Abstract
Objectives. Parents need meaningful and actionable information if they are to reduce household environmental health risks to their children. To address this issue, we tested the effectiveness of a multi-risk social/cognitive intervention on rural low-income parents' (1) environmental health self-efficacy and (2) stage of environmental health precautionary adoption.
Methods. Biomarker (lead, cotinine) and household samples (carbon monoxide, radon, mold/mildew, and drinking water contaminants) were collected from 235 families (399 adults, 441 children) in Montana and Washington states. Families were randomly assigned to intervention or control groups; intervention families received 4 visits from public health nurses who provided tailored information and guidance to parents; controls received usual and customary public health services.
Results. At 3 months, the intervention group had significantly higher scores on (1) all 6 risk-specific self-efficacy subscales (P < .01), (2) general environmental health self-efficacy (P < .001), (3) 5 of 6 risk-specific precaution adoption subscales (P < .05), and (4) general environmental health precaution adoption (P < .001).
Conclusions. The intervention yielded significant improvements in both outcomes. This evidence supported the need for a policy discussion addressing the added value that broadbased public health nurse interventions might bring to children's environmental health.
In previous work in rural Montana and Washington states, low-income families reported that much of the environmental health information they received was neither meaningful nor actionable.1–4 Parents viewed household environmental risks holistically, yet they almost always received agent (e.g., radon) or condition (e.g., asthma) specific educational pamphlets. Many parents reported being concerned about household risks, but felt “stuck” in their circumstances and unsure about what risk reduction steps to take; they asked for practical suggestions about what they could do to protect their children.1 These findings were consistent with those from other behavioral scientists who found that context- and image-based environmental health messages (e.g., Centers for Disease Control and Prevention [CDC] Healthy Homes portal) were often perceived as more meaningful than agent-focused information.5–10 This previous research also yielded evidence that when provided with detailed protocols, public health nurses had the requisite knowledge base to provide families with appropriate environmental risk reduction information. To further analyze these issues, a randomized controlled trial was designed to test the effectiveness of a household environmental health intervention on parents’ self-efficacy and precautionary actions.
The study used county level public health nurses to deliver the intervention. Although many similarities exist between public health nurses practicing in rural versus urban health departments, those in rural settings are more likely to work across programs and settings.11,12 In many places, rural public health nurse practice still involves an intimacy with the community that plays out in different ways across programs, initiatives, and stakeholder groups.13,14 This study focused exclusively on rural public health nurses because of their generalist role and daily involvement with locally defined public health concerns. To our knowledge, this study represented the first effort nationally to examine the effectiveness of a multirisk environmental health intervention delivered exclusively by public health nurses employed in local health departments.
The primary aim of the study was to analyze the effectiveness of a public health nurse delivered multiagent intervention on parents’ (1) environmental health self-efficacy and (2) stage of environmental health precaution adoption. We selected these 2 social/cognitive outcomes because they are both well-established correlates of improved health outcomes.15–17 A secondary aim of the study was to report household (carbon monoxide, radon, mold/mildew, water contaminants) and biomarker (lead, cotinine) data, explicating the frequency and magnitude of household environmental health risks in a previously unstudied sample of rural low-income children. In this article, the household and biomarker findings are presented first because they inform the intervention analyses.
METHODS
The translational environmental research in rural areas (TERRA) model was used as the conceptual foundation of the study. This model is predicated on the assumption that environmental risk reduction interventions have the potential to favorably impact both (1) the frequency and magnitude of environmental risks, and (2) family members’ perceptions of risk (e.g., mental models). Subsequently, these risks and risk perceptions are associated with health/behavioral outcomes that are proximal (e.g., precautionary actions to improve indoor air quality) or distal (e.g., changes in children's respiratory symptoms) in nature. Details addressing the development and utility of the TERRA model are cited elsewhere.4
Recruitment and Enrollment
All participants resided in either Gallatin County, Montana (2009 population: 89 824) or Whatcom County, Washington (2009 population: 196 529). Shared demographic features between the 2 counties included similar homeownership rates (62.4% Gallatin, 63.4% Whatcom), median housing values ($143K Gallatin, $156K Whatcom), and median household incomes ($53K Gallatin, $49K Whatcom).18 Participants were recruited from county public health departments (28%); Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) clinics (22%); and community contacts (50%). Participants were defined as rural and considered eligible to participate if they lived outside the city limits. This criterion was established to reach households receiving county versus city level services. Other eligibility criteria included (1) household income at or less than 250% of the federal poverty level, (2) a child aged 7 years or younger, (3) English language literacy, and (4) potable water from a nonmunicipal source. The water criterion enabled us to focus exclusively on households with private wells or small water systems (e.g., 1 well serving several homes or mobile homes); such systems have little regulatory oversight. Families received free household testing and gift cards totaling $40. Consent was obtained by all household adults and children (i.e., age appropriate assent). Protocols were approved by institutional review boards at the respective universities.
