Abstract
In the absence of scientific consensus on an appropriate theoretical framework, cumulative risk assessment and related research have relied on speculative conceptual models.
We argue for the importance of theoretical backing for such models and discuss 3 relevant theoretical frameworks, each supporting a distinctive “family” of models. Social determinant models postulate that unequal health outcomes are caused by structural inequalities; health disparity models envision social and contextual factors acting through individual behaviors and biological mechanisms; and multiple stressor models incorporate environmental agents, emphasizing the intermediary role of these and other stressors.
The conclusion is that more careful reliance on established frameworks will lead directly to improvements in characterizing cumulative risk burdens and accounting for disproportionate adverse health effects.
FORMAL ASSESSMENT OF combined health effects from exposure to multiple environmental agents dates back at least several decades.1 However, no cumulative risk assessment conducted by the US Environmental Protection Agency (EPA) has explicitly included nonchemical stressors (e.g., psychological and social factors), such as dilapidated housing, family conflict, and racial discrimination.1 Strategies to assess cumulative risk fall into 2 general categories: a “bottom–up” approach, which attempts to calculate an aggregate risk estimate by summing risks of individual constituents, and a “top–down” approach, which works backward from observed health effects to disaggregate cumulative risk into its component parts.2 Currently, principles and practices for conducting cumulative risk assessments are still in development, and there is no empirically verified theory guiding how best to combine and then assess risks from both chemical and nonchemical stressors.3,4 In the subsequent discussion, we examine why decisions about theoretical frameworks matter for cumulative risk assessment, and identify 3 main families of conceptual models that can be used to understand and estimate combined health risks from environmental, social, and psychological factors.
WHY THEORETICAL FRAMEWORKS MATTER
A theoretical framework is a formalized analytic schema that organizes important assumptions, concepts, indicators, and propositions into an ordered pattern that unambiguously delineates postulated causal factors and pathways. It functions as an intellectual blueprint that guides attempts to model and estimate cumulative health risks. Without such explicit theoretical ordering, several problems can occur. First, key assumptions remain implicit and can easily escape scientific scrutiny. Then, when the hypothesized model fails to fit observed phenomena, it is difficult to discern problems and devise solutions. Second, without explicit theoretical guidance, the assumptions that enable these combined assessments—cumulating across chemical and nonchemical stressors—can be contradictory or raise ambiguities that can only be resolved on an ad hoc, piecemeal basis. Third, absent explicit ties to theory, pragmatic considerations such as data availability can effectively steer the analysis and dictate which factors should be included and what relationships should count as valid.
In the early stages of exploration and development, conceptual models (and their visual displays in box-and-arrow diagrams) stand in for formal theories to provide a simplified inventory of concepts, relations, and propositions that can be linked to data. Those most likely to find traction among investigators do more than bundle propositions; they provide rationale and guidance for subsequent empirical investigations and identify targets for policy interventions. In effect, they stake out some uncharted terrain for further assessment, yielding not quite a map, but a partial sketch of what can be expected and where to look for it. These conceptual sketches necessarily involve simplifications and a sacrifice of information to achieve their purpose. However, when guided by a theoretical framework, the modeling process retains its coherence and grounding.
Our conventional conception of “models,” according to Morgan and Morrison,4 places them squarely between theories and the data needed to test them. Models are thought to function as mediators with both theoretical and operational implications, but are clearly distinct from either. Ideally, a theory yields multiple models that, in turn, generate sets of operationally testable propositions. Consistency with empirical data is the chief reference criterion for judging the model's adequacy and, ultimately, for supporting the theory. In this scheme, there is a sequential ordering of activities: first comes development of theory, then building of models, and finally testing with data.4 In practice, of course, especially in newly emerging problem areas, this sequence is rarely followed; theory development is bypassed in favor of proliferating conceptual models that both serve as theory and specify operational indicators.5
When models take on multiple functions, as well as provide a focal point for research activity, as they have in this context, they become difficult to evaluate.6 The adequacy of the model may depend more on its performance in problem framing than on any particular explanatory leverage it provides. We typically judge models of this kind based on their reasonableness or face validity; that is, whether their proposed causal ordering is plausible and whether they incorporate concepts of interest. Empirical validity is also a consideration, but most speculative models of the kind used in cumulative risk research and assessment can only be judged indirectly, based on partial evidence that applies to one portion of the model at a time. In the end, much of the collective judgment about the adequacy of any particular model is left to depend not so much on definitive empirical tests as on certain subjective qualities of the research, such as the reputational capital of the model's authors, the disciplines involved, institutional sponsorship, and reliance on familiar arguments to support its selection of indicators.
