Abstract
Adult cigarette smoking prevalence trends among African Americans (AAs) and Whites are similar. However, during the decline in youth smoking that occurred between the mid-1970s and the early 1990s, the drop in smoking rates among AA adolescents was more than double that among Whites. We examined the evidence for potential explanations for this phenomenon. On the basis of our findings, we propose that racial differences in parental attitudes, religious ties, negative perceptions and experiences of the health effects of smoking, worsening poverty, increased use of food stamps, and price sensitivity were major factors contributing to the more rapid decrease in and continued lower rates of smoking among AA youths.
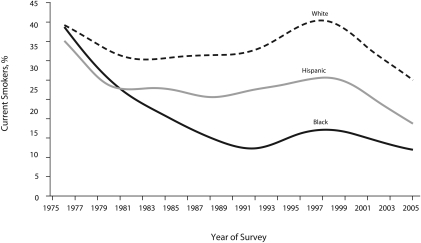
Tobacco smoking remains the leading cause of preventable death in the United States.1 African Americans (AAs) have particularly high rates of smoking-related morbidity and mortality,2 although their current smoking rates are similar to those of Whites.3,4 During the 1970s there was a substantial overall decline in teen smoking; however, the extent of the reduction differed substantially among racial and ethnic groups. Prevalence declined more rapidly among AA youths than it did among White and Hispanic youths. Smoking prevalence for AA youths continued to drop even as smoking prevalence for other groups stabilized in the 1980s.5,6 Figure 1 shows the change in past-30-day cigarette use prevalence over time across racial/ethnic groups.
FIGURE 1.
Thirty-day prevalence of cigarette use among African American, White, and Hispanic high school seniors: United States, 1976–2005.
Source. Nelson et al.7 Printed with permission.
Given nicotine's addictive power and health consequences, and given that most adult smokers began smoking in adolescence,8–10 reducing smoking among youths is a public health priority. An identification of the reasons behind the smoking decline among AA youths might inform policies and public health programming intended to reduce tobacco use among all youths. Previous studies examining the decline in smoking among AA adolescents during the 1970s and 80s7,11 speculated that alternative drug use,12 religious affiliations,13 and cigarette pricing12 were likely contributing factors in the decline. We reviewed the literature to explore these and other hypotheses that may account for the sharp decline in smoking among AA youths and the differential reduction rates between AA and White youths.
THE DECLINE IN ADOLESCENT CIGARETTE USE
The prevalence of cigarette use among adolescents in the United States decreased from the mid-1970s through the early 1980s, with remarkable declines occurring during 1976–1979 and 1980–1984.13,14 Prevalence leveled off in the mid-1980s before beginning to climb again in 1993.15–17 Trends were consistent across nationally representative studies, including National Household Surveys on Drug Abuse, High School Seniors Surveys, and the National Health Interview Survey.18
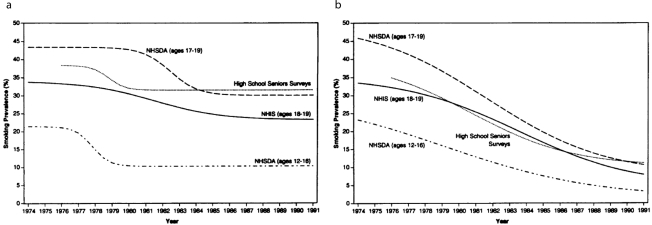
In the late 1970s stark differences began to emerge across racial and ethnic subgroups, especially between Whites and AAs. In 1977, the 30-day point prevalence for cigarette use was similar across White (38.3%), AA (36.7%), and Hispanic (35.7%) high school seniors.5,14 However, by 1985, there was a large gap in smoking prevalence between White and AA high school seniors, who were at 31.3% and 18.1%, respectively. Several studies consistently show that prevalence among White youths leveled throughout the remainder of the 1980s, while rates for AA students continued to decline5,15,18 (Figure 2), such that by 1992 White students were almost 4 times more likely to have smoked in the past 30 days than were their AA counterparts.14,17,18
FIGURE 2.
Cigarette smoking trends among (a) White adolescents and (b) African American adolescents across High School Seniors Surveys, NHSDA, and NHIS data: United States, 1974–1991.
Note. NHIS ;= ;National Health Interview Survey; NHSDA ;= ;National Household Surveys on Drug Abuse.Source. Nelson et al.18 Printed with permission.
Other studies of smoking among young adults have confirmed that as the high school seniors of the 1980s entered the young adult cohort, the decreased rates of smoking among AA young adults (aged 18–35 years) relative to Whites remained evident.3,18–20
The decline was consistent across gender17 and urbanicity; smoking rates fell for both rural and urban AAs. However, urban AA high school seniors had lower 30-day prevalence than did rural AAs.21 In 1992, the prevalence for AA urban girls had declined to 7.1%, compared with 9.4% for AA rural girls. The prevalence for urban AA boys was down to 10%, versus 20% for rural AA boys.21 Gaps in cigarette use between AA and White high school seniors also persisted regardless of urbanicity: approximately 34% of White rural boys, 33% of White rural girls, 29% of White urban boys, and 33% of White urban girls smoked during the same time period.21
LOGISTICAL CONCERNS REGARDING ACCURACY OF PREVALENCE FINDINGS
When gauging the accuracy of prevalence findings, a number of concerns present themselves, including the differential reliability of self-reported data by race/ethnicity, differential school dropout rates by race/ethnicity, and differential operationalization of variables among studies.
Differential Reliability of Self-Reports
The data from most youth smoking studies are self-reported, usually with no biochemical verification, leading to questions regarding reliability and validity.22 The validity of self-reports has been called into question several times because AA youths have been suspected of underreporting their drug use, and White youths have been suspected of overreporting it.13,23,24 Cotinine, the principal metabolite of nicotine, has been found to be a highly sensitive and specific indicator of the accuracy of self-reported tobacco use when measured in body fluids (e.g., saliva).25–27 A study by Wagenknecht et al.28 used cotinine measurement for biochemical verification and determined that although AA youths were more likely to be misclassified as nonsmokers than were White youths (5.7% vs 2.8%), the misreporting was small enough that it would not significantly bias results. A study of youths in the 7th through 10th grades that used cotinine measurement found that the validity of self-reports was generally comparable across ethnic groups,29 as have other studies.11,30 Also, the reduction in AA high school seniors reporting close friends smoking is indicative of the declining trend of youth prevalence and is a measure that youths have little reason to intentionally underreport.31
Differential Dropout Rates
Much of the data on youth smoking were collected in schools; thus, such studies did not include dropouts, absent youths, or truant youths. This limitation is a concern6,13,18,31 because dropouts and truants have significantly higher smoking rates than do those who regularly attend school or have graduated.32,33 Additionally, the dropout constituency may contribute to the differential prevalence, because AA youths have had higher dropout and truancy rates than have White youths.34–37 In the 1970s and early 1980s, about 21% of AAs aged 16 to 24 years had dropped out of high school, approximately twice the proportion of White youths.38 This trend was similar for younger adolescents29; one study found that 10% of AA eighth-graders had dropped out of school, compared with 5% of their White peers.34 AA youths had higher dropout rates and were less likely to be represented in school surveys, so the results of school surveys could not necessarily be extrapolated to AA youths who were not in school. Furthermore, truancy is a predictor of smoking onset for AA male youths,39 so prevalence of smoking rates could have been underestimated and could have actually been closer to the smoking rates among White youths.13
However, the high school dropout rate for AAs began declining in 1988.40 In 1993 the rate was 17% for AAs, only slightly higher than the rate for Whites (13%),41 which makes the findings of school surveys more generalizable to both White and AA youths.30 Also, studies that included dropout and truant youths found that AA youths were still significantly less likely to use cigarettes than were Whites.18,42–44 Even among a sample of youths in 7th through 10th grades,29 dropout rates were higher among minority youths, and smoking rates were higher among dropouts; and yet AAs still had lower smoking rates. The differential prevalence rates therefore appear to remain, even when accounting for truants and dropouts.
Differential Operationalization of Variables
Most studies of youth smoking have focused on cigarette use, the dominant form of tobacco, as the variable of interest. Therefore, “smoking” and “tobacco use” generally refer to cigarette use, although it is recognized that youths also use other forms of tobacco. There were no static criteria defining current smokers,43 although the most common definition in adolescent studies was any cigarette use within the last 30 days, casting a net wide enough to capture youths who may have been in the experimental or beginning stages of cigarette use.10,45 Most studies (e.g., those using Monitoring the Future data or government survey data) used this marker. A few studies (e.g., those using National Health Interview Survey data) strayed from past-month smoking and classified adolescents as current smokers if they had smoked at least 100 cigarettes in their lifetime and continued to smoke, a typical definition used in adult studies. One study exclusively used daily smoking status as its criterion for being a cigarette smoker.13
Although different measures were used, the patterns of changes in youth smoking remained similar across different surveys.43 In accordance with most adolescent studies, youth smoking rates usually reflect 30-day point prevalence unless otherwise noted. Adult smoking prevalence refers to having consumed 100 or more cigarettes in one's lifetime and continuing to smoke daily or occasionally. “Adolescent” and “youth” generally refer to high school seniors.
