Abstract
Objectives. We investigated whether, and under what conditions, informal caregiving is associated with improved self-reported physical and mental health, most notably in terms of cognitive functioning.
Methods. We performed a cross-sectional analysis of 2008 data from the Gazel Cohort Study, which involved 10 687 men and women aged 54 to 70 years. Multivariate linear and logistic regression models were used to estimate the associations between self-reported health and caregiving status and burden.
Results. Regular caregivers with the highest burden scores reported significantly worse health status than did noncaregivers for almost all of the physical and mental outcomes evaluated after adjustment for potential confounding factors. In particular, they reported more cognitive complaints (odds ratio [OR] = 1.44; 95% confidence interval [CI] = 1.21, 1.73). Conversely, caregivers with the lowest burden scores reported better perceived health status, less physical and mental tiredness, and fewer depressive symptoms (OR = 0.50; 95% CI = 0.37, 0.68) than did noncaregivers; however, they did not report decreases in cognitive difficulties (OR = 0.98; 95% CI = 0.81, 1.18).
Conclusions. Our findings support the hypothesis that caregiving can have positive effects on health, provided that caregiving activities themselves are not too heavy a burden.
The past few decades have been marked by substantial improvements in disability-free life expectancy across most developed countries.1 Yet, management of the dependent population has become an increasing matter of concern for policymakers given the speed and magnitude of population aging in these societies. In 2000 in France, the number of dependent individuals aged 60 years or older was estimated to be around 800 000, and worst-case scenarios predict that this population will increase by 80% by the end of the 2030s.2 Informal caregivers of dependent elderly individuals will thus assume a role of growing importance, whether in terms of quantity and quality of care provided or in terms of economic implications for health systems with tight resources.
A growing literature is focusing on the repercussions of caregivers’ activities on their mental and physical health. Most studies indicate that caregivers experience adverse consequences linked to the chronic stress and strain induced by continual or intense care tasks, generically referred to as “caregiver burden.”3–6 A few studies have also enlightened the possible positive repercussions of caregiving, mostly in connection with the feelings of personal fulfillment and satisfaction resulting from providing assistance.3,7,8 Moreover, recent studies have emphasized the beneficial influence on health of increases in physical activity resulting from care tasks, notably in terms of mortality.9,10 These diverse results stress the importance of considering caregivers as a multifaceted population with respect to the ways in which they cope emotionally, but also physically, with a dependent elderly person.
We investigated whether, and under what conditions, caregiving is associated with better self-reported physical and mental health, notably in terms of cognitive functioning. To our knowledge, no study has thus far evaluated these associations in a large population with a validated assessment tool that categorizes caregivers according to amount of perceived burden. We used 2008 data from the French Gazel Cohort Study to detail cross-sectional relationships.
METHODS
Electricité de France-Gaz de France (EDF-GDF) is France's national electricity and gas utility. The company employs approximately 150 000 workers in all regions of France. Since 1978, its medical department has maintained a comprehensive database of the company's workforce that includes demographic, socioeconomic, and occupational data on each employee.11,12 The Gazel Cohort Study was set up in 1989 to supplement these data with information from individual self-questionnaires on familial, social, and occupational environments along with lifestyle and health conditions. Details concerning recruitment, follow-up, and the characteristics of the volunteers have been described elsewhere.13,14
Briefly, 20 625 employees (5614 women and 15 011 men aged 35–50 years) consented to participate in the cohort. A postal questionnaire including a large set of systematically addressed items is sent to the participants on a yearly basis, and data are extracted regularly from the files of the personnel and the company's medical department as well as from national registers. In addition, different sets of questions are implemented in different study years. In 2008, a module of questions regarding informal caregiving status and burden was added.
Informal Caregiving Assessment
To be included in our cross-sectional analysis of 2008 Gazel cohort (n = 13 698) data, participants had to have answered the 2 questions regarding caregiving status (n = 11 443): “Are there one or more people aged more than 65 in your social sphere (spouse, family relative, other) who need assistance in their daily life?” and “If so, do you provide regular assistance to this person/these people?” Participants who answered yes to both questions were defined as regular caregivers.
We used the 22-item version of the Zarit Burden Interview (ZBI) to assess caregiving burden.15 The ZBI is a widely used self-administered questionnaire assessing the burden associated with providing home care for a person with functional–behavioral impairments. The items take into account caregivers’ finances, interpersonal relationships, and personal, professional, family, and social life. Each item, coded from 0 (never) to 4 (nearly always), quantifies the frequency of burdened feelings regarding these areas.
The French version of the ZBI has been psychometrically validated.16,17 We assessed the psychometric qualities of the ZBI in our sample, and the instrument showed good internal consistency (Cronbach α = 0.92). We calculated the sum of the 22 item scores for each caregiver, resulting in a global score with a range of 0 points (no burden) to 81 points (maximal burden; for score distribution details, see Figure A, available as a supplement to the online version of this article at http://www.ajph.org). Regular caregivers were stratified into 4 groups according to global score quartiles; the 1st quartile was made up of caregivers with the lowest burdens, and the 4th quartile was made up of caregivers with the highest burdens.
Participants not providing regular assistance to a dependent elderly person were stratified into 2 groups: those not having any dependent elderly individuals in their social sphere (“noncaregivers,” the reference group) and those having one or more dependent elderly individuals in their social sphere but not regularly caring for them (“potential regular caregivers”). Caregivers who did not fully complete the ZBI or who did not provide information on the primary characteristics of care recipients (n = 756) were excluded from study, resulting in a final study sample of 10 687 individuals. This sample did not differ from the other Gazel participants in terms of age; however, it included a higher percentage of men, and the educational level of its members was higher on average.