Whether policy stakes and sponsorship interests influence the specification of the model itself, as opposed to the framing of the problem or the inclusion of particular variables, is an open question. Still, it would be difficult to claim that values play no role in defining a particular causal order. The critical question is “how large a role do they play”? Beyond the values of the investigators often made explicit in reported results, there is also a question of how the choice of methodological approach unduly influences model content and the kinds of relationships that are actually tested. Some attribute the priority afforded biological processes over social processes to be a product of the explanatory framework that guides epidemiological practice.7,8 Schofield, for example, argues that instead of treating the social realm as a static, contextual factor impinging on individual behavior, the same attention given to biological mechanisms needs to be applied to mapping the dynamics of social processes.7 The potential for a variety of values, some ethical, others methodological, to affect the model's design reinforces the point made earlier that cumulative risk assessment models do not serve as mediators between theory and data, but rather embody elements of both without necessarily intending to do so.
Presently, the concept of cumulative risk is being framed and quantitative indicators defined according to the metaphor of multiple stressors that operate through mediating vulnerabilities to evoke receptor response. The meaningfulness and utility of any proposed stressor indicator depends on the pattern of relationships it maintains with other variables of interest; which is to say, it is contingent on an assumed theoretical framework. The framework sets expectations about each indicator's random error, about their correlations with other measures, and about their connection by inference with unmeasured constructs. This means that when the framework changes, so does the meaning and utility of its indicators. For researches and risk assessors, the first-order problem—which is the appropriate theoretical framework?—should be resolved before addressing the second-order problem—which measurement assumptions and associated indicators are best suited to the application at hand?
FRAMEWORKS AS “FAMILIES” OF CONCEPTUAL MODELS
It is desirable to locate sets of empirical findings within a larger context of a “family” of conceptual models with explicit links to a particular theoretical framework—where family refers to resemblances among conceptual models that share the same theoretical roots. In this way, key suppositions can be made explicit, and conclusions about the strength of the evidence from any particular model can incorporate judgments about results from the larger family of models, relative strength of family ties, and common assumptions about causal orderings. Within the general field of cumulative risk research, the multiple stressor metaphor provides some guidance. Multiple stressor models consider health inequality to be a product of exposure to some well-defined set of environmental stressors. Nonetheless, when it comes to including nonchemical stressors, there are 2 better established families of conceptual models that offer the advantages of an extensive theoretical framework and numerous applications. Social determinant models regard health principally as a product of social factors, and health disparity models depict it as more a product of biological and contextual interactions.
Considering multiple stressor studies as a family for purposes of comparison, all 3 families have a number of elements in common. All 3 are motivated by the injustice of unequal distributions of health risks and morbidity and mortality across social groups; trace the origins of health inequality to some features of social inequality and identify poverty and its effects as playing a major role; incorporate contextual factors and other features of place into their models; and posit pathways between the social realm and the physical domain that pass through psychological mechanisms. Despite considerable overlap in modeling strategies, each family's distinctive traits must be taken into account when applying it to a particular cumulative risk assessment.
In the sections to follow, we consider each of 3 distinctive (but overlapping) theoretical frameworks, which have been recast for our purposes as general families of models. We discuss the distinguishing traits of each family and pick a representative member of the family–a conceptual model drawn from the literature–that shows some promise for the advance of cumulative risk research. We then consider the merits of mingling models across families as a strategy for enrichment, and conclude with the difficult problem of deciding which model is best.
