Abstract
Objectives. We used Canadian population-based data to examine changes in the health of caregivers of children with complex health problems compared with caregivers of healthy children over a 10-year time period.
Methods. The National Longitudinal Survey of Children and Youth collected data biennially from 9401 children and their caregivers in 6 waves from 1994–1995 to 2004–2005. We conducted growth-curve analyses of these data to model self-reported general health and depressive symptoms for 4 groups of caregivers: caregivers of healthy children, and caregivers of children with 1, 2, or at least 3 of 4 conceptually distinct indicators of child health problems. We modeled covariates for children (age, gender, only-child status) and caregivers (age, gender, education, income, marital status).
Results. After we controlled for covariates, caregiver health outcomes worsened incrementally with increasing complexity of child health problems. Change in self-reported general health and depressive symptoms over the 10-year period was consistent across all groups of caregivers.
Conclusions. Poorer health among caregivers of children with health problems can persist for many years and is associated with complexity of child health problems. Attention to parental health should form a component of health care services for children with health problems.
Caring for any child is a demanding task, but parents of children with chronic physical or psychological health problems can face significantly greater caregiving challenges, including greater time demands,1,2 higher medical and other related costs,3–5 child care challenges,6–8 lower incomes,7,9,10 and employment constraints.8,9 Coupled with these challenges are societal changes (smaller family units, more single-parent families11) and trends in health care (innovations that increase life expectancy of children with severe disabilities,12 family-centered models of health care,13,14 increased emphasis on value for money spent on health care15,16) that may inadvertently increase the burden on caregivers of children with chronic health problems.
Evidence is now accumulating that these challenges have implications for caregiver health.1,2,5,9,17–20 For example, we recently showed that caregivers of children with health problems had more than twice the odds of having chronic health problems, activity limitations, and depressive symptoms compared with the population of caregivers of healthy children.21 Our broad definition of child “health problems” included approximately 26% of Canadian families, but we still found strong caregiver health effects, suggesting that the health of caregivers of children with health problems is an important public health issue.
Previous work examining the relationship between the caregiving situation and caregiver health has provided many cross-sectional snapshots of caregiver health, but relatively few controlled studies have examined whether these relationships change over time. Longitudinal studies that do exist have yielded strikingly diverse, if not contradictory, results. Initial findings among elderly caregivers of people with Alzheimer's disease22–24 and among caregivers of children25,26 have suggested that caregivers might experience worsening health over time as wear and tear accumulates, but these findings have been challenged by studies showing that both the physical and the psychological health of these caregivers remains relatively stable over the study periods (typically < 2 years).2,22,27,28
In other circumstances, caregiver health can improve over time. Mothers of children with cancer reported lower anxiety scores 20 months after the diagnosis than they did at the time of diagnosis.29,30 Similarly, levels of distress were initially elevated in mothers and fathers of children diagnosed with diabetes, but their symptoms resolved over a 12-month period.31 Other studies have demonstrated positive aspects of parenting—including decreases in anxiety, depression, and mortality—that may be tied to feelings of empowerment when the caregiver is able to provide effective help.32–36
Several methodological issues may have contributed to this variability in results. Studies have typically focused on relatively small samples that are limited in their power to demonstrate change. Many studies did not include control groups, making it impossible to examine relative changes in health. Existing longitudinal studies have often involved elderly caregivers or have only included children with specific health problems, producing results that may not generalize well to caregivers of children with a broader range of health problems. Most studies have also typically been limited to relatively short time frames (< 2 years; but see Brehaut et al.,9 Seltzer et al.,26 and Brown et al.36), and therefore may not be sensitive to processes that manifest over longer periods of time.
We examined a large-scale Canadian sample of children and caregivers to determine changes in the health of caregivers of children with health problems. By employing data from a population-based national study, we were able to conduct more sensitive analyses on a broader sample than has existed in the literature to date. We examined the extent to which the complexity of the child health problem affects caregiver health compared with a healthy comparison group. We examined the scope of caregiver health effects across a wide spectrum of childhood illness rather than limiting our study to a single clinical area. And because the data source offers 6 cycles of repeated measurements of caregiver health over the course of 10 years, we had an unprecedented opportunity to examine whether these effects change over a longer period of time.
METHODS
We drew our data from the National Longitudinal Survey of Children and Youth (NLSCY), a long-term study of the physical and social development of Canadian children, conducted jointly by Statistics Canada and Human Resources and Skills Development Canada.37 The person most knowledgeable (PMK) about the target child provided information about the child, himself or herself, and any spouse or partner. In approximately 90% of cases, the PMK was the child's biological mother. The first wave of interviews was conducted in 1994 and has been repeated biennially since then. We used data from cycles 1 (1994–1995) through 6 (2004–2005), when the youths were aged from 4 to 15 years. We did not include data from later cycles because PMKs no longer responded for children older than 15 years.
Procedures for sample selection have been reported elsewhere.21 In short, we limited the study sample to 1 child–PMK pair per household, which resulted in 9401 child–caregiver pairs at cycle 1 in 1994–1995. Additional sampling details are presented in the Appendix (available as a supplement to the online version of this article at http://www.ajph.org).
Types and Complexity of Child Health Problems
Our broad measure of child health problems has been detailed elsewhere.21,38 Briefly, we have shown that grouping individuals by combining several indicators (e.g., no indicators, 1 indicator, 2 or more indicators) produced broad categories of caregiving situations that were distinguishable according to both child and caregiver health. These 4 broad indicators of child health include (1) presence of an activity limitation, (2) functional problems as indicated by a Health Utilities Index cutoff score of 0.81,39 (3) presence of a chronic condition as determined by checklist response, and (4) elevated health services use. We developed these 4 indicators on the basis of concepts adapted from the Children with Special Health Care Needs screener.40 Further details about the models are presented in the Appendix.
