Abstract
Objectives. We examined school days missed for routine dental care versus dental pain or infection to determine the relationship between children's oral health status and school attendance and performance.
Methods. We used 2008 data from the North Carolina Child Health Assessment and Monitoring Program. The study sample, weighted to reflect the state's population, included 2183 schoolchildren. Variables assessed included school absences and performance, oral health status, parental education, health insurance coverage, race, and gender.
Results. Children with poor oral health status were nearly 3 times more likely (odds ratio = 3.89; 95% confidence interval = 1.96, 7.75) than were their counterparts to miss school as a result of dental pain. Absences caused by pain were associated with poorer school performance (P < .05), but absences for routine care were not. Mediation analyses revealed that oral health status was associated with performance independent of absence for pain.
Conclusions. Children with poorer oral health status were more likely to experience dental pain, miss school, and perform poorly in school. These findings suggest that improving children's oral health status may be a vehicle to enhancing their educational experience.
Oral health has been well established as a fundamental component of general health. As a policy talking point in the early 1980s, former US Surgeon General C. Everett Koop recognized the relationship between oral health and overall health and coined the often-repeated phrase “You're not healthy without good oral health.” Later, US Surgeon General David Satcher reinforced this concept by focusing national attention on oral health in Oral Health in America: A Report of the Surgeon General.1 This report explicated the role of oral health in overall health, emphasizing that oral health is a mirror for general health and that the oral cavity is a portal for infectious organisms. Recently established associations have been found between oral infections and diabetes,2 heart disease,3 stroke,4 and low-birth weight babies.5
Several chronic diseases are known to affect children, requiring significant adjustments in life management and leading to decreased quality of life. According to National Institutes of Health estimates, 20% to 30% of children and adolescents in the United States have chronic health conditions.6 Among the most prevalent diseases of childhood are dental caries, asthma, diabetes, and obesity, with dental caries being the most common, occurring 5 to 8 times more frequently than asthma, the second-most common condition.1 Data from the third National Health and Nutrition Examination Survey (1999–2002) indicated that 41% of children aged 2 to 11 years had dental caries in their primary teeth and 42% of those aged 6 to 19 years had caries in their permanent teeth.7
Chronic illness can interfere with a child's ability to succeed in school. Evidence shows that increases in missed school time caused by chronic illnesses can lead to declines in school performance.8,9 The National Health Interview Survey (NHIS) documented that 1.57 million school days were lost in 1980 as a result of dental problems.10 Using 1984 NHIS data, Waldman reported that children and adolescents aged younger than 18 years had approximately 5 million restricted activity days, more than 1.6 million days in bed, and more than 1.7 million missed school days as a result of acute dental conditions.11 A number commonly cited in the literature is that more than 51 million school hours are lost annually because of illnesses related to dental problems,1,12–20 a statistic emanating from an analysis of the 1989 NHIS data conducted by Gift et al.13
The 1989 NHIS was unique because it included a supplement focusing on oral health among those aged older than 2 years, along with questions about missed school and work as well as reduced normal activity because of dental visits or problems. Gift et al. analyzed this data set and found that nearly 3.9 million restricted activity days were reported for children and adolescents aged 18 years or younger.13 A major limitation of their study was that they did not address whether these dental visits were routine or emergency visits, and thus it is not possible to disentangle the nature of the visit that resulted in school absences or restricted activity.21
To our knowledge, there are no published US data examining the relationship between oral health and school achievement or performance. Several international studies have examined this relationship with the aim of using poor school performance as a proxy measure for dental treatment need.22–26 Generally, these studies have revealed positive correlations between oral health status and school performance, but the results are limited in their generalizability to the United States because of differences in number of school days per year, length of school days, and use of school-based dental clinics.
Research has shown that children in North Carolina follow the overall trend in the United States with respect to oral health status, with a high burden of dental disease and many children reporting related dental pain.27–29 Blumenshine et al. examined health factors affecting school performance in North Carolina children in 2006 and 2007, as well as the impact of poor oral health status on school performance, while controlling for other health and sociodemographic factors.30 Children with both poor oral and general health were 2.3 times more likely (95% confidence interval [CI] = 1.07, 5.67) to perform poorly in school than were those with both good oral and general health.