SOCIAL DETERMINANT MODELS
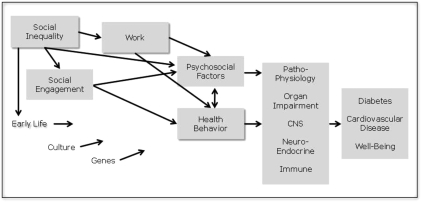
A stylized version of a social determinant conceptual model is depicted in Figure 1. It traces the source of health inequalities to social inequality, defined as the unequal distribution of economic and social resources and the opportunities for access to them. Causal pathways move to the right through material conditions, social engagement and psychological factors on to physiological and behavioral responses, and then to health status. As material conditions worsen, both social engagement and psychological coping are adversely affected, prompting pathophysiological processes and behavioral adaptations that ultimately lead to impairment and increased risk of premature death. Much of this model has been tested empirically in a piecemeal fashion, and results were incorporated into a 1998 World Health Organization commission report on social determinants.11
FIGURE 1.
A social determinant conceptual model.
Proponents argue that the impact of social inequality on population health is reflected in a strong and consistent empirical association that appears across levels of social organization, from nations to neighborhoods, and with only small variation based on alternative ways of measuring relative inequality and health.12,13 Critics contend that the observed effects are compositional rather than contextual.14–17 That is to say, that in geopolitical units with high relative inequality, there will be a higher proportion of poor people who face more serious health risks and that this proportion drives the observed relationship. The implications of this criticism for the social determinant approach are profound. If absolute income and not relative inequality are behind health inequalities, then social factors give way to material ones. As House pointed out, then there is no longer a need for pathways through social engagement, including levels of cohesion and social capital, and the psychological effects of relative deprivation are moot.17 Today, the issue remains unsettled.
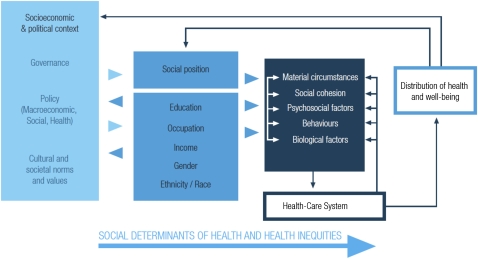
As a theoretical framework, the social determinant family offers the richest set of conceptual resources, grounded in a generation of research across components and variations in its basic models. The most recent effort to characterize the overall framework diagrammatically appears in Figure 2. Note that the position of the macro level social and political context assumes a larger profile than in the stylized version (Figure 1), and social class remains a central determinant.
FIGURE 2.
The social determinant theoretical framework from the World Health Organization.
Source. World Health Organization.18
HEALTH DISPARITY MODELS
The health disparity family of models overlaps with the social determinant approach but reorders the causal pathways so that social inequality and its proxies are no longer the primary driving factors. Instead, emphasis shifts to a variety of social and contextual conditions and their impact on health outcomes through individual behaviors and biological responses.19,20 The legacies of the social determinant approach, such as the inclusion of psychological and physiological pathways, and the elaboration of social context are still here. More generally, this approach influenced (and was influenced by) the form of ecological models in epidemiology and also altered the balance of emphasis in population-based studies toward social, as opposed to individual characteristics, linked to health.
