Abstract
Pain and depression are the most prevalent physical and psychological symptom-based disorders, respectively, and co-occur 30–50% of the time. However, their reciprocal relationship and potentially causative effects on one another have been inadequately studied. Longitudinal data analysis involving 500 primary care patients with persistent back, hip or knee pain were enrolled in the Stepped Care for Affective Disorders and Musculoskeletal Pain (SCAMP) study. Half of the participants had comorbid depression and were randomized to a stepped care intervention (n = 123) or treatment as usual (n = 127). Another 250 nondepressed patients with similar pain were followed in a parallel cohort. Outcomes were assessed at baseline, 3, 6, and 12 months. Mixed effects model repeated measures (MMRM) multivariable analyses were conducted to determine if change in pain severity predicted subsequent depression severity, and vice-versa. Change in pain was a strong predictor of subsequent depression severity (t-value = 6.63, p < .0001). Likewise, change in depression severity was an equally strong predictor of subsequent pain severity (t-value = 7.28, p < .0001). Results from the full cohort were similar in the clinical trial subgroup. In summary, pain and depression have strong and similar effects on one another when assessed longitudinally over 12 months.
Keywords: pain, depression, causation, prognosis, primary care, longitudinal
Introduction
Pain and depression are the most common physical and psychological symptom-based conditions, respectively, with co-occurrence rates of 30–50%.4,26,40 Moreover, the comorbidity of these two common and frequently chronic conditions has an additive adverse impact on quality of life, disability, and response to treatment.2,8,12,20,25,42 While the intimate linkage between pain and depression is well-established, the cause-effect relationship between these two pervasive conditions and its directionality is still being defined. A literature synthesis published in 1997 found greater evidence for depression being a consequence of pain rather than an antecedent.13 However, many of the studies available at that time were cross-sectional.
Several longitudinal studies published in the past decade have provided suggestive evidence for adverse influences of pain and depression on one other.5,14,15,17,39,49 However, only 3 studies15,17,49 have been conducted in actual patient samples, which are the most clinically relevant group; while pain is highly prevalent in the general population, only a subset of individuals are bothered enough to seek health care for their pain. Moreover, only one clinical17 and two community-based studies14,16 used multiple follow-up assessments of pain and depression with repeated measures analysis which is a more appropriate method for establishing longitudinal associations. Establishing whether antecedent severity or change of an independent variable predicts the subsequent level of a dependent/outcome variable is a particularly important step in moving beyond mere association towards a potentially cause-effect relationship. In this paper, we analyze data from 500 patients enrolled in the Stepped Care for Affective disorders and Musculoskeletal Pain (SCAMP) study.27 SCAMP included 250 primary care patients with chronic musculoskeletal pain and comorbid depression enrolled in a clinical trial and an additional 250 patients with similar pain but no depression. Our hypothesis is that over 12 months pain and depression will exhibit predictable influences on one other. Specifically, we postulate that changes in pain severity at an earlier time point predicts subsequent depression severity as well as the converse, i.e., changes in depression severity at an earlier time point predict subsequent pain severity.
Methods
Participant Enrollment
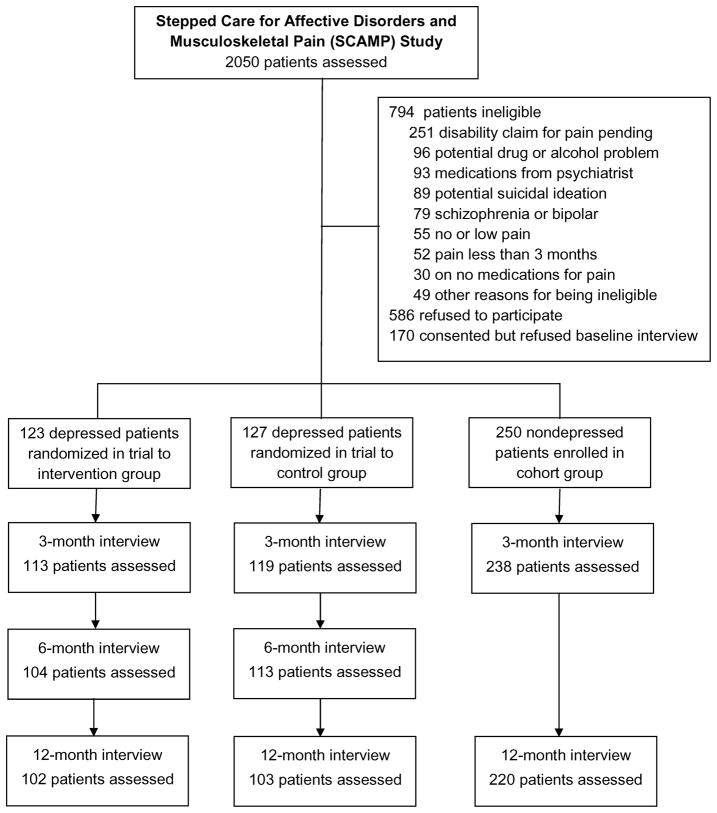
Details of the SCAMP study have been previously described.27 Figure 1 outlines the participant enrollment and follow-up in SCAMP. Briefly, a total of 500 patients with chronic musculoskeletal pain were enrolled and followed for 12 months. Patients were recruited from two primary care clinical systems in Indianapolis: the Indiana University Medical Group Primary Care system (6 community-based clinical sites were used) and the Richard L Roudebush Veterans Administration Medical Center 5 general medicine clinics. Recruitment occurred from January 2005 to June 2007 and follow-up concluded in June 2008. The 250 patients with comorbid depression participated in a randomized clinical trial of optimized antidepressant therapy and pain self-management, the results of which have been previously published.23 All 500 subjects underwent identical outcome assessments at baseline, 3 and 12 months by research assistants blinded to study arm. All subjects provided written consent, and the study was approved by the Indiana University Institutional Review Board.
Figure 1.