Previous research adds to the knowledge base regarding the relationship between poor general health and school performance but does not implicate oral health as a stand-alone factor in poor school performance. We concluded that more research is needed to assess school absences related to oral health visits and specifically the types of oral health concerns that contribute to absences. We also must determine whether oral health status affects a child's learning capabilities when he or she is present in school. With this backdrop, the overarching goal of our investigation was to examine the impact of poor oral health status on school performance in a more detailed manner. We specifically sought to document school absences related to routine dental care, dental pain, and infection, and to assess the extent to which children's oral health status is related to their school attendance and performance.
METHODS
We used 2008 data from the North Carolina Child Health Assessment and Monitoring Program (CHAMP) for our analyses. CHAMP is a follow-up to the North Carolina Behavioral Risk Factor Surveillance Survey (BRFSS), a federally mandated annual survey of adults aged 18 years or older conducted by all states and supported by the Centers for Disease Control and Prevention. The BRFSS does not have a child health component; however, as a follow-up to the BRFSS in North Carolina, the State Center for Health Statistics developed CHAMP in 2005 to annually collect data on a wide range of child health issues, including 26 sections ranging from general health to birth characteristics. The oral health section includes 5 questions, and the school performance section includes 3 questions.
CHAMP collects data from adults in households identified via random sampling to participate in the BRFSS. Adults are asked whether they have children aged younger than 18 years residing in their household. If so, they are asked to participate in CHAMP. If they agree and there is more than 1 child in the home, 1 child is selected for the survey through computer randomization. The respondent most familiar with the child's health is called on the telephone to complete the 15- to 20-minute interview.
Variable Measurement
CHAMP assessed parents’ perception of their children's oral health status in relation to their school attendance and performance. School performance was measured as follows: “How would you describe [your child's] grades in school over the past 12 months? Would you say they were mostly As, Bs, Cs, Ds, or Fs?” For the purposes of this investigation, we defined poor school performance as mostly Cs, Ds, or Fs. By adding 2 new questions in the oral health section of CHAMP, we were able to directly assess school absences related to routine dental care and dental pain or infection. These questions asked “During the past 12 months, about how many days did your child miss school because of routine dental care (e.g., check-ups, fillings,) or orthodontic visits?” and “During the past 12 months, about how many days did your child miss school because of a toothache, dental infection, or related ‘dental fever’? Include time spent at home not feeling well and time receiving dental care for the problem.”
Our major explanatory variable was the child's oral health status as reported by the adult household respondent. Oral health status was measured with the question “How would you rate the condition of [your child's] teeth? Would you say their condition is excellent, very good, good, fair, or poor?”
We also included 2 general health variables that focused on children's overall health status (excellent, very good, good, fair, or poor) and whether they had special health care needs (yes or no). In addition, we controlled for the following variables: child's gender, race (White, minority), ethnicity (Hispanic, non-Hispanic), and grade in school (K–5, 6–8, 9–12); highest level of education achieved in the household (less than high school, high school, some college, college or more); and health insurance coverage (public insurance, private insurance, military or other insurance, or uninsured).
Statistical Analysis
After examining descriptive statistics and bivariate associations between independent variables and school performance, we used multivariable logistic regression models to test the relationships between oral health status, school performance, and school attendance while accounting for control variables. Because we considered the potential for dental and general health variables to be highly correlated with school absence variables, we estimated logistic regression models after excluding each of these variables to further examine their relationship with poor school performance. We conducted mediation analyses to test whether school absence for dental pain was a mediator between oral health status and poor school performance.
We used the appropriate analytic weights to account for issues related to disproportionate sampling, including people living in households with different numbers of residential telephone numbers and different numbers of children in the home. Survey weights also adjusted for unequal nonresponse rates among different demographic groups. Stata version 10 (StataCorp LP, College Station, TX) was used in conducting all of the analyses.
RESULTS
Of the North Carolina BRFSS respondents with a child in the household, 3865 (64.7%) agreed to participate in the CHAMP survey, and 2987 (77.3%) completed the interview. Eliminating children not enrolled in public or private schools reduced the sample size to 2183. Eliminating respondents with missing or “don't know/not sure” responses further reduced the sample to 2120, giving us an analytic response rate of 35.5%. These 2120 children represented the final sample for the school attendance analyses. Because one of our goals was to examine school performance and the relevant CHAMP question relied on a child's letter grades, we limited the school performance analyses to children in schools using a letter grading system. The final sample for these performance analyses therefore included 1782 children, weighted to reflect the state's demographic characteristics.