Self-Reported Health Assessment
Four areas of self-reported health were evaluated: perceived health, depressive symptoms, cognitive complaints, and health events (hospitalizations and diseases). Perceived health was measured with 3 scales (general health, physical tiredness, and mental tiredness), with item responses ranging from very good (1) to very poor (8). Depressive symptoms were measured with the 20-item Center for Epidemiologic Studies Depression Scale. Male participants with a total score of at least 17 and female participants with a total score of at least 23 were defined as being at high risk for clinical depression.18
Cognitive complaints were assessed with 1 binary general question about participants’ memory (“Do you experience any difficulties concerning your memory?”) and 6 additional binary questions concerning difficulties related to memory, calculation, language, and spatial orientation. Participants were asked whether they had been hospitalized during the preceding 12 months, and they reported each disease or disorder that occurred during this period. Diseases were classified into 7 nonexclusive categories: cardiovascular, respiratory, digestive, osteoarticular, genitourinary, metabolic, and cancers (for a complete list of specific diseases, see Table A, available as a supplement to the online version of this article at http://www.ajph.org).
Covariates
Participants reported their marital status (married or living with a partner vs single, divorced, or widowed), educational level (less than high school vs high school or above), socioprofessional status (manager–executive, intermediate occupation [e.g., technicians and associate professionals], or office–manual worker), retirement status (active vs retired), engagement in sports activities (yes or no), current alcohol and tobacco consumption (yes or no), and the number of individuals in their household (1, 2, or 3 or more). The characteristics of the primary care recipient were also assessed, including the type of relationship with the caregiver (spouse, family, other), place of residence (own home, caregiver's home, retirement home, other), type of disability (mental, physical, or both), and presence of behavioral disorders (e.g., aggressiveness).
Statistical Analysis
We used the χ2 test and analyses of variance to evaluate differences in the characteristics of the study population according to caregiving status and burden. Among regular caregivers, we conducted tests for trends across levels of burden.
Analyses of covariance (for quantitative outcomes) and logistic regression analyses (for binary outcomes) were used to evaluate multivariate associations of caregiving status or burden with self-reported health. We identified confounding factors from the literature on health determinants and from univariate associations observed in our data. All models were adjusted at minimum for participants’ age, gender, educational level, occupational status, smoking status, alcohol consumption, and sports activities. Additional adjustments were made depending on the outcome assessed. Plausible interactions between caregiving status and the primary characteristics of caregivers and care recipients were evaluated.
In addition, we conducted sensitivity analyses in which caregivers were stratified according to the predefined ZBI score cut points (0–20 = little or no burden, 21–40 = mild to moderate burden, 41–60 = moderate to severe burden, 61–88 = severe burden) instead of ZBI score quartiles. We set the level of statistical significance for our analyses at P < .05 (2-tailed). SAS version 9.2 (SAS Institute, Cary, NC) was used in conducting all of the statistical analyses.
RESULTS
Participants ranged in age from 54 to 70 years, and 75.0% were men. Most of the participants were married or living with a partner (85.3%) and retired (87.6%), and 27.1% (n = 2901) were regular informal caregivers (for a complete description of the study population characteristics, see Table B, available as a supplement to the online version of this article at http://www.ajph.org).
Men (mean = 63.7 years, SD = 2.9) were older than women (mean = 61.0 years, SD = 4.2; P < .001) on average and were more likely to be married or to live with a partner (90.2% vs 70.8%; P < .001) and to have a high socioprofessional status (43.3% vs 18.3%; P < .001). Women were more likely to be caregivers (29.6% vs 26.3%; P < .001), and their mean ZBI global score (22.0; SD = 14.9) was higher than that of men (17.4; SD = 12.7; P < .001). ZBI score quartiles (increasing from no burden to maximum burden) among caregivers ranged from 0 to 8 points (1st quartile; n = 729), 9 to 15 points (2nd quartile; n = 718), 16 to 26 points (3rd quartile; n = 740), and 27 to 81 points (4th quartile; n = 714).
Characteristics of the study population according to caregiving status and burden are detailed in Table 1. Most of the participants who reported no regular caregiving activity did not have any dependent elderly individuals in their social sphere (i.e., noncaregivers; n = 7076); the remainder had dependent elderly people in their social sphere but did not regularly care for them (i.e., potential regular caregivers; n = 710). This latter group was characterized by a lower mean age, a higher percentage of men, a higher average socioprofessional status, and a higher percentage of individuals who were married or living with a partner.
TABLE 1.
