| Total | 224.19 (100.83) | 151.33 (65.04) | −72.85*** (−32.49) | −4.51 |
| Male | 204.84 (91.56) | 138.73 (57.93) | −66.11*** (−32.27) | −4.30 |
| Female | 243.69 (113.50) | 164.19 (74.74) | −79.49*** (−32.62) | −4.70 |
| Ages 20–59 y | 142.07 (67.23) | 93.22 (41.41) | −48.84*** (−34.38) | −4.89 |
| Ages 60–69 y | 595.62 (282.45) | 383.49 (160.42) | −212.12*** (−35.61) | −5.11 |
| Ages 70–79 y | 993.99 (480.67) | 724.64 (297.97) | −296.35*** (−29.81) | −3.20 |
| Non–ACS hospitalizationsb | ||||
| Total | 495.99 (165.40) | 449.50 (125.77) | −46.48*** (−9.37) | −1.39 |
| Male | 457.65 (195.24) | 417.14 (148.07) | −40.51*** (−8.85) | −1.40 |
| Female | 534.68 (165.23) | 482.37 (120.75) | −52.32*** (−9.79) | −1.38 |
| Ages 20–59 y | 451.94 (152.05) | 403.44 (111.06) | −48.49*** (−10.73) | −1.55 |
| Ages 60–69 y | 704.26 (272.18) | 648.15 (215.71) | −56.10*** (−7.97) | −1.30 |
| Ages 70–79 y | 889.85 (335.86) | 880.18 (292.82) | −9.66 (−1.09) | −0.30 |
Note. ACS = ambulatory care—sensitive. Ellipses indicate that data were not available.
Results from Poisson regression of the form log(# of hospitalizations) = B0+B1(year), where year is a linear term ranging from 0 (1999) to 9 (2007), and the mean annual percentage change = 100 [exp(B1)-1]. Population size (by sex or age group) is used as an offset.
Premature mortality is defined as < 65 y.
All government and contracted hospitals, per 10 000.
*P < .05; **P < .01; ***P < .001.
The bottom panel of Table 2 presents data on hospitalization rates. The ACS hospitalization rates declined by about a third, with an average yearly reduction of 4.5%. Rates for women were slightly higher than were those for men, although this is mostly attributable to differences in age distributions between the 2 groups. The ACS hospitalization rates for the oldest population were nearly 7 times higher than were those for the youngest age group. Non–ACS hospitalization rates were generally higher than were ACS hospitalization rates for each sex and age group and declined more slowly—about 10% overall with a yearly mean percentage change of 1.4%.
Table 3 presents results from regression models explaining changes in ACS hospitalization rates over time. The first column contains results for all hospitalizations. The model shows a negative relationship between the highest levels of FHP coverage and ACS hospitalization rates. This pattern is repeated for the male-only model in column 2. For women, both the middle and high levels of FHP coverage were significant and revealed a dose–response relationship. In the age-stratified models, both the middle and highest levels of FHP coverage were significant for the oldest groups showing a dose–response relationship similar to that seen in sex-stratified models. The magnitude of the FHP terms increased with each age group and in the oldest group was nearly 10 times higher than in the group aged 20 to 59 years. In all models, private hospital beds were statistically significant, positive, and of a similar magnitude; the 95% confidence intervals overlapped in all but the age 20 to 59 years model. All models, except that for ages 20 to 59 years, met all the assumptions of the dynamic model (m1 test was significant; m2 test was not significant; and the Sargan test was not significant).
TABLE 3.