Most of the children were boys (51.7%), between the ages of 5 and 11 years (51.6%), White (63.1%), and covered by private health insurance (60.3%). A substantial majority of parents reported their children to be in both excellent or very good oral health and excellent or very good general health (Table 1).
TABLE 1.
Characteristics of the Study Population: North Carolina Child Health Assessment and Monitoring Program, 2008
| Sample (n = 2120), No. (%) |
|
| Child gender | |
| Boy | 1097 (51.7) |
| Girl | 1023 (48.3) |
| Child age, y | |
| <5 | 50 (2.9) |
| 5–11 | 998 (51.6) |
| 12–14 | 499 (22.1) |
| >14 | 573 (23.4) |
| Grade in school | |
| K–5 | 962 (50.5) |
| 6–8 | 474 (21.7) |
| 9–12 | 684 (27.8) |
| Race | |
| White | 1466 (63.1) |
| Black | 334 (23.0) |
| Other | 320 (13.9) |
| Ethnicity | |
| Hispanic | 191 (10.1) |
| Non-Hispanic | 1929 (89.9) |
| Parental educational level | |
| < high school | 129 (6.6) |
| High school | 364 (16.0) |
| College/some college | 1627 (77.4) |
| Health insurance coverage | |
| Public/Medicaid/Indian Health Service | 512 (24.2) |
| Private/Health Choice | 1291 (60.9) |
| Military/other | 189 (8.9) |
| Uninsured | 128 (6.0) |
| Oral health status | |
| Excellent/very good | 1577 (73.2) |
| Good/fair/poor | 543 (26.8) |
| General health status | |
| Excellent/very good | 1744 (82.1) |
| Good/fair/poor | 376 (17.9) |
| Child has special health care needs | |
| Yes | 241 (11.2) |
| No | 1879 (88.8) |
| School performance | |
| Mostly As and Bs | 1494 (70.5) |
| Mostly Cs, Ds, and Fs | 288 (13.6) |
| No letter grading | 338 (15.9) |
| School absences caused by routine dental care, d | |
| 0 | 1656 (78.4) |
| 1 | 273 (13.0) |
| 2 | 127 (5.9) |
| ≥3 | 64 (2.7) |
| School absences caused by dental pain, d | |
| 0 | 2031 (96.1) |
| 1 | 50 (2.2) |
| 2 | 18 (0.9) |
| ≥3 | 21 (0.8) |
The results of the bivariate analyses examining factors associated with poor school performance revealed that gender (male), race (non-White), age (older), parental educational level (less than high school or high school), health insurance coverage (public, military or other, uninsured), special health care needs, general health status (good, fair, poor), and oral health status (good, fair, or poor) were related to poor school performance (P < .05). Bivariate analyses of school absences for routine dental care and poor school performance revealed no significant relationship; however, school absence secondary to dental pain or infection was related to poor school performance (P = .001).
Of the 2120 children in our sample, 1656 (78.1%) had not missed any school days for routine dental care during the past 12 months, whereas 464 (21.9%) had missed 1 or more days (273 had missed 1 day, 127 had missed 2 days, and 64 had missed 3 days or more). In comparison, 2031 children (96.1%) had not missed any school days as a result of dental pain or infection, and 89 children had missed 1 or more days (50 had missed 1 day, 18 had missed 2 days, and 21 had missed 3 or more days).
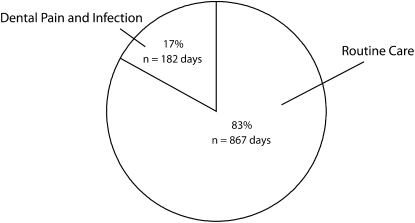
A total of 1049 school days were missed by the 2120 children for any reason related to dental care, an average of 0.49 days per child. Of these missed days, 182 (17.3%) were the result of dental pain or infection (Figure 1). Comparatively, 9166 school days were missed as a result of general illness or injury, an average of 4.32 days per child. The CHAMP survey also included a question targeting children diagnosed with asthma (n = 218), with parents asked to report the number of days of school missed as a result of their child's asthma. A total of 477 days were missed because of asthma, an average of 0.23 days per child for the overall sample.
