Abstract
Objectives. We developed and assessed AMIGAS (Amigas, Mujeres Latinas, Inform andonos, Gui andonos, y Apoy andonos contra el SIDA [friends, Latina women, informing each other, guiding each other, and supporting each other against AIDS]), a culturally congruent HIV prevention intervention for Latina women adapted from SiSTA (Sistas Informing Sistas about Topics on AIDS), an intervention for African American women.
Methods. We recruited 252 Latina women aged 18 to 35 years in Miami, Florida, in 2008 to 2009 and randomized them to the 4-session AMIGAS intervention or a 1-session health intervention. Participants completed audio computer-assisted self-interviews at baseline and follow-up.
Results. Over the 6-month follow-up, AMIGAS participants reported more consistent condom use during the past 90 (adjusted odds ratio [AOR] = 4.81; P < .001) and 30 (AOR = 3.14; P < .001) days and at last sexual encounter (AOR = 2.76; P < .001), and a higher mean percentage condom use during the past 90 (relative change = 55.7%; P < .001) and 30 (relative change = 43.8%; P < .001) days than did comparison participants. AMIGAS participants reported fewer traditional views of gender roles (P = .008), greater self-efficacy for negotiating safer sex (P < .001), greater feelings of power in relationships (P = .02), greater self-efficacy for using condoms (P < .001), and greater HIV knowledge (P = .009) and perceived fewer barriers to using condoms (P < .001).
Conclusions. Our results support the efficacy of this linguistically and culturally adapted HIV intervention among ethnically diverse, predominantly foreign-born Latina women.
Latinos are the largest and fastest-growing ethnic minority in the United States, currently composing 15% of the US population.1 Between 2000 and 2006, Latinos accounted for almost half of all US population growth, with nearly 40% of this increase attributed to foreign-born Latinos.2 Latinos are also disproportionately affected by the HIV epidemic.3 Between 2003 and 2006, more than half of Latinos diagnosed with HIV were foreign born, and the majority lived in the southern United States.4 The Miami, Florida, metropolitan area has the highest rate of new AIDS diagnoses in the United States (42.8/100 000 population)5 as well as a highly diverse Latino population.6 Thus, HIV prevention efforts for Latinos in Miami must address this diversity.
HIV diagnoses among Latina women (15/100 000) are 5 times the rate for White women, and annual HIV diagnoses have increased among foreign-born Latina women.3 In addition to language barriers and lack of access to regular health care, adherence to traditional gender roles can increase foreign-born Latina women's vulnerability to HIV.7–9 Widespread cultural values such as marianismo (Marianism), which stresses chastity before marriage and faithfulness, sexual passivity, and subservience after marriage, and simpatía, which stresses the importance of being agreeable and nonconfrontational in social relationships, can make negotiating and practicing safe sex challenging for Latina women.10,11
Although Latina women are disproportionately affected by HIV/AIDS, they remain an understudied and underserved population. Recent meta-analyses reveal that few HIV sexual risk reduction interventions have demonstrated efficacy in decreasing HIV-associated behaviors among adult Latina women,12 and available interventions do not address the cultural diversity of Latina women.13 We developed AMIGAS (Amigas, Mujeres Latinas, Informándonos, Guiándonos, y Apoyándonos contra el SIDA [friends, Latina women, informing each other, guiding each other, and supporting each other against AIDS]), a culturally appropriate adaptation of SiSTA (Sistas Informing Sistas about Topics on AIDS), a widely disseminated HIV risk-reduction intervention initially developed for African American women,14 and assessed its efficacy in a randomized, controlled trial. AMIGAS was delivered by Latina health educators to a diverse, predominantly immigrant population of Latina women in the Miami metropolitan area.
METHODS
The Centers for Disease Control and Prevention (CDC) funded the study from August 2007 to August 2010. Latina principal investigators and coinvestigators led the study team, and the majority of the health department staff and project partners at Emory University and the CDC were Latino or were fluent in Spanish. The study team members were from Cuba, Central American countries, the Dominican Republic, and Puerto Rico. Moreover, although most trials that have evaluated the efficacy of HIV interventions have been initiated by principal investigators at universities or other research institutions, the principal investigators and most coinvestigators for this study were from the Office of HIV/AIDS in the Miami–Dade County Health Department.
Recruitment and Study Design
We used community-based participatory research approaches to engage members of the ethnically diverse Latina community at all stages of the research. They participated in conceptualizing the study aims, adapting the HIV intervention materials, and developing assessment measures and recruitment strategies. Previous research described challenges in recruiting Latina women for health programs, and the observed disconnect between researchers and community members may exacerbate this challenge.15 Factors that have been reported as contributing to poor participation include violation of cultural norms such as personalismo (personalism), familismo (familism), and respeto (respect).16,17 Trusting relationships between researchers and communities, cultural adaptation of messages, and removal of language barriers can enhance Latina women's participation in health promotion trials.18 To address these issues, the AMIGAS study employed Latina outreach workers who had deep roots in the Latino community and extensive experience recruiting Latina women. The outreach workers were involved in identifying and selecting recruitment sites, conceptualizing recruitment strategies, developing culturally appropriate and appealing recruitment materials (written in Spanish and showing Latina women of varying hues), and disseminating recruitment materials.
