Abstract
Cumulative risk assessment is a science policy tool for organizing and analyzing information to examine, characterize, and possibly quantify combined threats from multiple environmental stressors.
We briefly survey the state of the art regarding cumulative risk assessment, emphasizing challenges and complexities of moving beyond the current focus on chemical mixtures to incorporate nonchemical stressors, such as poverty and discrimination, into the assessment paradigm. Theoretical frameworks for integrating nonchemical stressors into cumulative risk assessments are discussed, the impact of geospatial issues on interpreting results of statistical analyses is described, and four assessment methods are used to illustrate the diversity of current approaches.
Prospects for future progress depend on adequate research support as well as development and verification of appropriate analytic frameworks.
EXPOSURE TO MULTIPLE environmental agents, including biologic, chemical, physical, radiologic, and psychosocial stressors, can, under the right circumstances, modify the toxic effects of these same agents acting alone so that combined outcomes are either antagonistic (less than additive) or synergistic (more than additive).1–4 There is empirical evidence that interactive effects from exposure to a mixture of environmental stressors can contribute to three categories of adverse health effects: (1) those where exogenous agents interfere with normal development and distort physiologic function, such as neurobehavioral abnormalities and sex steroid hormonal disruption; (2) those where exogenous agents cause direct cellular damage, such as neurodegenerative diseases and cancer; and (3) those that contribute to illness through a combination of both physiologic disruption and cell damage, for example, in cardiovascular disease.1 Because traditional risk assessment has not routinely taken account of the potential for combined effects from exposure to diverse environmental factors, like those found in the real world, there is growing urgency about the need to develop effective and practical tools for assessing cumulative health risks.5–9
Cumulative risk assessment is a procedure for organizing and analyzing relevant information to examine, characterize, and possibly quantify the combined harmful effects from exposure to a mixture of environmental stressors.7,8 The National Research Council9 recently noted that although the need to evaluate combined risks from environmental stressors is becoming more acute, current practices do not adequately incorporate nonchemical stressors and important aspects of vulnerability into the assessment process. In the following, we provide a brief overview of the diversity of methods used to estimate cumulative health risks, distinguishing between traditional chemical-specific tools and the more recent approaches used to incorporate nonchemical stressors. Prominence is given to techniques that integrate psychological and social stressors, along with concepts of vulnerability, into the risk estimation procedure. The importance of spatial scale for analysis and interpretation of results is discussed, and practical applications of cumulative risk assessment are reviewed.
TECHNIQUES FOR CHEMICAL MIXTURES
In 1986, the Environmental Protection Agency (EPA)10 issued guidelines for evaluating health risks from chemical mixtures, which were updated in 200011 and expanded in 2006.12 The guidelines specified that when evaluating health effects, the first priority was to use evidence for the mixture of concern when it existed. If that was unavailable, the next highest priority was to use information about a similar mixture and, if no such information existed, the subsequent highest priority was to evaluate pairwise interactions between mixture constituents. Finally, if none of the preceding data were available, the default option was to assume that constituent interactions were additive. The 1986 guidelines made a distinction between dose additivity, where the mixture constituents had the same mechanism of action and the same health effects, and response additivity, where mixture constituents had the same health effects but different mechanisms of action. Most cumulative risk assessments since 1986 have focused on chemicals that have similar structure or similar mechanisms of action, such as evaluations of drinking water disinfectants, organophosphate pesticides, polycyclic aromatic hydrocarbons, polychlorinated biphenyls, and dioxins and furans.9
In the absence of biologically based physiologic, toxicokinetic, and toxicodynamic models for the chemical mixture of interest, assessors are forced to rely on science policy decisions that create methodological shortcuts, such as those summarized in Table 1, to estimate cumulative risk.4 When appropriate data are available, the interactive hazard index (HI) approach, which modifies the HI based on a specified function to describe empirical data for the combined effects of mixture constituent pairs, is preferable. The next most preferable method is the toxicity equivalency factor approach, which sums the toxicity of individual mixture components relative to the potency of an index compound. Next in preference is the margin of exposure approach, which uses toxicity equivalency factors to calculate the margin between the estimated exposure and either the reference dose or the reference concentration, as appropriate. If adequate data are not available to support any of these methods, then it is necessary to sum HIs for each mixture constituent, where the HI is calculated by dividing the estimated exposure by either the no observed adverse effect level or the benchmark dose. As a last resort, if no observed adverse effect levels and benchmark doses are not available, assessors can sum HIs for mixture components, where the HI is calculated by dividing the estimated exposure by the reference dose or the reference concentration. The National Research Council13 recently recommended that more emphasis be placed on evaluating cumulative risks from chemicals that contribute to common health effects but which may have different mechanisms of action, such as phthalates.