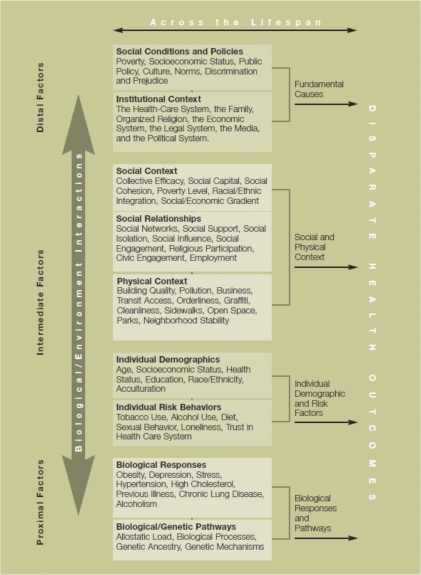
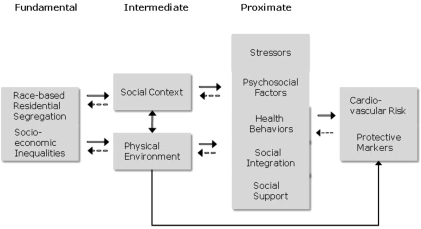
The health disparity framework, depicted in the summary graphic of Figure 3, was developed jointly by the Centers for Population Health and Health Disparities (CPHHD).21 A conceptual model from this family, developed by the Healthy Environment Partnership (HEP) in Detroit, Michigan,22 appears in Figure 4. The HEP model is a more conventional box-and-arrow version of the CPHHD framework (Figure 3). The HEP model takes the stacked boxes shown in the CPHHD graphic and creates an ordered sequence of effects moving from fundamental factors through intermediate to proximate. Where the CPHHD framework posits direct effects among each of its 4 major categories and disparate health outcomes, the HEP model variant arranges the categories in a strict order with fundamental factors operating through intermediate factors, and intermediate factors acting through proximate factors. The openness of the CPHHD framework carries over in this model, permitting a subordinate reciprocal effect that can operate in the opposite direction—proximate through intermediate to distal factors. This appears as a hedge of sorts, keeping relationships open until the covariance among empirical indicators can be examined. Ultimately, the CPHHD framework guiding this application serves as a menu rather than as a recipe.
FIGURE 3.
The health disparity theoretical framework supported by the National Cancer Institute.
Source. Centers for Population Health and Health Disparities.21
FIGURE 4.
A health disparity conceptual model.
Source. Schultz et al.22
Going from the framework to the HEP model, a few of the subcategories change relative position and some drop out altogether. Social relationships migrate from being an intermediate contextual effect to the proximate category, essentially getting a step closer to having a direct effect on health risk. Psychosocial factors are organized into their own subcategory, whereas the CPHHD framework spreads them between individual risk factors and biological responses. Individual demographics, including age, education, and race, drop out as indicators for health risk. The most important omission, from a social determinant perspective, is the exclusion of any measures of income or socioeconomic status. Socioeconomic inequality is included as a fundamental distal factor, but poverty and income do not appear in the model. Clearly, within the health disparity family of models there is considerable latitude for rearranging priority among causal factors, even if the logic does not change.
MULTIPLE STRESSOR MODELS
The multiple stressor models incorporate potential environmental pathways for analyzing health inequality more explicitly than the previous 2 families. Although the multiple stressor approach shares some categorical concerns with social determinant and health disparity models, this family's conceptual origins are found in ecological risk assessment.23,24 The key feature of these models is the presence of stressors and stress at multiple intermediary locations in the modeling space. The mechanisms are assumed to be analogous to the ways stress operates in ecological and other biologic systems, with consequent disruptive effects on the functioning and well-being of a particular system.25
There are 2 immediate consequences of these assumptions worth noting. First, the stress–response arc can displace consideration of any complicated interactional mechanisms associated with social relations, actor agency, and other nonmaterial contingencies. Second, what counts as stress and stressors by analogy includes “Any… entity that can induce an adverse response.”26 Although the candidates for ecosystem stressors may be well defined and measures of ecologic stress fully articulated, once we move to social settings, it becomes difficult to know what to exclude. The ability to assign priority to certain sources and effects becomes a function of being able, first, to step outside the ecological model analogy and, second, to translate available results back into the stress-receptor orientation. There is some advantage in being able to move from social kinds of stressors to biological ones and remain in the same register. For example, it makes it easier for risk assessors to consider social systems as a causal factor contributing to health inequalities. However, the need to stretch the stress-receptor model to accommodate social phenomena raises questions about whether the multiple stressor family represents an advance over the other 2 frameworks.