Predictors of Ambulatory Care–Sensitive Hospitalization Rates per 10 000 Adults, by Sex and Age: Brazilian Microregions, 1999–2007
| Alla (n = 3905) | Men (n = 3905) | Womenb (n = 4463) | 20–59 y (n = 3905) | 60–69 y (n = 3905) | 70–79c y (n = 3347) | |
| Family Health Program coverage | ||||||
| 0%–24% (Ref) | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Low (25%–49%) | −0.35 (-3.95, 3.26) | 0.06 (-3.62, 3.74) | −2.31 (-6.19, 1.57) | 0.12 (-2.73, 2.97) | −4.72 (-16.53, 7.09) | −19.21 (-44.55, 6.14) |
| Middle (50%–74%) | −3.46 (-8.10, 1.17) | −2.72 (-7.35, 1.91) | −6.24** (-10.87, -1.62) | −1.59 (-5.19, 2.00) | −18.1* (-32.61, -3.60) | −41.21** (-72.23, -10.19) |
| High (75%–100%) | −10.73*** (-16.14, -5.33) | −9.68*** (-15.14, -4.22) | −14.16*** (-20.39, -7.93) | −7.63*** (-11.92, -3.34) | −33.92*** (-50.84, -17.00) | −67.2*** (-103.06, -31.35) |
| Hospital beds per 10 000 | ||||||
| Public | 0.00 (-0.51, 0.50) | −0.02 (-0.33, 0.28) | −0.06 (-0.44, 0.32) | 0.12 (-0.35, 0.59) | 0.54 (-0.30, 1.38) | −2.21* (-4.37, -0.05) |
| Private or nonprofit | 0.26** (0.09, 0.42) | 0.28*** (0.12, 0.44) | 0.25** (0.06, 0.43) | 0.19** (0.05, 0.32) | 0.86** (0.27, 1.46) | 1.49** (0.42, 2.56) |
| m1 test (Z-value) | −8.71*** | −6.04*** | −9.35*** | −7.20*** | −8.73*** | −9.51*** |
| m2 test (Z-value) | −1.10 | −1.72 | −1.27 | −1.11 | −1.93 | 0.39 |
| Sargan test χ2 (df) | 411.1 (366) | 403.7 (366) | 419.6 (377) | 416.3 (366)* | 399.7 (366) | 360.5 (318) |
Table presents B coefficients and robust 95% confidence intervals in parentheses. All models controlled for log income per capita, clean water, illiteracy, health insurance, medical consultations per capita, premature mortality, and year effects. Dynamic models also included 1- and 2-year lagged dependent variables and treated all variables except for income as endogenous. M1 and m2 are tests for the first-order and second-order serial correlation in the first-differenced residuals. Sargan is a test of the over-identifying restrictions, under the null of instruments’ validity (with 2-step estimator).
The best fit for the model for women included only a 1-year lagged dependent variable.
The best fit for the model for the group aged 70 to 79 years included 1-, 2-, and 3-year lagged dependent variables.
*P < .05; **P < .01; ***P < .001.
Table 4 presents analyses of non–ACS hospitalization rates. In all models, the FHP variables were not statistically significant, whereas the coefficient for the private or nonprofit hospitals was significant and positive. Note that only the models for the oldest age groups, those aged 60 to 69 years and 70 to 79 years, met all the specification tests for dynamic panel models. Nevertheless, each model presented similarly consistent results.
TABLE 4.