TABLE 1.
Comparison of Quantitative Methods for Assessment of Cumulative Health Risks from Chemical Mixtures4
| Approach | Methodology |
| HIINT approach using evidence or mathematical theory on pairwise interactions; HIINT = ∑i f(HQ)pair (extensive data requirements) | Assumes sum of interactions between pairs of chemicals represent the whole mixture. Requires pairwise effect data for major constituents of the mixture. |
| Toxicity equivalency factor (TEF) approach; DoseTEQ = ∑(dosei for TEFi) (moderate data requirements) | Assumes the action of each chemical in the mixture is fully represented by an index chemical. Doses of all mixture constituents are treated as equivalent to the weighted sum of the activity of the mixture components. |
| Margin of exposure (MOE) approach using TEF; MOE = NOAEL ÷ DoseTEQ (moderate data requirements) | Assumes addititvity of effects for mixture constituents. Appears to avoid the extrapolations inherent in uncertainty factors, but introduces the added responsibility to make explicit and account for the scientific concerns that gave rise to uncertainty factors in the first place. Single number summary for exposure obscures distributional nature of exposures. |
| HI approach using NOAEL or BMD; HI = (HQ2)i = (Exposure Metrici ÷ NOAELi or BMDi) (minimal data requirements) | Assumes additivity of effects for mixture constituents. NOAELs and BMDs used for comparison instead of RfDs or RfCs, but single comparison value still makes it difficult to discern scientific judgments about uncertain factors and hides distributional nature of exposures. |
| HI approach using RfD or RfC; HI = (HQ2)i = ∑(Exposure Metrici ÷ RfDi or RfCi) (minimal data requirements) | Assumes additivity of effects for mixture constituents. Simplest approach with least resource requirements, but depends on scientific judgment to translate NOAELs or LOAELs into RfDs or RfCs. Not a true quantitative risk assessment, just a single comparison value that obscures scientific judgments about uncertainty factors and masks distributional nature of exposures. |
Note. BMD=benchmark dose; HI=hazard index; HIINT=interaction-based hazard index; HQ=hazard quotient; LOAEL=lowest observed adverse effect level; NOAEL=no observed adverse effect level; RfC=reference concentration; RfD=reference dose; TEQ=toxicity equivalency.
INCORPORATING NONCHEMICAL STRESSORS
As complicated as it is to evaluate interactive effects of chemical mixtures, even simple ones, the degree of difficulty increases dramatically when we attempt to include nonchemical stressors in the analysis. Particular attention has been focused lately on potentially important interactive effects of psychological and social stressors when they occur as part of exposures to complex environmental mixtures.8,14–18 The terms “allostasis” and “allostatic load” have been coined to help conceptualize the cumulative biological toll taken on the human body through physiologic responses to life's everyday stress-provoking demands. Allostasis refers to the adaptive processes that maintain homeostasis by producing mediators such as adrenalin, cortisol, and other chemical messengers that promote adaptation following acute stress. Allostatic load refers to the cumulative cost over time of allostasis, where allostatic overload can lead to serious pathophysiology through wear and tear on the body and brain from being chronically “stressed out.” The allostatic load model has been proposed as a framework for conceptualizing the cumulative biological burden exacted on an individual by allostasis, which is triggered by responses to the exigencies of day-to-day existence, including social conflict and other types of social dysfunction.15,17,18