FIGURE 1.
School days missed by study children for reasons related to dental care: North Carolina Child Health Assessment and Monitoring Program, 2008.
The results of multivariate analyses examining school absences resulting from dental pain or infection and routine dental care are shown in Table 2. Having public assistance or no health insurance was related to absences caused by dental pain or infection. Uninsured children were more likely than were those with private insurance to miss school for dental pain, but they were less likely to miss school for routine dental care. Children with good, fair, or poor oral health were nearly 3 times more likely than were children with very good or excellent oral health to miss school as a result of dental pain. Black children were less likely than were White children to miss school for routine dental care.
TABLE 2.
Results of Logistic Regression Analysis of Likelihood of School Absences as a Result of Dental Pain or Infection and Routine Dental Care: North Carolina Child Health Assessment and Monitoring Program, 2008
| Dental Pain or Infection, AOR (95% CI) |
Routine Dental Care, AOR (95% CI) |
|
| Child gender (boy vs girl) | 1.46 (0.83, 2.56) | 0.87 (0.67, 1.13) |
| Grade in school | ||
| 6–8 vs K–5 | 0.72 (0.33, 1.60) | 0.85 (0.60, 1.20) |
| 9–12 vs K–5 | 1.15 (0.59, 2.22) | 1.16 (0.86, 1.58) |
| Race | ||
| Black vs White | 0.59 (0.30, 1.16) | 0.53 (0.35, 0.81) |
| Other vs White | 1.40 (0.59, 3.31) | 1.37 (0.89, 2.12) |
| Ethnicity (Hispanic vs non-Hispanic) | 1.90 (0.68, 5.36) | 0.94 (0.54, 1.65) |
| Parental educational level | ||
| < high school vs college/some college | 0.98 (0.32, 2.96) | 1.14 (0.59, 2.19) |
| High school vs college/some college | 0.74 (0.36, 1.51) | 1.15 (0.79, 1.69) |
| Health insurance coverage | ||
| Public/Medicaid/Health Choice/Carolina ACCESS/IHS vs private | 2.34 (1.15, 4.78) | 1.69 (1.19, 2.41) |
| Military/other vs private | 2.20 (0.88, 5.51) | 1.18 (0.74, 1.89) |
| Uninsured vs private | 2.95 (1.21, 7.23) | 0.97 (0.55, 1.71) |
| Special health care needs (yes vs no) | 0.57 (0.26, 1.24) | 1.83 (1.24, 2.71) |
| Oral health status (good/fair/poor vs excellent/very good) | 3.89 (1.96, 7.75) | 1.35 (0.99, 1.83) |
| General health status (good/fair/poor vs excellent/very good) | 1.39 (0.67, 2.88) | 0.79 (0.55, 1.13) |
Note. AOR = adjusted odds ratio; CI = confidence interval; IHS = Indian Health Service. Sample size was n = 2120.
The variables associated with poor school performance in the multivariate analyses (Table 3) included gender (male), race (Black), grade in school (6–12), parental educational level (high school), health insurance (public), and special health care needs. When both health status and school absence variables were included in the model, children with good, fair, or poor oral health were more likely to perform poorly in school (odds ratio [OR] = 1.62; 95% CI = 1.10, 2.38). This relationship held even when school absence variables were excluded from the model (OR = 1.70; 95% CI = 1.16, 2.49). Excluding health status variables from the analyses revealed that children who missed school as a result of dental pain were more likely to perform poorly in school (OR = 1.94; 95% CI = 1.04, 3.63). Mediation analysis results revealed that school absence related to dental pain was not a mediator between oral health status and poor school performance; rather, we found an association between oral health status and school performance independent of absence related to dental pain.
TABLE 3.