Predictors of Non–Ambulatory Care–Sensitive Hospitalization Rates per 10 000 Adults, by Age: Brazilian Microregions, 1999–2007
| Alla (n = 3905) | Men (n = 3905) | Womenb (n = 4463) | 20–59 y (n = 3905) | 60–69 y (n = 3905) | 70–79c y (n = 3347) | |
| Family Health Program coverage | ||||||
| 0%–24% (Ref) | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Low (25%–49%) | 5.55 (-3.78, 14.89) | 1.41 (-7.11, 9.93) | 1.1 (-8.42, 10.61) | 5.71 (-3.34, 14.77) | 4.01 (-13.44, 21.47) | 1.58 (-26.09, 29.25) |
| Middle (50%–74%) | 2.21 (-8.79, 13.20) | −2.99 (-13.59, 7.61) | −5.23 (-16.71, 6.25) | 3.14 (-7.31, 13.59) | −3.8 (-23.14, 15.54) | −9.26 (-42.45, 23.93) |
| High (75%–100%) | 1.2 (-15.18, 17.58) | −5.21 (-21.20, 10.78) | −4.91 (-19.62, 9.80) | 4.96 (-10.74, 20.67) | −12.15 (-43.73, 19.42) | −32.72 (-76.37, 10.94) |
| Hospital beds per 10 000 | ||||||
| Public | −0.48 (-1.48, 0.52) | −0.43 (-1.75, 0.89) | −0.87 (-1.99, 0.24) | −0.61 (-1.41, 0.19) | 1.7 (-2.98, 6.39) | 1.65 (-5.81, 9.10) |
| Private or nonprofit | 0.95** (0.36, 1.54) | 0.72* (0.11, 1.33) | 1.13*** (0.75, 1.52) | 0.99*** (0.45, 1.52) | 1.18* (0.19, 2.17) | 1.45*** (0.62, 2.28) |
| m1 test (Z-value) | −5.87*** | −4.52*** | −9.56*** | −5.65*** | −5.20*** | −6.63*** |
| m2 test (Z-value) | −0.721 | −0.729 | −0.782 | −0.634 | −0.038 | 0.687 |
| Sargan test χ2 (df) | 440.94 (366)** | 427.51 (366)* | 449.05 (377)** | 445.79 (366)* | 402.42 (366) | 358.81 (318) |
Table presents B coefficients and robust 95% confidence intervals in parentheses. All models controlled for log income per capita, clean water, illiteracy, health insurance, medical consultations per capita, premature mortality, and year effects. Dynamic models also included 1- and 2-year lagged dependent variables and treated all variables except for income as endogenous. M1 and m2 are tests for the first-order and second-order serial correlation in the first-differenced residuals. Sargan is a test of the over-identifying restrictions, under the null of instruments’ validity (with 2-step estimator).
The best fit for the model for women only included a 1-year lagged dependent variable.
The best fit for the model for the group aged 70 to 79 years included 1-, 2-, and 3-year lagged dependent variables.
*P < .05; **P < .01; ***P < .001.
Figure 1 shows predicted ACS hospitalization rates adjusted for all variables contained in model 1 of Table 3. Predicted ACS hospitalization rates were highest (about 160/10 000) for a microregion with a private or nonprofit hospital bed ratio of 100 per 10 000 population and with less than 25% FHP coverage. The predicted ACS hospitalization rates dropped by about 10% for a high private or nonprofit hospital microregion with high (more than 75%) FHP coverage, although this proportion narrowed over time. In contrast, microregions with very few (less than 10/10 000) private or nonprofit hospital beds and low FHP coverage had about 35% lower predicted ACS hospitalization rates, and the lowest rates were found for low private or nonprofit hospital, high FHP microregions (about 70/10 000). Thus, in areas of both high and low private or nonprofit hospital supply, higher FHP availability was associated with substantially lower ACS hospitalization rates.
FIGURE 1.
Predicted ambulatory care–sensitive hospitalization rates, by Family Health Program coverage and contracted private or nonprofit hospital beds per 10 000 adults: Brazilian microregions, 1999–2007.
Notes. FHP = Family Health Program. High versus low FHP refers to 75% or higher population coverage versus 25% or less. High hospitals refers to high supply of contracted private or nonprofit hospital beds (100 per 10 000 or more) versus low (10 per 10 000 or fewer) supply. Results are predicted from dynamic panel model with control for log income per capita, indoor water availability, illiteracy, health insurance, medical consultations per capita, premature mortality, and lagged dependent variables.
DISCUSSION
This study has shown that ACS hospitalization rates have declined sharply in Brazil over the past decade. Some of this decline may be attributed to the expansion of the FHP, an integrated primary care network that has substantially increased access to basic medical services throughout the country. At the same time, hospital-level factors such as the proportion of contracted (private or nonprofit) hospitals were associated with higher ACS hospitalization rates, even when other factors were controlled.