Although the contribution of psychosocial stressors to cumulative risk and related health disparities is ill defined, there is clear and convincing evidence that health is not evenly distributed across levels of socioeconomic status (SES), and that people who have lower incomes, education, and occupational status, many of whom are people of color, are more likely to be unhealthy and to experience higher rates of morbidity and mortality.19,20 In addition, it is apparent that the burden of pollution all too often falls disproportionately on the disadvantaged and vulnerable,6,21 who also tend to have higher allostatic loads.14,22 The concept of allostatic load may provide a mechanism to link stress-induced biological responses to observed health disparities, and could be a valuable method for incorporating psychosocial stressors into cumulative risk assessments.8,20,22,23
There is empirical evidence that individuals in lower SES strata experience greater chronic stress, have lower perceived control at work, have lower levels of social support, and go through more events considered by them to be stressful.22 Moreover, they are more likely to have a substandard diet, reside in dilapidated housing and less safe neighborhoods, lack access to health care, smoke cigarettes and drink alcohol to excess, and, in general, to live more stressful and less healthful lives.20,21,23 Although these and associated factors undoubtedly contribute to allostatic load, discerning the mechanism by which psychosocial stressors influence cumulative risk and play a role in related health disparities depends, to a significant degree, on the posited analytic framework.24
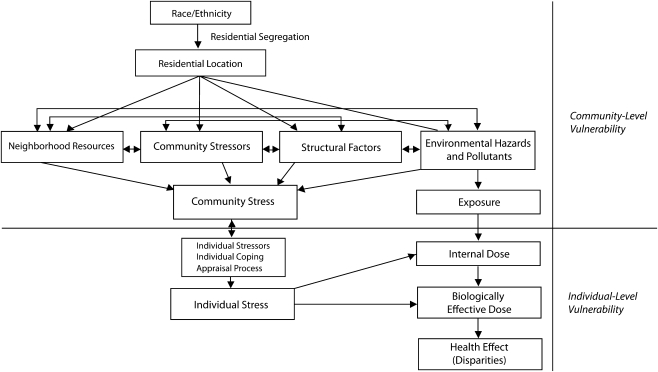
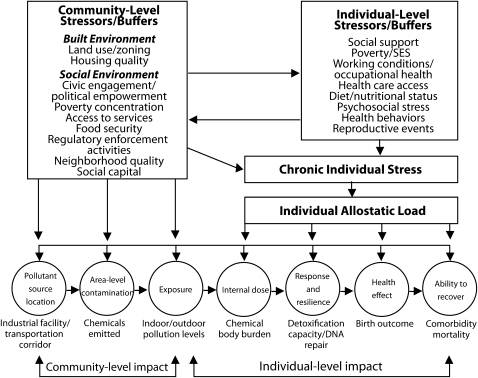
Two recent conceptual frameworks for analyzing combined health effects of chemical and nonchemical stressors conceive a key role for community- and individual-level variables. The first approach, shown in Figure 1, is a multiple effects model that focuses on the role of race and ethnicity in the creation of health disparities.25 The model emphasizes psychosocial stressors and associated chronic stress as mediating factors, and organizes them into categories contributing to community vulnerability or individual vulnerability. Juxtaposed alongside and interconnected is the conventional cascade of events leading from exposure to environmental pollutants, to internal dose, and ultimately to adverse health effects. The interactions among chemical and nonchemical stressors are postulated to account, at least in part, for observed health disparities. The second approach, shown in Figure 2, relies on an exposure–stress–effect framework in which both chemical and nonchemical factors contribute to chronic individual stress and allostatic load, which, in turn, increases individual vulnerability and thereby contributes to subsequent health disparities.23 As part of its causal logic, the model distinguishes between community- and individual-level stressors, buffers, and related health outcomes.
FIGURE 1.
Conceptual model for the combined effects of multiple stressors on health.25
FIGURE 2.
Conceptual model incorporating allostatic load with the combined effects of chemical and nonchemical stressors on health.23
Note. SES = socioeconomic status.
These two theoretical constructs each incorporate multiple levels of analysis and link the combined effects of chemical exposures and psychosocial stressors to explain, at least partially, existing health disparities. In doing so, they extend conventional ideas about exposure assessment beyond the individual to incorporate the broader concept of community sources for both chemical and nonchemical stressors, which are assumed to interact in ways that create unequal stress burdens. This focuses attention on questions about why and how differential cumulative exposures occur in the first place, the conditions under which they give rise to divergent health risks, and the mechanisms by which they ultimately translate into health disparities. Most attempts to explore these and related questions have started with the premise that the uneven geospatial distribution of chemical and nonchemical stressors leads to unequal cumulative exposure and related effects.