Results of Logistic Regression Analysis of Likelihood of Poor School Performance: North Carolina Child Health Assessment and Monitoring Program, 2008
| Main Model, AOR (95% CI) |
Model Excluding Health Status Variables, AOR (95% CI) |
Model Excluding Absence Variables, AOR (95% CI) |
|
| Child gender (boy vs girl) | 1.88 (1.29, 2.72) | 1.96 (1.35, 2.85) | 1.88 (1.30, 2.71) |
| Race | |||
| Black vs White | 1.82 (1.16, 2.86) | 1.89 (1.21, 2.95) | 1.84 (1.17, 2.89) |
| Other vs White | 0.84 (0.44, 1.60) | 0.87 (0.46, 1.64) | 0.83 (0.44, 1.58) |
| Grade in school | |||
| 6–8 vs K–5 | 1.72 (1.05, 2.82) | 1.71 (1.05, 2.78) | 1.71 (1.05, 2.79) |
| 9–12 vs K–5 | 2.74 (1.78, 4.22) | 2.58 (1.70, 3.92) | 2.72 (1.76, 4.19) |
| Parental educational level | |||
| < high school vs ≥ college | 1.51 (0.62, 3.67) | 1.66 (0.68, 4.06) | 1.57 (0.66, 3.75) |
| High school vs ≥ college | 2.25 (1.44, 3.51) | 2.41 (1.54, 3.76) | 2.22 (1.42, 3.47) |
| Ethnicity (Hispanic vs non-Hispanic) | 0.98 (0.43, 2.23) | 0.99 (0.44, 2.29) | 1.00 (0.44, 2.29) |
| Health insurance coverage | |||
| Public/Medicaid/Health Choice/Carolina ACCESS/IHS vs private | 1.99 (1.20, 3.29) | 2.03 (1.23, 3.35) | 1.98 (1.20, 3.26) |
| Military/other vs private | 1.79 (1.01, 3.16) | 1.73 (0.97, 3.06) | 1.80 (1.02, 3.18) |
| Uninsured vs private | 1.52 (0.77, 3.01) | 1.63 (0.85, 3.12) | 1.56 (0.79, 3.10) |
| Special health care needs (yes vs no) | 3.62 (2.27, 5.78) | 3.68 (2.37, 5.72) | 3.55 (2.22, 5.67) |
| Oral health status (good/fair/poor vs excellent/very good) | 1.62 (1.10, 2.38) | … | 1.70 (1.16, 2.49) |
| General health status (good/fair/poor vs excellent/very good) | 0.91 (0.58, 1.43) | … | 0.93 (0.59, 1.46) |
| Days of school absences for routine dental care | |||
| 1 vs 0 | 0.76 (0.45, 1.27) | 0.73 (0.44, 1.23) | … |
| 2 vs 0 | 1.05 (0.52, 2.11) | 1.06 (0.53, 2.10) | … |
| 3 vs 0 | 0.95 (0.42, 2.16) | 1.05 (0.46. 2.41) | … |
| School absence caused by dental pain (yes vs no) | 1.68 (0.88, 3.20) | 1.94 (1.04, 3.63) | … |
Note. AOR = adjusted odds ratio; CI = confidence interval; IHS = Indian Health Service. Sample size was n = 1782. Ellipses indicate information that was not included.
DISCUSSION
Policymakers and legislators frequently use the association between poor oral health and school attendance as an advocacy talking point; however, the commonly used US school attendance data emanate from the 1980s and are outdated.10–20 Existing data also fail to differentiate between routine visits and those associated with dental pain or infection.13,21 We used a contemporary data set including detailed questions on oral health and school performance, offering a snapshot of school absences for reasons related to dental care while differentiating between absences for routine dental visits and absences as a result of pain or infection. The 2 new questions we added to the oral health section of CHAMP assessed the number and cause of school days missed because of routine dental visits and dental problems, providing novel data to clarify the association between school absences related to dental care and school performance.
Our first 2 aims were to document school absences related to routine dental care and those related to dental pain or infection. In the 1989 NHIS data set that produced the commonly cited 51 million hours13 of school missed annually for reasons related to dental care, survey participants were asked to recall the amount of time missed in a specified 2-week period. As noted by Gift et al., this methodology probably resulted in underestimations13; in addition, the 1989 NHIS data set was a national one with 109 603 observations, whereas our data set was a statewide one with 2120 observations.
State requirements in North Carolina mandate a minimum of 180 school days and 1000 school hours per year (5.6 hours per day). According to the most recent data, the population of school-aged (K–12) children in North Carolina is 1 530 773. Using the minimum school time figures and extrapolating our sample of children to represent the entire population of children in the state, we found that 3 430 602 school hours were missed as a result of routine dental care and that 717 895 hours were missed as a result of dental pain or infection. Keeping in mind that most children attend school for longer than 5.6 hours a day, our extrapolations are probably an underestimation. Nevertheless, according to these extrapolations, North Carolina schoolchildren missed more than 4 million school hours for reasons related to dental care.