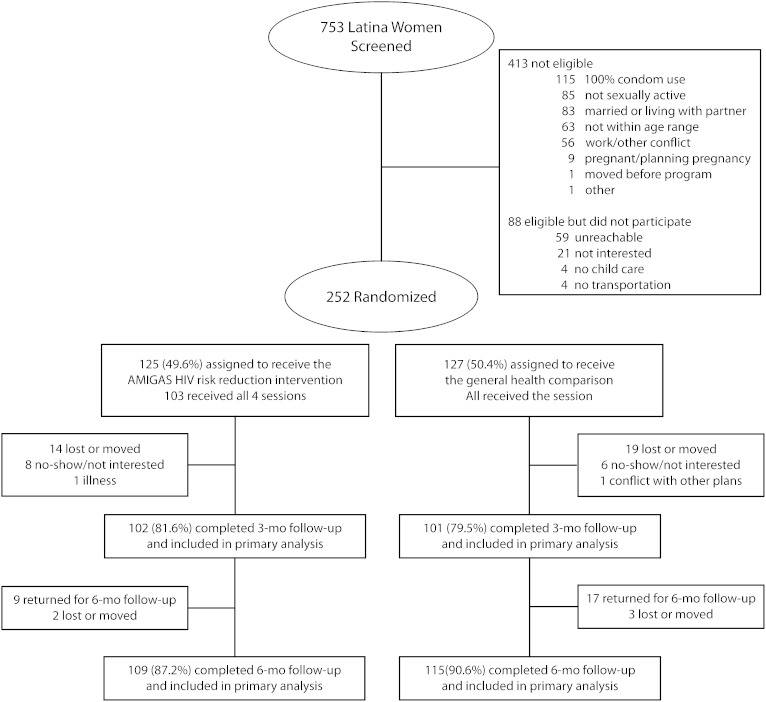
From October 2008 through October 2009, outreach workers screened a convenience sample of 753 self-identified Latina women from the Miami metropolitan area. Of these, 340 (45.2%) met the eligibility criteria of being a Spanish-speaking Latina woman aged 18 to 35 years; reporting unprotected vaginal intercourse with a male sexual partner during the past 90 days; being unmarried and not living with a male sexual partner; not being pregnant or planning pregnancy; and providing written informed consent. Of those who were ineligible, 48.4% were not sexually active or reported using condoms 100% of the time, 20% were married, and 15% were outside the specified age range. Of the 340 eligible women, 252 (74.1%) consented to participate, and most of these (n = 195, or 77%), were recruited by friends. The high participation rate reflected the outreach workers’ effectiveness in accessing and mobilizing the Latina women's social networks. All 252 women completed baseline assessments and were randomized to the study's 2 conditions (Figure 1). Participants received $50 gift cards for completing study assessments and $30 gift cards for attending each intervention session to compensate them for travel and out-of-pocket expenses.
FIGURE 1.
Participant allocation table for AMIGAS, a culturally congruent HIV prevention intervention for Latina Women: Miami, FL, 2008–2009.
Note. AMIGAS = Amigas, Mujeres Latinas, Informándonos, Guiándonos, y Apoyándonos contra el SIDA (friends, Latina women, informing each other, guiding each other, and supporting each other against AIDS).
We used a 2-arm, randomized, controlled trial design. We assigned participants to the study conditions after the baseline assessment with concealment-of-allocation procedures, defined by protocol and compliant with published recommendations.19 Before enrollment, an investigator used a random-numbers table to generate the allocation sequence. As participants completed baseline assessments, they received sealed opaque envelopes with their assignments. Participants were randomly assigned to either the AMIGAS HIV sexual risk reduction intervention or the general health comparison intervention.
Interventions
Before developing the AMIGAS adaptation, we conducted 3 focus groups with ethnically and culturally diverse Latina women to explore the factors that increased their HIV risks. We collected ethnographic data on their beliefs related to gender and social norms and sexual communication, as well as their knowledge and misconceptions concerning HIV. Information obtained from the focus groups, Latina HIV prevention workers, community representatives, and a review of the literature highlighted the importance of making the intervention culturally congruent. We used a published adaptation framework (ADAPT-ITT)20 to guide a systematic process of selecting and then adapting SiSTA, an HIV risk reduction intervention for young African American women that is widely disseminated with CDC support,21 for use with Latina women. Lessons learned through the cultural adaptation process by community agencies included the challenge—yet importance—of addressing the diverse languages, gender roles, and social norms prevalent among Latina women. We maintained the theoretical foundations of social cognitive theory,22 the theory of gender and power,23 and the core elements of the SiSTA intervention throughout the adaptation process from which AMIGAS emerged.
Latina health educators designed culturally appropriate activities and exercises that incorporated poetry by Latina women; reflections on ethnic pride that addressed the diversity of Latina women; recognition of the effects of social, relational, and gender norms, such as machismo, marianismo, and familismo, on Latina sexual behavior; attempts to dispel HIV misconceptions that are prominent in the Latina community; and role-playing with culturally salient and appropriate themes for Latina women in the Miami area, such as the effect of immigration status on sexual behaviors within relationships. The adapted curriculum was translated into Spanish by a translation services company and was reviewed, modified, back-translated into English, and finally approved by the study team. We then field-tested the adapted curriculum, and Latina community representatives reviewed it before implementation.
We trained 4 Latina health educators from the Miami–Dade County Health Department to deliver AMIGAS. The 3-day training provided a framework for delivering AMIGAS to Latina women at risk for HIV and aimed to enhance the health educators’ HIV-related knowledge and skills for delivery of AMIGAS with fidelity to the intervention curriculum. Trainees observed demonstrations of each AMIGAS activity, participated in group discussions and role-playing activities, and practiced teaching activities to demonstrate their knowledge of the curriculum and to experience delivering the intervention in a group setting.