Sample Characteristics According to Caregiving Status and Burden: Gazel Cohort Study, France, 2008
| Regular Caregiver Level of Burden |
||||||||
| Characteristic | Noncaregivers(n = 7076) | Potential Regular Caregivers (n = 710) | 1st Quartile(n = 729) | 2nd Quartile(n = 718) | 3rd Quartile(n = 740) | 4th Quartile(n = 714) | Pa | P for Trendb |
| ZBI global score | ||||||||
| Range | … | … | 0–8 | 9–15 | 16–26 | 27–81 | … | … |
| Mean (SD) | … | … | 4.7 (2.2) | 11.8 (2.0) | 20.5 (3.2) | 38.0 (9.7) | … | … |
| Age, y, mean (SD) | 63.2 (3.5) | 62.6 (3.4) | 62.9 (3.4) | 62.7 (3.3) | 62.6 (3.4) | 62.4 (3.4) | <.001 | .004 |
| Women, % | 24.5 | 21.0 | 20.2 | 24.2 | 27.2 | 37.7 | <.001 | <.001 |
| Marital status, % | .002 | .18 | ||||||
| Married/living with partner | 84.7 | 90.3 | 87.1 | 85.2 | 86.1 | 84.2 | ||
| Single/divorced/widowed | 15.3 | 9.8 | 13.0 | 14.8 | 13.9 | 15.9 | ||
| No. of individuals in household, % | <.001 | .25 | ||||||
| 1 | 13.0 | 7.9 | 9.8 | 12.4 | 12.3 | 12.0 | ||
| 2 | 76.7 | 80.4 | 80.1 | 74.2 | 75.1 | 72.2 | ||
| ≥3 | 10.3 | 11.7 | 10.1 | 13.5 | 12.6 | 15.7 | ||
| High school education or above, % | 27.2 | 31.4 | 24.8 | 26.4 | 27.4 | 27.9 | .14 | .17 |
| Socioprofessional category, %c | <.001 | .28 | ||||||
| Manager/executive | 37.4 | 44.9 | 32.3 | 35.0 | 36.5 | 32.4 | ||
| Intermediate occupationd | 52.6 | 48.0 | 54.5 | 55.2 | 55.2 | 57.8 | ||
| Office/manual worker | 10.0 | 7.1 | 13.2 | 9.8 | 8.3 | 9.8 | ||
| Retired, % | 87.6 | 88.0 | 88.9 | 89.4 | 86.7 | 85.7 | .29 | .03 |
| Engages in sports activities, % | 66.8 | 63.7 | 66.1 | 68.4 | 69.8 | 64.1 | .11 | .58 |
| Current smoker, % | 9.0 | 7.1 | 8.8 | 8.5 | 6.9 | 8.7 | .28 | .64 |
| Alcohol use, %e | 86.1 | 90.4 | 90.2 | 88.9 | 86.2 | 85.4 | <.001 | .002 |
| No. of glasses of alcohol per day, mean (SD) | 2.6 (1.9) | 2.9 (2.1) | 2.7 (1.9) | 2.8 (1.9) | 2.6 (1.9) | 2.6 (1.9) | <.001 | .03 |
Note. ZBI = Zarit Burden Interview. Burden levels were assessed with the ZBI; higher ZBI global score quartiles represent increased burden. Participants who answered yes to the 2 questions regarding caregiving status (“Are there one or more people aged more than 65 in your social sphere [spouse, family relative, other] who need assistance in their daily life?” and “If so, do you provide regular assistance to this person/these people?”) were defined as regular caregivers. Participants not providing regular assistance to a dependent elderly person were stratified as those not having any dependent elderly individuals in their social sphere (noncaregivers) and those having one or more dependent elderly individuals in their social sphere but not regularly caring for them (potential regular caregivers). Sample size was n = 10 687. Ellipses indicate that performing tests were not relevant.
Univariate analysis assessing differences across all categories of caregiving status and burden.
Univariate analysis assessing trends across quartiles of regular caregivers.
Most recent occupation.
Defined as a technician or associate professional.
At least 1 glass of wine, 1 beer, or 1 aperitif during the preceding week.
Among regular caregivers, the higher the burden, the higher were the percentages of women (P for trend < .001) and individuals who were still working (P for trend = .03); higher burdens were also associated with younger age (P for trend = .004) and less alcohol consumption (P for trend = .002). No significant marital status (P for trend = .18) or educational level (P for trend = .17) differences were observed across levels of burden.
Most of the care recipients were family relatives of the caregiver, were living in their own home, and had a physical disability as the origin of their dependency (Table 2 ). Higher numbers of care tasks provided, situations in which the care recipient was a spouse or family member, and situations in which the care recipient had a mental disability or a behavioral disorder were associated with significantly higher caregiver burdens.
TABLE 2.
Caregiving Elements and Characteristics of Primary Care Recipients: Gazel Cohort Study, France, 2008
| Regular Caregiver Level of Burden |
|||||
| 1st Quartile(n = 729) | 2nd Quartile(n = 718) | 3rd Quartile(n = 740) | 4th Quartile(n = 714) | P | |
| Caregiving element | |||||
| No. of care recipients, %a | <.001 | ||||
| 1 | 82.4 | 73.4 | 74.2 | 76.6 | |
| 2 | 14.7 | 21.6 | 22.2 | 18.9 | |
| ≥3 | 2.9 | 5.0 | 3.7 | 4.5 | |
| No. of care tasks provided, mean (SD)b | 3.3 (1.3) | 3.7 (1.3) | 4.0 (1.2) | 4.4 (1.3) | <.001 |
| No other informal caregiver, % | 18.2 | 17.1 | 28.0 | 37.9 | <.001 |
| Care recipient characteristic | |||||
| Age, y, mean (SD) | 85.9 (6.9) | 86.5 (6.3) | 86.4 (6.6) | 86.2 (7.7) | .48 |
| Women, % | 82.3 | 80.6 | 80.1 | 79.2 | .53 |
| Relationship with caregiver, % | <.001 | ||||
| Family relativec | 70.2 | 77.0 | 81.9 | 83.4 | |
| Spouse | 2.9 | 1.0 | 2.7 | 7.0 | |
| Other | 26.9 | 22.1 | 15.4 | 9.6 | |
| Place of residence, % | <.001 | ||||
| Own home | 75.5 | 67.7 | 64.1 | 54.3 | |
| Residing with the caregiver | 3.5 | 2.7 | 5.9 | 14.1 | |
| Retirement home | 16.6 | 23.6 | 25.6 | 26.1 | |
| Other | 4.3 | 6.1 | 4.4 | 5.5 | |
| Type of disability, % | <.001 | ||||
| Mental | 6.2 | 8.5 | 13.5 | 16.5 | |
| Physical | 82.5 | 74.7 | 63.4 | 48.8 | |
| Mental and physical | 11.2 | 16.8 | 23.1 | 34.8 | |
| Behavioral disorder, % | 3.1 | 7.6 | 11.2 | 25.4 | <.001 |
Note. Percentages may not total 100 because of rounding. Burden levels were assessed with the Zarit Burden Interview; higher global score quartiles represent increased burden. Sample size was n = 2901.