We grouped caregivers according to how many of the 4 key indicators of child ill health we identified for a given child. On the basis of our previous analyses and experience,21,41 we decided to use the number of these key indicators identified for a given child as a marker of the complexity of a child's health problems. That is, we hypothesize that caring for a child with a chronic condition alone, whatever that chronic condition might be, will usually be less complex (and will have fewer implications for caregiver health) than caring for a child with a chronic condition and an activity limitation, a chronic condition and high services use, or any other combination of 2 or more of the 4 key indicators. Furthermore, we hypothesized that children with health problems that are less complex would be relatively healthy and would have relatively healthy caregivers, whereas children with health problems that are more complex would have poorer health and would have caregivers with poorer health. We compared 4 groups of caregivers on the basis of the complexity of their child's health problems: caregivers of healthy children (0 health problem indicators) and caregivers of children identified by 1, 2, or 3 or more indicators.
Additional measures of child health served as validation of our notion that the number of key indicators was associated with child health. These PMK-reported measures were (1) child's general health as reported on a 5-point scale, where 1 represented “excellent” and 5 represented “poor” general health, (2) whether the child had sustained a serious injury over the past year (yes or no), and (3) estimated number of physician visits in the past year. We also included a measure of behavior problems on the basis of previous work. Further details are presented in the Appendix.
Caregiver Health and Covariates
We examined the trajectories of 2 self-reported caregiver health outcomes: general health (excellent/very good vs good/fair/poor) and depressive symptoms (on the basis of a shortened version of the Center for Epidemiological Studies Depression Scale).42,43 Further details are presented in the Appendix.
We included child gender and age at baseline in the growth-curve models as time-invariant covariates. We categorized the child's age at baseline (time 0) into 3 groups: ages 4 to 6 years, ages 7 to 9 years (reference group), and ages 10 to 11 years. We also included caregiver gender, baseline age (time 0), and educational attainment as time-invariant covariates. Time-varying covariates were income, marital status (single, never married, divorced/separated/widowed), and number of children (1, multiple). Further details are presented in the Appendix.
Analysis
We examined outcome and covariate descriptive statistics (proportions, means) separately for the 4 caregiver subgroups. We used the χ2 test and the t test as appropriate to examine intergroup comparisons, after adopting a strict α of 0.001. We used linear growth-curve models to examine caregiver depression over time, and we used logistic growth-curve models to examine caregivers’ self-reported general health. We retained significant interactions in the final model along with all baseline effects. We conducted descriptive analyses in SAS version 10.1 (SAS Institute, Cary, NC), and we conducted growth-curve analyses in MLwiN version 2.02 (Centre for Multilevel Modelling, Bristol, UK). Further details about the models are available in the Appendix.
RESULTS
We examined the 4 child health complexity groups (healthy, 1 indicator, 2 indicators, 3 or more indicators) in terms of both child (Table 1) and caregiver (Table 2) characteristics at baseline (1994–1995). Greater complexity was associated with a greater proportion of the children being male (range 47.2%–60.5%). Children in the 3 or more indicators group were somewhat older at baseline than were healthy children (3 or more indicators: 8.1 years; healthy: 7.4 years). As expected, the 4 groups differed on all child health status measures (Table 1).
TABLE 1.
Children's Demographic and Health Characteristics, by Child Health Indicator Group: National Longitudinal Survey of Children and Youth, Canada, 1994–2005
| Characteristics | Healthy Children (n = 3722), % or Mean (SD) | Children With 1 Health Indicator (n = 3229), % or Mean (SD) | Children With 2 Health Indicators (n = 1709), % or Mean (SD) | Children With ≥ 3 Health Indicators (n = 741), % or Mean (SD) |
| Demographics | ||||
| Male | 47.2bcd | 51.6acd | 58.6ab | 60.5ab |
| Age at baseline, y | 7.4d (2.4) | 7.4d (2.3) | 7.5d (2.3) | 8.1abc (2.1) |
| Only child | 18.6b | 14.4ad | 17.7 | 19.8b |
| Child health status at baseline | ||||
| Excellent/very good general health | 94.3bcd | 88.5acd | 74.4abd | 51.0abc |
| Injured in the past y | 7.8bcd | 13.3a | 14.3a | 16.1a |
| No. of doctor visits in the past y | 1.5bcd (1.4) | 4.1acd (6.0) | 7.0abd (8.9) | 13.2abc (17.9) |
| Behavior problems | 21.7bcd | 28.3acd | 36.0abd | 54.9abc |
Estimate differs significantly (P < .001) from group of healthy children.
Estimate differs significantly (P < .001) from group of children with 1 indicator.
Estimate differs significantly (P < .001) from group of children with 2 indicators.
Estimate differs significantly (P < .001) from group of children with ≥ 3 indicators.
TABLE 2.