Another key feature of this type of conceptual model is its explicit link to race and discrimination as a primary source of health disparities, as mediated through community and individual level factors. Consistent with the HEP model presented previously (Figure 4), segregation is specified as a community level manifestation of discrimination. Research showed the pivotal role played by discrimination,27 and the focus in many multiple stressor models on discrimination was motivated, in part, by environmental justice concerns. One advantage of juxtaposing multiple stressor models with models from other frameworks is to establish an explicit and promising link between research conducted by social and biomedical scientists and that conducted by ecologists and environmental health scientists.28
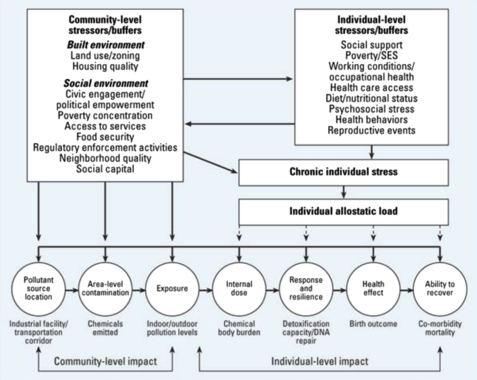
A stylized representation of the multiple stressor family is the exposure–disease model proposed by Gee and Payne-Sturges29 shown in Figure 5. Paralleling the model families described previously, this speculative model organizes potential factors affecting health inequality into a causal ordering. The model retains its modularity and nominal clustering of like concepts. Arrows move in one direction, in this case, from race/ethnicity through collective and individual level factors to health effects. The model features stress and stressors as mediating factors and organizes them into a twofold distinction between communities and individuals. The notion of vulnerability is also introduced, which permits some variation in predicted damage based on previous exposures and capacity to resist, adapt, or cope. The exposure–stress–effect framework, developed by Morello-Frosch and Shenassa30 and depicted in Figure 6, parallels in inclusiveness the theoretical frameworks shown previously. It posits that both chemical and nonchemical stressors contribute to individual stress and allostatic load (cumulative impact over time of adaptive processes to acute stress). Allostatic load, in turn, increases individual vulnerability, thereby contributing to subsequent health disparities. As part of its logic, this framework distinguishes between community and individual level stressors, buffers, and related health outcomes.
FIGURE 5.
The multiple stressor conceptual model.
Source. Gee and Payne-Sturges.29
FIGURE 6.
The multiple stressor theoretical framework cited by the US Environmental Protection Agency.
Source. Morello-Frosch and Shenassa.30
In contrast to the social determinant and health disparity frameworks, this family introduces a parallel set of exposure mechanisms and juxtaposes them onto the hierarchy of stressor–stress relationships. Although this makes explicit the physical mechanisms connecting environmental pollutants to health disparities in particular neighborhoods, it is not matched by a similar level of specification for the cascade of events by which community level stressors and related stress translate into individual levels stressors or stress. Here, more systematic reliance on other frameworks can have its greatest effect. Are there hierarchical effects best modeled as multilevel, nested relationships as in disparity modeling? Likewise, are there relevant structural effects that are irreducible to individual characteristics or psychological processes as in social determinant models? In either event, close scrutiny of the theoretical framework becomes a key to progress.
CONCLUSIONS
Much of the work in the field of cumulative risk is informed by a special class of models referred to s speculative, because they function primarily as conceptual aids and heuristics rather than as testable analytic schemas. Successive rounds of speculative modeling has influenced the direction of cumulative risk assessments and related research as much or more than any particular set of empirical results. These models can make assumptions about plausible links explicit and can simplify. The challenge is how to make them more susceptible to testing, so that empirical findings become more systematic and replicable. One answer is to move away from speculative models altogether and adopt formal modeling that provides for comprehensive specification and for joint, simultaneous estimation of most parameters. Urban sociologists, for example, made extensive use of formal models, deployed in structural equations, to test for the impact of neighborhood effects on problem behaviors.31 To be sure, the stakes are higher with a formal model, because disappointing empirical results can lead to its outright rejection. Depending on the estimation method, the more conservative strategy of segment-by-segment testing and incremental refinement may be largely ruled out.
A second option is to follow the path taken by the CPHHD20 for disparity research. They constructed an extensive inventory of concepts and posited certain theoretical relationships (see Figure 6); empirical components were then fashioned into models and tested by funded research centers. One problem with this approach is the possibility that a key feature with pivotal theoretical significance might be unintentionally omitted. In this instance, all modeling was eventually tied to empirical indicators, and replicable procedures were used for data assessment. The problem then becomes how the various model pieces are assembled together, especially when they happen to be rivals making different claims.