GEOSPATIAL DISTRIBUTION OF STRESSORS AND RISKS
A fundamental goal of environmental health sciences is to understand the complicated process by which exposures to environmental agents either cause or contribute to adverse health outcomes, and to intervene where appropriate to prevent or reduce environmentally induced illness and injury. The focus, therefore, of most environmental health research studies and intervention strategies is on three key variables: (1) the magnitude, duration, frequency, and timing of human exposure to environmental stressors, (2) the prevalence or incidence of adverse health effects caused or exacerbated by exposure to environmental agents, and (3) the link between exposure and effect, with particular emphasis on variability in susceptibility and sensitivity for both individuals and communities. All three factors exhibit significant geospatial variability, which means that exposure, effect, and the exposure–effect link are conditioned by geographic location and neighborhood boundaries, the spatial scale of analysis, and the spatial resolution of the aggregated data.26
Geographers have long recognized that results from statistical analyses of these kinds of variables depend on geospatial realities; a situation that they have termed the modifiable areal unit problem (MAUP).27 The implications of the MAUP for environmental health and cumulative risk assessment are noteworthy. For example, the true effect of exposure on disease occurrence is not a biological constant, but is modified by spatial scale. Disease patterns that appear random at one geospatial scale may appear clustered at another, and a regression analysis that is statistically significant at one spatial scale may be insignificant at a different scale. Thus, results of statistical analyses to compare exposure profiles among groups, infer causality, elucidate disease clusters, and characterize health disparities can change substantially depending on spatial boundaries, scale, and resolution. Consequently, a positive statistical finding linking environmental exposure with location of new disease cases suggests a possible association only at that particular spatial resolution of the data—which is to say, the resolution of exposure and health effects data circumscribes the spatial scale of detectable statistical association, thereby setting the context within which results must necessarily be interpreted.26
Studying health disparities and assessing cumulative environmental health risks from chemical and nonchemical stressors must unavoidably span multiple levels of analysis and different-sized geographic units. One way of visualizing the causal pathway from combined exposures through to adverse health outcomes assumes that causation flows from the macro level (e.g., government policies and regulations, market forces, institutional racism) to the meso level (e.g., neighborhood pollution levels, locally built and social environments, community resources) to the micro level (e.g., personal exposure concentrations, body burden measurements, health status, psychological factors, activities and behaviors, physical and demographic characteristics, economic realities).28,29 Choosing which levels and geospatial units to analyze depends on several factors, including the research objective, the causal model selected, the exposures and health outcomes of interest, and the extent to which data are available.29
The availability of data are often the determining factor in decisions about geospatial issues. For example, sociodemographic variables (e.g., age, race/ethnicity, income, education, occupation) as well as indicators of social disadvantage (e.g., uninsured, unemployed, poverty, single mother) and biologic vulnerability (e.g., pregnant women, infants and young children, elderly, infirm) are typically drawn mainly from the US Census30 based on information obtained in the short form (completed by all participants) or the more thorough long form (completed by about 1 in 6 households). This means that these data are only available at certain geographic scales used by the census, such as: block groups; census tracts; Minor Civil Divisions (MCDs); Micropolitan Statistical Areas (μSAs); and Metropolitan Statistical Areas (MSAs). By contrast, to estimate environmental health variables, it is usually necessary to use either public or private databases that summarize information on: (1) human exposures,31 including databases like the National-scale Air Toxics Survey32 or the Toxics Release Inventory;33 (2) body burdens using, for example, the National Report on Human Exposure to Environmental Chemicals34 or the National Health and Nutrition Examination Survey35 (NHANES); and (3) health status, relying on resources such as NHANES, the National Health Interview Survey,36 or the Surveillance Epidemiology and End Results37 program. Examples of the levels of geospatial scale for which data are available from selected sources are provided in Table 2.
TABLE 2.
Examples of Data Sources and Geospatial Levels Available for Analysis of Cumulative Health Risks29
| Data Source | Geospatial Levels Available |
| Demographic, economic, and social variables | |
| US Census | Block group, census tract, MCD, μSA, MSA |
| Environmental exposure | |
| AIRS (Aerometric Information Retrieval System) | County, MSA, state |
| NATA (National-scale Air Toxics Assessment) | Census tract, county, MSA, state |
| TRI (Toxic Release Inventory) | Individual facilities, county, state |
| SDWIS (Safe Drinking Water Info System) | Water system, county, MSA, state |
| SNAP (Superfund NPL Assessment Program) | Site locations, county, MSA, sate |
| Body burden | |
| NHANES (National Health & Nutrition Examination Survey) | Block group, census tract, county, MSA, state |
| National Report on Human Exposure | National reference ranges by pollutant |
| Health status | |
| NHANES | Block group, census tract, county, MSA, state |
| NHIS (National Health Interview Survey) | Block group, census tract, county, MSA, state |
| SEER (Surveillance Epidemiology & End Results) | Block group, census tract (CA only), MSA, state |
Note: MCD=minor civil division; μSA=micropolitan statistical area; MSA=metropolitan statistical area.