Caregivers’ Demographic and Health Characteristics, by Child Health Indicator Group: National Longitudinal Survey of Children and Youth, Canada, 1994–2005
| Characteristics | Caregivers of Healthy Children (n = 3722), % or Mean (SD) | Caregivers of Children With 1 Health Indicator (n = 3229), % or Mean (SD) | Caregivers of Children With 2 Health Indicators (n = 1709), % or Mean (SD) | Caregivers of Children With ≥ 3 Health Indicators (n = 741), % or Mean (SD) |
| Demographics | ||||
| Female | 90.2d | 91.3 | 92.2 | 94.2a |
| Age, y | 35.3bc (5.9) | 34.8a (5.6) | 34.5a (5.3) | 34.8 (5.5) |
| Relationship to child | ||||
| Biological mother | 88.4 | 89.6 | 90.4 | 89.5 |
| Biological father | 9.2d | 8.1 | 7.3 | 5.4a |
| Other | 2.4d | 2.3d | 2.3d | 5.1abc |
| Marital status at baseline | ||||
| Single, never married | 5.1 | 5.4 | 6.4 | 6.8 |
| Married, including common law | 85.7cd | 84.7d | 81.4a | 75.7ab |
| Divorced, widowed, separated | 9.2cd | 9.9d | 12.2ad | 17.5abc |
| Experienced a change in marital status during follow-up | 12.8 | 13.5 | 13.8 | 15.7 |
| Highest educational attainment at baseline | ||||
| < high school | 17.8 | 17.2 | 17.5 | 21.2 |
| High school graduate | 21.6 | 20.4 | 19.0 | 18.8 |
| Some postsecondary education | 27.6 | 27.7 | 30.6 | 29.8 |
| Postsecondary degree | 33.0 | 34.7 | 32.8 | 30.2 |
| Income | ||||
| Annual income, $ | 48 192 (35 792) | 48 465 (34 404) | 46 266 (30 027) | 44 034 (31 633) |
| < LICO ratio of 1.0 | 22.7d | 22.2d | 23.6 | 29.4ab |
| Health status at baseline | ||||
| Excellent/very good general health | 76.9bcd | 72.0ad | 68.7ad | 60.7abc |
| Depressive symptoms score,e cycle 1 (1994–1995) | 4.2bcd (5.0) | 4.8ad (5.3) | 5.4ad (5.7) | 7.1abc (7.0) |
Note. LICO = low-income cut-off, an indicator of low income based on family size and before-tax percentage of income spent on necessities.
Estimate differs significantly (P < .001) from group of healthy children.
Estimate differs significantly (P < .001) from group of children with 1 indicator.
Estimate differs significantly (P < .001) from group of children with 2 indicators.
Estimate differs significantly (P < .001) from group of children with ≥ 3 indicators.
Measured using a shortened version of the Center for Epidemiological Studies Depression Scale.
Overall, caregivers were mostly female (range 90.2%–94.2%), had a mean age of 35 years (34.5–35.3 years), and were the biological mother of the child (88.4%–90.4%). Caregivers of children with the most complex health problems were most likely to be divorced, widowed, or separated at baseline (healthy: 9.2%; 3 or more indicators: 17.5%). Differences in educational attainment between groups were small (overall χ2 (9) = 19.80; P = .02). An overall effect of income (χ2 (3) = 15.50; df = 1; P < .001) stemmed largely from those in the 3 or more indicators group reporting lower income than did caregivers in the other groups. Caregivers of children with more complex health problems were less likely to report excellent or very good health themselves (overall χ2 (3) = 100.20; P < .001) and reported more depressive symptoms (F (3, 9180) = 63.96; P < .001).
We reported parameter estimates (b) from the final growth-curve models for depressive symptoms (Table 3), and we reported parameter estimates and associated odds ratios (ORs) for self-reported health (Table 4). Estimates across our 4 child health complexity groups (b range = 0.47–2.73 for depressive symptoms; OR range = 0.34–0.69 for self-reported health) showed that baseline depressive symptoms increased with increasing child health complexity, and baseline self-reported health decreased with increasing child health complexity, after we controlled for all other factors in the models.
TABLE 3.
Parameter Estimates From Final Model of Caregiver Depressive Symptoms: National Longitudinal Survey of Children and Youth, Canada, 1994–2005
| b (SE) | |
| Baseline effects | |
| Intercept | 3.92* (0.14) |
| Caregiving status | |
| Healthy children (Ref) | 0.00 |
| Children with 1 indicator | 0.47* (0.10) |
| Children with 2 indicators | 0.75* (0.13) |
| Children with ≥ 3 indicators | 2.73* (0.20) |
| Male caregiver | –0.63* (0.18) |
| Caregiver age (centered at 35 y) | –0.04* (0.01) |
| Caregivers’ highest educational attainment | |
| < high school | 1.51* (0.15) |
| High school graduate (Ref) | 0.00 |
| Some postsecondary | 0.38* (0.13) |
| Postsecondary degree | −0.04 (0.13) |
| Income-to-LICO ratioa (centered at 1.0) | |
| Overall | –0.25* (0.03) |
| Caregivers of children with ≥ 3 indicatorsb | –0.37* (0.11) |
| Marital statusa | |
| Single, never married | 1.98* (0.15) |
| Married, including common-law (Ref) | 0.00 |
| Divorced, separated, or widowedb | 2.89* (0.15) |
| Male child | −0.08 (0.09) |
| Child age, y | |
| 4–6 | −0.12 (0.11) |
| 7–9 (Ref) | 0.00 |
| 10–11 | −0.04 (0.12) |
| Child is only childa | 0.18 (0.09) |
| Rate of change | |
| Linear | |
| Overall | –0.14* (0.06) |
| Divorced, separated, or widowedb | –0.26* (0.07) |
| Quadratic | 0.001 (0.01) |
| Random effects | |
| Level 1: within person | 15.56* (0.22) |
| Level 2: between person | |
| In initial status | 11.58* (0.43) |
| In linear rate of change | 1.86* (0.38) |
| In quadratic rate of change | 0.06* (0.02) |
Note. LICO = low-income cut-off, an indicator of low income based on family size and before-tax percentage of income spent on necessities.