Two trained Latina health educators presented AMIGAS in Spanish during 4 interactive group sessions lasting 2.5 hours each. The sessions took place on consecutive Thursday evenings at the Miami–Dade County HIV/AIDS Office, with 7 to 8 participants per group. A single trained Latina health educator delivered the general health intervention in Spanish to the women who were randomized to the comparison group. The single-session, 2.5-hour interactive group interventions also took place on Thursday evenings, with an average of 7 to 8 women. Comparison participants viewed a video in Spanish that provided basic HIV information. As with the AMIGAS intervention, we field-tested the general health intervention with Latina women recruited in Miami.
We used quality assurance procedures to monitor the fidelity of program delivery in both intervention curricula. A rater attended every AMIGAS and general health promotion session and recorded whether all activities were implemented with fidelity.
Session 1 of AMIGAS emphasized ethnic, cultural, and gender pride. This session explored the unique strengths, diversity, and beauty of Latina women; acknowledged the accomplishments of influential Latina women; featured readings of poetry by Latina women; reflected on the richness of cultural norms and values; discussed the unwritten rules or social norms prevalent in the Latina culture; and acknowledged the importance of family and religious beliefs among Latina women.
Session 2 emphasized the importance of healthy relationships. The health educators described how unhealthy relationships, including those characterized by abuse and coercion, can create barriers to practicing safer sex. This session also addressed reproduction, the female anatomy, and the value of one's body. Session 3 used video testimonials by Latina women who were living with HIV to enhance participants’ awareness of HIV risk practices and to dispel common myths about HIV in the Latina community. The health educators also discussed the HIV risk reduction strategies of abstinence, consistent condom use, and having fewer male sexual partners. Session 4 explored how experiences such as immigration, deportation, and acculturation can affect HIV risk among Latina women. The participants also engaged in role-playing activities that integrated these culturally appropriate themes and were designed to enhance women's confidence in initiating safer sex conversations, negotiating safer sex, and refusing unsafe sexual encounters.
To assess the efficacy of AMIGAS, we surveyed participants at baseline and at 3- and 6-month postintervention follow-ups. We collected data with the audio computer-assisted self-interviewing method, chosen to enhance confidentiality and participants’ comfort levels and to increase comprehension among women with low literacy. Participants completed the baseline surveys immediately before random assignment to the study conditions. Each assessment was implemented in Spanish and took approximately 45 minutes. Data collectors secured the interview data and were blinded to women's assignment to the intervention arms.
Outcome Measures
We selected consistent condom use as the primary outcome for the study because of its demonstrated effectiveness for reducing sexually transmitted HIV infections.24 We defined consistent condom use as reporting use of condoms with every sexual act in the 30 days and 90 days before the 3- and 6-month follow-ups.
Other self-reported behavioral outcomes were never using condoms, condom use at last vaginal intercourse, proportion of condom-protected vaginal intercourse acts (on average), and number of unprotected vaginal intercourse acts. Preliminary research indicated that anal and oral sex were low-prevalence behaviors; we therefore did not assess them.
We assessed psychosocial constructs with scales that were previously used with Latina women and had satisfactory psychometric properties. We measured cultural norms such as machismo and marianismo with a gender roles scale comprising 10 items, with higher scores indicating a less traditional view of gender roles (α = 0.70).9 We measured HIV knowledge on an 8-item scale, with higher scores indicating greater knowledge about HIV.25 We measured perceived barriers to condom use on a 29-item scale regarding attitudes that can impede participants’ ability to effectively use condoms, with higher scores indicating fewer perceived barriers (α = 0.95).26 We assessed participants’ self-efficacy for negotiating safe sex with their male partners with a 7-item scale (α = 0.90), with higher scores indicating greater comfort level with negotiating safer sex options.27 We measured feelings of power in relationships on a 9-item scale, with higher scores indicating increased feelings of power in a relationship (α = 0.87).28 We measured condom use self-efficacy with a 9-item scale regarding participants’ confidence in their ability to properly use condoms, with higher scores indicating greater self-efficacy (α = 0.90).29
Baseline differences between participants in the 2 interventions on sociodemographic, behavioral, and psychosocial variables with P values of .1 or lower were considered significant for purposes of identifying potential covariates. Of these variables, only the difference in health insurance status was significant. Overall, the majority of participants (72.5%; n = 182) did not have health insurance. At baseline, 81.6% (n = 102) of participants randomized to AMIGAS, and 63.5% (n = 80) of participants in the comparison intervention lacked insurance. Because of the significant difference between participants in the 2 interventions in the prevalence of health insurance at baseline (P = .001), we included this variable as a covariate in all subsequent data analyses.
Statistical Analysis
Analysts were blinded concerning the intervention arm to which participants were assigned. We used an intent-to-treat protocol to analyze participants’ outcomes relative to their assigned intervention, irrespective of the number of sessions they attended.30 At baseline, descriptive statistics summarized sociodemographic variables, psychosocial mediators, and sexual behaviors. We assessed differences between interventions with the t test for continuous variables and χ2 analysis for categorical variables.31 We added sociodemographic variables as covariates when baseline differences between women in the 2 study arms approached statistical significance (P < .1).