Flowchart of participants in the SCAMP trial. The reasons for patients not being assessed at 3-, 6-, and 12-month follow-up interviews included dropping out from the study, being unavailable for interviews, or being lost to follow-up.
To be eligible, patients had to have pain: (a) located in the low back, hip or knee; (b) persistent for 3 months or longer despite conventional analgesic treatment, defined as prior use of at least two different analgesics; and (c) at least moderate in severity, defined as a Brief Pain Inventory score of 5 or greater.6,50 Patients were classified as depressed if they had a PHQ-9 score ≥10 and endorsed depressed mood and/or anhedonia. More than 90% of patients fulfilling this PHQ-9 criterion have major depression or dysthymia, and the remaining patients have clinically significant depression with substantial functional impairment.30,29 Patients were classified as nondepressed if they had a PHQ-9 score ≤ 7. Those with scores of 8 or 9 were not enrolled in the study in order to create clearer separation from the depressed (PHQ-9 ≥ 10) and nondepressed (PHQ-9 ≤ 7) groups.
Outcome Measures
All baseline and follow-up outcome assessments were conducted by a research assistant blinded to group assignment and patient’s depression status. Pain severity was assessed with the Graded Chronic Pain Scale (GCPS), which ranges from 0 to 100, with scores of 40 to 60 representing moderate pain and 70 or greater severe pain.46 Depression severity was assessed, as a primary outcome, with the 20-item Hopkins Symptom Checklist (HSCL-20) which has established sensitivity to change36 and is widely used in effectiveness trials of depression in primary care.10,19,30,45,47 Depression diagnoses were established with the PRIME-MD, which categorizes individuals into 3 DSM-IV diagnostic subgroups: major depression, dysthymia, and other depression.43
Analysis
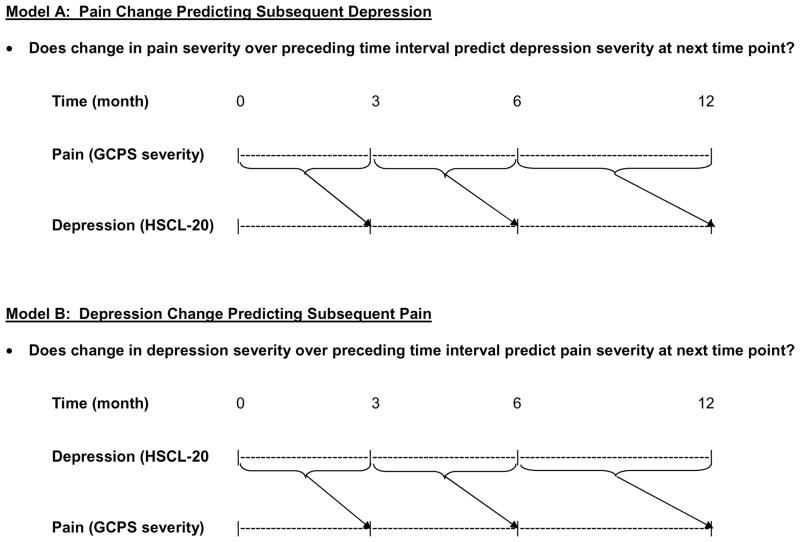
We postulated that change in pain severity would predict subsequent depression severity, and that change in depression severity would predict subsequent pain severity. Thus, we ran two models: the first in which a preceding change in pain severity was the predictor variable and subsequent depression severity the outcome variable, and the second in which a preceding change in depression severity was the predictor variable and subsequent pain severity the outcome variable (Figure 2) Each model was run in 3 steps: 1) unadjusted (i.e., predictor variable only); 2) adjusted for the covariates of age, sex, race, pain location (back vs. hip/knee), study site (university vs. VA clinics), and time in months since baseline assessment; and 3) fully adjusted for covariates plus the baseline value of the outcome variable. We used multivariable mixed effects models for repeated measures (MMRM) to assess the longitudinal relationship between pain and depression as well as time (i.e., timepoints of 0, 3, 6, and 12 months). Unlike traditional regression models, MMRM is able to accommodate the correlation structure among outcomes measured within the same subject. MMRM allows repeated measures from the same subject to share a common random effect. Thus, MMRM may represent a better fit model than the population-averaged models such as generalized estimating equations (GEE) analysis.
Figure 2.
Longitudinal analysis framework for examining whether change in pain severity predicts subsequent depression severity (Model A) and whether change in depression severity predicts subsequent pain severity (Model B).
The sample for our primary analysis comprised the full sample of 500 subjects. To test the robustness of our results, we also ran secondary models with the clinical trial group (n = 250) and the nondepressed cohort (n = 250) as well as the intervention (n = 123) and control (n = 127) arms of the clinical trial. The primary analysis conducted in the full sample used 3 time points in the models since the 250 nondepressed patients had assessments at baseline, 3, and 12 months. The secondary analyses conducted in the clinical trial group and its two treatment arms used 4 timepoints since the trial had the relevant pain and depression assessments at baseline, 3, 6, and 12 months. The magnitude of reciprocal effects between pain and depression were expressed as standardized effect sizes.21 The effect size was calculated as the amount of change in the dependent variable (e.g., subsequent depression severity) predicted by a particular unit of change in the predictor variable (e.g., antecedent change in pain severity) divided by the standard deviation at baseline of the outcome variable. Analyses were performed using SAS Version 9.1 (SAS Institute, Cary, North Carolina).
Results
Study Participants
The mean age of the study sample was 59 years; 52% were women; 58% were white, 38% black, and 4% other (Table 1). Regarding education, 27% had less than a high school education, 36% had completed high school only, and 37% had completed at least some college or trade school. The site of pain was the back in 55% of subjects and the hip or knee in 45%. The university clinics accounted for 60% of enrollment and the VA clinics for 40%. Pain severity was moderately severe as indicated by a GCPS pain severity score of 69.1 (on this scale, 40 to 60 represents moderate pain and 70 to 100 represents severe pain). By design, SCL-20 scores were significantly higher in the 250 depressed patients, with their mean score of 1.89 representing a moderately severe level of depression. Among the 250 depressed subjects, 74.8% met DSM-IV criteria for major depression, 20.8% for dysthymia only, and 4.4% for minor depression.