Although a relatively small percentage (approximately 4%) of our sample missed school as a result of dental pain or infection, it is important to consider the gravity of the effects on school attendance along with school performance. School absences caused by dental pain or infection were significantly related to parents’ reports of poor school performance, whereas school absences for routine dental care were not. These findings underscore the likelihood that school absence is not a stand-alone factor in considerations of school performance, providing further evidence that children experiencing pain or infection may have a diminished educational experience because their discomfort may inhibit their ability to perform well while at school.
Our third aim was to assess the extent to which children's oral health status is related to school attendance. The literature is outdated relative to school time missed for dental reasons.10–20 After controlling for other variables, we found that the poorer a child's oral health status, the higher his or her likelihood of missing school as a result of dental pain or infection. In fact, a child with good, fair, or poor oral health was nearly 3 times more likely (OR = 3.89; 95% CI = 1.96, 7.75) than was a child with very good or excellent oral health to be absent as a result of dental pain or infection. This finding supports the hypothesis that children with poor oral health are more likely to experience pain or infection that may have a negative impact on school attendance.
Our final aim was to examine the extent to which children's oral health status is related to their school performance. Although evidence exists that chronic illness can interfere with children's success in school8,9 and that dental caries may put them at a disadvantage for their overall development,10,11 a relationship between oral health status and school performance has not been previously reported. Poor oral health was related to a higher likelihood of poor school performance in our multivariate analyses.
We estimated logistic regression models excluding health status and school absence variables to account for the potential for these variables to be highly correlated. Even when the school absence variables were excluded, there was still a relationship between poor oral health and the likelihood of poor school performance. Furthermore, without the health variables in the model, we found a relationship between poor school performance and absence related to dental pain or infection. These results show a negative impact of poor oral health status on a child's school performance with or without school absence variables in the model. A child missing school as a result of dental pain or infection also had a negative effect on school performance.
Our mediation analyses revealed that school absence resulting from dental pain was not a mediating variable in the relationship between good, fair, or poor oral health status and poor school performance. Although missing school because of dental pain may have an impact on performance, there appears to be something fundamental in the relationship between oral health status and school performance independent of attendance. This finding suggests that a child with poor oral health is at an increased risk of having a diminished educational experience. We hypothesize that a child with poor oral health is more likely to have pain or infection that not only leads to school absences but also detracts from his or her ability to perform well whether present in school or studying at home.
Strengths and Limitations
No cause-and-effect relationships can be inferred from our cross-sectional data. Also, because CHAMP is a telephone survey, the sampling frame is restricted to households that have a telephone. Research has shown some differences in households with and without a telephone. For example, individuals with low incomes and those living in rural areas are less likely than are their counterparts to live in a household with a telephone.31 However, we used poststratification adjustments for age, race, gender, and other variables in our multivariate analyses that helped minimize the impact of these differences.
Another potential limitation is that the CHAMP school performance and dental health variables are subjective measures; however, published data support the strength of such subjective reports. For example, Talekar et al. analyzed data from the third National Health and Nutrition Examination Survey and found a good correlation between presence of clinical disease and parent-defined need for dental treatment as well as perceptions of poor oral health.32 Similarly, Jokovic et al. studied the level of agreement between mothers and children regarding the child's oral health–related quality of life and found substantial agreement between parent and child.33 One might also argue that parents’ perceptions of academic performance are subjective, but several studies have examined the validity of parental reports of language and literacy development in preschool-aged children.34–36 In the aggregate, these investigations have revealed strong correlations between parents’ perceptions and their child's language development and academic achievement.
The strengths of this study include the wealth of child health information available in CHAMP and the detailed questions regarding oral health and school performance. The new questions we added to the oral health section directly assessed the number and cause of missed school days secondary to routine dental visits and dental problems, helping to clarify the relationship between school absence and performance, a concept not previously examined in the United States to our knowledge.
Conclusions
Our study provides updated information on school absences for dental care. We found that children missed an average of 0.5 days of school for reasons related to such care, with 17% of these absences associated with pain or infection. For comparison's sake, although the numbers are not directly comparable because of the small sample size (n = 218), children missed an average of approximately 0.2 days of school as a result of asthma.