We assessed the intervention effects of AMIGAS from baseline assessment to 3 months, from the 3-month to the 6-month follow-up, and for the entire 6-month study period (from baseline to the final follow-up). We analyzed the intervention effects for each 3-month assessment period with logistic regression to compute adjusted odd ratios (AORs) for dichotomous outcomes and linear regression to compute adjusted means and mean differences for continuous outcomes.32,33 Each regression model included the corresponding baseline measure as a covariate in the analysis as well as a measure of intraclass correlation.
To assess the AMIGAS intervention effects for the entire 6-month follow-up period, we constructed logistic and linear generalized estimating equation regression models to control for repeated within-person measurements.34,35 These models incorporated the study conditions as well as covariates and outcomes. We adjusted models for the corresponding baseline measure and covariates to obtain AORs and adjusted mean differences. We also computed the 95% confidence interval (CI) and the corresponding P value. For each model, we calculated adjusted means and standard errors. We computed percentage relative change for continuous variables as the difference between the adjusted means for each condition divided by the adjusted mean for the comparison condition.
RESULTS
Of the 252 randomized participants, 125 were assigned to the AMIGAS intervention and 127 to the general health promotion intervention. One participant's data were lost and therefore were not included in data analysis. Participants’ average age was 30.3 (SD = 6.86) years, 43.8% (n = 110) had 12 years or less of education, the majority (54.8%; n = 136) were receiving public assistance, 42.2% (n = 106) were employed, and 13.9% (n = 35) received most of their money from their main sexual partner. During the past year, women reported having, on average, 2.45 sexual partners (SD = 1.33); 45.8% (n = 115) reported having only 1 sexual partner. However, in the past 90 days, most participants (79.3%; n = 199) had only 1 sexual partner, and this was generally a main sexual partner (64.5%; n = 162). Women who had a main sexual partner had been in that relationship for an average of 3.4 years (SD = 5.14).
Participants
Participants were predominantly foreign born: 38.2% (n = 96) were from South American countries, 25.5% (n = 64) from Cuba, 19.9% (n = 50) from Central American countries, 4% (n = 10) from the Dominican Republic, 2% (n = 5) from Puerto Rico, and 1.6% (n = 4) from Mexico. Only 8.8% (n = 22) were born in the United States. Most participants (81.7%; n = 205) reported having legal status in the United States, had arrived when they were aged 22.0 (SD = 8.0) years, and had resided in the United States for 9.2 (SD = 8.4) years.
In both interventions, 98% of the activities were completed as outlined in the curricula. Participants’ attendance was high: 82.4% (n = 103) of participants completed all 4 AMIGAS sessions, and all participants (n = 127) completed the single general health promotion session. On a 5-point scale, participants indicated comparably high ratings for satisfactory delivery of AMIGAS (mean = 4.60; SD = 0.51) and the general health intervention (mean = 4.55; SD = 0.52).
Of the 125 participants who were assigned to the AMIGAS intervention, 102 (81.6%) completed the 3-month assessment, and 109 (87.2%) completed the 6-month assessment. Of the 127 participants allocated to the general health intervention, 101 (79.5%) completed the 3-month assessment, and 115 (90.6%) completed the 6-month assessment. We found no significant differences in attrition between AMIGAS and comparison intervention participants (P = .24).
Intervention Effects
For the primary outcome, we measured the proportion of participants reporting consistent condom use in both intervention groups. Over the entire 6-month follow-up period, AMIGAS participants were 4.8 times as likely as comparison participants to report using condoms consistently during the past 90 days (P < .001) and 3.1 times as likely to report using condoms consistently during the past 30 days (P < .001; Table 1). Similarly, over the entire 6-month follow-up period, AMIGAS participants were 53% less likely than were comparison participants to report never having used condoms during the past 90 days (AOR = 0.47; 95% CI = 0.27, 0.81; P = .007) and 48% less likely to report never having used condoms during the past 30 days (AOR = 0.52; 95% CI = 0.30, 0.90; P = .02). Finally, AMIGAS participants were 2.8 times as likely as were comparison participants to report using condoms at last sexual encounter (P < .001).
TABLE 1.
Effects of AMIGAS and Comparison HIV Interventions for Latina Women on Condom Use Behaviors: Miami, FL, 2008–2009
| Baseling Assessmenta |
3-Month Assessmenta |
6-Month Assessmenta |
GEE Model Baseline to 6-Month Assessment |
|||||||||
| Behavior | AMIGAS, % | Comparison, % | AMIGAS, % | Comparison, % | AORb (95% CI) | P | AMIGAS, % | Comparison, % | AOR (95% CI) | P | AOR (95% CI) | P |
| Consistent condom use | ||||||||||||
| Past 90 d | 5.9 | 4.8 | 43.5 | 14.7 | 5.59 (2.45,12.75) | < .001 | 39.0 | 14.3 | 4.87 (2.27, 10.42) | < .001 | 4.81 (2.48, 9.35) | < .001 |
| Past 30 d | 9.2 | 11.9 | 50.6 | 24.7 | 3.13 (1.48, 6.61) | .003 | 45.5 | 24.5 | 3.36 (1.64, 6.90) | < .001 | 3.14 (1.78, 5.56) | < .001 |
| Never used condoms | ||||||||||||
| Past 90 d | 55.5 | 49.2 | 22.8 | 42.1 | 0.33 (0.15, 0.72) | .005 | 27.0 | 38.1 | 0.54 (0.28, 1.03) | .06 | 0.47 (0.27, 0.81) | .007 |
| Past 30 d | 60.5 | 61.0 | 30.6 | 44.9 | 0.60 (0.27, 1.33) | .21 | 30.3 | 47.1 | 0.48 (0.25, 0.94) | .03 | 0.52 (0.30, 0.90) | .02 |
| Condom use at last sexual encounter | 19.4 | 20.6 | 60.8 | 32.7 | 3.54 (1.88, 6.68) | < .001 | 52.3 | 36.3 | 1.96 (1.12, 3.40) | .02 | 2.76 (1.64, 4.65) | < .001 |
Note. AMIGAS = Amigas, Mujeres Latinas, Informándonos, Guiándonos, y Apoyándonos contra el SIDA (friends, Latina women, informing each other, guiding each other, and supporting each other against AIDS); AOR = adjusted odds ratio; CI = confidence interval; GEE = generalized estimating equation.