The enrollment target was set at 228 households. This target assumed 80% power, 15% attrition, 2-sided α at 0.05, a mean difference between groups of 0.4 with a SD of ±1 for environmental health self-efficacy, and a 20% absolute difference in the proportion reporting action for environmental health precaution adoption. These calculations yielded a minimum sample size of 99 households per group.
Data Collection and Intervention
Data were collected at baseline (T1) and at 3 months (T2). At the T1 visit, household data (water samples, carbon monoxide [CO], in-wall humidity, evidence of moisture damage, and radon [in Gallatin County only]) were collected during a home assessment. Airborne radon was determined not to be a risk factor in Whatcom County; thus samples were not collected at that performance site. Drinking water samples were collected and handled in accordance with standard methods for drinking water analyses19; Environmental Protection Agency certified laboratories performed all analyses. Water quality parameters included bacteria (total coliform and Escherichia coli), nitrate, nitrite, and basic metals (calcium, magnesium, sodium, iron, zinc, manganese, copper, lead, and arsenic); anions (sulfate, chloride, fluoride), hardness, alkalinity, pH, specific conductivity, and 2 screening tests. One test determined the presence/absence of hydrocarbons from fuels, solvents, and other volatile organic compounds, and the other the presence/absence of pesticides and other synthetic organic compounds. Compounds detected by the screening tests were identified and quantified. These tests were designed for the economical screening of private well water. CO was measured at all combustion sources (e.g., wood stove) using a Dwyer Series 450 Carbon Monoxide Monitor (Michigan City, IN; range = 0–2000 ppm). In-wall humidity (as a proxy measure for mold/mildew risk) was measured using a protimeter (General Electric Surveymaster, Billerica, MA). Airborne radon was measured using a short-term collection device (α Energy Labs, Carrollton, Texas) placed in the lowest level of the home where children played. All radon levels of 4 picocuries per liter or greater were re-tested using a 90-day test. In addition to household samples, 2 biomarkers were taken from children aged 7 years or younger. Salivary cotinine as a measure of tobacco smoke exposure was measured by Salimetrics (State College, Pennsylvania). Blood lead was measured by Tamarac Laboratories (Denver, Colorado). Pilot tests of study measures were completed before the initiation of this study. Additional pilot work was also conducted to address the feasibility and transport issues associated with shipping biologic and chemical samples from rural settings to their respective analysis laboratories.
Ten public health nurses delivered the intervention. All the public health nurses were female, held either a bachelor's or master's degree in nursing, and had worked as a public health nurse an average of 12.9 years. The nurses completed 10–12 hours of training that included information addressing the study goals, timeline, intervention sequence, and how to deliver a tailored intervention. Weekly follow-up meetings were held between the study manager and the nurses. Additional details addressing the public health nurses’ background and training are cited elsewhere.20 The intervention involved 4 home visits; visits were completed over a 4- to 6-week period between T1 and T2. Each visit lasted approximately 1 hour. Public health nurses were trained using standard protocols and monitored by on-site coordinators. The intervention was developed using materials from CDC's Healthy Homes Initiative.10 During visits, the public health nurse used an interactive book to guide the family through a review of risks room by room. Each family's household/biomarker results were posted into window cutouts throughout the book. For example, the CO results were posted inside a window on the book page showing pictures of furnaces and stoves. This format ensured consistency in intervention quality/dose, yet enabled the provision of tailored health messages. Health information was tailored by having the nurse first differentiate between household/biomarker test results that were below versus above the threshold value (or presence vs absence). Standard messages were used to discuss all results within threshold levels; messages were also developed for tests that were frequently found to be above the threshold (e.g., airborne radon). Messages addressing household test results that far exceeded the threshold and/or requiring unusually complex explanations were developed by having the public health nurse work with the appropriate technical expert on the study team (e.g., water quality expert). Participants received increasingly complex environmental health information (e.g., CO at visit 1, water quality at visit 4) at successive visits. Participants with positive water sample results (e.g., E. coli) were provided with tailored information pertaining to specific contaminants. Precautionary actions ranged from guidance on well disinfection to how to obtain low-cost, point-of-use filtration devices; all water-related guidance to families was provided by an environmental engineer with water system and public health expertise. All precautionary actions recommended by the public health nurses were intended to be (1) effective and (2) no cost/low cost. In those rare instances in which no low-cost options were effective or available, participants were provided with additional information addressing local home weatherization and utility payment programs.