Including the primary care recipient.
Care tasks were as follows: presence and support, assistance with basic activities, assistance with household activities, assistance with finances and paperwork, assistance with respect to supervision, and assistance with respect to in-home help.
Parent, grandparent, or parent-in-law of the caregiver.
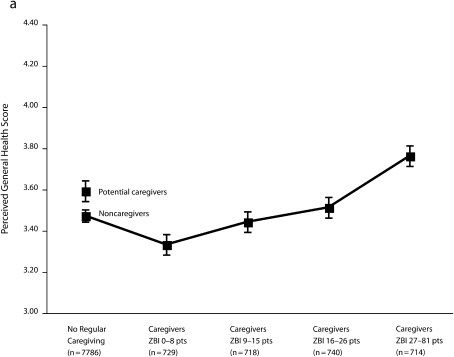
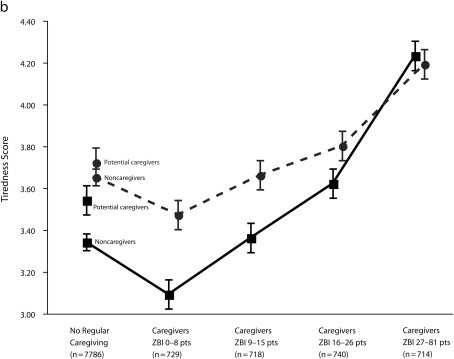
After adjustment, regular caregivers with the lowest burdens reported better perceived general health and less physical and mental tiredness than did noncaregivers, but these outcomes gradually changed as caregiver level of burden increased because regular caregivers in the 3rd and 4th quartiles of burden reported less favorable outcomes than did noncaregivers (Figure 1).
FIGURE 1.
Associations of caregiving status and burden with (a) perceived general health and (b) physical and mental tiredness: Gazel Cohort Study, France, 2008.
Note. ZBI = Zarit Burden Interview. Mean values (bars are standard errors) from linear regression models (adjusted for age, gender, educational level, most recent occupation, retirement status, smoking status, alcohol consumption, and sports activity) are shown. For differences across noncaregivers and quartiles of caregivers, P < .001 for perceived general health and for physical and mental tiredness. Higher scores indicate poorer self-reported health. Solid line represents mental tiredness score. Dotted line represents physical tiredness score. Sample size was n = 10 687.
As can be seen in Table 3, a similar J-shaped pattern of association was observed between caregiving status and depressive symptoms: caregivers with the lowest burdens were half as likely as were noncaregivers to be depressed (odds ratio [OR] = 0.50; 95% confidence interval [CI] = 0.37, 0.68), whereas caregivers with the highest burdens were at significantly increased risk of depression (OR = 2.26; 95% CI = 1.86, 2.75) compared with their noncaregiving counterparts. This pattern of association was not observed for physical health events; relative to noncaregivers, regular caregivers in all categories had the same or a higher risk of having had a disease in the preceding 12 months.
TABLE 3.
Multivariate Associations of Self-Reported Mental and Physical Health With Caregiving Status and Burden: Gazel Cohort Study, France, 2008
| Potential Regular Caregivers (n = 710), OR (95% CI) | Regular Caregiver Level of Burden |
|||||
| Noncaregivers(n = 7076; Ref) | 1st Quartile (n = 729), OR (95% CI) | 2nd Quartile (n = 718), OR (95% CI) | 3rd Quartile (n = 740), OR (95% CI) | 4th Quartile (n = 714), OR (95% CI) | ||
| Depressiona | ||||||
| Total | 1.00 | 1.54*** (1.24, 1.91) | 0.50*** (0.37, 0.68) | 0.78 (0.60, 1.01) | 1.05 (0.83, 1.33) | 2.26*** (1.86, 2.75) |
| Menb | 1.00 | 1.39*** (1.08, 1.79) | 0.54*** (0.39, 0.76) | 0.75 (0.55, 1.02) | 1.19 (0.91, 1.55) | 2.58*** (2.03, 3.27) |
| Womenc | 1.00 | 2.11*** (1.37, 3.25) | 0.38* (0.17, 0.83) | 0.87 (0.52, 1.45) | 0.74 (0.45, 1.22) | 1.80*** (1.28, 2.54) |
| Cognitive complaintsd | ||||||
| Memory difficulties | 1.00 | 1.32** (1.10, 1.59) | 0.98 (0.81, 1.18) | 1.22* (1.02, 1.47) | 1.18 (0.98, 1.41) | 1.44*** (1.21, 1.73) |
| Memory lapses in daily living activities | 1.00 | 1.08 (0.78, 1.50) | 0.99 (0.70, 1.39) | 1.28 (0.93, 1.75) | 1.17 (0.86, 1.60) | 1.68*** (1.28, 2.21) |
| Difficulty retaining new information | 1.00 | 1.16 (0.90, 1.49) | 0.92 (0.70, 1.21) | 1.04 (0.80, 1.35) | 1.09 (0.85, 1.39) | 1.21 (0.96, 1.53) |
| Difficulty remembering past events | 1.00 | 1.40** (1.10, 1.77) | 0.98 (0.75, 1.28) | 0.97 (0.74, 1.27) | 1.02 (0.79, 1.31) | 1.53*** (1.22, 1.92) |
| Calculation difficulties | 1.00 | 1.07 (0.72, 1.61) | 1.18 (0.78, 1.78) | 1.04 (0.68, 1.60) | 1.48* (1.03, 2.12) | 1.45* (1.04, 2.02) |
| Language difficulties | 1.00 | 1.34** (1.08, 1.67) | 0.86 (0.67, 1.11) | 1.26* (1.00, 1.58) | 1.34** (1.08, 1.66) | 1.29* (1.04, 1.60) |
| Spatial orientation difficulties | 1.00 | 1.28 (0.71, 2.34) | 0.98 (0.47, 2.04) | 1.23 (0.65, 2.33) | 1.43 (0.81, 2.55) | 1.59 (0.97, 2.61) |
| Health events in preceding 12 mo | ||||||
| Hospitalizations | 1.00 | 0.95 (0.76, 1.19) | 0.92 (0.74, 1.15) | 0.88 (0.70, 1.10) | 1.03 (0.83, 1.27) | 0.84 (0.67, 1.06) |