Several possible explanations exist for the observed results. First, the rapid expansion of the FHP may have indeed resulted in improved adult health, reducing the need for hospital admission through better diagnosis, treatment, or management of the chronic diseases that make up the bulk of the ACS hospitalization list. There is evidence that the FHP is associated with better management of some chronic conditions, and since 2004 a systematic effort to develop clinical guidelines for identification, diagnosis, and treatment of such diseases, including provision of essential drugs (free to the consumer) for control of hypertension and diabetes.35,36 Further, the FHP uses community health agents to actively screen populations (in their homes) for risk factors such as smoking and hypertension; to refer high-risk individuals to the health center; to develop group interventions to aid in smoking cessation, improve physical activity, and manage diabetes; and to develop community-based health education programs.35 Although the quality and intensity of these activities varies by location, this study could serve as an indication that they may reduce the need for hospitalization for at least some ACS conditions.37,38
At the same time, the consistent association of ACS hospitalization rates with the supply of private or nonprofit hospital beds questions the simple interpretation of attributing the magnitude of ACS hospitalization rates to access and quality of primary care. In Brazil, hospitals vary enormously in terms of their ownership, administration, and receptivity to market pressures.39 There has been some evidence of induced demand in Brazil for certain procedures among private and nonprofit hospitals, and the fact that both ACS and non–ACS conditions were positively associated with private or nonprofit but not public sector hospital supply strengthens the case for induced demand.40 Alternatively, a greater supply of private and nonprofit sector hospital beds may be present where the FHP itself is weaker. Although the growth in FHP access has occurred throughout the entire country, it has been functioning longer primarily in smaller, more rural municipalities, even though an explicit policy to expand the program to large urban areas has been in place since 2004.41 Previous studies have shown that it takes time before the FHP becomes consolidated within a municipality and this learning curve has been associated with poorer outcomes.10,42
Changes in the relative prices associated with different hospital procedures may also explain some of the decline in ACS hospitalization rates, as government payments for procedures associated with lower-complexity conditions (several of which are on the ACS hospitalization list) are less than are those associated with more complex conditions.43 Although hospitals may have favored admissions for conditions that might be more lucrative, this fact would not explain why private or nonprofit hospitals were found to be associated with higher ACS hospitalization rates than public hospitals, because both are paid according to the same government rates.
Finally, declining ACS hospitalization rates may also be related to a shifting of tasks from hospitals to ambulatory specialist care. This phenomenon could be interpreted as improved management for such conditions if they mean avoiding unnecessary hospital-based care. Although considerable work has been conducted in examining primary care and the hospital sector in Brazil, few studies have examined providers of secondary care, so little evidence exists on which to test this hypothesis.
Study Strengths and Limitations
Strengths of this study include the fact that all public sector hospitalizations for adults were included in the analysis. The length of follow-up and use of microregions allowed for calculation of stable hospitalization rates over nearly a decade. Statistical analyses adjusted for the endogenous nature of the main exposure variable (FHP coverage) and other independent variables. Although the results of these models may be more conservative than traditional fixed-effects models, they are more robust to a number of biases inherent in many previous studies of the FHP and its effects on health outcomes.
The main weakness of the study is the ecological nature of its design; we could not distinguish between those hospitalizations that occurred among individuals who were served by the FHP and those who were not. In fact, even at the individual level, there is currently no standard way to reliably develop a user profile within the national health system, although efforts are under way to implement a national health identification card. We were not able to test all possible factors associated with the need for hospitalization, nor were we able to adjust at the individual level for case mix. Instead, we assessed the overall public health impact of ACS hospitalization rates on the national level as a whole and used aggregate values from the microregion to control for health needs. The size of the database (nearly 60 million hospitalizations) and the lack of a unique user identification also made it unfeasible to use linkage methods to distinguish between first-time admissions and subsequent readmissions or to use other approaches such as multilevel models. Finally, we used the total population as our denominator, and this method may have underestimated all hospitalization rates, as a proportion of the population may not have been at risk for hospitalization in the public sector because they had private health insurance. However, even those with private health insurance are not excluded from the public health system, and controlling for this phenomenon would require many additional assumptions.