Table 1.
Characteristics of the 500 Subjects Enrolled in SCAMP Study
| Characteristic | Depressed Intervention Arm (N=123) | Depressed Control Arm (N=127) | Non- depressed (N=250) |
|---|---|---|---|
| Age, mean (SD) age, yr | 55.2 (12.6) | 55.8 (11.0) | 62.5 (14.1) |
| Women, n (%) | 69 (56) | 63 (50) | 127 (51) |
| Race, n (%) | |||
| White | 75 (61) | 76 (60) | 140 (56) |
| Black | 42 (34) | 49 (39) | 100 (40) |
| Other | 6 (5) | 2 (2) | 10 (4) |
| Education, n (%) | |||
| Less than high school | 28 (23) | 32 (25) | 65 (26) |
| High school | 54 (44) | 48 (38) | 78 (31) |
| At least some college or trade school | 41 (33) | 46 (37) | 107 (43) |
| Married, n (%) | 48 (39) | 44 (35) | 97 (39) |
| Clinical site, n (%) | |||
| University clinics | 73 (59) | 75 (59) | 152 (61) |
| Veteran Administration (VA) | 50 (41) | 52 (41) | 98 (39) |
| Pain location, n (%) | |||
| Back | 76 (62) | 75 (59) | 126 (51) |
| Hip or knee | 47 (38) | 52 (41) | 122 (49) |
| Median duration of pain, yr | 8 | 10 | 10 |
| Mean (SD) no. of medical diseases | 2.74 (1.56) | 2.65 (1.42) | 2.62 (1.39) |
| Mean (SD) HSCL-20 depression severity * | |||
| Baseline | 1.83 (0.66) | 1.94 (0.65) | 0.69 (0.53) |
| 3 months † | 1.04 (0.62) | 1.74 (0.70) | 0.63 (0.47) |
| 12 months † | 1.14 (0.69) | 1.68 (0.75) | 0.80 (0.61) |
| Mean (SD) GCPS pain severity * | |||
| Baseline | 72.7 (17.6) | 72.8 (15.4) | 65.4 (16.2) |
| 3 months † | 66.9 (21.4) | 75.9 (16.7) | 68.3 (17.9) |
| 12 months † | 67.8 (25.0) | 74.7 (17.5) | 66.8 (20.0) |
HSCL-20 = Hopkins Symptom Checklist 20-item depression scale (score range, 0 to 4). GCPS = Graded Chronic Pain Scale (score range, 0 to 100)
Number of intervention, control, and nondepressed subjects evaluated was 113, 119, and 238 at 3 months, and 102, 103, and 220 at 12 months
Cross-Sectional Association between Changes in Pain and Depression
There was a moderate correlation (all P values < .0001) between change in GCPS pain severity and change in HSCL-20 depression severity from baseline to 3 months (r = .26), from 3 months to 6 months (r = .37), and from 6 months to 12 months (r = .28).
Longitudinal Association between Changes in Pain and Depression
Results of the MMRM multivariable modeling summarized in Table 2 confirm that a preceding change in pain severity was a strong predictor of subsequent depression severity and, conversely, a preceding change in depression severity was a strong predictor of subsequent pain severity. Several findings should be emphasized. First, the parameter estimates are positive, indicating that worsening in one variable predicts subsequent greater severity of the other, and improvement predicts less severity. In other words, worsening pain during a preceding time interval predicts more severe depression, and pain improvement predicts less severe depression. Likewise, depression change has a similar predictive relationship to subsequent pain. Second, antecedent changes in pain and depression had comparable effects on one another as reflected in the similar magnitude of the t-values. Third, adjusting for covariates as well as the baseline value of the outcome variable did not substantially reduce the parameter estimates. Fourth, model results from the primary analysis in the full sample of 500 subjects did not change in the secondary analyses run in the 250 clinical trial participants, the 250 nondepressed cohort participants, or the intervention (n = 123) or control (n = 127) arms of the trial. Since the intervention itself reduced pain and depression in the clinical trial,23 our similar findings for the intervention and control arms suggest that pain change and depression change predict outcomes independent of treatment group.
Table 2.
Pain Change as a Predictor of Depression and Depression Change as a Predictor of Pain over 12 Months*
| Sample | Predictor (Independent) Variable | |||||
|---|---|---|---|---|---|---|
| Model A Pain (GCPS Severity) Change [predicting depression] | Model B Depression (HSCL-20) Change [predicting pain] | |||||
| Beta | T | P | Beta | T | P | |
| Primary analysis | ||||||
| Full sample (n = 500) | ||||||
| Unadjusted | .0030 | 4.31 | < .0001 | 5.15 | 4.38 | < .0001 |
| Adjusted for covariates | .0030 | 4.40 | < .0001 | 5.33 | 4.54 | < .0001 |
| Fully adjusted for covariates + baseline value of outcome variable | .0043 | 6.62 | < .0001 | 7.23 | 6.46 | < .0001 |
| Secondary analyses | ||||||
| Clinical trial group (n = 250) | ||||||
| Unadjusted | .0045 | 5.49 | < .0001 | 5.33 | 4.89 | < .0001 |
| Adjusted for covariates | .0045 | 5.45 | < .0001 | 5.32 | 4.88 | < .0001 |
| Fully adjusted for covariates + baseline value of outcome variable | .0047 | 5.81 | < .0001 | 5.52 | 5.15 | < .0001 |
| Intervention arm in clinical trial (n = 123) | ||||||
| Fully adjusted for covariates + baseline value of outcome variable | .0035 | 3.36 | .0009 | 4.57 | 2.90 | .004 |
| Control arm in clinical trial (n = 127) | ||||||
| Fully adjusted for covariates + baseline value of outcome variable | .0063 | 4.87 | < .0001 | 6.84 | 4.74 | < .0001 |
| Nondepressed cohort group (n = 250) | ||||||
| Fully adjusted for covariates + baseline value of outcome variable | .0026 | 3.59 | .0004 | 9.50 | 4.42 | < .0001 |
Mixed effects repeated measures multivariable models examining preceding pain change as a predictor of subsequent depression (Model A), and preceding depression change as a predictor of subsequent pain (Model B). A positive coefficient means that improvement in the predictor variable is associated with reduction in the severity of the outcome variable, while worsening in the predictor variable is associated with an increase in severity of the outcome variable.