Unadjusted proportions.
Adjusted for baseline value of the outcome variable and having health insurance; comparison intervention was the referent for computing the AOR.
Over the entire 6-month follow-up period, AMIGAS participants reported a significantly higher mean percentage of condom use during the past 90 days (relative change = 55.72%; P < .001) and the past 30 days (relative change = 43.75%; P < .001) than did comparison participants (Table 2). Over the entire 6-month follow-up period, AMIGAS participants reported a significantly lower mean number of episodes of unprotected vaginal intercourse during the past 90 days than did comparison participants (relative change = −33.98%; P = .007) and a nonsignificant trend of fewer episodes of self-reported unprotected vaginal intercourse in the previous 30 days (relative change = −31.63%; P = .06; Table 2).
TABLE 2.
Effects of AMIGAS and Comparison HIV Interventions for Latina Women on Condom Use Behaviors: Miami, FL, 2008–2009
| Baseline Assessment |
3-Month Assessment |
6-Month Assessment |
GEE Model Baseline to 6-Month Assessment |
|||||||||
| Behavior | AMIGAS, Unadjusted Mean (SD) | Comparison, Unadjusted Mean (SD) | AMIGAS, Adjusted Mean (SD) | Comparison, Adjusted Mean (SD) | Relative Change,a % (95% CI) | P | AMIGAS, Adjusted Mean (SD) | Comparison, Adjusted Mean (SD) | Relative Change,a % (95% CI) | P | Relative Change,a % (95% CI) | P |
| Condom use (past 90 d), % | 22.65 (32.93) | 24.45 (33.20) | 59.50 (4.24) | 33.23 (4.90) | 79.06 (43.51, 114.58) | < .001 | 55.88 (4.16) | 38.58 (4.02) | 44.84 (15.06, 74.58) | .003 | 55.72 (29.39, 82.05) | < .001 |
| Condom use (past 30 d), % | 22.47 (34.38) | 22.58 (35.50) | 57.49 (4.68) | 40.08 (4.56) | 43.44 (10.67, 76.19) | .009 | 56.16 (4.33) | 40.15 (4.30) | 39.87 (9.81, 69.96) | .009 | 43.75 (18.38, 69.11) | < .001 |
| Unprotected vaginal intercourse (past 90 d), % | 17.58 (24.97) | 18.32 (18.74) | 10.59 (1.80) | 17.39 (1.74) | −39.10 (−67.86, −10.34)) | .008 | 10.92 (1.78) | 15.57 (1.70) | −29.87 (−61.12, 1.40) | .06 | −33.98 (−58.67, −9.30) | .007 |
| Unprotected vaginal intercourse (past 30 d), % | 7.20 (10.04) | 6.82 (6.42) | 4.85 (0.89) | 6.68 (0.86) | −27.40 (−64.68, 9.83) | .15 | 5.04 (1.05) | 7.28 (1.10) | −30.77 (−72.33,10.65) | .15 | −31.63 (−65.01, 1.76) | .06 |
Note. AMIGAS = Amigas, Mujeres Latinas, Informándonos, Guiándonos, y Apoyándonos contra el SIDA (friends, Latina women, informing each other, guiding each other, and supporting each other against AIDS); CI = confidence interval; GEE = generalized estimating equation.
Relative change = [mean difference between AMIGAS and comparison/mean for the comparison group × 100%] and 95% CI around the relative change.
We also observed marked differences in hypothesized psychosocial mediators of HIV risk-reduction behaviors. Over the entire 6-month follow-up period, AMIGAS participants reported fewer traditional views of gender roles (P = .008) than did comparison participants; they also had higher HIV knowledge scores (P = .009) and reported fewer perceived barriers to using condoms (P < .001), greater self-efficacy for negotiating safe sex (P < .001), greater perception of power in their relationships (P = .02), and greater self-efficacy for using condoms (P < .001; Table 3).
TABLE 3.