Covariate is time-varying; all other covariates are fixed at baseline values.
Term has a significant interaction with at least 1 caregiver group.
Estimates indicate values that are significantly different (P < .05) from zero.
TABLE 4.
Parameter Estimates From Final Model of Caregiver Self-Reported Health (excellent/very good vs good/fair/poor): National Longitudinal Survey of Children and Youth, Canada, 1994–2005
| b (SE) | OR | |
| Baseline effects | ||
| Intercept | 1.67* (0.09) | |
| Caregiving status | ||
| Caregivers of healthy children (Ref) | 0.00 | 1.00 |
| Caregivers of children with 1 indicator | –0.36* (0.07) | 0.69* |
| Caregivers of children with 2 indicators | –0.56* (0.08) | 0.57* |
| Caregivers of children with ≥ 3 indicators | –1.07* (0.11) | 0.34* |
| Male caregiver | –0.40* (0.11) | 0.67* |
| Caregiver age (centered at 35 y) | -0.01 (0.01) | 0.99 |
| Caregivers’ highest educational attainment | ||
| < high school | –0.86* (0.09) | 0.42* |
| High school graduate (Ref) | 0.00 | 1.00 |
| Some postsecondary | 0.01 (0.08) | 1.01 |
| Postsecondary degree | 0.20* (0.08) | 1.22* |
| Income-to-LICO ratioa (centered at 1.0) | 0.29* (0.03) | 1.34* |
| Marital statusa | ||
| Single, never married | –0.46* (0.09) | 0.63* |
| Married, including common-law (Ref) | 0.00 | 1.00 |
| Divorced, separated, widowed | –0.16* (0.07) | 0.85* |
| Male child | –0.11* (0.06) | 0.90* |
| Child's age, y | ||
| 4–6 | –0.22* (0.07) | 0.80* |
| 7–9 (Ref) | 0.00 | 1.00 |
| 10–11 | 0.02 (0.07) | 1.02 |
| Child is only childa | –0.37* (0.06) | 0.69* |
| Rate of change | ||
| Linear | –0.18* (0.02) | 0.84* |
| Income-to-LICO ratio (centered at 1.0)ab | –0.03* (0.01) | |
| Caregivers of children aged 4–6 y with ≥ 3 indicatorsb | –0.14* (0.06) | |
| Random effects | ||
| Level 2: between person | ||
| In initial status | 3.35* (0.14) | |
| In linear rate of change | 0.06* (0.01) | |
Note. Note. LICO = low-income cut-off, an indicator of low income based on family size and before-tax percentage of income spent on necessities; OR = odds ratio.
Covariate is time-varying; all other covariates are fixed at baseline values.
Term has a significant interaction with at least 1 caregiver group.
Estimates indicate values that are significantly different (P < .05) from zero.
We also found significant associations at baseline for several caregiver characteristics. Male caregivers had lower depression scores (b = −0.63) and poorer general health (OR = 0.67) than did female caregivers. Caregivers with less than a high school education reported more depressive symptoms (b = 1.51) and worse self-reported health (OR = 0.42) than did high school graduates. Higher income levels were associated with fewer depressive symptoms (b = −0.25) and better self-reported health (OR = 1.34). Both divorced/separated/widowed and single caregivers reported more depressive symptoms (b = 2.89 and b = 1.98, respectively) and worse self-reported health (OR = 0.63 and OR = 0.85, respectively) than did married caregivers. Finally, we found significant associations for child age, gender, and only-child status for self-reported health: caregivers of boys (OR = 0.90), young children aged 4 to 6 years (OR = 0.80), and only children (OR = 0.69) reported poorer overall health than did other caregivers.
Parameter estimates for rate of change indicated that there were significant decreases over time in both depressive symptoms and self-rated health. The decrease in depressive symptoms was slight (a decrease of 0.14 units out of 36 every 2 years), whereas the decrease in self-reported health was steeper (OR = 0.84). Rate of change in depressive symptoms varied according to marital status, with caregivers who were divorced, separated, or widowed having a greater decrease in depressive symptoms over time than did caregivers who were married. The rate of change in self-reported health varied according to income, such that caregivers with higher income showed a steeper decline in self-reported excellent or very good health than did caregivers at lower income levels.
The effect of most covariates was similar across caregiver groups. However, in the depressive symptoms model, the effect of income on baseline depressive symptoms differed for caregivers of children with 3 or more indicators (b = −0.37), indicating that income had a greater impact on reducing baseline depressive symptoms among caregivers of children with 3 or more indicators than it did among caregivers of healthy children. In the self-reported health model, the effect of the child's age (4–6 vs 7–9 years) differed for caregivers of children with 3 or more indicators (b = −0.14), indicating that there was a sharper decline in self-reported health for caregivers of children with 3 or more indicators who were aged 4–6 years at baseline than there was for other caregivers.