CUMULATIVE RISK ASSESSMENT IN PRACTICE
Numerous applications of various forms of cumulative risk assessment for chemical mixtures have been reported over the past decade,3,32,38,39 and summaries of available methods and tools have been published by the EPA12,40–42 and others.29,43 However, assessment of cumulative health effects from a combination of both chemical and psychosocial stressors is still in its infancy,8,9 and substantial efforts are devoted to proposing and testing theoretical paradigms, causal orderings, and analytic frameworks.7,20,23–25,44,45 Without a scientific consensus regarding conceptual approaches and causal pathways to structure empirical inquiry, an assortment of methodologies has been used. Four recent examples serve to illustrate the diversity of techniques currently available: the Cumulative Environmental Hazard Inequality Index46 (CEHII) developed at the University of California–Berkeley; the World Health Organization's (WHO's) Urban Health Equity Assessment and Response Tool47 (Urban HEART); the EPA's Community-Focused Exposure and Risk Screening Tool42 (C-FERST); and the Environmental Justice Strategic Enforcement Screening Tool48 (EJSEAT) from EPA's Office of Enforcement and Compliance Assistance.
The CEHII is a method proposed by scientists at the University of California–Berkeley for creating an index summarizing racial, ethnic, and socioeconomic inequalities from the cumulative effects of multiple environmental hazards.46 Individual environmental inequity indexes are calculated based on unequal burdens of selected environmental hazards for groups defined by race/ethnicity and socioeconomic status. The CEHII combines putative effects of individual environmental hazards using either an additive or multiplicative model, and is calculated using the cumulative proportion of the study population, ranked by area-based racial/ethnic and socioeconomic composition—starting from the most disadvantaged—in combination with the cumulative environmental hazard aggregated based on specific weighting factors. The index can be used to characterize disparities in cumulative impact for relatively large geographic regions and is suitable for application at the regional level, such as counties or metropolitan areas. The CEHII method reduces the dimensionality of the targeted variables by collecting them in functional combinations, which are based on pragmatic considerations and require assumptions about appropriate combination rules and the scale of resulting composite indicators.
The assessment component of WHO's Urban HEART is a method for identifying and analyzing health disparities between people living in different sections of a city or between people belonging to different socioeconomic groups within or across cities.47 Data are collected and analyzed for two categories of “core” indicators: (1) health outcome indicators, including (a) summary indicators, such as infant mortality rate and (b) disease-specific mortality/morbidity indicators, such as age-standardized diabetes death rate per 100 000 persons; and (2) indicators of social determinants of health, including (a) indicators of environmental and physical hazards associated with living conditions, such as access to safe drinking water and sanitation services, (b) indicators of social and human development, such as access to education and health services, (c) indicators of economic status, such as job opportunities and potential for generating income, and (d) indicators of good governance, such as public participation in decision-making and government spending on health. Data for each indicator can, as appropriate, be disaggregated by population group (e.g., sex or age), location (e.g., neighborhood or district), or socioeconomic group (e.g., education or income). The indicators are arrayed in an urban health equity matrix to evaluate the comparative conditions of cities or neighborhoods within cities. Results for each geographic area are presented as color-coded profiles highlighting the highest comparative risks. The findings can be used to identify which geospatial areas or population groups are at highest cumulative risk, and tracking the indicators over time can provide information about trends. Because the dimensionality of the targeted variables is not reduced by forming functional combinations, there are few added measurement assumptions and no scaling beyond rank orders of relative size.
The EPA's C-FERST is a web-based tool—with links to existing EPA information and techniques—that is being developed for use by communities in identifying and prioritizing combined risks from chemical and nonchemical stressors.42 It will incorporate relevant data, maps, model results, and local data collection methods, and will contain exposure-based cumulative risk characterizations. Although the current version focuses primarily on chemical stressors, future versions will include information on interactions and effects of nonchemical agents, such as noise and psychological stress, and exposures and risk will be calculated so that they can be summed across chemical and nonchemical stressors. Where a quantitative assessment spanning multiple environmental stressors is not possible, C-FERST will provide aggregate exposure or risk estimates so that users can examine the data collectively as part of a semiquantitative cumulative risk assessment. This is a mixed measurement approach that combines the two previously described methodologies to form a more complex picture of cumulative risk. It necessarily requires abundant assumptions to sustain it, and its conceptual underpinnings remain a work in progress. Nevertheless, C-FERST offers legitimate promise as an accessible, transparent, and practical assessment tool for use by members of affected communities.
The EJSEAT is intended to provide consistent identification of geographic areas with disproportionately higher burdens of harmful environmental features.48 It is composed of 18 indicator variables divided into four categories: environmental—six indicators; compliance—four indicators; human health—two indicators; and sociodemographic—six indicators. Normalization procedures and a simple algorithm are used to identify areas with elevated EJSEAT scores, which indicate a high burden of dangerous or undesirable conditions. Values for all 18 EJSEAT indicator variables, which are derived from publicly available databases, have been obtained by the EPA for each of the approximately 65 000 census tracts in the United States.