Effects of AMIGAS and Comparison HIV Interventions for Latina Women on Psychosocial Mediators: Miami, FL, 2008–2009
| Baseline Assessment |
3-Month Assessment |
6-Month Assessment |
GEE Model Baseline-6-Month Assessment |
|||||||||
| Mediator | AMIGAS, Unadjusted Mean (SD) | Comparison, Unadjusted Mean (SD) | AMIGAS, Adjusted Mean (SD) | Comparison, Adjusted Mean (SD) | Relative Change,a % (95% CI) | P | AMIGAS, Adjusted Mean (SD) | Comparison, Adjusted Mean (SD) | Relative Change,a % (95% CI) | P | Relative Change,a % (95% CI) | P |
| Traditional views of gender roles (range = 10–40) | 26.66 (4.81) | 27.48 (4.49) | 29.71 (0.42) | 28.25 (0.42) | 5.17 (1.01, 9.33) | .01 | 30.29 (0.41) | 29.16 (0.40) | 3.88 (0.02, 7.79) | .05 | 4.41 (1.17, 7.66) | .008 |
| HIV knowledge (range = 1–8) | 6.49 (1.32) | 6.65 (1.38) | 7.56 (0.08) | 7.30 (0.08) | 3.56 (0.57, 6.88) | .02 | 7.49 (0.08) | 7.28 (0.08) | 2.88 (−0.03, 5.86) | .05 | 3.25 (0.82, 5.69) | .009 |
| Condom barriers (range = 29–116) | 79.04 (17.16) | 79.00 (17.95) | 91.31 (1.48) | 85.08 (1.48) | 7.32 (2.43, 12.22) | .003 | 94.87 (1.40) | 87.05 (1.37) | 8.98 (4.55, 13.43) | < .001 | 8.12 (4.25, 11.99) | < .001 |
| Sexual negotiation self-efficacy (range = 7–28) | 19.11 (5.81) | 19.89 (5.22) | 23.39 (0.41) | 21.27 (0.41) | 9.97 (4.44, 15.46) | < .001 | 23.79 (0.42) | 21.61 (0.41) | 10.09 (4.75, 15.44) | < .001 | 10.12 (5.65, 14.59) | < .001 |
| Power in relationship (range = 9–36) | 25.94 (5.52) | 26.36 (5.22) | 28.42 (0.42) | 27.23 (0.42) | 4.37 (0.05, 8.70) | .05 | 29.09 (0.43) | 27.94 (0.42) | 4.12 (−0.14, 8.41) | .06 | 4.12 (0.54, 7.71) | .02 |
| Condom use self-efficacy (range = 9–27) | 20.71 (5.05) | 21.24 (4.42) | 24.59 (0.35) | 22.08 (0.35) | 11.37 (6.93, 15.79) | < .001 | 24.33 (0.40) | 22.31 (0.39) | 9.05 (4.10, 13.93) | < .001 | 10.39 (6.44, 14.34) | < .001 |
Note. AMIGAS = Amigas, Mujeres Latinas, Informándonos, Guiándonos, y Apoyándonos contra el SIDA (friends, Latina women, informing each other, guiding each other, and supporting each other against AIDS); CI = confidence interval; GEE = generalized estimating equation.
Relative change = [mean difference between AMIGAS and comparison/mean for the comparison group x 100%] and 95% CI around the relative change.
DISCUSSION
Our study was among the first linguistic and cultural adaptations of an HIV sexual risk reduction intervention to demonstrate marked increases in HIV-protective behaviors for an ethnically diverse population of Latina women. Over the entire 6-month follow-up period, AMIGAS participants were more than 4.5 times as likely as comparison participants to use condoms consistently during the past 90 days and 53% less likely to report having never used condoms during the past 90 days. AMIGAS participants reported statistically significant reductions in the mean number of unprotected vaginal intercourse acts and statistically significant increases in percentage condom use and condom use at last sexual encounter. We also observed favorable changes in hypothesized psychosocial mediators of HIV risk-reduction behaviors, with the majority of changes significant across the entire 6-month follow-up period and for each of the 3-month assessment periods. It is noteworthy that we obtained these results in a population composed predominantly of Latina immigrants who reported being in long-term sexual relationships. This is particularly important because stable, long-term relationships can create significant barriers for women who try to negotiate safer sex with their male partners.28
A recent meta-analysis described the importance of using health care providers, counselors, or professional facilitators to implement HIV sexual risk reduction interventions for Latinos.12 Our results extended these findings, highlighting the importance of using Latina health educators to implement HIV sexual risk reduction interventions for Latina women. The Latina health educators implemented the AMIGAS curriculum with remarkable fidelity. Of all the activities outlined in the curriculum, 98% were independently rated as having been correctly implemented. The participants also gave health educators superior ratings for the manner in which they delivered the curriculum.
The efficacy of AMIGAS may also be partly attributable to inclusion of Latina women and integration of Latina cultural values in all facets of the study, from the conceptualization, adaptation, and implementation of the intervention to the recruitment and retention of participants and study evaluation. Another factor that may have contributed to the demonstrated efficacy of AMIGAS in reducing HIV-associated sexual risk behaviors was the study team's decision to adapt SiSTA, an HIV intervention for young adult African American women that has been assessed by a randomized controlled study, is widely disseminated with CDC support and is extremely popular with service provider organizations. The adaptation process remained faithful to the underlying theories and core elements of the original SiSTA intervention.
Limitations
We relied on self-report data, had a relatively short follow-up, were unable to assess condom use by partner type, and lacked objective and quantifiable biological outcomes, such as incident sexually transmitted infections, to assess intervention efficacy. Future trials of HIV interventions conducted with ethnically diverse samples of Latina women would benefit by addressing these limitations.
An additional methodological limitation was that our comparison intervention also focused on HIV, rather than serving as a true placebo to guard against Hawthorne effects. Thus, future HIV prevention trials would benefit from inclusion of a time-equivalent comparison condition that focuses on a topic other than HIV prevention but addresses a relevant and important health issue for Latina women.