To further evaluate school absences related to dental care, one needs to consider not only the average number of days missed but the impact of absences. Although only 17% of the absenteeism in this study was associated with dental pain or infection, such absences increased the likelihood of poor school performance, whereas absences for routine dental care did not. Finally, it is also important to consider the mechanism by which children's oral health status affects their school performance. Children in good, fair, or poor oral health were more likely to perform poorly in school, suggesting that dental disease may adversely affect children's performance independent of school absences. Altogether, our findings suggest that improving children's oral health status may be a vehicle to enhancing their educational experience.
Acknowledgments
We acknowledge the North Carolina Child Health Assessment and Monitoring Program (CHAMP) and the North Carolina Center for Health Statistics for their leadership on behalf of the CHAMP initiative.
Human Participant Protection
The internal review board of the North Carolina Center for Health Statistics approved this study. The North Carolina Child Health Assessment and Monitoring Program data have no identifying information, are anonymous, and are available in a public use data set.
References
- 1.Oral Health in America: A Report of the Surgeon General. Rockville, MD: National Institute of Dental and Craniofacial Research; 2000 [Google Scholar]
- 2.Mealey BL, Oates TW. Diabetes mellitus and periodontal diseases. J Periodontol. 2006;77(8):1289–1303 [DOI] [PubMed] [Google Scholar]
- 3.Bahekar AA, Singh S, Saha S, et al. The prevalence and incidence of coronary heart disease is significantly increased in periodontitis: a meta-analysis. Am Heart J. 2007;154(5):830–837 [DOI] [PubMed] [Google Scholar]
- 4.Haraszthy VI, Zambon JJ, Trevisan M, et al. Identification of periodontal pathogens in atheromatous plaques. J Periodontol. 2000;71(10):1554–1560 [DOI] [PubMed] [Google Scholar]
- 5.Boggess KA, Beck JD, Murtha AP, et al. Maternal periodontal disease in early pregnancy and risk for a small for-gestational-age infant. Am J Obstet Gynecol. 2006;194(5):1316–1322 [DOI] [PubMed] [Google Scholar]
- 6.National Institutes of Health Chronic illness self-management in children. Available at: http://grants.nih.gov/grants/guide/pa-files/PA-03-159.html. Accessed December 12, 2010
- 7.Beltran-Aguilar ED, Barker LK, Canto MT, et al. Surveillance for dental caries, dental sealants, tooth retention, edentulism, and enamel fluorosis. MMWR Surveill Summ. 2005;54(3):1–44 [PubMed] [Google Scholar]
- 8.Wolfe BL. The influence of health on school outcomes: a multivariate approach. Med Care. 1985;23(10):1127–1138 [DOI] [PubMed] [Google Scholar]
- 9.Fowler MG, Johnson MP, Atkinson SS. School achievement and absence in children with chronic health conditions. J Pediatr. 1985;106(4):683–687 [DOI] [PubMed] [Google Scholar]
- 10.Reisine ST. Dental health and public policy: the social impact of dental disease. Am J Public Health. 1985;75(1):27–30 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Waldman HB. Another perspective on children's dental needs and demand for services during the 1980s. ASDC J Dent Child. 1987;54(5):344–348 [PubMed] [Google Scholar]
- 12.Amschler DH. A hidden epidemic: dental disparities among children. J Sch Health. 2003;73(1):38–40 [DOI] [PubMed] [Google Scholar]
- 13.Gift HC, Reisine ST, Larach DC. The social impact of dental problems and visits. Am J Public Health. 1992;82(12):1663–1668 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Peterson J, Niessen L, Nana Lopez GM. Texas public school nurses’ assessment of children's oral health status. J Sch Health. 1999;69(2):69–72 [DOI] [PubMed] [Google Scholar]
- 15.Schwarz C, Lui E. The link between school performance and health insurance: current research. Available at: http://www.consumersunion.org/pdf/hiresearch.pdf. Accessed December 12, 2010
- 16.US Dept of Health and Human Services National call to action to promote oral health. Available at: http://www.surgeongeneral.gov/topics/oralhealth/nationalcalltoaction.html. Accessed December 12, 2010