Covariates controlled for in models were age, sex, race, pain location, study site, and time in months since baseline.
Magnitude of Reciprocal Effects between Pain and Depression
The baseline SD of the HSCL-20 in the full sample is 0.845, and the baseline SD of the GCPS is 16.8. Using the parameter estimates from the full model in Table 2, an antecedent 10 point change in GCPS pain severity predicts a subsequent change in HSCL-20 depression severity of .043 (i.e., the parameter estimate of .0043 multiplied by 10). Previous research suggests that a 2 to 3 point change in pain on a 0 to 10 scale numeric rating scale represents a clinically important difference at the patient level11, which would correspond to a 20 to 30 point change on the 0 to 100 GCPS scale. Thus, a 20 to 30 change in GCPS pain severity predicts a subsequent HSCL-20 change of .086 to .129, corresponding to an effect size of .10 (.086/.0845) to .15 (.129/.845). Similar calculations show that a 0.5 antecedent change in HSCL-20 depression severity, often considered clinically significant31, predicts a subsequent GCPS change of 3.64 (i.e., the parameter estimate of 7.28 multiplied by 0.5), or effect size of .22 (3.64/16.8).
Effects of Other Covariates on Subsequent Pain and Depression Severity
Not surprisingly, all models also showed that baseline severity of the outcome variable was a strong predictor of the outcome, i.e., those with more severe pain at baseline had greater pain severity at follow-up (P < .0001) and those with more severe depression at baseline had greater depression severity at follow-up (P < .0001). What is notable is that the predictor variables (pain change and depression change) remained highly significant even after controlling for baseline severity of the outcome variable.
The time in months since the baseline assessment had an independent association with reduced pain severity in the full sample (P < .0001) as well as most subgroups including the clinical trial group (P = .001), the nondepressed cohort (P = .003), and the intervention arm (P < .001); only the control arm showed no association (P = .36). In contrast, time was independently associated with depression severity only in the full sample (P < .001) and the nondepressed cohort (P < .0001) where the passage of time was associated with increased depression severity. This is likely due to a floor effect in that those nondepressed patients who change over time are more likely to show increased scores on a depression measure since their scores were already low at baseline. Of note, the SCAMP intervention itself produced improvement in both pain and depression severity as reported in the main results from our trial;23 thus; the findings reported above are the effects of time independent of the beneficial effects related to the intervention.
Only one other covariate (clinic site) had any predictive relationship with outcomes: enrollment from the community-based clinics serving a lower socioeconomic urban population (compared to enrollment from the VA clinics) predicted worse future pain (but not depression) in the full sample model and all subgroup models except the intervention group. Neither gender, age, race, or pain location (back vs. hip/knee) were independent predictors of subsequent pain or depression severity.
Discussion
Earlier reviews had concluded that chronic pain was a risk factor for subsequent depression but were inconclusive regarding depression as a risk factor for pain.9,13 However, our study findings add to the handful of longitudinal studies which support an equal adverse influence of pain and depression on one another. At the same time, pain and depression are independent conditions, since half to two-thirds of patients suffer from one but not the other. Still, their frequent co-occurrence coupled with their adverse influences on one another strengthens the case for a coordinated approach to recognition and management.
Table 3 summarizes the previous longitudinal studies along with our current study. Four of the 8 studies assessed patients just at baseline and a single follow-up point. The other 4 studies used a repeated measures analytic strategy incorporating multiple follow-up assessment points. Three of these 4 studies confirmed the reciprocal relationship between pain and depression. Our use of MMRM analysis helps to establish within-subject associations between pain and depression, in contrast to GEE which assesses group average associations.32,34 Moreover, our examination of how antecedent change in one condition predicts subsequent severity of the other condition makes an even stronger case for a bidirectional causative relationship between pain and depression.
Table 3.