Conclusions
In addition to potentially informing health policy in Brazil, this study may also have several implications for other countries. First, as Brazil and other middle- and low-income countries follow World Health Organization guidance to move to expand and consolidate primary health care as the basis of their health systems, measures such as ACS hospitalization rates are likely to become increasingly important to analyze trends over time, explore geographic variations, and identify changes in health care needs among aging populations. Second, although the use of existing administrative data can shed light on processes of health care reform, within such complex and rapidly changing environments interpretation of changes in ACS hospitalization rates may require greater care than might be the case for more established health care systems in richer countries. For example, rates of change in ACS hospitalizations may need to be assessed independently of absolute levels. Third, it is essential to take public, private, and nonprofit sector providers of primary and hospital care into account when one is conducting national-level assessments of health system performance. In countries without a national health system and corresponding data, this will require use of ongoing surveys and other techniques to adequately capture changes at the facility and population levels. Despite these challenges, we hope that continued adaptation and demonstration of tools such as ACS hospitalization rates will further encourage their use in assessment and improvement of primary care and health system performance worldwide.
Acknowledgments
The study was supported by the Brazilian Ministry of Health.
Thanks to Mario Piscoya for database management and Andressa Costa for research assistance. The authors also thank Claunara Mendonça and the members of the Internações para Condições Sensíveis à Atençào Primaria–Brazil project for comments and suggestions on earlier versions of the article.
Human Participant Protection
This study was exempt from review because it involved the collection and study of existing data that were publicly available and in which the information was recorded in such a manner that individuals cannot be identified, directly or through identifiers linked to the individuals.
References
- 1.Billings J, Anderson GM, Newman LS. Recent findings on preventable hospitalization. Health Aff (Millwood). 1996;15(3):239–249 [DOI] [PubMed] [Google Scholar]
- 2.Billings J, Zeitel L, Lukomnik J, Carey TS, Blank AE, Newman L. Impact of socioeconomic status on hospital use in New York City. Health Aff (Millwood). 1993;12(1):162–173 [DOI] [PubMed] [Google Scholar]
- 3.Bindman AB, Grumbach K, Osmond D. Preventable hospitalizations and access to health care. JAMA. 1995;274(4):305–311 [PubMed] [Google Scholar]
- 4.Menec VH, Sirski M, Attawar D, Katz A. Does continuity of care with a family physician reduce hospitalizations among older adults? J Health Serv Res Policy. 2006;11(4):196–201 [DOI] [PubMed] [Google Scholar]
- 5.Roos LL, Walld R, Uhanova J, Bond R. Physician visits, hospitalizations, and socioeconomic status: ambulatory care sensitive conditions in a Canadian setting. Health Serv Res. 2005;40(4):1167–1185 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Magan P, Otero A, Alberquilla A, Ribera JM. Geographic variations in avoidable hospitalizations in the elderly, in a health system with universal coverage. BMC Health Serv Res. 2008;8:42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Marquez-Calderon S, Rodriguez del Aguila MM, Perea-Milla E, Ortiz J, Bermudez-Tamayo C. Factors associated with hospitalization for ambulatory care sensitive conditions in municipalities [in Spanish]. Gac Sanit. 2003;17(5):360–367 [DOI] [PubMed] [Google Scholar]