Debate still abounds surrounding the accuracy of prevalence assessments of AA youth smoking because of additional study logistics (i.e., undersampling of segregated and rural AA communities,46,47 giving socially desirable responses,48,49 and participant–interviewee dynamics49). However, between 1992 and 2006 there was a marked drop in lung cancer incidence and death rates among people aged 20 to 39 years, with a significantly steeper reduction among AA adults, mirroring the observed drop in AA youth smoking 10 to 20 years earlier. This finding provides strong evidence for an actual decline in smoking among AA youths from the 1970s through the 1990s because the differential reduction in AA young adult lung cancer cases is highly likely to be attributable to the differential decline smoking among AA youths.50
DECREASED INITIATION, INCREASED CESSATION, AND DELAYED INITIATION
The drop in AA youths’ smoking prevalence seems to be a function, in part, of decreased initiation and increased cessation. About 44% of all high school seniors reported having quit smoking in 1984. Additionally, AA initiation rates have been steadily decreasing since 1975, such that between 1979 and 1989 only 2.2% of AA youths aged 12 to 17 years reported initiating cigarette use each year, compared with 6% of White youths.33,45 A longitudinal study of youths aged 11 to 17 years who reported they had never tried cigarettes in 1989 found that AAs were significantly less likely than were Whites to have tried cigarette smoking 4 years later.51
Smoking rates for White high school seniors in 1992 (32%) and White adults aged 18 to 34 years in 1995 (29.7%) were similar, but the 1995 rate for AA adults (21%) was nearly double the 1992 rate for AA high school seniors (10%).3,19 This finding suggests that a higher proportion of AAs waited until young adulthood to initiate smoking. The prevalence of cigarette smoking among AAs aged 20 to 24 years was 47.1% in 1974; that rate dropped to 38.7% in 1983 and to 17.3% in 1990, which was below the national average.19,52 In 1978, 38.7% of AAs aged 18 to 34 years were current smokers, and that rate dropped to 21% in 1995.3 The decline in White smokers in this age group was not as steep, dropping from 37% in 1978 to 29.7% in 1995. The Centers for Disease Control and Prevention notes that this decreasing prevalence pattern is consistent with the reported decline in high school students smoking during the 1970s and 1980s—which, at first glance, discredits the delayed initiation hypothesis.19
However, evidence suggests that AAs start smoking at older ages than Whites do.53 Several retrospective and longitudinal studies of adult smokers found that AAs were more likely than were Whites to delay initiation until age 17 or later.3,54–56 Another study found that between 1970 and 1992, the proportion of AA youths who initiated smoking at ages 14, 15, or 16 years had decreased, but initiation of regular smoking among AAs aged 18 and 19 years had increased.56 More than half of the AA adult smokers in one study initiated smoking as young adults, and 40% did not begin to smoke regularly until ages 18 to 21 years.57 Other studies reported similar findings.58,59
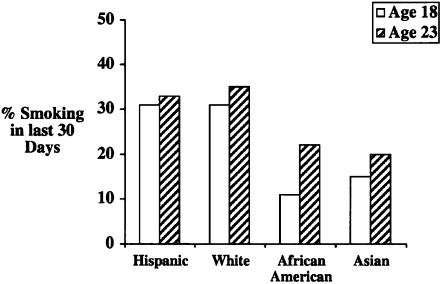
Another longitudinal study of young smokers conducted from 1985 to 1995 showed that whereas the rate for both Whites and Hispanics aged 18 years was 31%,60 AAs had the lowest rate, at 11%. However, in the 5-year transition into adulthood, by age 23 years AA youths had the biggest increase in smoking prevalence, jumping to 20%; their White and Hispanic peers only rose to 33% and 35%, respectively (Figure 3). This larger increase in smoking rates among AA young adults may have resulted from their newfound ability to afford to purchase cigarettes as they entered the workforce. Although there is evidence of delayed smoking initiation among AAs and partial “catching up” in the postschool years, the lower smoking prevalence among AAs compared with Whites appears to persist into young adulthood.
FIGURE 3.
Thirty-day smoking rates among people aged 18 and 23 years, by race/ethnicity: United States, 1990 and 1995.
Source. Fisher et al.49 Printed with permission.
FACTORS EXPLAINING THE DECLINE IN SMOKING
We have established that, compared with other racial/ethnic groups, fewer AA youths have initiated smoking, and AA youths have tended to wait longer to initiate smoking, resulting in lower smoking prevalence among AA youths. But what is causing these trends? A number of hypotheses have been proposed.
Other Forms of Tobacco, Alcohol, and Other Drugs
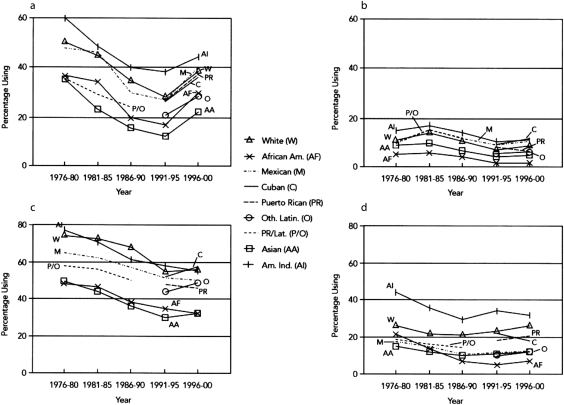
Some authors have suggested that AA youths have substituted other forms of tobacco, alcohol, or other drugs for cigarettes.11,12 However, there was an overall decline in the use of both licit and illicit drugs among AA high school seniors from the mid-1970s through the early 1990s alongside the decline in cigarette use (Figure 4).5,13,14 Cocaine was the only drug for which use increased slightly, during the mid-1970s and early 1980s.6,13 Cocaine use increased across all races, but it was lowest for AAs, reaching only 6% annual prevalence at its peak in 1983.6 AA youths usually had one of the lowest use rates across all substances,13 and use rates were not high enough to account for a shift from tobacco use.
FIGURE 4.
Prevalence of use of (a) marijuana, (b) cocaine, (c) alcohol, and (d) tobacco among high school seniors, by race/ethnicity: United States, 1976–2000.
Source. Wallace et al.6 Printed with permission.
As for other forms of tobacco, most studies focused mainly on cigarettes or smokeless tobacco, and smokeless tobacco use has always been very low among AA youths, reaching its peak of 4.5% in 1988 and 1989.5 There are few data on the use of other tobacco products (OTPs) such as cigars, pipes, bidis, and kreteks during this time period because they did not gain popularity or receive national or academic attention until the mid-1990s.8,61 National studies did not inquire about OTPs until 1999,8 but recent studies show that AA high school seniors had relatively low usage rates for cigars, bidis, pipes, and kreteks.62 AA youths were more likely to use bidis than White youths, but national AA rates were only 4.9%.61 Lower rates of general tobacco use have persisted among AA 12th graders62 despite the options of smokeless tobacco and OTPs, making it highly unlikely that the decline in AA youth smoking was caused by AA youths using OTPs.
Attitudes Toward Cigarette Use
The theory of reasoned action and the theory of planned behavior63 posit that intention is the strongest determinant for performing a behavior. They also propose that intention is influenced by a person's attitude toward performing a particular behavior and by the person's motivation to comply with the attitudes and beliefs of people who hold key roles in the person's life.
Attitude and intention are the strongest predictors for youth smoking.64,65 AA youths were significantly more likely than were White youths to have negative attitudes, beliefs, and expectations toward cigarette use; to view cigarettes as undesirable; and to have low intentions to smoke. AA youths were also more likely than were Whites to hold negative views of smokers, to disapprove of smoking, and to see smoking as a dirty habit.3,10,11,66,67
Public Health Education Efforts
Several studies have attributed the considerable drop in smoking among youths and adults to the 1964 Surgeon General's report on smoking68–70 and other public awareness efforts, including the introduction of health warnings on cigarette packs in 1966. Research specifically assessing the report's impact on youths is sparse, but Pierce and Gilpin71 have demonstrated that the amount of health-related tobacco coverage in the news reflected trends in public awareness and adult and adolescent cessation rates into the 1980s.