| Cardiovascular disease | 1.00 | 1.18 (1.00, 1.39) | 0.93 (0.79, 1.10) | 1.01 (0.86, 1.19) | 1.16 (0.98, 1.36) | 1.29** (1.09, 1.52) |
| Respiratory disease | 1.00 | 0.97 (0.78, 1.20) | 0.83 (0.67, 1.03) | 1.00 (0.81, 1.24) | 1.16 (0.95, 1.42) | 1.21 (1.00, 1.48) |
| Digestive disease | 1.00 | 1.15 (0.97, 1.37) | 1.06 (0.90, 1.27) | 1.16 (0.98, 1.38) | 1.20* (1.01, 1.42) | 1.45*** (1.23, 1.72) |
| Osteoarticular disease | 1.00 | 1.17 (0.98, 1.39) | 1.12 (0.94, 1.34) | 1.13 (0.94, 1.34) | 1.23* (1.03, 1.47) | 1.44*** (1.19, 1.74) |
| Genitourinary disease | 1.00 | 1.06 (0.88, 1.29) | 0.95 (0.78, 1.16) | 1.09 (0.90, 1.32) | 1.22* (1.02, 1.47) | 1.29** (1.07, 1.55) |
| Metabolic disease | 1.00 | 1.16 (0.98, 1.38) | 1.09 (0.92, 1.29) | 0.96 (0.81, 1.14) | 0.96 (0.81, 1.14) | 1.05 (0.88, 1.25) |
| Cancer | 1.00 | 0.92 (0.60, 1.41) | 0.74 (0.46, 1.17) | 0.97 (0.64, 1.47) | 0.77 (0.49, 1.22) | 1.28 (0.88, 1.87) |
Note. CI = confidence interval; OR = odds ratio. Burden levels were assessed with the Zarit Burden Interview; higher global score quartiles represent increased burden. Analyses controlled for age, gender, educational level, occupational status, retirement, smoking status, alcohol consumption, and sports activities. Adjusted pseudo-R2 values ranged from 0.04 to 0.06 for depressive state models, from 0.04 to 0.09 for cognitive complaints models, and from 0.01 to 0.03 for health events models. Participants who answered yes to the 2 questions regarding caregiving status (“Are there one or more people aged more than 65 in your social sphere [spouse, family relative, other] who need assistance in their daily life?” and “If so, do you provide regular assistance to this person/these people?”) were defined as regular caregivers. Participants not providing regular assistance to a dependent elderly person were stratified as those not having any dependent elderly individuals in their social sphere (noncaregivers) and those having one or more dependent elderly individuals in their social sphere but not regularly caring for them (potential regular caregivers). Sample size was n = 10 687.
Total scores of 17 or above among men and 23 or above among women on the Center for Epidemiologic Studies Depression Scale indicate a high risk for clinical depression.
n = 8014.
n = 2673.
Additional adjustment was made for depression, sleep disorders, and number of individuals in the household.
*P < .05; **P < .01; ***P < .001.
Results concerning cognitive complaints are also shown in Table 3. After additional control for depressive symptoms, sleep disorders, and number of individuals in the household, caregivers with the lowest burdens had similar risks of experiencing memory, calculation, language, and spatial orientation difficulties as did noncaregivers. Risks of memory and language difficulties were significantly increased among individuals in the 2nd quartile of burden, and risks of calculation difficulties were significantly increased among those in the 3rd quartile of burden. Caregivers in the highest quartile reported significantly, or nearly significantly, altered functioning in the case of all cognitive indicators.
Finally, potential regular caregivers had poorer status scores than did noncaregivers and low-burden caregivers for almost all health outcomes. Notably, they had worse perceived general health and more mental tiredness (Figure 1) and were at significantly higher risk of depression and memory difficulties (Table 3).
No significant interactions between caregiving burden and the primary characteristics of the care recipient existed for any of the health outcomes. Separate analyses according to participant gender showed similar patterns of associations among men and among women for all outcomes, although there was a significant interaction between gender and caregiving in the unstratified analysis focusing on depression (P = .04). Also, similar patterns of associations were revealed in sensitivity analyses in which regular caregivers were stratified according to the ZBI cut points instead of quartiles of burden (Table C, available as a supplement to the online version of this article at http://www.ajph.org).