Summary of Longitudinal Studies Examining the Reciprocal Relationship between Pain and Depression
| Study | Year | Sample | N | Pain type | Other features | Duration (mo.) | Followup assessments | Pain/Depression measures | Repeated Measures Analysis* | Significant Study Findings |
|---|---|---|---|---|---|---|---|---|---|---|
| Single endpoint | ||||||||||
| Gureje 15 | 2001 | Clinical (primary care) | 3,197 | Any | 12 | 1 | Binary/Continuous | None | Current pain predicts future onset of depression. Current depression predicts future onset of pain. |
|
| Williams 49 | 2004 | Clinical (neurology) | 483 | Any | 12 | 2 | Continuous/Continuous | None | Change in pain severity predicts subsequent depression severity Change in depression severity predicts subsequent pain severity |
|
| Chou 5 | 2007 | Community | 3,654 | Any | 24 | 1 | Binary/Continuous | None | Current pain predicts future onset of depression. Current depression predicts future onset of pain. |
|
| Meyer 39 | 2007 | Community | 55,690 | Back | Age ≥ 65 | 24 | 1 | Binary/Binary | None | Current pain predicts future onset of depression. Current depression predicts future onset of pain. |
| Serial endpoints | ||||||||||
| Geerlings 14 | 2002 | Community | 652 | Any | Age ≥ 55 Half were depressed |
36 | 7 | Categorical/Continuous | GEE | Current pain level predicts subsequent depression severity Current depression severity predicts subsequent pain level Disability is not a mediator of pain-depression relationship |
| Hurwitz 17 | 2003 | Clinical (primary care) | 681 | Back | All had pain | 18 | 3 | Binary/Binary | GEE | Current pain and disability predict subsequent depression Current depression predicts subsequent pain and disability |
| Hawker16 | 2010 | Community | 529 | Hip or knee | Age ≥ 55 | 2 | 4 | 2 Continuous | Continuous/Path analysis | Current pain predicts subsequent depression through its effects on fatigue and pain-specific disability. Depression and fatigue have a strong reciprocal relationship Fatigue and pain-specific disability (but not depression) predict worse pain. |
| Kroenke | 2011 | Clinical (primary care) | 500 | Back, hip or knee | All had pain Half were depressed |
12 | 4 | Continuous/Continuous | MMRM | Change in pain severity predicts subsequent depression severity Change in depression severity predicts subsequent pain severity |
GEE = Generalized estimating equations (GEE) analysis; MMRM = mixed effects model repeated measures
One of the 4 studies with repeated measures analysis used path analysis instead of MMRM as the principal analytic strategy.16 In addition to pain and depression, fatigue and pain-specific disability were also entered into the path analysis. The conclusions from this study were more nuanced. First, pain did predict subsequent depression but these effects appeared to be mediated through fatigue and pain-specific disability. Second, depression and fatigue had strong effects on one another. Third, fatigue and pain-specific disability (but not depression) predicted subsequent pain. One must be cautious in directly comparing findings from this study with our results generated by MMRM and the two studies using GEE, since path analysis uses a quite different analytic framework than MMRM and GEE. More fundamentally, the inclusion of fatigue and pain-specific disability as explanatory variables in models examining the pain-depression dyad is debatable. Fatigue is not only a core symptom of depressive disorders but the two conditions have strong reciprocal relationships. Moreover, disability is powerfully influenced by both depression and pain. Including a pain-specific disability measure may not yield the same results as including a more general disability measure that is sensitive to the influences of both pain and depression. Using a general disability measure, Geerlings did not find that disability mediated the pain-depression relationship.14 What is clear from Table 3 is that all 8 longitudinal studies using disparate patient populations, pain and depression measures, analytic strategies, and adjustment for different confounders confirm that current pain or pain change predicts future depression, while 7 of the 8 studies confirm that current depression or depression change predicts future pain.
A variety of factors have been postulated to explain the pain-depression relationship. With respect to physiological explanations, both nociceptive and affective pathways coincide anatomically.4,9 Also, norepinephrine and serotonin, which are central in the pathophysiology of mood disorders, are also involved in the gate-control mechanism of pain. Recent research is exploring polymorphisms in pain-mood candidate genes as a potential etiological factor.38 Affective disorders may result in heightened attention towards painful stimuli.9,48 Maladaptive coping skills, low self-efficacy, and other cognitive-behavioral factors may play mediating roles.7,9,48 There may be “third factors” common to both conditions (e.g., greater physical comorbidity, lower socioeconomic status) that may serve as predisposing or accentuating factors.33 A fuller discussion of potential mechanisms are discussed in detail elsewhere.4,9,13,38,48
Strengths of our study include the diverse and clinically complex nature of our sample (i.e., patients with clinical pain and depression were studied), a reasonably large sample size, and repeated assessment with standardized measures over 12 months. Several limitations should also be acknowledged. While we had a good distribution of depression severity due our sampling procedures, all patients had pain of at least moderate severity. Thus, pain severity had a more restricted distribution than depression severity. However, the follow-up depression and pain scores in the 3 groups (Table 1) as well as standard deviations confirm there was a spectrum of change for both pain and depression represented in the full sample. Second, the 250 depressed patients in SCAMP participated in a randomized clinical trial whereas the 250 nondepressed patients were assessed in an observational fashion. However, the fact that our results were similar in the clinical trial sample, its two treatment arms, and the full sample of depressed and nondepressed subjects, somewhat ameliorates concerns about confounding by an intervention effect.
A third study limitation is our lack of a separate patient-rated global measure for both pain and depression; therefore, we could not categorize patients as improved, unchanged, or worse by an independent measure. Using cutpoints on the continuous pain and depression measures to operationally define categories would be problematic since equal percentage changes in depression and pain may not be clinically equivalent, the percent changes might differ (i.e., be asymmetric) for clinically significant improvement vs. worsening, and the boundaries for cutpoints between improved, unchanged, and worse would be somewhat arbitrary. Had our study included patient-rated global categories of improved, unchanged, and worse, we could have examined whether the effects of worsening and improvement are equivalent. For example, it is possible that worsening in pain has a greater magnitude of effect on subsequent depression than improvement. Fourth, both pain and depression in our sample was predominantly chronic in nature, and our analyses therefore tended to pick up changes in pain and depression severity more often than the incidence of either symptom-based condition. At the same time, both pain and depression are chronic and/or recurrent in many patients, exhibiting a waxing and waning pattern of severity rather than a dichotomous “on-off” clinical course. To this end, our findings in patients with clinical pain and depression complement results from longitudinal epidemiological studies which have examined pain and depression as risk factors for the incidence of one another.
In summary, our findings coupled with recent longitudinal clinical and epidemiological studies highlight the importance of investigating pain and depression as fellow travelers, both when caring for patients and conducting research. More often than not, their presence and severity should be assessed jointly rather than singly, and the detection of one should trigger a search for the other for several reasons. First, the presence of both pain and depression is associated with substantially greater disability than the presence of either condition alone.2,4 Additionally, the presence of both conditions increases health care use and costs.1 Second, analyses of clinical trials and other longitudinal studies have shown that the presence of pain may reduce the effectiveness of treatment targeted at depression and, similarly, the presence of depression may reduce the response of pain to therapy.3,28,35,37,44 The MMRM results of our trial as well the GEE results in the trial by Hurwitz et al17 showed that the amount of pain change predicted subsequent depression severity, and vice-versa, even after controlling for intervention effects. Since the comorbidity of pain and depression is 30–50%, failure to recognize one condition while treating the other may result not only in added morbidity from the unrecognized condition but also suboptimal outcomes in the condition being targeted for treatment.