Those in the control group received a letter that included their test results and threshold values for each risk. Phone numbers for the health department and other resources were also provided. A few participants in the control group had test results posing an immediate risk (e.g., high CO levels); these situations were managed on a case-by-case basis by study personnel. To preserve randomization, such cases were analyzed according to original group assignment, thus biased toward the null.
Measures
Demographic and socioeconomic measures included years of formal education, rent versus homeowner status, health insurance status, and current occupation(s). Questions were also asked regarding activities in the home associated with environmental health risks (e.g., hobbies, crafts, contaminated work clothes). The study focused on 2 proximal outcomes that were measured in the primary household adult (e.g., primary family member caring for children; typically the mother or grandmother): (1) environmental health self-efficacy and (2) environmental health precaution adoption. Self-efficacy was defined as the belief that one's actions could produce desired results.21 Bandura's Guide for Constructing Self-Efficacy Scales was used to develop and pilot test the self-efficacy instrument.22,23 Self-efficacy (range 0–100) was measured 2 ways: as general environmental health self-efficacy (1 subscale) and as risk-specific self-efficacy (6 subscales addressing 6 risks). Eleven items measured general environmental health self-efficacy; 18 items were risk-specific (6 risks). Each risk-specific self-efficacy score addressed 3 facets of risk reduction (i.e., identify the risk, determine if home is safe, and act to reduce exposure). The instrument was circulated among environmental health experts to assess content validity.22 Reliability was established for general environmental health (Cronbach's α ≥ 0.80); α values ranged from 0.78 to 0.94 for the risk-specific subscales.
Environmental health precaution adoption was conceptualized as one's stage of precautionary action and measured using Weinstein's Precaution Adoption Process Model.17,24,25 Like many related stage-of-change concepts,26,27 precautionary action was conceptualized as a cognitive behavioral process ranging from (1) unaware of issue, (2) unengaged by issue, (3) decided not to act, (4) decided to act, to (5) already taken action. Precaution adoption was measured 2 ways: as general environmental health precaution adoption (sum of agents with forward progress) and as risk-specific precaution adoption (6 risks). Risk-specific precaution adoption was measured by forward progress, regardless of how many steps forward (dichotomous outcome: yes or no). General environmental health precaution adoption was measured by totaling risk-specific precaution adoption and then defined as forward progress on at least 3 of the 6 risks. The approach to measurement was consistent with that of Weinstein et al.25 addressing precautionary behaviors in response to radon risks.
Statistical Analysis
Data verification was performed using double data entry for a random sample of 10%; this procedure yielded an error rate of less than 2%. Analyses were based on original group allocation. Analyses focused on intervention effectiveness at T2 (3 months). Continuous data were summarized as means ±SDs and categorical data as frequencies (percentages). Descriptive variables included gender, age, race, ethnicity, years of education, annual household income, marital status, general housing condition (per data collector), and homeowner status (rent vs own). Outcome measures included mean self-efficacy score for each risk (3 questions), mean general behavior score (11 questions), environmental health precaution adoption (yes/no) for each risk, and general environmental health risk precaution adoption (defined as precaution adoption for 3 or more risks).
The purpose of the analysis was to test the hypothesis that relative to controls, those in the intervention group would have significantly improved scores for self-efficacy and precaution adoption; observations were taken at baseline (preintervention) and at 3 months (postintervention). To examine treatment effects, both linear (i.e., self-efficacy) and logistic (i.e., general environmental health precaution adoption and risk-specific precaution adoption) generalized estimating equation (GEE) models (SAS, 9.1 PROC GENMOD, SAS Institute, Cary, North Carolina) were used. For analyses examining self-efficacy, the T1 value was included as a covariate to adjust for any differences among participants at baseline. Precaution adoption was defined as progress from T1, eliminating the need to adjust for baseline. For each outcome, separate GEE models were run, including group assignment (control = 0, intervention = 1) and site (Whatcom County = 0, Gallatin County = 1), and the interactions between these variables as independent variables. For linear GEE models, group means, SDs, and χ2 P values were reported. The linear GEE coefficients (The linear GEE coefficient (b) and the corresponding 95% confidence intervals (CIs) were the basis of statements regarding trends about group differences in outcomes. 95% confidence intervals [CIs]) were the basis of statements regarding trends about group differences in outcomes. For logistic GEE models, the odds ratio and corresponding 95% CIs based on empirical self-efficacy scores and χ2 P value were reported. Results presented were based on reduced models eliminating all nonsignificant interaction terms. Nonsignificant terms were not reported.