- 8.Valenzuela Lopez MI, Gaston Morata JL, Melguizo Jimenez M, Valenzuela Lopez MM, Bueno Cavanillas A. To identify primary care interventions that reduce hospitalisation of people over 65 due to ambulatory care sensitive conditions [in Spanish]. Aten Primaria. 2007;39(10):525–532 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ansari Z, Laditka JN, Laditka SB. Access to health care and hospitalization for ambulatory care sensitive conditions. Med Care Res Rev. 2006;63(6):719–741 [DOI] [PubMed] [Google Scholar]
- 10.Guanais FC, Macinko J. The health effects of decentralizing primary care in Brazil. Health Aff (Millwood). 2009;28(4):1127–1135 [DOI] [PubMed] [Google Scholar]
- 11.Elias PE. Public healthcare policy in Brazil: the Brazilian society and the construction of universality in the Brazilian health system [in Portuguese]. Cien Saude Colet. 2008;13(Suppl 2):2023–2026, discussion 2026–2028 [DOI] [PubMed] [Google Scholar]
- 12.La Forgia GM, Harding A. Public-private partnerships and public hospital performance in Sa˜o Paulo, Brazil. Health Aff (Millwood). 2009;28(4):1114–1126 [DOI] [PubMed] [Google Scholar]
- 13.de Carvalho DM. Hospital care financing in Brazil [in Portuguese]. Cien Saude Colet. 2007;12(4):879–892 [DOI] [PubMed] [Google Scholar]
- 14.Macinko J, Marinho de Souza Mde F, Guanais FC, da Silva Simoes CC. Going to scale with community-based primary care: an analysis of the family health program and infant mortality in Brazil, 1999-2004. Soc Sci Med. 2007;65(10):2070–2080 [DOI] [PubMed] [Google Scholar]
- 15.Aquino R, de Oliveira NF, Barreto ML. Impact of the family health program on infant mortality in Brazilian municipalities. Am J Public Health. 2009;99(1):87–93 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Guanais F, Macinko J. Primary care and avoidable hospitalizations: evidence from Brazil. J Ambul Care Manage. 2009;32(2):115–122 [DOI] [PubMed] [Google Scholar]
- 17.Divisa˜o do Brasil em mesorregiões e microrregiões geográficas. Rio de Janeiro, Brazil: Instituto Brasileiro de Geografia e Estatística; 1992. Available at: http://biblioteca.ibge.gov.br. Accessed March 19, 2010 [Google Scholar]
- 18.International Classification of Diseases, Tenth Revision. Geneva, Switzerland: World Health Organization; 2007 [Google Scholar]
- 19.Alfradique ME, Bonolo Pde F, Dourado I, et al. Ambulatory care sensitive hospitalizations: elaboration of Brazilian list as a tool for measuring health system performance (Project ICSAP–Brazil) [in Portuguese]. Cad Saude Publica. 2009;25(6):1337–1349 [DOI] [PubMed] [Google Scholar]
- 20.Goldani MZ, Barbieri MA, Silva AAM, Bettiol H. Trends in prenatal care use and low birthweight in Southeast Brazil. Am J Public Health. 2004;94(8):1366–1371 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Pan American Health Organization Brazil: health situation analysis and trends summary. Available at: http://www.paho.org/english/dd/ais/cp_076.htm. Accessed March 30, 2010 [Google Scholar]
- 22.Economic and Social Research Council International Microdata Scoping Studies Project: Brazil. January 2007. Available at: http://www.esrcsocietytoday.ac.uk/ESRCInfoCentre/IDF/conpapers/default.aspx. Accessed March 30, 2010
- 23.Brazilian Institute of Geography and Statistics Banco multidimensional de estatísticas. 2009. Available at: http://www.ibge.gov.br. Accessed March 30, 2010
- 24.Instituto de Pesquisa Econômica Aplicada Dados macroeconômicos e regionais. Available at: http://www.ipeadata.gov.br. Accessed December 15, 2009