Conclusions
The CDC encourages health departments and community organizations to use evidence-based behavioral interventions in their HIV prevention programs.36 In practice, many service providers adapt these interventions to facilitate implementation, encourage community ownership, and increase acceptability of the interventions by new target populations. Providers may also deliver interventions that they have developed on their own or with research partners.37 Ours was the first successful efficacy trial of a systematic linguistic and cultural adaptation of an evidence-based intervention for use with a diverse Latina population.
Our study also illustrated the successful adaptation of an intervention by a health department. Key contributing factors to this success were very high levels of commitment and effort by health department staff throughout the process. Additional contributing factors were a strong partnership and effective collaboration of the health department with other community agencies and university researchers.38
The experience of adapting and assessing the efficacy of the AMIGAS intervention enhanced the health department's capacity to seek and obtain federal and nonfederal funding for its prevention efforts and to conduct research; it also highlighted the importance of including community members in all aspects of the research: study design, tailoring of survey instruments, development of intervention vignettes, and intervention materials for the study population. Future researchers should consider the value of engaging health departments and other community agencies in conceptualizing, adapting, implementing, and evaluating HIV risk reduction interventions.
Acknowledgments
This study was funded by the Centers for Disease Control and Prevention (contract 200-2007-23647) and the Emory University Center for AIDS Research (grant P30 AI050409).
We acknowledge all those who assisted us, including our health educators, Esther Concepcíon, Jersey García, Lily Martin, Belkis Perea, Clery Quirós, Angélica Urbina, and Virginia Muñoz; our project recruiters, Rut Bográn-Licona and Ana Maria Santiesteban; our data collection assistants, Anna Barreiro and Ericka Cordova; our support staff, Damaries Cruz, Reynayira Guido, and Luz Lang; and those who trained us, Zaida Castillo and Nikia Braxton. We also appreciate all the support from the Latina women in the program.
Human Participant Protection
The study protocol was approved by the institutional review boards of the State of Florida Department of Health, the Centers for Disease Control and Prevention, and Emory University.
References
- 1.US Bureau of the Census. Facts for features. Hispanic Heritage Month 2007: Sept. 15–Oct. 15. Available at: http://www.census.gov/newsroom/releases/archives/facts_for_features_special_editions/cb07-ff14.html. Accessed November 13, 2010.
- 2.US Bureau of the Census. Hispanic origin and/or Latino tables from the statistical abstract of the United States: 2004–2005. Table 41:18. Available at: http://www.census.gov/statab/www/sa04hisp.pdf. Accessed November 13, 2010.
- 3.Centers for Disease Control and Prevention. HIV/AIDS among Hispanics—United States, 2001–2005. MMWR Morb Mortal Wkly Rep. 2007;56(40):1052–1057. [PubMed] [Google Scholar]
- 4.Espinoza L, Hall HI, Selik RM, Hu X. Characteristics of HIV infection among Hispanics, United States 2003–2006. J Acquir Immune Defic Syndr. 2008;49(1):94–101. [DOI] [PubMed] [Google Scholar]
- 5.Centers for Disease Control and Prevention. HIV Surveillance Report, 2008. Vol. 20 Atlanta, GA: US Department of Health and Human Services; 2010. Available at: http://www.cdc.gov/hiv/surveillance/resources/reports/2008report/table24.htm. Accessed November 13, 2010. [Google Scholar]
- 6.Uribe CL, Darrow WW, Villanueva LP, Obiaja KC, Sanchez-Bana E, Gladwin H. Identifying HIV risk-reduction strategies for Hispanic populations in Broward County. Ann Epidemiol. 2009;19(8):567–574. [DOI] [PubMed] [Google Scholar]
- 7.Gomez C, Marín BV. Gender, culture and power: barriers to HIV prevention strategies for women. J Sex Res. 1996;33(4):355–362. [Google Scholar]
- 8.Marín BV. HIV prevention in the Hispanic community: sex, culture, and empowerment. J Transcult Nurs. 2003;14(3):186–192. [DOI] [PubMed] [Google Scholar]
- 9.Marín BV. Cultural issues in HIV prevention for Latinos: should we be changing gender roles. : Oskamp S, Thompson S, Understanding and Preventing HIV Risk Behavior: Safer Sex and Drug Use. Thousand Oaks, CA: Sage; 1996:157–176. [Google Scholar]
- 10.Stevens ED. Marianismo: the other face of machismo in Latin America. : Discatello A, Female and Male in Latin America. Pittsburgh, PA: University of Pittsburgh Press; 1973:89–102. [Google Scholar]
- 11.Triandis HC, Marín G, Lisansky J, Betancourt H. Simpatía as a cultural script of Hispanics. J Pers Soc Psychol. 1984;47(6):1363–1375. [Google Scholar]
- 12.Herbst JH, Kay LS, Passin WF, et al. A systematic review and meta-analysis of behavioral interventions to reduce HIV risk behaviors of Hispanics in the United States and Puerto Rico. AIDS Behav. 2007;11(1):25–47. [DOI] [PubMed] [Google Scholar]