Potential confounding by baseline variables (household income in $5000 increments and education) was examined by assessing (1) whether inclusion of the variable changed the group and group*time coefficients by greater than 10% and (2) if the χ2 P value for the parameter was significant (P < .05). For models in which income and/or education were significant, the results reported for group were adjusted for income or education. For households that attrited, all data from the last observed visit were carried forward and used for any incomplete visits, yielding a conservative estimate of the intervention and possibly underestimating the self-efficacy scores for the GEE model parameters. Aside from missing data due to attrition, less than 1% of other data were missing.
RESULTS
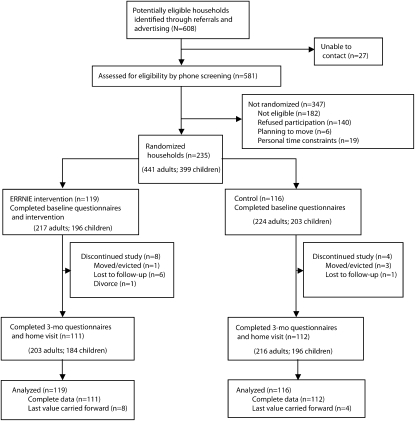
Of 608 referrals, 581 were available for eligibility screening, 336 were eligible, and 235 were randomized and enrolled (Figure 1). Among the 81 eligible referrals who declined participation, primary reasons cited included personal time constraints (25%), primary contact not interested (17%), spouse or partner not interested (14%), planning to move (7%), and nurse coming into home too invasive (7%). Twelve households (8 intervention and 4 control) dropped out between baseline and T2. Ninety-seven percent of intervention households completed the entire intervention (all 4 visits). Participants included 235 primary adults, 206 secondary adults (e.g., spouse, partner, grandparent), and 399 children ≤ 7 years of age. The intervention group (n = 119) and control group (n = 116) were balanced in regard to demographics (gender, age, race, ethnicity, education level of primary adult), socioeconomic (household income), and household (living condition, rent/own) characteristics. Primary adults in the study were generally female (intervention = 93%; control = 92%), non-Hispanic White (intervention = 91%; control = 90%), and married (intervention = 76%; control = 82%). The race/ethnicity distribution of the sample was similar to county level census data for Gallatin and Whatcom counties.28,29 The average age ±SD of primary adult participants for the intervention and control groups was 32.9 ±7.1 and 33.1 ± 6.5 years, respectively. The annual household income for one quarter of the households was less than $25 000 (intervention: 29%; control: 26%) and approximately half reported annual household incomes between $25 000 and $50 000 (intervention = 52%; control = 55%). The average ±SD years of education of the primary adult was 15.2 ±2.3 for the intervention group and 15.0 ±2.3 for the control group. Housing condition was rated “good” (vs poor or moderate) for 74% of intervention households and 69% of control households; more than half of the participants owned (vs rented) their homes (intervention = 60%; control = 51%).
FIGURE 1.
Flow of participant households: household environmental health intervention delivered by rural public health nurses, Gallatin County, MT, and Whatcom County, WA, 2009.
Note. ERRNIE = environmental risk reduction through nursing interventions and education.
Household Samples and Biomarkers
Analyses addressing household tests by group are listed in Table 1. The occurrence and type of contaminants found were similar between groups. Sixty-four percent of households had at least 1 risk above threshold levels; 30% had at least 1 water-related risk. Total coliforms were present in 39 (17%) of water samples; E. coli was found in 2%. Four homes had elevated nitrate levels (range = 12.8–15.4 mg/L). Elevated arsenic levels ranging from 0.01 to 0.074 milligrams per liter were found in 17 (7%) of the homes. Pesticides found in 6 (3%) homes included aldrin/dieldrin, Bis (2-ethylhexl) phthalate, and trace amounts of chlordane. Volatile organic compounds including trace amounts of chloroform, toluene, di-n-butyl phthalate, and trihalomethanes were found in 4 (2%) homes. Elevated 2-day airborne radon levels were found in 28% (35/127) of Gallatin County households (range = 4.2–92.5 pCi/L). Because radon was not considered a risk in Whatcom County (verified by pilot work), households in that county were not tested. Elevated in-wall humidity levels and/or physical signs of moisture damage were noted in 74 (31%) households; wood moisture equivalent (WME) readings above the threshold (i.e., 20% WME) were found in 38 of these 74 households. Elevated CO readings (range = 40–264 ppm) were recorded for 20 (9%) of the households. Cotinine was elevated in 12 (3%) of the 388 children tested (range = 5.1–86.32 ng/mL). Three (< 1%) of the 350 children tested had elevated blood lead levels (range = 5.5–9.2 μg/dL).