Furthermore, AA adolescents may be differentially affected by the public health and risk messages in antismoking programming,33 especially in campaigns specifically targeting them.71–75 Ethnically focused research is sparse for the period of interest, although a later study found that AA 10th and 12th graders had significantly higher recall of antismoking ads and reported that they were affected by antismoking ads more than Whites were.14 Studies examining differential effects of the American Legacy Foundation's “Truth” campaign found that AA youths were more likely to be affected by antitobacco advertising than were their White peers because AA youths had lower rates of smoking initiation and held stronger antitobacco views.76,77 This finding may suggest that AA youths may pay attention to, interpret, and process antitobacco media and health education efforts differently from White youths. If AA youths attended to and processed antismoking messages differently, that would be consistent with their stronger concerns about severe cigarette-related health issues.3,11,78,79
Family
Unlike White youths, parental sociodemographic factors (e.g., parent education) and socioeconomic status were not associated with smoking among AA youths.80,81 Even maternal smoking did not seem to significantly affect smoking status in AA youths.82 Rather, parental concern about smoking was one of the major correlates of cigarette use for AA youths.79,83 AA parents were more likely than were White parents to oppose smoking and to explicitly express antismoking sentiments, which may have influenced their children's attitudes.78,84–87 Their higher levels of parental involvement in smoking prevention and closer parent-child interaction and supervision were more likely to reduce the likelihood of smoking for AAs than for Whites.78,81,86,87 AA parents also monitored their children more closely, which might have allowed fewer opportunities for errant behaviors.88,89
One factor that may have particularly affected AA youths’ smoking prevalence was the rather large increase in the proportion of AA youths living in households with only the mother, which rose from 29.5% in 1970 to 51.2% in 1990 (compared with a corresponding change from 7.8% to 16.2% in White households).90 Mothers have a lower smoking prevalence and more negative views of smoking across racial groups, so the increased proportion of AA youths living in households headed by the mother may help explain AA youths’ attitudes about smoking.
Peers and Community
Peer use is one of the strongest predictors of cigarette use among adolescents, regardless of ethnicity, though AA youths were less likely to be negatively influenced by friends who smoked.64,78,82,88,91–96 AA youths were less likely than were White youths to report being affected by perception of prevalence, and they were also less likely to report having friends who engaged in smoking or drug behaviors.11,67 Perhaps, as a result of these factors, they were consequently less likely to be offered cigarettes,60 leading to fewer opportunities to begin experimenting.
The AA community and AA culture have held unfavorable views toward smoking.13,60 AA adults were more likely to consider smoking as a serious problem and concern, to favor restricting youth access to cigarettes, and to forbid smoking in their cars.3,97 Prominent AA community leaders have spoken out against cigarettes and have developed antismoking campaigns targeting the AA community.98 AA youths living in predominantly AA neighborhoods were less likely to smoke than were AAs living in predominantly White environs,99 suggesting that youth smoking was less acceptable in the AA community. A focus group study found that AA youths were more likely to believe that more White youths smoked and that AA youths considered smoking as a White activity,87 suggesting that racial/ethnic pride may have played a role as well.100
An additional factor that may have differentially affected attitudes toward smoking among AA youths was the increased visible health impact of smoking on AA adults starting in the 1970s. For example, between 1950 and 1960, age-adjusted death rates from lung cancer among AA men surpassed those among White men, and they remained more than 30% higher from the 1970s through the 1990s.3 The experience of seeing an increasing number of smoking-caused deaths in the community and among family members may have strengthened antismoking attitudes among AA youths and families since the 1970s.
Religion
Most religions have rather conservative views about substance use, so it is not surprising that the extent of religious activity served as a protective factor against cigarette use for both White and AA youths, even after controlling for key sociodemographic factors.13,101–106 The relationship was stronger for AAs,99 perhaps because AAs in this birth cohort have consistently been found to have higher rates of worship attendance and other religious activities than White youths, largely because of parental mandates.31,107–116 Furthermore, AA youths often cited moral and ethical reasons for not smoking,79 suggesting a motivation to comply with the church's antidrug tenets. Perhaps this finding is also a reflection of AA youths being more religiously involved.
Youth participation in religious activity has also been linked to positive social relationships and prosocial behavior,117,118 higher self-esteem,119 lower stress,120 successful academic work, positive ethnic identity formation, and enduring positive relationships,121–124 many of which have been inversely associated with cigarette and drug use.10,39,64,125 Involvement in the church may also be associated with stronger family ties,126–128 which have a favorable impact on AA youths’ smoking rates. Youths with strong religious ties and familial bonds were even less likely to use alcohol and drugs.118,129 However, there is little evidence to suggest a specific increase in religious participation among AA youths in the United States since the 1970s.130
Cigarette Pricing and Taxes
Studies have shown that cigarette use was inversely correlated with cigarette price increases.10,131–134 Minorities, lower-income people, and youths were even more likely to reduce or quit smoking in response to cigarette price increases.10,135,136 Studies estimated that youths were at least 3 times more responsive to price increases than adults were, such that for each 10% increase in cigarette price, there was an estimated 7% to 14% decline in adolescent prevalence.137–141 AA youths were even more responsive,128,137 such that there was a 16.5% drop in prevalence for young AA men in response to price increases, compared with 8.6% for young White men.142 AA smokers aged between 18 and 24 years were more responsive to price than were older smokers.135
Between 1979 and 1984, accounting for inflation and price adjustment, the cost of cigarettes increased by 14%; between 1984 and 1989, the cost of cigarettes increased an additional 23%.33 These increases in price coincide with the large drop in AA youths’ cigarette smoking; as cigarette use among White youths began to level off in the 1980s, the rates for AA youths continued to decline.5,14,18 Several have argued that these patterns may be reflective of the inability of minority youths, who are often from lower-income households with less disposable income than White families,143 to financially initiate or sustain the behavior.24,137,144 It has also been suggested that financial hardship itself leads to greater religiosity and stronger familial ties, which have been associated with lower smoking rates.24,145
An additional economic impact differentially affecting AA families stems from the marked increase in use of food stamps within AA families from the late 1960s onward. In the late 1960s, $64 worth of food stamps could be purchased for $20, but by 1977 food stamps were provided for much larger amounts at no charge. In 1970, 4.3 million American families received food stamps; that figure escalated to 26.6 million by 1995. A study of a representative sample of US children aged 1 to 20 years from 1968 to 1997 (during which time the country's unemployment rate more than doubled) found that 90% of AA children lived at some time with a family in receipt of food stamps (compared with 37% of White children).146 Food stamps cannot be used to purchase tobacco, so during this time frame a much greater proportion of the disposable income of AA families consisted of benefits (such as food stamps) that could not be used for tobacco. This may partly explain the differential decrease in youth smoking rates from the 1970s to the 1990s.147
Restricted Access to Minors and Smoking Bans
Until the 1970s, several tobacco companies—including Lorillard Tobacco, the maker of Newport cigarettes—used a marketing strategy that consisted of dispensing free cigarettes, either in buy-1-get-1-free promotions or free giveaways, especially in urban areas. These giveaways made cigarettes widely available, and tobacco companies have been accused of specifically targeting AA youths with the free product. This may in part contribute to the initially high rates of AA smokers, which were more comparable to those of White youths before the sudden decline. When a ban was implemented in the 1970s outlawing the distribution of free cigarettes, the removal of free cigarettes during this time period may have contributed to the reduction of smoking among AA youths.148 The widespread distribution of free mentholated cigarettes to AA youths throughout the 1960s may even help explain the initially comparable rates of AA and White youth smokers in the early 1970s.
Later bans and restrictions do not appear to make substantial contributions to the decline in AA youth smoking. Bans restricting the sale of cigarettes to minors usually defined “minors” as children younger than 18 years, although laws were often not enforced and merchants continued to sell cigarettes to minors during the 1970s, throughout the 1980s, and into the 1990s.149 Studies employing youths to buy cigarettes found that cigarettes were easily accessible; minors were able to successfully purchase cigarettes 68% to 100% of the time.150–152 Other surveys, with respondents as young as 13 years, found that 68% of minor smokers reported that they successfully bought their own cigarettes.153,154 One study found that when minors presented clerks with identification showing their age as a minor, clerks were even more likely to sell cigarettes to them.155 Furthermore, merchants were more likely to sell to AA youths than to White youths,156 and AA youths were more likely than were Whites to live in communities where merchants sold to minors,157,158 did not ask for identification,159 and sold single cigarettes (“loosies”).160,161 Youths also had relatively easy access via vending machines, although stores and gas stations were the most frequent source of youth cigarette purchases.10,153,159
Restrictions on smoking in public and dates of implementation varied by state, but most states had laws banning tobacco use by students in schools.10 Although studies found that the strength of state smoking laws was a significant predictor of reduced cigarette use,68,162 these laws most likely did not make major contributions to the decline in smoking prevalence among AA youths. Because of their status as minors, youths were likely not able to smoke in many indoor establishments anyway because of parents, teachers, or other authority figures.