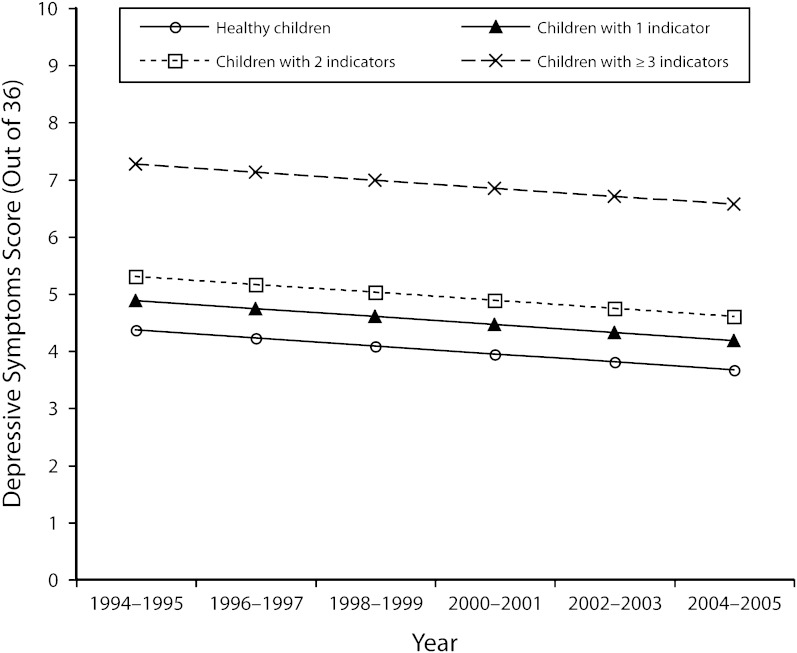
Figure 1 summarizes the effect of child health complexity on predicted depression scores on the basis of growth-curve model estimates and caregivers’ average descriptive profiles at baseline. After we controlled for all covariates, all 4 groups showed slight but significant decreases in depression scores (i.e., improvements in psychological health) over the follow-up period, a rate of decrease that was parallel for all groups. Caregivers of children with 3 or more indicators had significantly more depressive symptoms across the entire follow-up period than did caregivers of children in other indicator groups.
FIGURE 1.
Depressive symptoms scores for caregivers of children with health problems and caregivers of healthy children: National Longitudinal Survey of Children and Youth, Canada, 1994–2005.
Note. Model estimates derived from growth-curve analyses that included covariates for children's health indicators, age, gender, and only-child status, and for caregivers’ age, gender, education, income, and marital status.
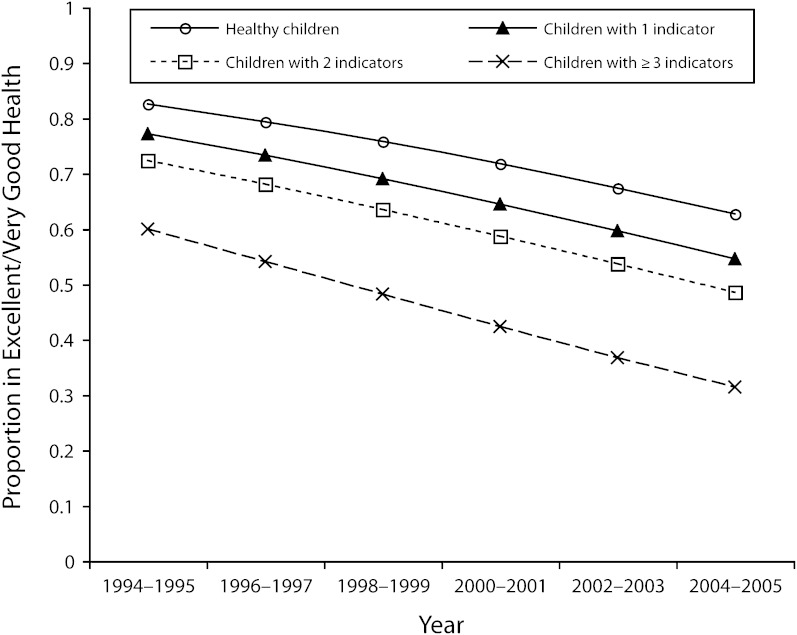
Figure 2 shows the effect of child health complexity on general health scores. The percentage of caregivers reporting excellent or very good health decreased by at least 20% across the 10-year time period, a rate of change that was consistent for all 4 groups. Caregivers of children with the most complex health problems were 15% to 20% less likely to report excellent or very good health across the entire time window compared with caregivers of children in all other groups.
FIGURE 2.
Self-reported health of caregivers of children with health problems and caregivers of healthy children: National Longitudinal Survey of Children and Youth, Canada, 1994–2005.
Note. Model estimates derived from growth-curve analyses including covariates for children's health indicators, age, gender, and only-child status, and for caregivers’ age, gender, education, income, and marital status.
DISCUSSION
We used a large-scale, population-based sample of caregivers to examine how varying degrees of child health problems affected caregiver health over time. Decrements in self-reported caregiver health were associated with child health complexity over the entire 10-year span of the study. Furthermore, caregivers of children with more complex health problems reported poorer general health and more depressive symptoms than did caregivers of children with less complex health problems who in turn reported poorer health and more depressive symptoms than did caregivers of healthy children. These results support the notion that, on a population-based scale, caregiver health is affected by both the presence of children's health problems and the complexity of those problems. These findings contrast sharply with hypotheses that caregiver health effects are short-lived and thus decrease over time and with hypotheses that caregiver health effects may increase over time because of caregiver wear and tear.2,25,26 Instead, caregiver health decrements associated with complexity of children's health problems were maintained over many years. On a population level, caregiver health decrements are probably best thought of as a relatively constant effect over time.
Although our findings suggest that the relationship between complexity and caregiver health remains consistent over time, results also indicate significant differences in the trajectories of caregiver health at the individual level (i.e., there were significant random effects). Changes in caregiver health associated with significant life events (e.g., diagnosis of the child, birth of other children) might be expected to affect caregiver health transiently. Because this analysis observed the cohort over a fixed period of time and collected data every 2 years, we could not examine these individual and time-specific events in any detail. Important fluctuations in caregiver health over time according to individual life events may well exist, but detailed examination of such effects was beyond the scope of our study and would be better served by other study designs.