DISCUSSION
In our analysis of a French adult sample, regular informal caregivers with the highest burden scores reported significantly worse physical and mental health, and in particular more cognitive impairment, than did people not having any dependent elderly individuals in their social sphere. Conversely, the caregivers with the lowest burdens reported better perceived health status and less depressive symptoms than did noncaregivers, but they did not report decreases in cognitive difficulties. These associations remained statistically significant after potential confounding factors had been taken into account and did not differ according to the gender of the participant or the characteristics of the care recipient. Furthermore, the observed differences in perceived general health and tiredness scores (ranging from 0.4 to 1.1 points) were clinically relevant and consistent with the onset of a large range of physical and mental diseases.19
The percentages of regular caregivers in our study sample were relatively high in comparison with those observed in other population data, especially among men (26% of men aged 59–70 years, compared with 30% of women aged 54–70 years). Indeed, according to previous research percentages of individuals providing care for older adults range from 4% to 22% in Europe.20 In a recent National Alliance for Caregiving report, adult caregivers of recipients aged 50 years or older were estimated to account for 19% of the US population, with two thirds being women.21
There are several reasons for these discrepancies in caregiving prevalence, notably temporal trends in disability rates and our somewhat less stringent definitions of caregiving (i.e., assistance in daily activities, whatever the types and numbers of tasks performed) and care recipients (i.e., any mentally or physically disabled individuals aged 65 years or older in the caregiver's social sphere) relative to those used in previous reports. The primary characteristics of the Gazel study participants, who represent a rather healthy, mainly recently retired population, and the fact that participants identified themselves as caregivers (as opposed to care recipients or health professionals identifying them as such) may also partially explain our high caregiving rate among men.
The burden perceived by caregivers was also lower in our study than in previous analyses in which the French version of the ZBI has been used.16,17,22 This difference can be partly explained by the fact that a majority of our caregivers were men who, on average, reported lower perceived burdens than did women. Moreover, previous studies involving French-speaking populations mostly focused on spousal care recipients with dementia, whereas the majority of our caregivers were assisting elderly individuals with physical (but not mental) disabilities and, less frequently, behavioral disorders. As a result of these considerations, we used ZBI global score quartiles to categorize caregivers rather than the predefined ZBI cut points validated among caregivers of elderly people with dementia. However, when we conducted sensitivity analyses using the ZBI cut points the findings were similar to those detailed here.
The influence of informal caregiving on health is the subject of an extensive yet sometimes inconsistent literature. Conventional wisdom links caregiving to a decline in health through various pathways related to chronic stress, most notably depressed immune state,23 greater cardiovascular reactivity,24 and psychological distress.25 Consistent with this chronic stress theory, several studies have described caregiving as a predictor of depression26,27 and cardiovascular conditions.28 Yet, in a number of cases results are somewhat less straightforward, in particular those regarding mortality; some longitudinal studies have shown that caregiving is a mortality risk factor,29,30 whereas others have not.7,9 Recent research has related this inconsistency to the need to better account for caregivers’ increased physical activity, which could partly mediate the association between caregiving and health.9,10
In any case, these results stress the importance of considering caregivers not simply as a homogeneous group in terms of risks of adverse health events but rather as a complex population with levels of risk that vary according to the way they cope (physically, mentally, and emotionally) with a dependent elderly relative or friend. A strength of our study is that we took this variance into account by stratifying caregivers according to their self-perceived level of burden, using a validated scale that was also closely linked to the intensity of the caregiving activity in question, and by adjusting for physical activity in our multivariate analyses.
Depression was significantly less frequent, general health status was better, and physical and mental tiredness was less frequent among caregivers in our sample in the lowest quartile of burden relative to participants not having any dependent elderly individuals in their social sphere. These findings provide additional strength to the hypothesis that informal caregiving can have a positive impact on health, provided the tasks involved are not the source of too much burden. In addition to the probable benefits of moderately increased physical activity, several factors could explain this seemingly paradoxical relationship between caregiving and health. One possible explanation is that the personal fulfillment and satisfaction derived from providing assistance to a close or beloved person can lead to an increase in perceived health status.8,31 Caregivers may also reduce risk behaviors to make sure they can effectively alleviate the weaknesses and incapacities of the care recipient.
A few previous studies have evaluated the influence of caregiving on cognitive functioning. Most were performed among small samples composed of spousal caregivers,25,32–34 and one was carried out among a large sample of older female spouses.35 All described an increased risk of poor cognitive performance among caregivers that may have been partly mediated by psychological distress, depression, and social isolation. Our findings are in line with these results and provide evidence of cognitive complaints among a large sample of caregivers who were mostly men and the offspring of the care recipient even after relevant adjustments.
Furthermore, our results suggest that these symptoms appear early among caregivers, even those with low levels of burden; indeed, we observed significant increases in memory complaints among individuals with ZBI scores as low as 9 to 15. Interestingly, this relationship that originated at very low levels of burden was also observed for depression and for perceived health and tiredness scores. These findings seem to show that caregivers with little or no burden (as defined by the usual ZBI score cut point of 20 or below) may actually correspond to a rather heterogeneous population in terms of adverse health events.
In our study, we separated noncaregivers (those not providing care because they did not report any dependent elderly individuals in their social sphere) from potential regular caregivers (those not regularly providing care despite the presence of an elderly dependent person), allowing us to focus specifically on the former group. Not having made this distinction would have led to an inaccurate evaluation of the impact of regular caregiving, whether positive or negative, on self-reported health. Indeed, potential caregivers reported particularly poor health relative to noncaregivers but also relative to regular caregivers with low burdens. This “healthy regular caregiver effect” lends support to previous research indicating the importance of mental and physical health in both the beginning and the continuing process of caregiving,36 as well as emphasizing the need for future public health policies to focus specifically on potential caregivers.
Limitations
The cross-sectional design of our study precludes any conclusions about causality in the associations we observed. In particular, it does not allow establishing the direction of the relationships between caregiving status, burden, and health. Although it is likely that, as described in previous research, prevalent diseases may worsen caregivers’ burden,37,38 one cannot rule out the possibility that an increased caregiving burden can in itself lead to a decrease in health status. With respect to cognitive symptoms, it seems more likely that the observed significant associations should be interpreted as a negative impact of caregiving on mental health.