Screening is facilitated by the development of brief measures that are effective for both detecting and monitoring pain and depression.22,24,41 Even if screening for both conditions is not initially performed, the failure of either pain or depression to respond adequately to treatment should prompt screening for the other member of the dyad. Some treatments may be effective in both conditions (though not always to the same degree), such as antidepressants and cognitive-behavioral therapy.18 In other cases, symptom-specific treatments (e.g., optimized analgesic therapy, pain self-management programs, referrals to pain specialists or mental health professionals) may be necessary if the persistence of one condition is interfering with the amelioration of the other. Future research should continue to clarify both biological and other mechanisms underpinning the interdependency of pain and depression. Meanwhile, clinical care may be enhanced by joint attention to pain and depression rather than an either-or approach.
Perspective.
This study strengthens the evidence for a bidirectional and potentially causative influence of pain and depression on one another. A change in severity of either symptom predicts subsequent severity of the other symptom. Thus, recognition and management of both conditions may be warranted, particularly when treatment focused on one condition is not leading to an optimal response.
Footnotes
Disclosures
This study was supported by a grant from the National Institute of Mental Health to Dr. Kroenke (MH-071268). None of the authors have any financial or other conflicts of interest to disclose relevant to this paper.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Arnow BA, Blasey CM, Lee J, Fireman B, Hunkeler EM, Dea R, Robinson R, Hayward C. Relationships among depression, chronic pain, chronic disabling pain, and medical costs. Psychiatric Services. 2009;60:344–350. doi: 10.1176/ps.2009.60.3.344. [DOI] [PubMed] [Google Scholar]
- 2.Arnow BA, Hunkeler EM, Blasey CM, Lee J, Constantino MJ, Fireman B, Kraemer HC, Dea R, Robinson R, Hayward C. Comorbid depression, chronic pain, and disability in primary care. Psychosom Med. 2006;68:262–268. doi: 10.1097/01.psy.0000204851.15499.fc. [DOI] [PubMed] [Google Scholar]
- 3.Bair MJ, Robinson RL, Eckert GJ, Stang PE, Croghan TW, Kroenke K. Impact of pain on depression treatment response in primary care. Psychosom Med. 2004;66:17–22. doi: 10.1097/01.psy.0000106883.94059.c5. [DOI] [PubMed] [Google Scholar]
- 4.Bair MJ, Robinson RL, Katon W, Kroenke K. Depression and pain comorbidity: a literature review. Arch Intern Med. 2003;163:2433–2445. doi: 10.1001/archinte.163.20.2433. [DOI] [PubMed] [Google Scholar]
- 5.Chou K. Reciprocal relationship between pain and depression in older adults: evidence from the English Longitudinal Study of Ageing. J Affect Disord. 2007;102:115–123. doi: 10.1016/j.jad.2006.12.013. [DOI] [PubMed] [Google Scholar]
- 6.Cleeland CS. Measurement of pain by subjective report. In: Foley KM, editor. Advances in Pain Research and Therapy. 1989. pp. 391–403. [Google Scholar]
- 7.Covic T, Adamson B, Spencer D, Howe G. A biopsychosocial model of pain and depression in rheumatoid arthritis: a 12-month longitudinal study. Rheumatology (Oxford) 2003;42:1287–1294. doi: 10.1093/rheumatology/keg369. [DOI] [PubMed] [Google Scholar]
- 8.Demyttenaere K, Bonnewyn A, Bruffaerts R, Brugha T, de GR, Alonso J. Comorbid painful physical symptoms and depression: prevalence, work loss, and help seeking. J Affect Disord. 2006;92:185–193. doi: 10.1016/j.jad.2006.01.007. [DOI] [PubMed] [Google Scholar]
- 9.Dersh J, Polatin PB, Gatchel RJ. Chronic pain and psychopathology: research findings and theoretical considerations. Psychosom Med. 2002;64:773–786. doi: 10.1097/01.psy.0000024232.11538.54. [DOI] [PubMed] [Google Scholar]
- 10.Dietrich AJ, Oxman TE, Williams JW, Jr, Schulberg HC, Bruce ML, Lee PW, Barry S, Raue PJ, Lefever JJ, Heo M, Rost K, Kroenke K, Gerrity M, Nutting PA. Re-engineering systems for the treatment of depression in primary care: cluster randomised controlled trial. BMJ. 2004;329:602–605. doi: 10.1136/bmj.38219.481250.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dworkin RH, Turk DC, Wyrwich KW, Beaton D, Cleeland CS, Farrar JT, Haythornthwaite JA, Jensen MP, Kerns RD, Ader DN, Brandenburg N, Burke LB, Cella D, Chandler J, Cowan P, Dimitrova R, Dionne R, Hertz S, Jadad AR, Katz NP, Kehlet H, Kramer LD, Manning DC, McCormick C, McDermott MP, McQuay HJ, Patel S, Porter L, Quessy S, Rappaport BA, Rauschkolb C, Revicki DA, Rothman M, Schmader KE, Stacey BR, Stauffer JW, von ST, White RE, Witter J, Zavisic S. Interpreting the clinical importance of treatment outcomes in chronic pain clinical trials: IMMPACT recommendations. J Pain. 2008;9:105–121. doi: 10.1016/j.jpain.2007.09.005. [DOI] [PubMed] [Google Scholar]