Comparing results from our 2 primary outcomes (depressive symptoms and overall self-reported health, Table 3 and Table 4) is instructive. First, the direction of effect over time is inconsistent; psychological health appears to improve over time, whereas self-reported health worsens. Interestingly, both patterns are consistent with epidemiological studies of the general population,44,45 perhaps suggesting that caregiver groups do not differ importantly from the larger population in the rate of change in their health but instead differ primarily in overall level of health. Second, although both outcomes show statistically significant effects of complexity, the difference in depressive symptoms between the most extreme groups is a modest 2 to 3 points on a 36-point scale, whereas for self-reported health the difference is 20% to 25% in the reported prevalence of excellent or very good health. Both results support a single explanation: child health complexity has relatively little effect on the rate of change over time.
Our results show an association between child health complexity and caregiver health, but we cannot assess whether the stress of caregiving is the primary cause of poorer caregiver health or whether other unmeasured variables are involved. For example, recent work36,46,47 examining population-level data on elderly caregivers has shown that an important distinction may exist between the burden of caregiving and the stress associated with seeing a loved one suffering. When these 2 constructs are separated, more caregiving can be associated with better health and reduced mortality, findings consistent with other demonstrations of positive consequences of caregiving.29,31,33–36,48 Furthermore, we cannot assess which components of child health complexity (e.g., health status, presence of behavior problems) cause these changes in caregiver health. Future work could examine whether such distinctions can improve on existing models of the relationships underlying the health of caregivers of children with disabilities.38
Limitations
Some limitations of our study warrant consideration. First, although our sample of child–caregiver pairs was drawn from a large population-based study and included an extensive range of child health problems and caregiving situations, the sample is not representative of all Canadian caregivers. The NLSCY was designed as a nationally representative sample of children, not caregivers. In addition, by limiting our sample to 1 child per caregiver and to a specific child age range, we may have introduced bias that led to higher rates of caregiver income, education, and 2-parent households compared with national norms.49 Whether such a bias would substantially affect our findings is unknown, although an affluence bias might suggest that the true complexity effects are underestimated in our study.
Second, the measures used in the NLSCY were derived from parental reports that may not accurately reflect child health problems. There is also an issue of shared method variance, wherein parents who report poor health in their children may be more likely to report poor health for themselves. However, parent reports have been shown to be relatively reliable for a variety of severe health conditions.50–53
Third, although our growth-curve model examined both fixed and random effects, the latter were limited to only intercept and rate-of-change components. We made this analytic decision on the basis of modeling and convergence constraints. However, it is conceivable that other covariates in the model would have also exhibited random effects if they had been examined. For example, our caregiver groups represent heterogeneous caregiving and child health situations. Including these as fixed covariates in the model precluded the identification of significant between-individual differences within the caregiver groups.
Finally, our definition of child health problem complexity included the consequences of child illness (e.g., use of health services) rather than specific child health conditions. This approach allowed caregivers experiencing very diverse caregiving situations to be grouped together in our analyses, which may have masked differences among specific caregiving situations. This approach is garnering support in the caregiver literature because information based on such broad categorizations may be more useful in high-level policy decisions. However, future work comparing caregiving subgroups should better clarify models of caregiver health. For example, children with externalizing behavior problems in addition to other health conditions may have a particular impact on caregiver health.9,54,55
Conclusions
We found clear evidence of poorer overall self-reported health and more depressive symptoms among caregivers of children with health problems, an effect that persisted over the study period of 10 years. Furthermore, the caregiver health effect increased with increasing complexity of the child health problems: caregivers of children with more complex disorders reported their own health as incrementally poorer. These findings show that poorer health among caregivers of children with health problems was not transient but lasted many years, and that the risk to caregiver health increased with increasing complexity of children's health problems. The interwoven nature of child and family health is becoming increasingly apparent and deserves further exploration. Increased awareness of these patterns may lead providers and policymakers to a better understanding of how to serve these families.
Acknowledgments
This project was funded by the Canadian Institutes of Health Research (grant MOP-77620).
We thank Kelly Carroll and Dr. Rubab Arim for contributions to article development and 3 anonymous reviewers for their helpful comments.
Human Participant Protection
The Ottawa Hospital Research Ethics Board approved the study protocol.