CONCLUSIONS AND RECOMMENDATIONS
Development of appropriate procedures for evaluating combined threats from multiple environmental stressors is vital for understanding and resolving issues like health disparities and environmental injustices.6,8,9,49,50 Although techniques for assessment of combined effects from chemical mixtures have been around for more than 20 years, they are still confined largely to relatively simple combinations. The formal inclusion of nonchemical stressors in cumulative risk assessments, specifically factors like residential crowding, neighborhood crime, and levels of social support, is a comparatively recent development that is hindered by unavailability of appropriate data, a deficiency of mechanistic understanding, and lack of consensual or verified analytic frameworks to direct research activity. We believe development of workable processes and practices for assessing cumulative health risk depends on implementation of a coordinated, overarching strategy that methodically works through a series of logical steps.
Identify high-priority communities and populations likely to be at increased cumulative risk from exposure to a mixture of chemical and nonchemical stressors. This step could be accomplished at a national scale using an expert panel to prioritize generic at-risk populations (e.g., children who live in disadvantaged circumstances near major sources of pollution) and locations (e.g., poor, inner city neighborhoods), or it could be done at a local scale using available information on pollution sources, ambient concentrations, and socioeconomic characteristics to distinguish high-risk situations (e.g., immigrant families who are migrant farm workers) and settings (e.g., an economically depressed community adjacent to major freeways, industrial facilities, and abandoned waste sites) (for example, WHO's HEART47 and EPA's EJSEAT48).
Specify a prescribed analytic framework that formalizes postulated causal factors and pathways that will serve as a guide for collection and interpretation of empirical data. This step requires explicit commitment to a particular conceptual model that provides a simplified inventory of critical assumptions, concepts, indicators, and propositions, including a schematic representation depicting postulated connections among independent variables and between independent and dependent variables (for example, Linder and Sexton24).
Undertake a coordinated research effort centered on the targeted population or community, including laboratory and field research aimed at (1) elucidating the magnitude, duration, frequency, and timing of relevant exposures, (2) determining whether mixture-related health effects are additive, antagonistic, or synergistic, and (3) explicating important interactive mechanisms of toxicity among mixture components. The emphasis must be on the complex, day-to-day exposures of real people that are the focal point of the cumulative risk assessment. Studies should answer the important (but difficult) questions, even if only imprecisely, rather than trying to answer the less important (but easier) questions definitively (for example, Callahan and Sexton8 or the National Research Council's 2009 Report9).
Conduct a thorough assessment of cumulative health risks in the target population or community using the chosen analytic framework as a guide and relying on the best available data and most up-to-date scientific methods. Bridging the gap between the needs of risk assessors and existing scientific knowledge and understanding will likely require numerous science policy decisions to resolve critical uncertainties, which means that results may necessarily be semiquantitative or qualitative. Nevertheless, it is imperative to gain the experience and learn the lessons needed to eventually construct a workable system for assessing the severity of cumulative health risks in complicated, real-world situations (for example, EPA's C-FERST47).
Use empirical and conceptual results to modify, revise, or discard the analytic framework as a practical guide to assess cumulative health risks. The goal is to appraise the framework rigorously and refine or reject it based on a thorough evaluation of relevant research findings and knowledge gained from conducting cumulative risk assessments in the field (for example, Linder and Sexton24).
Future progress is contingent not only on adequate funding to carry out the necessary studies, but also on advances in conceptual approaches, theoretical paradigms, and diagnostic frameworks that structure the research enterprise appropriately—helping us to ask the right questions, design the right studies, and draw the right conclusions.
Acknowledgments
This work was partially supported by the US EPA. The authors have no financial conflicts to declare.
The authors wish to acknowledge the helpful comments of Michael A. Callahan, MDB, Inc. and Onyemaechi Nweke, US EPA.