- 12.Emptage NP, Sturm R, Robinson RL. Depression and comorbid pain as predictors of disability, employment, insurance status, and health care costs. Psychiatr Serv. 2005;56:468–474. doi: 10.1176/appi.ps.56.4.468. [DOI] [PubMed] [Google Scholar]
- 13.Fishbain DA, Cutler R, Rosomoff H, Rosomoff RS. Chronic pain-associated depression: antecedent or consequence of chronic pain? A review. Clin J Pain. 1997;13:116–137. doi: 10.1097/00002508-199706000-00006. [DOI] [PubMed] [Google Scholar]
- 14.Geerlings SW, Twisk JW, Beekman AT, Deeg DJ, van TW. Longitudinal relationship between pain and depression in older adults: sex, age and physical disability. Soc Psychiatry Psychiatr Epidemiol. 2002;37:23–30. doi: 10.1007/s127-002-8210-2. [DOI] [PubMed] [Google Scholar]
- 15.Gureje O, Simon GE, Von Korff M. A cross-national study of the course of persistent pain in primary care. Pain. 2001;92:195–200. doi: 10.1016/s0304-3959(00)00483-8. [DOI] [PubMed] [Google Scholar]
- 16.Hawker GA, Gignac MAM, Badley E, Davis AM, French MR, Li Y, Perruccio AV, Power JD, Sale J, Lou W. A longitudinal study to explain the pain-depression link in older adults with osteoarthritis. Arthritis Care Res. doi: 10.1002/acr.20298: 2010. [DOI] [PubMed] [Google Scholar]
- 17.Hurwitz EL, Morgenstern H, Yu F. Cross-sectional and longitudinal associations of low-back pain and related disability with psychological distress among patients enrolled in the UCLA Low-Back Pain Study. J Clin Epidemiol. 2003;56:463–471. doi: 10.1016/s0895-4356(03)00010-6. [DOI] [PubMed] [Google Scholar]
- 18.Jackson JL, O’Malley PG, Kroenke K. Antidepressants and cognitive-behavioral therapy for symptom syndromes. CNS Spectr. 2006;11:212–222. doi: 10.1017/s1092852900014383. [DOI] [PubMed] [Google Scholar]
- 19.Katon W, Von Korff M, Lin E, Simon G, Walker E, Unutzer J, Bush T, Russo J, Ludman E. Stepped collaborative care for primary care patients with persistent symptoms of depression: a randomized trial. Arch Gen Psychiatry. 1999;56:1109–1115. doi: 10.1001/archpsyc.56.12.1109. [DOI] [PubMed] [Google Scholar]
- 20.Katona C, Peveler R, Dowrick C, Wessely S, Feinmann C, Gask L, Lloyd H, Wager E, Williams AC, Wager E. Pain symptoms in depression: definition and clinical significance. Clin Med. 2005;5:390–395. doi: 10.7861/clinmedicine.5-4-390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kazis LE, Anderson JJ, Meenan RF. Effect sizes for interpreting changes in health status. Med Care. 1989;27:S178–S189. doi: 10.1097/00005650-198903001-00015. [DOI] [PubMed] [Google Scholar]
- 22.Krebs EE, Lorenz KA, Bair MJ, Damush TM, Wu J, Sutherland J, Asch SM, Kroenke K. Development and initial validation of the PEG, a three-item scale assessing pain intensity and interference. J Gen Intern Med. 2009;24:733–738. doi: 10.1007/s11606-009-0981-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kroenke K, Bair MJ, Damush TM, Wu J, Hoke S, Sutherland J, Tu W. Optimized antidepressant therapy and pain self-management in primary care patients with depression and musculoskeletal pain: a randomized controlled trial. JAMA. 2009;301:2099–2110. doi: 10.1001/jama.2009.723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kroenke K, Spitzer RL, Williams JBW, Lowe B. An ultra-brief screening scale for anxiety and depression: the PHQ-4. Psychosomatics. 2009;50:613–621. doi: 10.1176/appi.psy.50.6.613. [DOI] [PubMed] [Google Scholar]
- 25.Kroenke K. The interface between physical and psychological symptoms. J Clin Psychiatry Primary Care Companion. 2003;5(suppl 7):11–18. [Google Scholar]
- 26.Kroenke K. Somatic symptoms and depression: a double hurt. Prim Care Companion J Clin Psychiatry. 2005;7:148–149. doi: 10.4088/pcc.v07n0401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kroenke K, Bair M, Damush T, Hoke S, Nicholas G, Kempf C, Huffman M, Wu J, Sutherland J. Stepped Care for Affective Disorders and Musculoskeletal Pain (SCAMP) study Design and practical implications of an intervention for comorbid pain and depression. Gen Hosp Psychiatry. 2007;29:506–517. doi: 10.1016/j.genhosppsych.2007.08.005. [DOI] [PubMed] [Google Scholar]
- 28.Kroenke K, Shen J, Oxman TE, Williams JW, Jr, Dietrich AJ. Impact of pain on the outcomes of depression treatment: results from the RESPECT trial. Pain. 2008;134:209–215. doi: 10.1016/j.pain.2007.09.021. [DOI] [PubMed] [Google Scholar]
- 29.Kroenke K, Spitzer RL, Williams JBW. The PHQ-9: Validity of a brief depression severity measure. J Gen Intern Med. 2001;16:606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kroenke K, West SL, Swindle R, Gilsenan A, Eckert GJ, Dolor R, Stang P, Zhou XH, Hays R, Weinberger M. Similar effectiveness of paroxetine, fluoxetine, and sertraline in primary care: a randomized trial. JAMA. 2001;286:2947–2955. doi: 10.1001/jama.286.23.2947. [DOI] [PubMed] [Google Scholar]