This study has other limitations that should be taken into consideration as well. Our sample was initially composed of workers (three quarters of whom were men) who volunteered to participate in a study on health. Therefore, the participants do not reflect the general population of France but, rather, represent a relatively healthy and employed or recently retired subpopulation. The Gazel cohort, however, is comprised of a wide range of socioeconomic levels, and the epidemiologic profile of the study population is close to that of the French general population in terms of distributions of disorders and of causes of death.39,40 Furthermore, few previous studies have focused on the health of caregivers who were mostly men and offspring of the care recipient. Another limitation relates to the lack of detail concerning the health of care recipients and the care services provided, most notably in terms of durations and frequencies of assistance, which prevents a precise quantification of caregiving intensity.
Conclusions
Our results highlight the close and complex relationships between caregiving and health status. In particular, they emphasize the need to use validated tools to precisely take into account the regularity of caregiving activities and the level of caregivers’ burden when screening for populations at risk for adverse outcomes.
Although our study adds further evidence for potentially beneficial effects of regular caregiving on perceived general health, tiredness, and depressive symptoms, this is not the case concerning cognitive complaints. Longitudinal investigations and intervention programs using objective performance tests will be necessary to better delineate the influences of informal caregiving and its associated burdens on the development of cognitive impairments. Such information would be particularly useful for policymakers aiming to provide efficient assistance to caregivers as well as care recipients.
Acknowledgments
The Gazel Cohort Study was funded by EDF-GDF and Inserm, and received grants from the Cohortes Santé TGIR Program, Agence Nationale de la Recherche (ANR) and Agence Française de Sécurité Sanitaire de l'Environnement et du Travail (AFSSET).
We express our thanks to EDF-GDF, especially to the Service Général de Médecine de Contrôle and to the Caisse Centrale d'Action Sociale du personnel des industries électriques et gazières. We wish to acknowledge the Cohortes team of Inserm U1018-Université Versailles St-Quentin responsible for management of the Gazel Cohort Study database. We also thank Diane Cyr and Aurélien Latouche for their assistance in the writing of this article.
Human Participant Protection
The Gazel Cohort Study was approved by the Commission Nationale de l'Informatique et des Libertés and the Ethics Evaluation Committee of Inserm. Participants provided written informed consent.
References
- 1.Christensen K, Doblhammer G, Rau R, Vaupel JW. Ageing populations: the challenges ahead. Lancet. 2009;374(9696):1196–1208 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Duée M, Rebillard C. Santé et protection sociale: dépendance. : Données Sociales: La Société Française. Paris, France: National Institute for Statistics and Economic Studies; 2006:613–619 [Google Scholar]
- 3.Carretero S, Garces J, Rodenas F, Sanjose V. The informal caregiver's burden of dependent people: theory and empirical review. Arch Gerontol Geriatr. 2009;49(1):74–79 [DOI] [PubMed] [Google Scholar]
- 4.Doran T, Drever F, Whitehead M. Health of young and elderly informal carers: analysis of UK census data. BMJ. 2003;327(7428):1388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Morimoto T, Schreiner AS, Asano H. Caregiver burden and health-related quality of life among Japanese stroke caregivers. Age Ageing. 2003;32(2):218–223 [DOI] [PubMed] [Google Scholar]
- 6.Schulz R, Martire LM. Family caregiving of persons with dementia: prevalence, health effects, and support strategies. Am J Geriatr Psychiatry. 2004;12(3):240–249 [PubMed] [Google Scholar]
- 7.Brown SL, Smith DM, Schulz R, et al. Caregiving behavior is associated with decreased mortality risk. Psychol Sci.. 2009;20(4):488–494 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lopez J, Lopez-Arrieta J, Crespo M. Factors associated with the positive impact of caring for elderly and dependent relatives. Arch Gerontol Geriatr. 2005;41(1):81–94 [DOI] [PubMed] [Google Scholar]
- 9.Fredman L, Cauley JA, Satterfield S, et al. Caregiving, mortality, and mobility decline: the Health, Aging, and Body Composition (Health ABC) Study. Arch Intern Med. 2008;168(19):2154–2162 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fredman L, Cauley JA, Hochberg M, Ensrud KE, Doros G. Mortality associated with caregiving, general stress, and caregiving-related stress in elderly women: results of caregiver-study of osteoporotic fractures. J Am Geriatr Soc. 2010;58(5):937–943 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Goldberg M, Blanc M, Chastang JF, Blanc C, Sommer M. The health data base of a nationwide company—its use in epidemiological studies. J Occup Med. 1982;24(1):47–52 [PubMed] [Google Scholar]
- 12.Goldberg M, Chevalier A, Imbernon E, Coing F, Pons H. The epidemiological information system of the French national electricity and gas company: the SI-EPI project. Med Lav. 1996;87(1):16–28 [PubMed] [Google Scholar]
- 13.Goldberg M, Leclerc A, Chastang JF, et al. Mise en place d'une cohorte épidémiologique à Electricité de France-Gaz de France: recrutement des volontaires. Principales caractéristiques de l’échantillon. Rev Epidemiol Sante Publique. 1990;38:265–268, 378–380 [Google Scholar]