TABLE 1.
Household Environmental Health Risk Profiles at Baseline: Household Environmental Health Intervention Delivered by Rural Public Health Nurses, Gallatin County, MT, and Whatcom County, WA, 2009
| Intervention Group |
Control Group |
|||
| Attribute | No. (%) | Elevated Value Range | No. (%) | Value Range |
| No. households | 119 | 116 | ||
| Carbon monoxide ≥ 35 ppma | 7 (8) | 51-116 | 13 (15) | 40–264 |
| Water contaminants | 36 (30) | 34 (29) | ||
| Coliforms | 20 (17) | 19 (16) | ||
| Escherichia coli | 2 (2) | 4 (3) | ||
| Lead ≥ 0.015, mg/L | 1 (< 1) | 0.02 | 0 (0) | – |
| Nitrate ≥ 10, mg/L | 3 (3) | 12.8–14.7 | 1 (1) | 13.2 |
| Copper ≥ 1.3, mg/L | 0 (0) | – | 1 (1) | 1.7 |
| Arsenic ≥ 0.01, mg/L | 7 (6) | 0.01–0.05 | 10 (9) | 0.01–0.07 |
| Fluoride ≥ 2,b mg/L | 0 (0) | – | 3 (3) | 2.12–7.85 |
| Hardness ≥ 500, mg/L | 1 (< 1) | 559 | 0 (0) | – |
| Pesticidesc | 5 (4) | 1 (1) | ||
| Herbicidesd | 0 (0) | 1 (1) | ||
| VOCe | 3 (3) | 1 (1) | ||
| In-wall humidity ≥ 18% WMEf | 37 (31) | 37 (32) | ||
| 2-d airborne radon > 4.0 pCig | 19 (31) | 5.0–89.4 | 16 (26) | 4.2–92.5 |
| Biomarkers in children | ||||
| No. children | 199 | 200 | ||
| Cotinine > 5 ng/mLh | 10 (5) | 5.1–86.3 | 2 (1) | 23.8–28.2 |
| Lead ≥ 5 μg/dLi | 2 (1) | 5.5–9.1 | 1 (< 1) | 5.7 |
Note. VOC = volatile organic compounds; WME = wood moisture equivalent.
65 households (35 intervention, 30 control) had only electric utilities.
Fluoride not tested for 27 households (15 intervention, 12 control).
Pesticides by type found per group: intervention: trace amounts of chlordane, aldrin/dieldrin with unknown petroleum byproducts; control: bis(2-ethylhexyl) phthalate.
Herbicides by type found in control group: picloram.
VOC by types found per group: intervention: trace amounts of toluene, chloroform, bis(2-ethylhexyl) phthalate, di-n-butyl phthalate; control: trace amounts of trihalomethanes.
Elevated in-wall humidity required WME ≥ 18% and physical signs of moisture damage.
Radon testing was not conducted for the 108 households in Whatcom County, where levels are known to be below Environmental Protection Agency safety levels.
Saliva samples for cotinine testing were not collected from 4 children in the intervention group and 7 children in the control group.
Blood samples for lead testing were not collected from 21 children in the intervention group and 28 children in the control group.