- 17.Oral health and learning: when children's oral health suffers, so does their ability to learn. Available at: http://www.mchoralhealth.org/PDFs/learningfactsheet.pdf. Accessed December 12, 2010 [PubMed]
- 18.Community Partnerships for Healthy Children The statistical facts of dental health. CPHC Spotlight. 2000;2(5):6 [Google Scholar]
- 19.Gift HC. Oral health outcomes research—challenges and opportunities. : Slade GD, Measuring Oral Health and Quality of Life. Chapel Hill, NC: Dept of Dental Ecology, University of North Carolina; 1997:25–46 [Google Scholar]
- 20.Ries PW. Current estimates from the National Health Interview Survey: United States, 1984. Vital Health Stat 10. 1986;No. 156 [PubMed] [Google Scholar]
- 21.National Center for Health Statistics Current estimates from the National Health Interview Survey: United States, 1989. Vital Health Stat 10. 1992;No. 183 [PubMed] [Google Scholar]
- 22.Gherunpong S, Tsakos G, Sheiham A. The prevalence and severity of oral impacts on daily performances in Thai primary school children. Health Qual Life Outcomes. 2004;2:57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Muirhead VE, Locker D. School performance indicators as proxy measures of school dental treatment needs: a feasibility study. J Public Health Dent. 2006;66(4):269–272 [DOI] [PubMed] [Google Scholar]
- 24.Jiang H, Petersen PE, Peng B, Tai B, Bian Z. Self-assessed dental health, oral health practices, and general health behaviors in Chinese urban adolescents. Acta Odontol Scand. 2005;63(6):343–352 [DOI] [PubMed] [Google Scholar]
- 25.Crowley E, O'Brien G, Marcenes W. School league tables: a new population based predictor of dental restorative treatment need. Community Dent Health. 2003;20(2):78–82 [PubMed] [Google Scholar]
- 26.Tsakos G, Gherunpong S, Sheiham A. Can oral health-related quality of life measures substitute for normative needs assessments in 11 to 12-year-old children? J Public Health Dent. 2006;66(4):263–268 [DOI] [PubMed] [Google Scholar]
- 27.North Carolina Institute of Medicine Task Force on Dental Care Access Report to the North Carolina General Assembly and the Secretary of the North Carolina Department of Health and Human Services. Available at: http://www.nciom.org/wp-content/uploads/NCIOM/docs/dentalrpt.pdf. Accessed December 12, 2010
- 28.NC Dept of Health and Human Services Division of Public Health. 2008–2009 annual report: North Carolina Oral Health Section. Available at: http://www.ncdhhs.gov/dph/oralhealth/library/includes/08-09%20OHS%20Annual%20Report.pdf. Accessed December 12, 2010
- 29.Rozier GR, King RS. Defining the need for dental care in North Carolina: contributions of public health surveillance of dental diseases and conditions. N C Med J. 2005;66(6):438–444 [PubMed] [Google Scholar]
- 30.Blumenshine SL, Vann WF, Jr, Gizlice Z, Lee JY. Children's school performance: impact of general and oral health. J Public Health Dent. 2008;68(2):82–87 [DOI] [PubMed] [Google Scholar]
- 31.Miles DR, Herrick H, Ford CA. The North Carolina Child Health Assessment and Monitoring Program: survey methodology and data collection. Available at: http://www.schs.state.nc.us/SCHS/pdf/Primer18_WEB_051210.pdf. Accessed December 12, 2010
- 32.Talekar BS, Rozier G, Slade GD, Ennett ST. Parental perceptions of their preschool-aged children's oral health. J Am Dent Assoc. 2005;136(3):364–372 [DOI] [PubMed] [Google Scholar]
- 33.Jokovic A, Locker D, Stephens M, Kenny D, Tompson B, Guyatt G. Measuring parental perceptions of child oral health-related quality of life. J Public Health Dent. 2003;63(2):67–72 [DOI] [PubMed] [Google Scholar]
- 34.Feldman HM, Dale PS, Campbell TF, et al. Concurrent and predictive validity of parent reports of child language at ages 2 and 3 years. Child Dev. 2005;76(4):856–868 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Dickinson DK, DeTemple J. Putting parents in the picture: maternal reports of preschoolers’ literacy as a predictor of early reading. Early Child Res Q. 1998;13(2):241–261 [Google Scholar]
- 36.Gilger JW. Using self-report and parental-report survey data to assess past and present academic achievement of adults and children. J Appl Dev Psychol. 1992;13(2):235–256 [Google Scholar]