- 25.Ministry of Health of Brazil–Departamento de Atença˜o Básica Saúde da Família no Brasil: uma análise de indicadores selecionados. Brasília, DF, Brazil: Minstério da Saúde do Brasil; 2006 [Google Scholar]
- 26.Ministry of Health of Brazil Datasus. Sistema de informações sobre mortalidade (SIM). Secretaria de Vigilancia em Saude. Available at: http://tabnet.datasus.gov.br. Accessed March 4, 2010
- 27.Brazilian Institute of Geography and Statistics Projeça˜o da populaça˜o do Brasil por sexo e idade 1980-2050. Revisa˜o 2008. Rio de Janeiro, Brazil: Informaça˜o Demográfica e Socioeconômica, N; 24; 2008 [Google Scholar]
- 28.Green WH. Econometric Analysis. 5th ed New York, NY: Macmillan Publishing; 2003 [Google Scholar]
- 29.Arellano M, Bond S. Some tests of specification for panel data: Monte Carlo evidence and an application to employment equations. Rev Econ Stud. 1991;58:277–297 [Google Scholar]
- 30.Wawro G. Estimating dynamic panel data models in political science. Polit Anal. 2002;10(1):25–48 [Google Scholar]
- 31.Wooldridge J. Econometric Analysis of Cross Section and Panel Data. Cambridge, MA: MIT Press; 2002 [Google Scholar]
- 32.Bond S. Dynamic panel data models: a guide to microdata methods and practice. Oxford, England: Institute for Fiscal Studies and Nuffield College; 2002. Available at: http://www.cemmap.ac.uk/wps/cwp0209.pdf. Accessed March 30, 2010 [Google Scholar]
- 33.Roodman D. How to do xtabond2: an introduction to difference and system GMM in Stata. Stata J. 2009;9(1):86–136 [Google Scholar]
- 34.Windmeijer F. A finite sample correction for the variance of linear efficient two-step GMM estimators. J Econom. 2005;126:25–51 [Google Scholar]
- 35.Ministry of Health of Brazil, Secretaria de Atença˜o à Saúde, Departamento de Atença˜o Básica Clinical prevention of cardiovascular, cerebrovascular, and renal diseases [in Portuguese]. Cadernos de Atença˜o Básica. 2006:14 [Google Scholar]
- 36.Rodrigues MA, Facchini LA, Piccini RX, et al. Use of primary care services by elderly people with chronic conditions, Brazil. Rev Saude Publica. 2009;43(4):604–612 [DOI] [PubMed] [Google Scholar]
- 37.Facchini LA, Piccini RX, Tomasi E, et al. Evaluation of the effectiveness of Primary Health Care in South and Northeast Brazil: methodological contributions [in Portuguese]. Cad Saude Publica. 2008;24(Suppl 1):S159–S172 [DOI] [PubMed] [Google Scholar]
- 38.Souza ML, Garnelo L. “It sure ain't easy!”: an ethnographic study of primary health care for patients with hypertension and/or diabetes in Manaus, Amazonas State, Brazil [in Portuguese]. Cad Saude Publica. 2008;24(suppl 1):S91–S99 [DOI] [PubMed] [Google Scholar]
- 39.La Forgia GM, Couttolenc BF. Hospital Performance in Brazil: The Search for Excellence. Washington, DC: The World Bank; 2008 [Google Scholar]
- 40.Castro MS, Travassos C, Carvalho MS. Impact of health services delivery on hospital admission utilization in Brazil [in Portuguese]. Rev Saude Publica. 2005;39(2):277–284 [DOI] [PubMed] [Google Scholar]
- 41.Ministry of Health of Brazil Projeto de expansa˜o e consolidaça˜o da saúde da família – PROESF. Available at: http://dtr2002.saude.gov.br/proesf. Accessed April 12, 2010
- 42.Aquino R, Barreto ML. The Family Health Program in Brazil and the adequacy of its coverage indicator [in Portuguese]. Cad Saude Publica. 2008;24(4):905–914 [DOI] [PubMed] [Google Scholar]
- 43.Levin JA. The Influence of Health Policies in the Indicators Derived From the Hospital Information System of the National Health System in Brazil [master's thesis; in Portuguese] Rio de Janeiro, Brazil: Universidade do Estado do Rio de Janeiro; 2006 [Google Scholar]