- 31.Kroenke K, Zhong X, Theobald D, Wu J, Tu W, Carpenter JS. Somatic symptoms in patients with cancer experiencing pain or depression: prevalence, disability, and health care use. Arch Intern Med. 2010;170:1686–1694. doi: 10.1001/archinternmed.2010.337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lee Y, Nelder JA. Conditional and marginal models: another view. Statistical Science. 2004;21:219–238. [Google Scholar]
- 33.Leuchter AF, Husain MM, Cook IA, Trivedi MH, Wisniewski SR, Gilmer WS, Luther JF, Fava M, Rush AJ. Painful physical symptoms and treatment outcome in major depressive disorder: a STAR*D (Sequenced Treatment Alternatives to Relieve Depression) report. Psychol Med. 2009 doi: 10.1017/S0033291709006035. [DOI] [PubMed] [Google Scholar]
- 34.Lindsey JK, Lambert P. On the appropriateness of marginal models for repeated measurement in clinical trials. Statist Med. 1998;17:447–469. doi: 10.1002/(sici)1097-0258(19980228)17:4<447::aid-sim752>3.0.co;2-g. [DOI] [PubMed] [Google Scholar]
- 35.Linton SJ. A review of psychological risk factors in back and neck pain. Spine. 2000;25:1148–1156. doi: 10.1097/00007632-200005010-00017. [DOI] [PubMed] [Google Scholar]
- 36.Lowe B, Unutzer J, Callahan CM, Perkins AJ, Kroenke K. Monitoring depression treatment outcomes with the patient health questionnaire-9. Med Care. 2004;42:1194–1201. doi: 10.1097/00005650-200412000-00006. [DOI] [PubMed] [Google Scholar]
- 37.Mavandadi S, Ten Have TR, Katz IR, Durai UN, Krahn DD, Llorente MD, Kirchner JE, Olsen EJ, Van Stone WW, Cooley SL, Oslin DW. Effect of depression treatment on depressive symptoms in older adulthood: the moderating role of pain. J Am Geriatr Soc. 2007;55:202–211. doi: 10.1111/j.1532-5415.2007.01042.x. [DOI] [PubMed] [Google Scholar]
- 38.Max MB, Wu T, Atlas SJ, Edwards RR, Haythornthwaite JA, Bollettino AF, Hipp HS, McKnight CD, Osman IA, Crawford EN, Pao M, Nejim J, Kingman A, Aisen DC, Scully MA, Keller RB, Goldman D, Belfer I. A clinical genetic method to identify mechanisms by which pain causes depression and anxiety. Mol Pain. 2006;2:14. doi: 10.1186/1744-8069-2-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Meyer T, Cooper J, Raspe H. Disabling low back pain and depressive symptoms in the community-dwelling elderly. Spine. 2007;32:2380–2386. doi: 10.1097/BRS.0b013e3181557955. [DOI] [PubMed] [Google Scholar]
- 40.Miller LR, Cano A. Comorbid chronic pain and depression: who is at risk? J Pain. 2009;10:619–627. doi: 10.1016/j.jpain.2008.12.007. [DOI] [PubMed] [Google Scholar]
- 41.Mitchell AJ, Coyne JC. Do ultra-short screening instruments accurately detect depression in primary care? A pooled analysis and meta-analysis of 22 studies. Br J Gen Pract. 2007;57:144–151. [PMC free article] [PubMed] [Google Scholar]
- 42.Shih M, Hootman JM, Strine TW, Chapman DP, Brady TJ. Serious psychological distress in U.S. adults with arthritis. J Gen Intern Med. 2006;21:1160–1166. doi: 10.1111/j.1525-1497.2006.00573.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Spitzer RL, Williams JB, Kroenke K, Linzer M, deGruy FV, III, Hahn SR, Brody D, Johnson JG. Utility of a new procedure for diagnosing mental disorders in primary care. The PRIME-MD 1000 study. JAMA. 1994;272:1749–1756. [PubMed] [Google Scholar]
- 44.Thielke SM, Fan MY, Sullivan M, Unutzer J. Pain limits the effectiveness of collaborative care for depression. Am J Geriatr Psychiatry. 2007;15:699–707. doi: 10.1097/JGP.0b013e3180325a2d. [DOI] [PubMed] [Google Scholar]
- 45.Unutzer J, Katon W, Callahan CM, Williams JW, Jr, Hunkeler E, Harpole L, Hoffing M, Della Penna RD, Noel PH, Lin EH, Arean PA, Hegel MT, Tang L, Belin TR, Oishi S, Langston C. Collaborative care management of late-life depression in the primary care setting: a randomized controlled trial. JAMA. 2002;288:2836–2845. doi: 10.1001/jama.288.22.2836. [DOI] [PubMed] [Google Scholar]
- 46.Von Korff M, Ormel J, Keefe FJ, Dworkin SF. Grading the severity of chronic pain. Pain. 1992;50:133–149. doi: 10.1016/0304-3959(92)90154-4. [DOI] [PubMed] [Google Scholar]
- 47.Williams JW, Jr, Barrett J, Oxman T, Frank E, Katon W, Sullivan M, Cornell J, Sengupta A. Treatment of dysthymia and minor depression in primary care: A randomized controlled trial in older adults. JAMA. 2000;284:1519–1526. doi: 10.1001/jama.284.12.1519. [DOI] [PubMed] [Google Scholar]
- 48.Williams LJ, Jacka FN, Pasco JA, Dodd S, Berk M. Depression and pain: an overview. Acta Neuropsychiatrica. 2006;18:79–87. doi: 10.1111/j.1601-5215.2006.00130.x. [DOI] [PubMed] [Google Scholar]
- 49.Williams LS, Jones WJ, Shen J, Robinson RL, Kroenke K. Outcomes of newly referred neurology outpatients with depression and pain. Neurology. 2004;63:674–677. doi: 10.1212/01.wnl.0000134669.05005.95. [DOI] [PubMed] [Google Scholar]
- 50.Williams LS, Jones WJ, Shen J, Robinson RL, Weinberger M, Kroenke K. Prevalence and impact of pain and depression in neurology outpatients. J Neurol Neurosurg Psychiatry. 2003;74:1587–1589. doi: 10.1136/jnnp.74.11.1587. [DOI] [PMC free article] [PubMed] [Google Scholar]