Advertising to African American Audiences
Tobacco companies targeted their marketing strategies toward AA communities in the late 1970s and early 1980s.3 However, smoking rates among AA youths still declined, despite the fact that they were undeniably bombarded with cigarette advertising and promotions as the tobacco industry designed products made specifically for AAs, forged alliances with prominent cultural organizations such as the NAACP, created corporate sponsorships, and donated scholarships to AA college students.3,163,164 Regardless, the advertisements did not seem to effectively appeal to AA youths,3 who were more likely than were White youths to have negative interpretations of cigarette advertisements.75
Discussion
Between the mid-1970s and early 1990s, AA youths experienced a sizable and ubiquitous decline in cigarette smoking rates that was much steeper than the decline that occurred among their White peers. Both decreased initiation rates and increased quit rates among AA youths contributed to the reduction in prevalence. It appears that the lowered smoking rates among AA youths in the 1980s may have been partially offset by a delay in initiation until age 18 years or older.57 Although AAs had significantly lower smoking rates than did Whites in adolescence, smoking rates among AA and White adults were similar.4,10 However, the primary reason for similar smoking rates between adult AAs and adult Whites (despite lower initiation rates in AAs) appears to be that adult AA smokers have consistently had lower smoking cessation rates than have Whites, despite smoking significantly fewer cigarettes per day.55,165,166 Recent studies have found that the lower quit rates among AA adult smokers appear to be specific to the 80% of AA smokers who prefer mentholated cigarettes.167–169 The delay of tobacco initiation combined with lower cessation rates in adulthood lead adult AAs to have a smoking prevalence similar to that of adult Whites.
From the mid-1970s through the early 1990s, AA adolescents experienced a decline in use of marijuana, alcohol, and other drugs, contradicting the theory that AA youths turned to alternative substances. If AAs had turned their attention to other substances as an alternative for initiating cigarette use64,94 or to replace cigarettes upon cessation, there would be a marked increase in the prevalence of other substances. However, the data do not support this. Also, alternative forms of tobacco, alcohol, and other drugs were usually used in tandem with cigarettes and not in lieu of them.52,170
The removal of free cigarettes in AA communities coincides with the onset of the decline and may have contributed to it. This could have delayed initiation of cigarette use or prompted sudden cessation. Although Tauras171 attributes the decline in youth smoking to other laws restricting access to minors, a vast body of literature shows that youths, especially AA youths, had easy access to cigarettes.
Cigarette prices seemed to be one of the major forces driving consumption. As cigarette prices rose, cigarette use among youths declined, especially among AA youths, who were particularly responsive to climbing cigarette prices. Several studies speculated that price was more influential on AA youths because they had less disposable income than did White youths136 to spend on cigarettes, alcohol, and other substances,24,136 which was a result of higher adult and youth unemployment rates more frequently affecting AA families172–174 during that time.146
In addition to the overall effects on US smoking prevalence of the surgeon general's warning about the negative health consequences of cigarettes, the literature suggests that antitobacco programming had differential effects on AA and White youths. This finding is consistent with the tendency of AA youths to cite negative health consequences as reasons for not smoking. From the 1950s through the 1990s, AA male lung cancer rates increased significantly more than did White male lung cancer rates, perhaps adding to the negative perception of smoking and its impact on health among AA youths. In addition, AA youths were less likely to perceive benefits associated with smoking, such as appetite suppression and weight control.82,175 White adolescents were more likely than were AA adolescents to report that they used cigarettes to control their appetite and weight.53 White female adolescents were also more likely to perceive smoking as a behavior that empowered them and enhanced their image, whereas AA female adolescents were more likely to believe that people smoked because others smoked.79,87 Perhaps when there are fewer perceived benefits, there is less of an incentive to begin or maintain smoking behavior.176,177
Additional protective factors, such as family ties and peer prevalence and influence, may also have contributed to reduced cigarette use. AA youths held negative attitudes toward smoking, which is predictive of nonsmoking behavior. They also experienced lower amounts of prosmoking and social influences, which may have helped further fuel their own antismoking views. With respect to key relationships, AA youths had stronger parental and religious ties than did White youths; consequently, they had increased motivation to comply with the strong antismoking positions, attitudes, and views of their parents, church leaders, and peers. Cigarette use patterns for high school seniors were also inversely related to level of school involvement, number of social evenings out, and level of religious commitment.13,39 The level of prosocial activities (e.g., family, church, or community involvement) and sports were found to be negatively associated with smoking.64,79,94,99 AAs who had higher grades, who were heavily involved in school, or who felt that college was a viable option in their future were less likely to smoke.32,64,82
Perhaps all of these correlates were related to the amount of direct adult influence and supervision as provided in schools, places of worship, and homes.13 Although the literature does not suggest marked changes in these latter factors during the period of interest, it is possible these factors supplemented the decline driven by other (largely socioeconomic) factors.
Conclusions
Increases in cigarette price caused by increased federal and state excise taxes have become a crucial policy tool for reducing cigarette use, especially among AA youths.131,177,178 The literature suggests that social and economic factors may have contributed in tandem to the steeper reductions in tobacco use among AA youths than among White youths during the mid-1970s and early 1990s. The timing of a large increase in the proportion of AA youths living in single-mother households, increased economic difficulty, increased dependence on food stamps, and increases in cigarette prices may have particularly affected AA youths’ smoking more than White youths’ smoking.
In addition, communications from the US surgeon general regarding the negative consequences of cigarettes, increased lung cancer rates among AA men, and the removal of free cigarette marketing may have also led to a drop in smoking among AA youths. AA youths were more likely to have parents with antismoking views, close parental ties, strong religious affiliations, positive prosocial activities, fewer smoking peers, and lower peer influence; these factors may have performed an additional protective function, although such factors may have existed before the onset of the decline.
Hypotheses attributing AA youths’ decline in tobacco use to AA youths using alternative drugs, having restricted access to cigarettes, being less honest in surveys, or having lower attendance at school were not supported. The relative reduction in AA youths smoking since the mid-1970s has likely caused the relative reduction in lung cancer rates in young adult AAs from the 1990s into the 21st century.
Acknowledgments
During the preparation of this article, Jonathan Foulds was funded by the New Jersey Department of Health and Senior Services, the Rutgers Community Health Foundation, and the Penn State Cancer Institute.
Human Participant Protection
No protocol approval was necessary because no human research participants were involved.