The third, and perhaps least satisfying, option is to develop guidance on best practices for modeling in cumulative risk research. To be useful, this exercise must begin with some clarity as to the model's expected function. Is it heuristic, structural, analogous, metaphoric, operational, or testable? Once that is settled and, assuming some structural modularity (e.g., independent subsets of relations), the viability of a particular model may rest on the empirical testing of a small set of relationships. Although there are no conclusive tests for overall model validity, the weight of evidence regarding acceptance or rejection of the model itself can be inferred from a focused research program, even if postulated relationships and causal pathways can only be evaluated one at a time. This follows the logic of identifying bases of corroboration and relying on multiple sources and hybrid tests, a path common to modeling in the social determinants framework.
Overall, the choice of a guiding theoretical framework (or family of models) is pivotal for realistic and reliable assessment of health risks from human exposure to a combination of chemical and nonchemical stressors. The underlying conceptual model, and the framework that supports it, affects virtually every aspect of cumulative risk assessment, including decisions about
identification of independent and dependent variables, as well as the specification of interrelationships among confounders and cofactors;
which indicators or surrogate measures should be used to characterize the impact of multiple stressors on a community;
the degree to which the link between exposure to multiple stressors and related health effects can be quantified;
how vulnerability factors exacerbate or modulate effects of chemical and nonchemical stressors;
the distribution of nonchemical stressors across geospatial units and population groups, and
whether an index or profile can be constructed to represent cumulative risk from multiple stressors for a particular community or population.
The bottom line is that explicit attention to relevant theoretical frameworks, as part of a program of continuous improvement in modeling, is necessary to understand, assess, and ameliorate disproportionate cumulative risk burdens. Organizations, such as the EPA, who are developing cumulative risk assessment guidance, would be well advised to address, explicitly, the theoretical framework under which these assessments will be done and to consider the import of their corresponding assumptions.
Acknowledgments
This work was partially supported by funding from the US Environmental Protection Agency. Earlier versions of some of the ideas developed here were discussed at Strengthening Environmental Justice Research and Decision Making: A Symposium on the Science of Disproportionate Environmental Health Impacts, March 17–19, 2010, Washington, DC.
The authors wish to acknowledge the helpful comments of Michael A. Callahan, MDB, Inc. and Onyemaechi Nweke, US Environmental Protection Agency.
Human Participant Protection
No human subjects were involved in this research.
References
- 1.National Research Council Science and Decisions: Advancing Risk Assessment. Washington, DC: National Academy Press; 2009 [PubMed] [Google Scholar]
- 2.Menzie CA, MacDonell MM, Mumtaz M. A phased approach for assessing combined effects from multiple stressors. Environ Health Perspect. 2007;115(5):807–816 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Callahan MA, Sexton K. If cumulative risk is the answer, what is the question? Environ Health Perspect. 2007;115(5):799–806 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sexton K, Linder SH. The role of cumulative risk assessment in decisions about environmental justice. Int J Environ Res Public Health. 2010;7(11):4037–4049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Morgan MS, Morrison M, Models as Mediators. New York, NY: Cambridge University Press; 1999 [Google Scholar]
- 6.Boumas M. Built-in justification. : Morgan MS, Morrison M, Models as Mediators. New York, NY: Cambridge University Press; 1999:66–96 [Google Scholar]
- 7.Schofield T. Health inequity and its social determinants: a sociological commentary. Health Sociol Rev. 2007;16(2):105–114 [Google Scholar]
- 8.Venkatapuram S, Marmot M. Epidemiology and social justice in light of social determinants of health research. Bioethics. 2009;23(2):79–89 [DOI] [PubMed] [Google Scholar]