References
- 1.Carpenter DO, Arcaro K, Spink DC. Understanding the human health effects of chemical mixtures. Environ Health Perspect. 2002;110(suppl 1):25–42 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kortenkamp A, Faust M, Scholze M, et al. Low-level exposure to multiple chemicals: reason for human health concerns. Environ Health Perspect. 2007;115(suppl 1):106–114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Monosson E. Chemical mixtures: considering the evolution of toxicology and chemical assessment. Environ Health Perspect. 2005;113(4):383–390 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sexton K, Hattis D. Assessing cumulative health risks from exposure to environmental mixtures—three fundamental questions. Environ Health Perspect. 2007;115(5):825–832 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.U.S. Environmental Protection Agency Guidance on Cumulative Risk Assessment, Part 1 Planning and Scoping. Washington, DC: EPA Science Policy Council; 1997 [Google Scholar]
- 6.Institute of Medicine Toward Environmental Justice: Research, Education, and Health Policy Needs. Washington, DC: National Academy Press; 1999 [PubMed] [Google Scholar]
- 7.U.S. Environmental Protection Agency Framework for Cumulative Risk Assessment. Washington, DC: EPA Risk Assessment Forum; 2003 [Google Scholar]
- 8.Callahan MA, Sexton K. If cumulative risk assessment is the answer, what is the question? Environ Health Perspect. 2007;115(5):799–806 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.National Research Council Science and Decisions: Advancing Risk Assessment. Washington, DC: National Academies Press; 2009 [PubMed] [Google Scholar]
- 10.U.S. Environmental Protection Agency Guidelines for the Health Risk Assessment of Chemical Mixtures. Washington, DC: EPA Risk Assessment Forum; 1986 [Google Scholar]
- 11.U.S. Environmental Protection Agency Supplementary Guidance for Conducting Health Risk Assessment of Chemical Mixtures. Washington, DC: EPA Risk Assessment Forum; 2000 [Google Scholar]
- 12.U.S. Environmental Protection Agency Considerations for Developing Alternative Health Risk Assessment Approaches for Addressing Multiple Chemicals, Exposures, and Effects. Washington, DC: National Center for Environmental Assessment; 2006 [Google Scholar]
- 13.National Research Council Phthalates and Cumulative Risk Assessment: The Tasks Ahead. Washington, DC: National Academies Press; 2008 [PubMed] [Google Scholar]
- 14.McEwen BS. Allostasis and allostatic load: implications for neuropsychopharmacology. Neuropsychopharmacology. 2000;22(2):108–124 [DOI] [PubMed] [Google Scholar]
- 15.McEwen BS. Stressed or stressed out: what is the difference? J Psychiatry Neurosci. 2005;30(5):315–318 [PMC free article] [PubMed] [Google Scholar]
- 16.McEwen BS. Physiology and neurobiology of stress and adaptation: central role of the brain. Physiol Rev. 2007;87:873–904 [DOI] [PubMed] [Google Scholar]
- 17.McEwen BS, Wingfield JC. The concept of allostasis in biology and medicine. Horm Behav. 2003;43:2–15 [DOI] [PubMed] [Google Scholar]
- 18.Seeman TE, McEwen BS, Rowe JW, et al. Allostatic load as a marker of cumulative biological risk: MacArthur studies of successful aging. Proc Natl Acad Sci USA. 2001;98(8):4770–4775 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Fiscella K, Williams DR. Health disparities based on socioeconomic inequalities: implications for urban health care. Acad Med. 2004;79(12):1139–1147 [DOI] [PubMed] [Google Scholar]
- 20.deFur PL, Evans GW, Cohen Hubal EA, et al. Vulnerability as a function of individual and group resources in cumulative risk assessment. Environ Health Perspect. 2007;115(5):817–824 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sexton K. Sociodemographic aspects of human susceptibility to toxic chemicals: do class and race matter for realistic risk assessment? Environ Toxicol Pharmacol. 1997;4:261–269 [DOI] [PubMed] [Google Scholar]
- 22.Szanton SL, Gill JM, Allen JK. Allostatic load: a mechanism of socioeconomic health disparities? Biol Res Nurs. 2005;7(1):7–15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Morello-Frosch R, Shenassa ED. The environmental “riskscape” and social inequality: implications for explaining maternal and child health disparities. Environ Health Perspect. 2006;114(8):1150–1153 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Linder SH, Sexton K. Conceptual models for cumulative risk assessment. Am J Public Health. 2011; 101(suppl 1):S74–S81 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gee GC, Payne-Sturges DC. Environmental health disparities: a framework integrating psychosocial and environmental concepts. Environ Health Perspect. 2004;112(17):1645–1650 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sexton K, Waller LA, McMaster RB, et al. The importance of spatial scale for environmental health policy and research. Hum Ecol Risk Assess. 2002;8(1):109–125 [Google Scholar]