References
- 1.Centers for Disease Control and Prevention Smoking-attributable mortality, years of potential life lost, and productivity losses—United States, 2000–2004. MMWR Morb Mortal Wkly Rep. 2008;57(45):1226–1228 [PubMed] [Google Scholar]
- 2.Ries LAG, Melbert D, Krapcho M, et al. SEER cancer statistics review, 1975–2004. Bethesda, MD: NationalCancer Institute; 2006. Available at: http://seer.cancer.gov/csr/1975_2004. Revised November 15, 2007. Accessed July 13, 2011 [Google Scholar]
- 3.US Department of Health and Human Services Tobacco Use Among US Racial/Ethnic Minority Groups—African Americans, American Indians and Alaska Natives, Asian Americans and Pacific Islanders, and Hispanics. Atlanta, GA: US Dept of Health and Human Services, Public Health Service; 1998 [Google Scholar]
- 4.Centers for Disease Control and Prevention Cigarette smoking among adults—United States, 2007. MMWR Morb Mortal Wkly Rep. 2008;57(45):1221–1226 [PubMed] [Google Scholar]
- 5.Johnston LD, O'Malley PM, Bachman JG, et al. Demographic Subgroup Trends for Various Licit and Illicit Drugs, 1975–2004. Ann Arbor, MI: Institute for Social Research; 2005 [Google Scholar]
- 6.Wallace JM, Bachman JG, O'Malley PM, et al. Tobacco, alcohol, and illicit drug use: racial and ethnic differences among US high school seniors, 1976–2000. Public Health Rep. 2002;117(1, suppl. 1):S67–S75 [PMC free article] [PubMed] [Google Scholar]
- 7.Nelson DE, Mowery P, Asman K, et al. Long-term trends in adolescent and young adult smoking in the United States: metapatterns and implications. Am J Public Health. 2008;98(5):905–915 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Centers for Disease Control and Prevention Tobacco use among middle and high school students—United States, 1999. MMWR Morb Mortal Wkly Rep. 2000;49(3):49–53 [PubMed] [Google Scholar]
- 9.Gilpin EA, White VM, Pierce JP. What fraction of young adults are at risk for future smoking, and who are they? Nicotine Tob Res. 2005;7(5):747–759 [DOI] [PubMed] [Google Scholar]
- 10.US Department of Health and Human Services Preventing Tobacco Use Among Young People. Rockville, MD: US Dept of Health and Human Services, Public Health Service; 1994 [Google Scholar]
- 11.Wallace JM, Jr, Bachman JG. Explaining racial/ethnic differences in adolescent drug use: the impact of background and lifestyle. Soc Probl. 1991;38(3):333–357 [Google Scholar]
- 12.Bachman JG, Wallace JM, O'Malley PM, et al. Racial/ethnic differences in smoking, drinking, and illicit drug use among American high school seniors, 1976–89. Am J Public Health. 1991;81(3):372–377 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pampel FC, Aguilar J. Changes in youth smoking, 1976–2002: a time-series analysis. Youth Soc. 2008;39(4):453–479 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Johnston LD, O'Malley PM, Bachman JG, et al. Monitoring the Future: National Survey Results on Drug Use, 1975–2004—Volume II: College Students and Adults Ages 19–45. Bethesda, MD: National Institute on Drug Abuse; 2005 [Google Scholar]
- 15.Centers for Disease Control and Prevention Cigarette smoking among youth—United States, 1989. MMWR Morb Mortal Wkly Rep. 1991;40(41):712–715 [PubMed] [Google Scholar]
- 16.Centers for Disease Control and Prevention Incidence of initiation of cigarette smoking—United States, 1965–1996. MMWR Morb Mortal Wkly Rep. 1998;47(39):837–840 [PubMed] [Google Scholar]
- 17.An LC, O'Malley PM, Schulenberg JE, et al. Changes at the high end of risk in cigarette smoking among US high school seniors, 1976–1995. Am J Public Health. 1999;89(5):699–705 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Nelson DE, Giovino GA, Shoplan DR, et al. Trends in cigarette smoking among US adolescents, 1974 through 1991. Am J Public Health. 1995;85(1):34–40 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Centers for Disease Control and Prevention Trends in smoking initiation among adolescents and young adults—United States, 1980–1989. MMWR Morb Mortal Wkly Rep. 1995;44(28):521–525 [PubMed] [Google Scholar]
- 20.Flint AJ, Novotny TE. Trends in Black/White differences in current smoking among 18- to 24-year-olds in the United States, 1983–1993. Am J Public Health. 1998;14(1):19–24 [DOI] [PubMed] [Google Scholar]
- 21.Sarvela PD, Cronk CE, Isberner FR. A secondary analysis of smoking among rural and urban youth using the MTF data set. J Sch Health. 1997;67(9):372–375 [DOI] [PubMed] [Google Scholar]
- 22.Russell MAH. The nicotine trap: a 40-year sentence for four cigarettes. Br J Addict. 1990;85(2):293–300 [DOI] [PubMed] [Google Scholar]
- 23.Bauman KE, Ennett SE. Tobacco use by Black and White adolescents: the validity of self-reports. Am J Public Health. 1994;84(3):394–398 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kandel DB. Ethnic differences in drug use: patterns and paradoxes. : Botvin GJ, Schinke SP, Orlandi MA, Drug Abuse Prevention With Multiethnic Youth. Thousand Oaks, CA: Sage Publications; 1995:81–104 [Google Scholar]
- 25.Jarvis MJ, Tunstall-Pedoe H, Feyerabend C, et al. Comparison of tests used to distinguish smokers from nonsmokers. Am J Public Health. 1987;77(11):1435–1438 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Etzel RA. A review of the use of saliva cotinine as a marker of tobacco smoke exposure. Prev Med. 1990;19(2):190–197 [DOI] [PubMed] [Google Scholar]
- 27.Patrick DL, Cheadle A, Thompson DC, et al. The validity of self-reported smoking: a review and meta-analysis. Am J Public Health. 1994;84(7):1086–1093 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wagenknecht LE, Burke GL, Perkins LL, et al. Misclassification of smoking status in the CARDIA study: a comparison of self-report with serum cotinine levels. Am J Public Health. 1992;82(1):33–36 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wills TA, Cleary SD. The validity of self-reports of smoking: analyses by race/ethnicity in a school sample of urban adolescents. Am J Public Health. 1997;87(1):56–61 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Oetting ER, Beauvais F. Adolescent drug use: findings of national and local surveys. J Consult Clin Psychol. 1990;58(4):385–394 [DOI] [PubMed] [Google Scholar]
- 31.Johnston LD, Bachman JG, O'Malley PM. Monitoring the Future: Questionnaire Responses From the Nation's High School Seniors. Ann Arbor, MI: Institute for Social Research; 1993 [Google Scholar]
- 32.Bachman JG, Johnston LD, O'Malley PM. Smoking, drinking, and drug use among American high school students: correlates and trends, 1975–1979. Am J Public Health. 1981;71(1):59–69 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gilpin EA, Pierce JP. Trends in adolescent smoking initiation in the United States: is tobacco marketing an influence? Tob Control. 1997;6(2):122–127 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Smith TM. Findings From the Condition of Education, 1994—No. 2: The Educational Progress of Black Students. Washington, DC: National Center for Education Statistics, US Dept of Education, Office of Educational Research and Improvement; 1995 [Google Scholar]
- 35.US Census Bureau Current Population Survey (CPS), October Supplement 1972–2004. Washington, DC: US Census Bureau; 2005 [Google Scholar]
- 36.Epstein L, Tamir A. Health-related behavior of adolescents: change over time. J Adolesc Health Care. 1984;5(2):91–95 [DOI] [PubMed] [Google Scholar]
- 37.Mensch BS, Kandel DB. Dropping out of high school and drug involvement. Sociol Educ. 1988;61(2):95–113 [Google Scholar]
- 38.Planty M, Hussar W, Snyder T, et al. The Condition of Education 2008. Washington, DC: National Center for Education Statistics, Institute of Education Sciences, US Dept of Education; 2008 [Google Scholar]
- 39.Brown TN, Schulenberg J, Bachman JG, et al. Are risk and protective factors for substance use consistent across historical time? National data from the high school classes of 1976 through 1997. Prev Sci. 2001;2(1):29–44 [DOI] [PubMed] [Google Scholar]
- 40.Frase MJ. Dropout Rates in the United States: 1988. Washington, DC: US Dept of Education, Office of Educational Research and Improvement, National Center for Education Statistics; 1989 [Google Scholar]
- 41.Kominski R, Adams A. Educational Attainment in the United States: March 1993 and 1992. Washington, DC: US Census Bureau; 1994 [Google Scholar]
- 42.National Institute on Drug Abuse National Household Study on Drug Abuse: Main Findings 1985. Washington, DC: National Institute on Drug Abuse; 1988 [Google Scholar]