- 14.Goldberg M, Leclerc A, Bonenfant S, et al. Cohort profile: the GAZEL Cohort Study. Int J Epidemiol. 2007;36(1):32–39 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zarit SH, Reever KE, Bach-Peterson J. Relatives of the impaired elderly: correlates of feelings of burden. Gerontologist. 1980;20(6):649–655 [DOI] [PubMed] [Google Scholar]
- 16.Hébert R, Bravo G, Girouard D. Fidélité de la traduction française de trois instruments d’évaluation des aidants naturels de malades déments. Can J Aging. 1993;12(3):324–337 [Google Scholar]
- 17.Hébert R, Bravo G, Préville M. Reliability, validity and reference values of the Zarit Burden Interview for assessing informal caregivers of community-dwelling older persons with dementia. Can J Aging. 2000;19(4):494–507 [Google Scholar]
- 18.Fuhrer R, Rouillon F. La version française de l’échelle CES-D (Center for Epidemiologic Studies-Depression Scale): description et traduction de l’échelle d'autoévaluation. Psychiatr Psychobiol. 1989;4:163–166 [Google Scholar]
- 19.Goldberg P, Gueguen A, Schmaus A, Nakache JP, Goldberg M. Longitudinal study of associations between perceived health status and self reported diseases in the French Gazel cohort. J Epidemiol Community Health. 2001;55(4):233–238 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Jacobs T, Lodewijckx E, Craeynest K, De Koker B, Vanbrabant A. Measuring informal care: a synthesis of European practices and a new proposal. Retraite et Société. 2005;46:59–87 [Google Scholar]
- 21.National Alliance for Caregiving Caregiving in the U.S.: a focused look at those caring for someone age 50 or older. Available at: http://assets.aarp.org/rgcenter/il/caregiving_09.pdf. Accessed March 17, 2011
- 22.Andrieu S, Balardy L, Gillette-Guyonnet S, et al. Burden experienced by informal caregivers assisting Alzheimer's patients in the REAL.FR study. Rev Med Interne. 2003;24(suppl 3):351s–359s [DOI] [PubMed] [Google Scholar]
- 23.Vedhara K, Cox NK, Wilcock GK, et al. Chronic stress in elderly carers of dementia patients and antibody response to influenza vaccination. Lancet. 1999;353(9153):627–631 [DOI] [PubMed] [Google Scholar]
- 24.King AC, Baumann K, O'Sullivan P, Wilcox S, Castro C. Effects of moderate-intensity exercise on physiological, behavioral, and emotional responses to family caregiving: a randomized controlled trial. J Gerontol A Biol Sci Med Sci.. 2002;57(1):M26–M36 [DOI] [PubMed] [Google Scholar]
- 25.Mackenzie CS, Wiprzycka UJ, Hasher L, Goldstein D. Associations between psychological distress, learning, and memory in spouse caregivers of older adults. J Gerontol B Psychol Sci Soc Sci. 2009;64(6):742–746 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gallicchio L, Siddiqi N, Langenberg P, Baumgarten M. Gender differences in burden and depression among informal caregivers of demented elders in the community. Int J Geriatr Psychiatry. 2002;17(2):154–163 [DOI] [PubMed] [Google Scholar]
- 27.Tennstedt S, Cafferata GL, Sullivan L. Depression among caregivers of impaired elders. J Aging Health. 1992;4(1):58–76 [DOI] [PubMed] [Google Scholar]
- 28.Lee S, Colditz GA, Berkman LF, Kawachi I. Caregiving and risk of coronary heart disease in U.S. women: a prospective study. Am J Prev Med. 2003;24(2):113–119 [DOI] [PubMed] [Google Scholar]
- 29.Schulz R, Beach SR. Caregiving as a risk factor for mortality: the Caregiver Health Effects Study. JAMA. 1999;282(23):2215–2219 [DOI] [PubMed] [Google Scholar]
- 30.Christakis NA, Allison PD. Mortality after the hospitalization of a spouse. N Engl J Med. 2006;354(7):719–730 [DOI] [PubMed] [Google Scholar]
- 31.Kramer BJ. Gain in the caregiving experience: where are we? What next? Gerontologist. 1997;37(2):218–232 [DOI] [PubMed] [Google Scholar]
- 32.de Vugt ME, Jolles J, van Osch L, et al. Cognitive functioning in spousal caregivers of dementia patients: findings from the prospective MAASBED study. Age Ageing. 2006;35(2):160–166 [DOI] [PubMed] [Google Scholar]
- 33.Vitaliano PP, Echeverria D, Yi J, Phillips PE, Young H, Siegler IC. Psychophysiological mediators of caregiver stress and differential cognitive decline. Psychol Aging. 2005;20(3):402–411 [DOI] [PubMed] [Google Scholar]
- 34.Vitaliano PP, Zhang J, Young HM, Caswell LW, Scanlan JM, Echeverria D. Depressed mood mediates decline in cognitive processing speed in caregivers. Gerontologist. 2009;49(1):12–22 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lee S, Kawachi I, Grodstein F. Does caregiving stress affect cognitive function in older women? J Nerv Ment Dis. 2004;192(1):51–57 [DOI] [PubMed] [Google Scholar]
- 36.McCann JJ, Hebert LE, Bienias JL, Morris MC, Evans DA. Predictors of beginning and ending caregiving during a 3-year period in a biracial community population of older adults. Am J Public Health. 2004;94(10):1800–1806 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Majerovitz SD. Predictors of burden and depression among nursing home family caregivers. Aging Ment Health. 2007;11(3):323–329 [DOI] [PubMed] [Google Scholar]
- 38.van den Heuvel ET, de Witte LP, Schure LM, Sanderman R, Meyboom-de Jong B. Risk factors for burn-out in caregivers of stroke patients, and possibilities for intervention. Clin Rehabil. 2001;15(6):669–677 [DOI] [PubMed] [Google Scholar]
- 39.Chevalier A, Leclerc A, Blanc C, Goldberg M. Disparités sociales et professionnelles de la mortalité des travailleurs d'Electricité de France-Gaz de France. Population (Paris). 1987;6:863–879 [Google Scholar]
- 40.Chevalier A, Goldberg M, Godard C, et al. Cancer incidence among active male workers at Electricité de France-Gaz de France. Rev Epidemiol Santé Publique. 1996;44(1):25–36 [PubMed] [Google Scholar]