- 9.Goldman N. Social inequalities in health: disentangling the underlying mechanisms. : Conference Proceedings of the Seminar on Demography and Epidemiology: Frontiers in Population Health and Aging. Washington, DC: Georgetown University; 2001 [Google Scholar]
- 10.Bruner E, Marmot M. Social organization, stress, and health. : Marmot M, Wilkinson R, The Social Determinants of Health. New York, NY: Oxford University Press; 1999 [Google Scholar]
- 11.Wilkinson R, Marmot M, The Social Determinants of Health: The Solid Facts. 2nd ed Copenhagen: World Health Organization Regional Office for Europe; 2003 [Google Scholar]
- 12.Kawachi I, Kennedy B. Income inequality and health: pathways and mechanisms. Health Serv Res. 1999;34(1 pt 2):215–227 [PMC free article] [PubMed] [Google Scholar]
- 13.Wilkinson R. The Impact of Inequality. New York, NY: The New Press; 2005 [Google Scholar]
- 14.House JS, Lepkowski JM, Kinney AM, et al. The social stratification of aging and health. J Health Soc Behav. 1994;35(3):213–234 [PubMed] [Google Scholar]
- 15.Lynch JW, Kaplan G, Cohen RD, et al. Do cardiovascular risk factors explain the relation between socioeconomic status, risk of all-cause mortality, and acute myocardial infarction? Am J Epidemiol. 1996;144(10):934–942 [DOI] [PubMed] [Google Scholar]
- 16.Mellor JM, Milyo J. Reexamining the evidence of an ecological association between income inequality and health. J Health Polit Policy Law. 2001;26(3):487–522 [DOI] [PubMed] [Google Scholar]
- 17.House JS. Relating social inequalities in health and income. J Health Polit Policy Law. 2001;26(3):523–532 [DOI] [PubMed] [Google Scholar]
- 18.Commission on Social Determinants of Health Closing the Gap in a Generation: Health Equity Through Action on the Social Determinants of Health. Final Report of the Commission on the Social Determinants of Health. Geneva: World Health Organization; 2008. Available at http://whqlibdoc.who.int/publications/2008/9789241563703_eng.pdf. Accessed December 10, 2009 [Google Scholar]
- 19.Braveman P. Health disparities and health equity: concepts and measurement. Annu Rev Public Health. 2006;27:167–194 [DOI] [PubMed] [Google Scholar]
- 20.Warnecke RB, Oh A, Breen N, et al. Approaching health disparities from a population perspective: the National Institutes of Health Centers for Population Health and Health Disparities. Am J Public Health. 2008;98(9):1608–1615 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Centers for Population Health and Health Disparities Cells to Society: Overcoming Health Disparities. Unpublished Report; 2007. Available at http://cancercontrol.cancer.gov/populationhealthcenters/cphhd/documents/CPHHD_report.pdf. Accessed February 10, 2010 [Google Scholar]
- 22.Schulz AJ, Kannan S, Dvonch JT, et al. Social and physical environments and disparities in risk for cardiovascular disease: the healthy environments partnership conceptual model. Environ Health Perspect. 2005;113(12):1817–1825 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.US Environmental Protection Agency Framework for Ecological Risk Assessment. EPA/630/R-92/001 Washington, DC: US Environmental Protection Agency; 1992 [Google Scholar]
- 24.deFur PL, Evans GW, Cohen Hubal EA, et al. Vulnerability as a function of individual and group resources in cumulative risk assessment. Environ Health Perspect. 2007;115(5):817–824 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.US Environmental Protection Agency Stressor Identification Guidance Document. EPA/-822-B-00-025 Washington, DC: Environmental Protection Agency; 2000 [Google Scholar]
- 26.US Environmental Protection Agency Framework for Cumulative Risk Assessment. EPA/630/P-02/001F Washington, DC: Environmental Protection Agency; 2003:74 [Google Scholar]
- 27.Institute of Medicine Unequal Treatment. Washington, DC: National Academy Press; 2002 [Google Scholar]
- 28.Payne-Sturges D, Gee GC. National environmental health measures for minority and low-income populations: tracking social disparities in environmental health. Environ Res. 2006;102(2):154–171 [DOI] [PubMed] [Google Scholar]
- 29.Gee GC, Payne-Sturges DC. Environmental health disparities: a framework integrating psychosocial and environmental concepts. Environ Health Perspect. 2004;112(17):1645–1650 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Morello-Frosch R, Shenassa ED. The environmental riskscape and social inequality: implications for explaining maternal and child health disparities. Environ Health Perspect. 2006;114(8):1150–1153 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sampson RJ, Morenoff JD, Gammon-Rowley T. Assessing neighborhood effects. Annu Rev Sociol. 2002;28:443–478 [Google Scholar]