- 43.Harrison L. Understanding the differences in youth drug prevalence rates produced by the MTF, NHSDA, and YRBS studies. J Drug Issues. 2001;31(3):665–694 [Google Scholar]
- 44.Kopstein AN, Roth PT. Drug Abuse Among Racial/Ethnic Groups. Rockville, MD: US Dept of Health and Human Services, Public Health Service, National Institutes of Health, National Institute on Drug Abuse; 1993 [Google Scholar]
- 45.Anderson CM, Burns DM. Pattern of adolescent initiation rates over time: national and California data. : Burns DM, Amacher RH, Smoking and Tobacco Control Monograph No. 14. Washington, DC: US Dept of Health and Human Services, National Institutes of Health, National Cancer Institute; 2001:157–170 [Google Scholar]
- 46.Dell JL, Whitman S, Shah AM, Silva A, Ansell D. Smoking in 6 diverse Chicago communities—a population study. Am J Public Health. 2005;95(6):1036–1042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Link MW, Mokdad AH, Stackhouse HF, et al. Race, ethnicity, and linguistic isolation as determinants of participation in public health surveillance surveys. Prev Chronic Dis. 2005;2(2). Available at: http://www.cdc.gov/pcd/issues/2005/apr/04_0142c.htm. Accessed July 13, 2011 [PMC free article] [PubMed] [Google Scholar]
- 48.Nelson DE, Powell-Griner E, Town M, et al. A comparison of national estimates from the National Health Interview Survey and the Behavioral Risk Factor Surveillance System. Am J Public Health. 2003;93(8):1335–1341 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Fisher MA, Taylor GW, Shelton BJ, et al. Age and race/ethnicity-gender predictors of denying smoking, United States. J Health Care Poor Underserved. 2008;19(1):75–89 [DOI] [PubMed] [Google Scholar]
- 50.Jemal A, Center MM, Ward E. The convergence of lung cancer rates between Blacks and Whites under the age of 40, United States. Cancer Epidemiol Biomark Prev. 2009;18(12):3349–3352 [DOI] [PubMed] [Google Scholar]
- 51.Faulkner DL, Escobedo LG, Zhu B, et al. Race and the incidence of cigarette smoking among adolescents in the United States. J Natl Cancer Inst. 1996;88(16):1158–1160 [DOI] [PubMed] [Google Scholar]
- 52.US Department of Health and Human Services Reducing the Health Consequences of Smoking: 25 Years of Progress. Rockville, MD: US Dept of Health and Human Services, Public Health Service; 1989 [Google Scholar]
- 53.Klesges RC, Elliott VE, Robinson LA. Chronic dieting and the belief that smoking controls body weight in a biracial, population-based adolescent sample. Tob Control. 1997;6(2):89–94 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Geronimus AT, Neidert LJ, Bound J. Age patterns of smoking in US Black and White women of childbearing age. Am J Public Health. 1993;83(9):1258–1264 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Escobedo LG, Anda RF, Smith PF, et al. Sociodemographic characteristics of cigarette smoking initiation in the United States: implications for smoking prevention policy. JAMA. 1990;264(12):1550–1555 [PubMed] [Google Scholar]
- 56.Juon HS, Ensminger ME, Sydnor KD. A longitudinal study of developmental trajectories to young adult cigarette smoking. Drug Alcohol Depend. 2002;66(3):303–314 [DOI] [PubMed] [Google Scholar]
- 57.Trinidad DR, Gilpin EA, Lee L, Pierce JP. Has there been a delay in the age of regular smoking onset among African Americans? Ann Behav Med. 2004;28(3):152–157 [DOI] [PubMed] [Google Scholar]
- 58.White HR, Nagin D, Replogle E, et al. Racial differences in trajectories of cigarette use. Drug Alcohol Depend. 2004;76(3):219–227 [DOI] [PubMed] [Google Scholar]
- 59.Guggenheimer J, Zullo TG, Kruper DC, et al. Changing trends of tobacco use in a teenage population in Western Pennsylvania. Am J Public Health. 1986;76(2):196–197 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Ellickson PL, Perlman M, Klein DJ. Explaining racial/ethnic differences in smoking during the transition to adulthood. Addict Behav. 2003;28(5):915–931 [DOI] [PubMed] [Google Scholar]
- 61.Soldz S, Huyser DJ, Dorsey E. Characteristics of users of cigars, bidis, and kreteks and the relationship to cigarette use. Prev Med. 2003;37(3):250–258 [DOI] [PubMed] [Google Scholar]
- 62.Centers for Disease Control and Prevention Tobacco use among middle and high school students—United States, 2002. MMWR Morb Mortal Wkly Rep. 2003;52(45):1096–1098 [PubMed] [Google Scholar]
- 63.Ajzen I, Fishbein M. Understanding Attitudes and Predicting Social Behavior. Englewood Cliffs, NJ: Prentice Hall; 1980 [Google Scholar]
- 64.White HR, Violette NM, Metzger L, et al. Adolescent risk factors for late-onset smoking among African American young men. Nicotine Tob Res. 2007;9(1):153–161 [DOI] [PubMed] [Google Scholar]
- 65.Conrad KM, Flay BR, Hill D. Why children start smoking cigarettes: predictors of onset. Brit J Addiction. 1992;87(12):1711–1724 [DOI] [PubMed] [Google Scholar]
- 66.Wallace JM, Bachman JG, O'Malley PM, et al. Racial/ethnic differences in adolescent drug use: exploring possible explanations. : Botvin G, Schinke S, Orlandi M, Drug Abuse Prevention With Multiethnic Youth. Thousand Oaks, CA: Sage Publications; 1995 [Google Scholar]
- 67.Ellickson PL, Orlando M, Tuker JS, Klein DJ. From adolescence to young adulthood: racial/ethnic disparities in smoking. Am J Public Health. 2004;94(2):293–299 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Simonich WL. Government Antismoking policies. New York, NY: Peter Lang Publishing; 1991 [Google Scholar]
- 69.Warner KE. Effects of the antismoking campaign: an update. Am J Public Health. 1989;79(2):144–151 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Hamilton JL. The demand for cigarettes: advertising, the health scare, and the cigarette advertising ban. Rev Econ Stat. 1972;54(4):401–411 [Google Scholar]
- 71.Pierce JP, Gilpin EA. News media coverage of smoking and health is associated with changes in population rates of smoking cessation but not initiation. Tob Control. 2001;10(2):145–153 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Bauman K, Padgett C, Koch G. A media-based campaign to encourage personal communication among adolescents about not smoking cigarettes: participation, selection, and consequences. Health Educ Res. 1989;4(1):35–44 [Google Scholar]
- 73.Cella DF, Tulsky DS, Sarafian B, et al. Culturally relevant smoking prevention for minority youth. J Sch Health. 1992;62(8):377–380 [DOI] [PubMed] [Google Scholar]
- 74.Hunkeler EF, Davis EM, McNeil B, et al. Richmond quits smoking: a minority community fights for health. : Bracht N, Health Promotion at the Community Level. Newbury Park, CA: Sage; 1990 [Google Scholar]
- 75.Kaufman JS, Jason LA, Sawlski LM, et al. Comprehensive multi-media program to prevent smoking among Black students. J Drug Educ. 1994;24(2):95–108 [DOI] [PubMed] [Google Scholar]
- 76.Cowell AJ, Farrelly M, Chou R. Assessing the impact of the national ‘truth’ antismoking campaign on beliefs, attitudes and intent to smoke by race/ethnicity. Ethn Health. 2009;14(1):75–91 [DOI] [PubMed] [Google Scholar]
- 77.Farrelly MC, Nonnemaker J, Davis KC, et al. The influence of the national truth campaign on smoking initiation. Am J Prev Med. 2009;36(5):379–384 [DOI] [PubMed] [Google Scholar]
- 78.Zollinger TW, Saywell RM, Wooldridge SJ. Racial differences in adolescent tobacco use, environments, and attitudes. Paper presented at: 131st Annual Meeting of the American Public Health Association; November 2003; San Francisco, CA [Google Scholar]
- 79.Taylor WC, Ayars CL, Gladney AP, et al. Beliefs about smoking among adolescents—gender and ethnic differences. J Child Adolesc Subst Abuse. 1999;8(3):37–54 [Google Scholar]
- 80.Wallace JM, Forman TA, Guthrie BJ, et al. The epidemiology of alcohol, tobacco and other drug use among Black youth. J Stud Alcohol. 1999;60(6):800–809 [DOI] [PubMed] [Google Scholar]
- 81.Griesler PC, Kandel DB. Ethnic differences in correlates of adolescent cigarette smoking. J Adolesc Health. 1998;23(3):167–180 [DOI] [PubMed] [Google Scholar]
- 82.Headen SW, Bauman KE, Deane GD, et al. Are the smoking correlates of cigarette smoking initiation different for Black and White adolescents? Am J Public Health. 1991;81(7):854–858 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Skinner ML, Haggerty KP, Catalano RF. Parental and peer influences on teen smoking: are White and Black families different? Nicotine Tob Res. 2009;11(5):558–563 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Flay BR, Brannon BR, Johnson CA, et al. The television school and family smoking prevention and cessation project. Prev Med. 1988;17(5):585–607 [DOI] [PubMed] [Google Scholar]