- 27.Openshaw W. The Modifiable Areal Unit Problem. Concepts and Techniques in Modern Geography No. 38. Norwich, CT: Geo Books; 1984 [Google Scholar]
- 28.Schulz A, Northridge ME. Social determinants of health: implications for environmental health promotion. Health Educ Behav. 2004;31(4):455–471 [DOI] [PubMed] [Google Scholar]
- 29.Soobader M, Cubbin C, Gee GC, et al. Levels of analysis for the study of environmental health disparities. Environ Res. 2006;102:172–180 [DOI] [PubMed] [Google Scholar]
- 30.U.S. Census Bureau Statistical Abstracts. Available at: www.census.gov. Accessed June 11, 2010
- 31.Sexton K, Selevan SG, Wagener DK, et al. Estimating human exposures to environmental pollutants: availability and utility of existing databases. Arch Environ Health. 1992;47(6):398–407 [DOI] [PubMed] [Google Scholar]
- 32.U.S. Environmental Protection Agency National Air Toxics Assessments. Technology Transfer Network Air Toxics Web Site. Available at: www.epa.gov/ttn/atw/natamain/. Accessed June 9, 2010
- 33.U.S. Environmental Protection Agency Toxic Release Inventory (TRI) Program. Available at: www.epa.gov/tri. Accessed June 3, 2010
- 34.Centers for Disease Control and Prevention National Report on Human Exposure to Environmental Chemicals. Available at: www.cdc.gov/exposurereport/. Accessed June 3, 2010
- 35.Centers for Disease Control and Prevention National Health and Nutrition Examination Survey. Available at: www.cdc.gov/nchs/nhanes.htm. Accessed June 3, 2010
- 36.Centers for Disease Control and Prevention National Health Interview Survey. Available at: www.cdc.gov/nchs/nhis.htm. Accessed June 3, 2010
- 37.National Cancer Institute Surveillance Epidemiology and End Results. National Institutes of Health, U.S. Department of Health and Human Services; Washington, DC: Available at: http://seer.cancer.gov/. Accessed June 9, 2010 [Google Scholar]
- 38.Linder SH, Marko D, Sexton K. Cumulative cancer risk from air pollution in Houston: disparities in risk burden and social disadvantage. Environ Sci Technol. 2008;42(12):4312–4322 [DOI] [PubMed] [Google Scholar]
- 39.Seeman T, Merkin SS, Crimmins E, et al. Education, income, and ethnic differences in cumulative biological risk profiles in a national sample of U.S. adults. Soc Sci Med. 2008;66(1):72–87 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.U.S. Environmental Protection Agency Concepts, Methods and Data Sources for Cumulative Health Risk Assessment of Multiple Chemicals, Exposures and Effects: A Resource Document. Washington, DC: National Center for Environmental Assessment; 2007 [Google Scholar]
- 41.Barzyk TM, Conlon KC, Chanine T, et al. Tools available to communities for conducting cumulative exposure and risk assessments. J Expo Sci Environ Epidemiol. 2010;20:371–385 [DOI] [PubMed] [Google Scholar]
- 42.Zartarian VG, Schultz BD. The EPA's human exposure research program for assessing cumulative risk in communities. J Expo Sci Environ Epidemiol. 2010;20(4):351–358 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Payne-Sturges D, Gee GC. National environmental health measures for minority and low-income populations: tracking social disparities in environmental health. Environ Res. 2006;102:154–171 [DOI] [PubMed] [Google Scholar]
- 44.Payne-Sturges D, Gee GC, Crowder K, et al. Workshop summary: connecting social and environmental factors to measure and track environmental health disparities. Environ Res. 2006;102:146–153 [DOI] [PubMed] [Google Scholar]
- 45.Morello-Frosch R, Lopez R. The riskscape and the color line: examining the role of segregation in environmental health disparities. Environ Res. 2006;102:181–196 [DOI] [PubMed] [Google Scholar]
- 46.Su JG, Morello-Frosch R, Jesdale BM, et al. An index for assessing demographic inequalities in cumulative environmental hazards with application to Los Angeles, California. Environ Sci Technol. 2009;43(20):7626–7634 [DOI] [PubMed] [Google Scholar]
- 47.World Health Organization Urban HEART: Urban Health Equity Assessment and Response Tool. WHO Center for Health Development. Kobe, Japan: WHO Publications; 2010 [Google Scholar]
- 48.National Environmental Justice Advisory Council. Nationally Consistent Environmental Justice Screening Approaches. Report submitted to the Office of Environmental Justice, U.S. Environmental Protection Agency; Washington, DC: NEJAC; May 2010 [Google Scholar]
- 49.National Environmental Justice Advisory Council Ensuring Risk Reduction in Communities with Multiple Stressors: Environmental Justice and Cumulative Risks/Impacts. Report submitted to the Office of Environmental Justice, U.S. Environmental Protection Agency; Washington, DC: NEJAC; 2004 [Google Scholar]
- 50.Sexton K, Linder SH. The role of cumulative risk assessment in decisions about environmental justice. Int J Environ Res Public Health. 2010;7(11):4037–4049 [DOI] [PMC free article] [PubMed] [Google Scholar]