- 13.Lyles CM, Crepaz N, Herbst JH, Kay LS. Evidence-based HIV behavioral prevention from the perspective of the CDC's HIV/AIDS Prevention Research Synthesis Team. AIDS Educ Prev. 2006;18(suppl):21–31. [DOI] [PubMed] [Google Scholar]
- 14.DiClemente RJ, Wingood GM. A randomized controlled trial of an HIV sexual risk reduction intervention for young African-American women. JAMA. 1995;274(16):1271–1276. [PubMed] [Google Scholar]
- 15.Larkey LK, Gonzalez JA, Mar LE, Namino G. Latina recruitment for cancer prevention education via Community Based Participatory Research strategies. Contemp Clin Trials. 2009;30(1):47–54. [DOI] [PubMed] [Google Scholar]
- 16.Castro FG, Cota MK, Vega SC. Health promotion in Latino populations: a sociocultural model for program planning, development and evaluation. : Huff RM, Kline MV, Promoting Health in Multicultural Populations: A Handbook for Practicioners. Thousand Oaks, CA: Sage Publications; 1999:137–223. [Google Scholar]
- 17.Escobar-Chaves SL, Tortolero SR, Masse LC, Watson KB, Fulton JE. Recruiting and retaining minority women: findings from the Women on the Move study. Ethn Dis. 2002;12:242–251. [PubMed] [Google Scholar]
- 18.Moreno-John G, Gachie A, Fleming CM. Ethnic minority older adults participating in clinical research: developing trust. J Aging Health. 2004;16:93S–123S. [DOI] [PubMed] [Google Scholar]
- 19.Schulz KF. Subverting randomization in controlled trials. JAMA. 1995;274:1456–1458. [PubMed] [Google Scholar]
- 20.Wingood GM, DiClemente RJ. The ADAPT-ITT model: A model for adapting evidence-based HIV interventions. J Acquir Immune Defic Syndr. 2008;47(suppl 1):S40–S46. [DOI] [PubMed] [Google Scholar]
- 21.Centers for Disease Control. Diffusion of effective behavioral interventions project fact sheet. Available at: http://www.effectiveinterventions.org/Libraries/General_Docs/10-1022_DEBI_overview_factsheet.sflb.ashx. Accessed November 21, 2010.
- 22.Bandura A. Social cognitive theory and exercise of control over HIV infection. : DiClemente RJ, Peterson J, Preventing AIDS: Theories and Methods of Behavioral Interventions. New York, NY: Plenum Publishing; 1994:25–59. [Google Scholar]
- 23.Wingood GM, DiClemente RJ. Application of the theory of gender and power to examine HIV-related exposures, risk factors and effective interventions for women. Health Educ Behav. 2000;27(5):539–565. [DOI] [PubMed] [Google Scholar]
- 24.de Vincenzi I. A longitudinal study of human immunodeficiency virus transmission by heterosexual partners. European Study Group on Heterosexual Transmission of HIV. N Engl J Med. 1994;331(6):341–346. [DOI] [PubMed] [Google Scholar]
- 25.Sikkema KJ, Kelly JA, Winett RA, et al. Outcomes of a randomized community-level HIV prevention intervention for women living in 18 low-income housing developments. Am J Public Health. 2000;90(1):57–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.St Lawrence JS, Chapdelaine AP, Devieux JG, O'Bannon RE, 3rd, Brasfield TL, Eldridge GD. Measuring perceived barriers to condom use: psychometric evaluation of the condom barriers scale. Assessment. 1999;6(4):391–404. [DOI] [PubMed] [Google Scholar]
- 27.Marín BV, Gómez CA, Tschann JM, Gregorich SE. Self-efficacy to use condoms in unmarried Latino adults. Am J Community Psychol. 1998;26(1):53–71. [DOI] [PubMed] [Google Scholar]
- 28.Wingood GM, DiClemente RJ. Partner influences and gender-related factors associated with noncondom use among young adult African-American women. Am J Community Psychol. 1998;26(1):29–51. [DOI] [PubMed] [Google Scholar]
- 29.Marín BV, Gómez CA, Tschann JM, Gregorich SE. Condom use in unmarried Latino men: a test of cultural constructs. Health Psychol. 1997;16(5):458–467. [DOI] [PubMed] [Google Scholar]
- 30.Piantadosi S. Clinical Trials: A Methodologic Perspective. New York, NY: John Wiley & Sons; 1997. [Google Scholar]
- 31.Fleiss JL, Levin B, Paik MC. Statistical Methods for Rates and Proportions. 3rd ed New York, NY: Wiley & Sons; 2003. [Google Scholar]
- 32.Hosmer DW, Lemeshow SL. Applied Logistic Regression. New York, NY: John Wiley & Sons; 1989. [Google Scholar]
- 33.Kleinbaum DG, Kupper LL, Muller KE, et al. Applied Regression Analysis and Other Multivariable Methods. New York, NY: Duxbury Press; 1998. [Google Scholar]
- 34.Hardin JW, Hilbe JM. Generalized Estimating Equations. New York, NY: Chapman & Hall; /CRC; 2003. [Google Scholar]
- 35.Liang KY, Zeger SL. Longitudinal data analysis using generalized linear models. Biometrika. 1986;73(1):13–22. [Google Scholar]
- 36.Centers for Disease Control and Prevention. 2003–2008. HIV prevention community planning guide. Available at: http://www.cdc.gov/hiv/pubs/hiv-cp.htm. Accessed November 29, 2010.
- 37.Painter TM, Ngalame P, Lucas B, Lauby J, Herbst JH. Strategies used by community-based organizations when evaluating their locally developed HIV prevention interventions for minority populations: lessons learned from CDC's innovative interventions project. AIDS Educ Prev. 2010;22(5):387–401. [DOI] [PubMed] [Google Scholar]
- 38.Bogart LM, Uyeda K. Community-based participatory research: partnering with communities for effective and sustainable behavioral health interventions. Health Psychol. 2009;28(4):391–393. [DOI] [PMC free article] [PubMed] [Google Scholar]