- 85.Flay BR, Hu F, Siddiqui O, et al. Differential influence of parental smoking and friends’ smoking on adolescent initiation and escalation of smoking. J Health Soc Behav. 1994;35(3):248–265 [PubMed] [Google Scholar]
- 86.Koepke D, Flay BR, Johnson CA. Health behaviors in minority families: the case of cigarette smoking. Fam Community Health. 1990;13(1):35–43 [Google Scholar]
- 87.Mermelstein R; Tobacco Control Network Writing Group. Explanation of ethnic and gender differences in youth smoking: a multi-site, qualitative investigation. Nicotine Tob Res. 1999;1(suppl 1):S91–S98 [DOI] [PubMed] [Google Scholar]
- 88.Wallace JM, Muroff J. Preventing substance abuse among African American children and youth: race differences in risk factor exposure and vulnerability. J Prim Prev. 2002;22(3):235–261 [Google Scholar]
- 89.Catalano RF, Morrison DM, Wells EA, et al. Ethnic differences in family factors related to early drug initiation. J Stud Alcohol. 1992;53(3):208–217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90. Child Trends Databank Family structure. Available at: www.childtrendsdatabank.org/?q=node/231. Accessed March 3, 2011
- 91.Baker TB, Brandon TH, Chassin L. Motivational influence on cigarette smoking. Annu Rev Psychol. 2004;55:463–491 [DOI] [PubMed] [Google Scholar]
- 92.Unger JB, Rohrback LA, Cruz TB, et al. Ethnic variation in peer influence on adolescent smoking. Nicotine Tob Res. 2001;3(2):167–176 [DOI] [PubMed] [Google Scholar]
- 93.Botvin GJ, Naker E, Botvin EM, et al. Factors promoting cigarette smoking among Black youth: a causal modeling approach. Addict Behav. 1993;18(4):397–405 [DOI] [PubMed] [Google Scholar]
- 94.Gardiner PS. African American teen cigarette smoking: a review. : Burns DM, Amacher RH, Smoking and Tobacco Control Monograph No. 14. Washington, DC: US Dept of Health and Human Services, National Institutes of Health, National Cancer Institute; 2001:213–225 [Google Scholar]
- 95.Mermelstein R. Ethnicity, gender and risk factors for smoking initiation: an overview. Nicotine Tob Res. 1999;1(suppl 2):S39–S43 [DOI] [PubMed] [Google Scholar]
- 96.Gritz ER, Prokhorov AV, Hudmon KS, et al. Cigarette smoking in a multiethnic population of youth: methods and baseline findings. Prev Med. 1998;27(3):365–384 [DOI] [PubMed] [Google Scholar]
- 97.Royce JM, Hymowitz N, Corbett K, et al. Smoking cessation factors among African Americans and Whites. Am J Public Health. 1993;83(2):220–226 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.McIntosh H. Black teens not smoking in great numbers. J Natl Cancer Inst. 1995;87(8):564. [DOI] [PubMed] [Google Scholar]
- 99.Xue Y, Zimmerman MA, Caldwell CH. Neighborhood residence and cigarette smoking among urban youths: the protective role of prosocial activities. Am J Public Health. 2007;97(10):1865–1872 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Braithwaite RL, Griffin JP, Bhalakia A, Braithwaite M, Arriola KJ. Cultural identification and tobacco use among African American middle school students. Am J Health Stud. 1999;15(2):82–91 [Google Scholar]
- 101.Amey CH, Albrecht SL, Miller MK. Racial differences in adolescent drug use: the impact of religion. Subst Use Misuse. 1996;31(10):1311–1332 [DOI] [PubMed] [Google Scholar]
- 102.Brownfield D, Sorenson AM. Religion and drug use among adolescents: a social support conceptualization and interpretation. Deviant Behav. 1991;12(3):259–276 [Google Scholar]
- 103.Gorsuch RL. Religious aspects of substance abuse and recovery. J Soc Issues. 1995;51(2):65–83 [Google Scholar]
- 104.Khavari KA, Harmon TM. The relationship between the degree of professed religious belief and use of drugs. Int J Addict. 1982;17(5):847–857 [DOI] [PubMed] [Google Scholar]
- 105.McBride DC, Mutch PB, Chitwood DD. Religious Belief and the Initiation and Prevention of Drug Use Among Youth. Thousand Oaks, CA: Sage; 1996 [Google Scholar]
- 106.Miller L, Davies M, Greenwald S. Religiosity and substance use and abuse among adolescents in the National Comorbidity Survey. J Am Acad Child Adolesc Psychiatry. 2000;39(9):1190–1197 [DOI] [PubMed] [Google Scholar]
- 107.Johnston LD, Bachman JG, O'Malley PM. Monitoring the Future: Questionnaire Responses From the Nation's High School Seniors. Ann Arbor, MI: Institute for Social Research; 1976 [Google Scholar]
- 108.Johnston LD, Bachman JG, O'Malley PM. Monitoring the Future: Questionnaire Responses From the Nation's High School Seniors. Ann Arbor, MI: Institute for Social Research; 1981 [Google Scholar]
- 109.Johnston LD, Bachman JG, O'Malley PM. Monitoring the Future: Questionnaire Responses From the Nation's High School Seniors. Ann Arbor, MI: Institute for Social Research; 1986 [Google Scholar]
- 110.Johnston LD, Bachman JG, O'Malley PM. Monitoring the Future: Questionnaire Responses From the Nation's High School Seniors. Ann Arbor, MI: Institute for Social Research; 1991 [Google Scholar]
- 111.Johnston LD, Bachman JG, O'Malley PM. Monitoring the Future: Questionnaire Responses From the Nation's High School Seniors. Ann Arbor, MI: Institute for Social Research; 1992 [Google Scholar]
- 112.Johnston LD, Bachman JG, O'Malley PM. Monitoring the Future: Questionnaire Responses From the Nation's High School Seniors. Ann Arbor, MI: Institute for Social Research; 1994 [Google Scholar]
- 113.Johnston LD, Bachman JG, O'Malley PM. Monitoring the Future: Questionnaire Responses From the Nation's High School Seniors. Ann Arbor, MI: Institute for Social Research; 1995 [Google Scholar]
- 114.Johnston LD, Bachman JG, O'Malley PM. Monitoring the Future: Questionnaire Responses From the Nation's High School Seniors. Ann Arbor, MI: Institute for Social Research; 1996 [Google Scholar]
- 115.Donahue MJ, Benson PL. Religion and the well-being of adolescents. J Soc Issues. 1995;51(2):145–160 [Google Scholar]
- 116.Chatters LM, Taylor RJ, Lincoln KD. African American religious participation: a multi-sample comparison. J Sci Study Relig. 1999;38(1):132–145 [Google Scholar]
- 117.Brown DR, Gary LE. Religious socialization and educational attainment among African Americans: an empirical assessment. J Negro Educ. 1991;60(3):411–426 [Google Scholar]
- 118.Forliti JE, Benson PL. Young adolescents: a national study. Relig Educ. 1986;81(2):199–224 [Google Scholar]
- 119.Ellison CG. Religious involvement and self-perception among Black Americans. Soc Forces. 1993;71(4):1027–1055 [Google Scholar]
- 120.Grant KE, O'Koon JH, Davis TH, et al. Protective factors affecting low-income urban African American youth exposed to stress. J Early Adolesc. 2000;20(4):388–417 [Google Scholar]
- 121.Damon W. Setting the Stage for the Development of Wisdom: Self-Understanding and Moral Identity During Adolescence. Philadelphia, PA: Templeton Foundation; 2000 [Google Scholar]
- 122.Donelson E. Psychology of religion and adolescents in the United States: past to present. J Adolesc. 1999;22(2):187–204 [DOI] [PubMed] [Google Scholar]
- 123.Smith C. Religious participation and parental moral expectations and supervision of American youth. Rev Relig Res. 2003;44(4):414–424 [Google Scholar]
- 124.Steele LL. Research in faith development. Christ Educ J. 1989;9(2):21–30 [Google Scholar]
- 125.Warheit GJ, Biafora FA, Zimmerman R, et al. Self-rejection/derogation, peer factors, and alcohol, drug, and cigarette use among a sample of Hispanic, African-American, and White non-Hispanic adolescents. Int J Addict. 1995;30(2):97–116 [DOI] [PubMed] [Google Scholar]
- 126.Amoateng AY, Bahr SJ. Religion, family, and adolescent drug use. Sociol Perspect. 1986;29(1):53–76 [Google Scholar]
- 127.Bahr SJ, Maughan SL, Marcos AC, et al. Family, religiosity, and the risk of adolescent drug use. J Marriage Fam. 1998;60(4):979–992 [Google Scholar]
- 128.Brody GH, Stoneman Z, Flor D. Parental religiosity, family processes, and youth competence in rural, two-parent African American families. Dev Psychol. 1996;32(4):696–706 [Google Scholar]
- 129.Belgrave FZ, Johnson J, Nguyen A. Stress and tobacco use among African-American adolescents: the buffering effect of cultural factors. J Drug Educ. 2010;40(2):173–188 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Schwadel P. Age, period, and cohort effects on US religious service attendance: the declining impact of sex, southern residence, and Catholic affiliation. Sociol Relig. 2010;71(1):2–24 [Google Scholar]
- 131.Lewit EM, Coate D. The potential for using excise taxes to reduce smoking. J Health Econ. 1982;1(2):121–145 [DOI] [PubMed] [Google Scholar]