References
- 1.Breslau N, Staruch K, Mortimer E. Psychological distress in mothers of disabled children. Am J Dis Child. 1982;136(8):682–686. [DOI] [PubMed] [Google Scholar]
- 2.Gowen J, Johnson-Martin N, Goldman B, Appelbaum M. Feelings of depression and parenting competence of mothers of handicapped and nonhandicapped infants: a longitudinal study. Am J Ment Retard. 1989;94(3):259–271. [PubMed] [Google Scholar]
- 3.Smyth-Staruch K, Breslau N, Weitzman M, Gortmaker S. Use of health services by chronically ill and disabled children. Med Care. 1984;22(4):310–328. [DOI] [PubMed] [Google Scholar]
- 4.Ireys HT, Anderson G, Shaffer T, Neff J. Expenditures for care of children with chronic illnesses enrolled in Washington State Medicaid program, fiscal year 1993. Pediatrics. 1997;100(2 pt 1):197–204. [DOI] [PubMed] [Google Scholar]
- 5.Burton P, Phipps S. Economic costs of caring for children with disabilities in Canada. Can Public Policy. 2009;35(3):269–290. [Google Scholar]
- 6.Damiani G, Rosenbaum P, Swinton M, Russell D. Frequency and determinants of formal respite service use among caregivers of children with cerebral palsy in Ontario. Child Care Health Dev. 2004;30(1):77–86. [DOI] [PubMed] [Google Scholar]
- 7.The Health of Canada's Children: A CICH Profile. 3rd ed Ottawa, Ontario, Canada: Canadian Institute of Child Health; 2000. [Google Scholar]
- 8.Irwin S, Lero D. In Our Way: Child Care Barriers to Full Workforce Participation Experienced by Parents of Young Children With Special Needs—and Potential Remedies. Cape Breton, Nova Scotia, Canada: Breton Books; 1997. [Google Scholar]
- 9.Brehaut JC, Kohen DE, Raina P, et al. The health of primary caregivers of children with cerebral palsy: how does it compare with that of other Canadian caregivers? Pediatrics. 2004;114(2):e182–e191. [DOI] [PubMed] [Google Scholar]
- 10.Parish SL, Cloud JM. Financial well-being of young children with disabilities and their families. Soc Work. 2006;51(3):223–232. [DOI] [PubMed] [Google Scholar]
- 11.Dumas J, Péron Y. Marriage and Conjugal Life in Canada. Ottawa, Ontario: Statistics Canada, Demography Division; 1992. Catalogue 91-543E. [Google Scholar]
- 12.Eicher PS, Batshaw ML. Cerebral palsy. Pediatr Clin North Am. 1993;40(3):537–551. [DOI] [PubMed] [Google Scholar]
- 13.Family Support for Children with Disabilities Act, Statutes of Alberta chapter F-5.3 (2004).
- 14.Rosenbaum P, King S, Law M, Evans JS. Family-centered service: a conceptual framework and research review. Phys Occup Ther Pediatr. 1998;18(1):1–20. [Google Scholar]
- 15.Schulz R, Beach S. Caregiving as a risk factor for mortality: the Caregiver Health Effects study. JAMA. 1999;282(23):2215–2219. [DOI] [PubMed] [Google Scholar]
- 16.Chappell N. Social Support and Aging. Toronto, Ontario: Butterworths; 1992. [Google Scholar]
- 17.Beckman PJ. Influence of selected child characteristics on stress in families of handicapped infants. Am J Ment Defic. 1983;88(2):150–156. [PubMed] [Google Scholar]
- 18.McKinney B, Peterson R. Predictors of stress in parents of developmentally disabled children. J Pediatr Psychol. 1987;12(1):133–150. [DOI] [PubMed] [Google Scholar]
- 19.Dyson L, Edgar K, Crnic K. Psychological predictors of adjustment by siblings of developmentally disabled children. Am J Ment Retard. 1989;94(3):292–302. [PubMed] [Google Scholar]
- 20.Frey KS, Greenberg MT, Fewell RR. Stress and coping among parents of handicapped children: a multidimensional approach. Am J Ment Retard. 1989;94(3):240–249. [PubMed] [Google Scholar]
- 21.Brehaut JC, Kohen DE, Garner RE, et al. Health among caregivers of children with health problems: findings from a Canadian population-based study. Am J Public Health. 2009;99(7):1254–1262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Goode KT, Haley W, Roth D, Ford G. Predicting longitudinal changes in caregiver physical and mental health: a stress process model. Health Psychol. 1998;17(2):190–198. [DOI] [PubMed] [Google Scholar]
- 23.Haley WE, Levine EG, Brown SL, Bartolucci AA. Stress, appraisal, coping, and social support as predictors of adaptational outcome among dementia caregivers. Psychol Aging. 1987;2(4):323–330. [DOI] [PubMed] [Google Scholar]
- 24.Haley WE, Roth DL, Coleton MI, et al. Appraisal, coping, and social support as mediators of well-being in Black and White family caregivers of patients with Alzheimer's disease. J Consult Clin Psychol. 1996;64(1):121–129. [DOI] [PubMed] [Google Scholar]
- 25.Magni G, Carli M, De Leo D, Tshilolo M, Zanesco L. Longitudinal evaluations of psychological distress in parents of children with malignancies. Acta Paediatr Scand. 1986;75(2):283–288. [DOI] [PubMed] [Google Scholar]
- 26.Seltzer MM, Greenberg JS, Floyd FJ, Pettee Y, Hong J. Life course impacts of parenting a child with a disability. Am J Ment Retard. 2001;106(3):265–286. [DOI] [PubMed] [Google Scholar]
- 27.Schulz RH, Williamson GA. 2-year longitudinal study of depression among Alzheimer's caregivers. Psychol Aging. 1991;6(4):569–578. [DOI] [PubMed] [Google Scholar]
- 28.Vitaliano PP, Russo J, Young HM, Teri L, Maiuro RD. Predictors of burden in spouse caregivers of individuals with Alzheimer's disease. Psychol Aging. 1991;6(3):392–402. [DOI] [PubMed] [Google Scholar]
- 29.Dahlquist LM, Czyzewski DI, Jones CL. Parents of children with cancer: a longitudinal study of emotional distress, coping style, and marital adjustment two and twenty months after diagnosis. J Pediatr Psychol. 1996;21(4):541–554. [DOI] [PubMed] [Google Scholar]
- 30.Sawyer M, Antoniou G, Toogood I, Rice M, Baghurst P. Childhood cancer: a 4-year prospective study of the psychological adjustment of children and parents. J Pediatr Hematol Oncol. 2000;22(3):214–220. [DOI] [PubMed] [Google Scholar]
- 31.Northam E, Anderson P, Adler R, Werther G, Warne G. Psychosocial and family functioning in children with insulin-dependent diabetes at diagnosis and one year later. J Pediatr Psychol. 1996;21(5):699–717. [DOI] [PubMed] [Google Scholar]
- 32.Beach SR, Schulz R, Yee J, Jackson S. Negative and positive health effects of caring for a disabled spouse: longitudinal findings from the caregiver health effects study. Psychol Aging. 2000;15(2):259–271. [DOI] [PubMed] [Google Scholar]
- 33.Lawton M, Brody EM, Saperstein AR. Respite for Caregivers of Alzheimer's Patients: Research and Practice. New York, NY: Springer; 1991. [Google Scholar]
- 34.Cohen CA, Colantonio A, Vernich L. Positive aspects of caregiving: rounding out the caregiver experience. Int J Geriatr Psychiatry. 2002;17(2):184–188. [DOI] [PubMed] [Google Scholar]
- 35.Kramer B. Gain in the caregiving experience: where are we? What next? Gerontologist. 2005;37(2):218–232. [DOI] [PubMed] [Google Scholar]
- 36.Brown SL, Smith DM, Schulz R, et al. Caregiving behavior is associated with decreased mortality risk. Psychol Sci. 2009;20(4):488–494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Statistics Canada, Human Resources Development Canada. National Longitudinal Survey of Children: Overview of Survey Instruments for 1994–1995 Data Collection, Cycle 1. Ottawa, Ontario, Canada: Statistics Canada; 1995. [Google Scholar]
- 38.Raina P, O'Donnell M, Schwellnuss H, et al. Caregiving process and caregiver burden: conceptual models to guide research and practice. BMC Pediatr. 2004;4:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kopec JA, Williams JI, To T, Austin PC. Measuring population health: correlates of the Health Utilities Index among English and French Canadians. Can J Public Health. 2000;91(6):465–470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Bethell CD, Read D, Stein RE, Blumberg SJ, Wells N, Newacheck PW. Identifying children with special health care needs: development and evaluation of a short screening instrument. Ambul Pediatr. 2002;2(1):38–48. [DOI] [PubMed] [Google Scholar]
- 41.Kohen DE, Brehaut JC, Garner RE, et al. Conceptualizing childhood health problems using survey data: a comparison of key indicators. BMC Pediatr. 2007;7:40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Radloff LS. The CES-D scale: a self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1(3):385–401. [Google Scholar]
- 43.Poulin C, Hand D, Boudreau B. Validity of a 12-item version of the CES-D used in the National Longitudinal Survey of Children and Youth. Chronic Dis Can. 2005;26(2–3):65–72. [PubMed] [Google Scholar]
- 44.Jones CJ, Livson N, Peskin H. Paths of psychological health: examination of 40-year trajectories from the intergenerational studies. J Res Pers. 2006;40(1):56–72. [Google Scholar]
- 45.Hopman W, Towheed T, Anastassiades T, et al. Canadian normative data for the SF-36 health survey. The Canadian Multicentre Osteoporosis Study Research Group. CMAJ. 2000;163(3):265–271. [PMC free article] [PubMed] [Google Scholar]
- 46.Schulz R, Hebert RS, Dew MA, et al. Patient suffering and caregiver compassion: new opportunities for research, practice, and policy. Gerontologist. 2007;47(1):4–13. [DOI] [PubMed] [Google Scholar]
- 47.Amirkhanyan AA, Wolf DA. Caregiver stress and noncaregiver stress: exploring the pathways of psychiatric morbidity. Gerontologist. 2003;43(6):817–827. [DOI] [PubMed] [Google Scholar]
- 48.Beach C, Croskerry P, Shapiro M. Profiles in patient safety: emergency care transitions. Acad Emerg Med. 2003;10(4):364–367. [DOI] [PubMed] [Google Scholar]
- 49.Ferguson JH. National Institutes of Health Concensus Development Conference Statement: diagnosis and treatment of attention-deficit/hyperactivity disorder (ADHD). J Am Acad Child Adolesc Psychiatry. 2000;39(2):182–193. [DOI] [PubMed] [Google Scholar]
- 50.Harlow SD, Linet MS. Agreement between questionnaire data and medical records: the evidence for accuracy of recall. Am J Epidemiol. 1989;129(2):233–248. [DOI] [PubMed] [Google Scholar]
- 51.Heliovaara M, Aromaa A, Klaukka T, Knekt P, Joukamaa M, Impivaara O. Reliability and validity of interview data on chronic diseases: the Mini-Finland Health Survey. J Clin Epidemiol. 1993;46(2):181–191. [DOI] [PubMed] [Google Scholar]
- 52.Russell KMW, Hudson M, Long A, Phipps S. Assessment of health-related quality of life in children with cancer: consistency and agreement between parent and child reports. Cancer. 2006;106(10):2267–2274. [DOI] [PubMed] [Google Scholar]
- 53.Varni JW, Limbers CA, Burwinkle TM. Parent proxy-report of their children's health-related quality of life: an analysis of 13 878 parents’ reliability and validity across age subgroups using the PedsQLTM 4.0 Generic Core Scales. Health Qual Life Outcomes. 2007;5:2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.King G, King S, Rosenbaum P, Goffin R. Family-centered caregiving and well-being of parents of children with disabilities: linking process with outcome. J Pediatr Psychol. 1999;24(1):41–53. [Google Scholar]
- 55.Lach LM, Kohen D, Garner RE, et al. The health and psychosocial functioning of caregivers of children with neurodevelopmental disorders. Disabil Rehabil. 2009;31(8):607–618. [DOI] [PubMed] [Google Scholar]