- 132.Gruber J, Köszegi B. Is addiction “rational”? Theory and evidence. Q J Econ. 2001;116(4):1261–1303 [Google Scholar]
- 133.Ross H, Chaloupka V. The effect of cigarette prices on youth smoking. Health Econ. 2003;12(3):217–230 [DOI] [PubMed] [Google Scholar]
- 134.Dedobbeleer N, Béland F, Contandriopoulos AP, et al. Gender and the social context of smoking behavior. Soc Sci Med. 2004;58(1):1–12 [DOI] [PubMed] [Google Scholar]
- 135.Centers for Disease Control and Prevention Response to increases in cigarette prices by race/ethnicity, income, and age groups—United States, 1976–1993. MMWR Morb Mortal Wkly Rep. 1998;47(29):605–609 [PubMed] [Google Scholar]
- 136.Evans WN, Farrelly MC. The compensating behavior of smokers: taxes, tar, and nicotine. Rand J Econ. 1998;29(3):578–595 [PubMed] [Google Scholar]
- 137.Ding A. Youth are more sensitive to price changes in cigarettes than adults. Yale J Biol Med. 2003;76(3):115–124 [PMC free article] [PubMed] [Google Scholar]
- 138.Grossman M, Chaloupka FJ. Cigarette taxes: the straw to break the camel's back. Public Health Rep. 1997;112(4):290–297 [PMC free article] [PubMed] [Google Scholar]
- 139.Lewit EM, Coate D, Grossman M. The effects of government regulation on teenage smoking. J Law Econ. 1981;24(3):545–569 [Google Scholar]
- 140.Nonnemaker JM, Farrelly MC. Smoking initiation among youth: the role of cigarette excise taxes and prices by race/ethnicity and gender. J Health Econ. 2011;30(3):560–567 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Carpenter C, Cook PJ. Cigarette taxes and youth smoking: new evidence from national, state, and local Youth Risk Behavior Surveys. J Health Econ. 2008;27(2):287–299 [DOI] [PubMed] [Google Scholar]
- 142.Chaloupka FJ, Pacula RS. Sex and race differences in young people's responsiveness to price and tobacco control policies. Tob Control. 1999;8(4):373–377 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Lichter DT, Eggebeen DJ. Rich kids, poor kids: changing income inequality among American children. Soc Forces. 1993;71(3):761–780 [Google Scholar]
- 144.Barnes G, Farrell M, Banerjee S. Family influences on alcohol abuse and other problem behaviors among Black and White adolescents in a general population sample. J Res Adolesc. 1994;4(2):183–201 [Google Scholar]
- 145.Bradshaw M, Ellison CG. Financial hardship and psychological distress: exploring the buffering effects of religion. Soc Sci Med. 2010;71(1):196–204 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Rank MR, Hirschl TA. Estimating the risk of food stamp use and impoverishment during childhood. Arch Pediatr Adolesc Med. 2009;163(11):994–999 [DOI] [PubMed] [Google Scholar]
- 147.Rank MR, Hirschl TA. Likelihood of using food stamps during the adulthood years. J Nutr Educ Behav. 2005;37(3):137–146 [DOI] [PubMed] [Google Scholar]
- 148.Kluger R. Ashes to Ashes. New York, NY: Vintage Books; 1997 [Google Scholar]
- 149.US Department of Health and Human Services State Oversight of Tobacco Sales to Minors. Washington, DC: US Dept of Health and Human Services; 1995 [Google Scholar]
- 150.DiFranza JR, Savageau JA, Aisquith BF. Youth access to tobacco: the effects of age, gender, vending machine locks, and “It's the Law” programs. Am J Public Health. 1996;86(2):221–224 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Rigotti NA, DiFranza JR, Chang Y, et al. The effect of enforcing tobacco-sales laws on adolescents’ access to tobacco and smoking behavior. N Engl J Med. 1997;337(15):1044–1051 [DOI] [PubMed] [Google Scholar]
- 152.Feighery E, Altman DG, Shaffer GT. The effects of combining education and enforcement to reduce tobacco sales to minors. JAMA. 1991;266(22):3168–3171 [PubMed] [Google Scholar]
- 153.Cummimgs KM, Sciandra E, Pechacek TF, et al. Where teens get their cigarettes: a survey of the purchasing habits of 13–16 year olds in 12 US communities. Tob Control. 1992;1(4):264–267 [Google Scholar]
- 154.Centers for Disease Control and Prevention Accessibility of cigarettes to youths aged 12–17 years—United States, 1989. MMWR Morb Mortal Wkly Rep. 1992;41(27):485–488 [PubMed] [Google Scholar]
- 155.Levinson AH, Hendershott S, Byers TE. The ID effect on youth access to cigarettes. Tob Control. 2002;11(4):296–299 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Landrine H, Klonoff EA, Alcaraz R. Racial discrimination in minors’ access to tobacco. J Black Psychol. 1997;23(2):135–147 [Google Scholar]
- 157.Landrine H, Klonoff EA, Fritz JM. Preventing cigarette sales to minors: the need for contextual sociocultural analysis. Prev Med. 1994;23(3):322–327 [DOI] [PubMed] [Google Scholar]
- 158.Voorhees CC, Swank RT, Stillman FA, et al. Cigarette sales to African-American and White minors in low-income areas of Baltimore. Am J Public Health. 1997;87(4):652–654 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Centers for Disease Control and Prevention Accessibility of tobacco products to youths aged 12–17 years—United States, 1989 and 1993. MMWR Morb Mortal Wkly Rep. 1996;45(6):125–130 [PubMed] [Google Scholar]
- 160.Klonoff EA, Fritz JM, Landrine H, et al. The problem and sociocultural context of single-cigarette sales. JAMA. 1994;271(8):618–620 [PubMed] [Google Scholar]
- 161.Landrine H, Klonoff E, Alcaraz R. Minors’ access to single cigarettes in California. Prev Med. 1998;27(4):503–505 [DOI] [PubMed] [Google Scholar]
- 162.Evans W, Farrelly M, Montgomery E. Do workplace smoking bans reduce smoking? Am Econ Rev. 1999;89(4):728–747 [Google Scholar]
- 163.Rosenberg NJ, Siegel M. Use of corporate sponsorship as a tobacco marketing tool: a review of tobacco industry sponsorship in the USA, 1995–99. Tob Control. 2001;10(3):239–246 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Yerger VB, Malone RE. African American leadership groups: smoking with the enemy. Tob Control. 2002;11(4):336–345 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Novotny TE, Warner KE, Kendrick JE, et al. Socioeconomic factors and racial smoking differences in the United States. Am J Public Health. 1988;78(9):1187–1189 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Kiefe CI, Williams OD, Lewis CE, et al. Ten-year changes in smoking among young adults: are racial differences explained by socioeconomic factors in the CARDIA study? Am J Public Health. 2001;91(2):213–218 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Gandhi KK, Foulds J, Steinberg MB, et al. Lower quit rates among African American and Latino menthol smokers at a tobacco treatment clinic. Int J Clin Pract. 2009;63(3):360–367 [DOI] [PubMed] [Google Scholar]
- 168.Gundersen DA, Delnevo CD, Wackowski O. Exploring the relationship between race/ethnicity, menthol smoking, and cessation in a nationally representative sample of adults. Prev Med. 2009;49(6):553–557 [DOI] [PubMed] [Google Scholar]
- 169.Foulds J, Pletcher M, Hooper M, et al. Do smokers of menthol cigarettes find it harder to quit smoking? Nicotine Tob Res. 2010;12(suppl 2):S102–S109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.DeMoor C, Elder JP, Young RL, Wildey MB, Molgaard CA. Generic tobacco use among four ethnic groups in a school age population. J Drug Educ. 1989;19(3):257–270 [DOI] [PubMed] [Google Scholar]
- 171.Tauras JA. Differential impact of state tobacco control policies among race and ethnic groups. Addiction. 2007;102(suppl S2):95–103 [DOI] [PubMed] [Google Scholar]
- 172.Iden G. The labor force experience of Black youth: a review. Mon Labor Rev. 1980;103(8):10–16 [Google Scholar]
- 173.Ihlanfeldt K, Sjoquist D. Job accessibility and racial differences in youth employment rates. Am Econ Rev. 1990;80(1):267–276 [Google Scholar]
- 174.Quillian L. The decline of male employment in low-income Black neighborhoods, 1950–1990. Soc Sci Res. 2003;32(2):220–250 [Google Scholar]
- 175.Camp DE, Klesges RC, Relyea G. The relationship between body weight concerns and adolescent smoking. Health Psychol. 1993;12(1):24–32 [DOI] [PubMed] [Google Scholar]
- 176.Barton J, Chassin L, Presson CC, et al. Social image factors as motivators of smoking initiation in early and middle adolescence. Child Dev. 1982;53(6):1499–1511 [PubMed] [Google Scholar]
- 177.Peterson DE, Zeger SL, Remington PL, et al. The effect of state cigarette tax increases on cigarette sales, 1955 to 1988. Am J Public Health. 1992;82(1):94–96 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Centers for Disease Control and Prevention Cigarette smoking before and after an excise tax increase and an antismoking campaign—Massachusetts, 1990–1996. MMWR Morb Mortal Wkly Rep. 1996;45(44):966–970 [PubMed] [Google Scholar]