Impact of Intervention
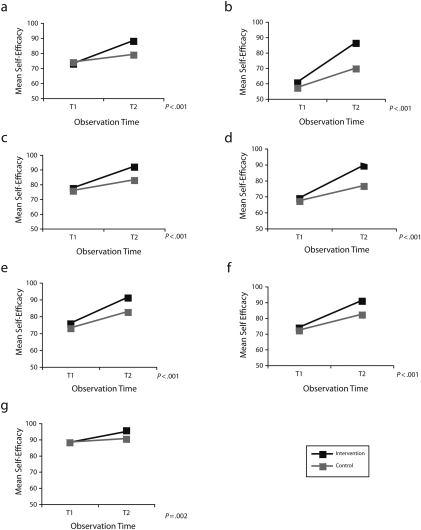
Results addressing self-efficacy scores are presented in Figure 2. The intervention yielded significantly higher self-efficacy scores for general environmental health self-efficacy and all 6 risk-specific self-efficacy scores. Comparing the intervention to the control group at 3 months, general environmental health self-efficacy scores (mean ±SD) were significantly higher for the intervention group (intervention = 88.0 ±2.1; control = 78.8 ±6.4; P < .001). The intervention increased scores for general environmental health self-efficacy by 9 to 10 points (b = 9.5; 95% CI = 6.5, 12.5). All risk-specific self-efficacy scores were statistically significantly higher for the intervention group compared with the control group. The greatest differences (mean ±SD) at T2 were found for radon (intervention = 86.2 ±22.1; control = 69.7 ±27.7; P < .001) and lead (intervention = 89.2 ±15.6; control = 76.6 ±22.2; P < .001), where the intervention was associated with an increase in radon self-efficacy scores of 14 (b = 14.1; 95% CI = 8.5, 19.6) and lead self-efficacy scores of 12 (b = 12.0; 95% CI = 7.4, 16.0). Similar differences in mean self-efficacy scores between groups at 3 months were found for CO, in-wall humidity, and water contaminants: CO (intervention = 91.9 ±13.5; control = 82.9 ±19.1; P < .001), in-wall humidity (intervention = 90.8 ±14.2; control = 82.0 ±16.7; P < .001), and water contaminants (intervention = 91.0 ±14.1; control = 82.6 ±18.9; P < .001). The smallest increase was found for the second-hand smoke score (intervention = 94.6 ±9.8; control = 90.3 ±14.0; P = .002).
FIGURE 2.
Differences in self-efficacy between groups; household environmental health intervention delivered by rural public health nurses, Gallatin County, MT, and Whatcom County, WA, 2009.
Controlled for in the analyses comparing groups, years of education was associated with higher self-efficacy scores for general environmental health self-efficacy and for 5 of the 6 risk-specific self-efficacy scores (all P values < .05, except in-wall humidity was nonsignificant). Every additional year of education was associated with an increase of 1 point for general environmental health self-efficacy, second-hand smoke, water contaminants, lead, CO, and 2 points for radon self-efficacy scores (based on linear GEE coefficients for education ranging between 0.8 and 1.9; all P values < .05). Increasing increments of household income of $5000 were associated with a 1 point increase in self-efficacy toward limiting CO exposure, in-wall humidity, and general environmental health self-efficacy (linear GEE coefficients range = 0.8–1.0; all P values < .05). Self-efficacy toward limiting radon exposure was 8 points higher for Gallatin County than for Whatcom County participants (b = 8.1; 95% CI = 2.1, 14.0; P = .009). No other differences in risk-specific self-efficacy scores between the sites were found.
Table 2 summarizes the analyses comparing precaution adoption between groups (intervention vs control). At 3 months, 70% of intervention participants reported precaution adoption for at least 3 environmental health risks compared with only 38% of the control group participants (OR = 3.9; 95% CI = 2.2, 6.7; P < .001). A higher percentage of those in the intervention group reported precaution adoption toward lead (61.3% vs 34.5%; OR = 3.0; 95% CI = 1.8, 5.1; P < .001), CO (51.3% vs 30.2%; OR = 2.4; 95% CI = 1.4, 4.2; P = .001), radon (58.8% vs 47.4%; OR = 2.4; 95% CI = 1.1, 5.2; P = .03), in-wall humidity (62.2% vs 39.7%; OR = 2.5; 95% CI = 1.5, 4.2; P = .006), and water contaminants (59.7% vs 45.7%; OR = 1.8; 95% CI = 1.1, 2.9; P = .03). The intervention had little or no impact on precaution adoption for second-hand smoke (P = .4).
TABLE 2.
Precaution Adoption of Intervention and Control Groups at 3 Months: Household Environmental Health Intervention Delivered by Rural Public Health Nurses, Gallatin County, MT, and Whatcom County, WA, 2009
| EH Measurea | Intervention Group, No. (%) | Control, No. (%) | Group Effect, OR (95% CI) | Pbc |
| General EH precaution adoptiond | ||||
| ≥3 EH risks | 83 (69.8) | 44 (37.9) | 3.9 (2.2, 6.7) | < .001 |
| EH risk-specific precaution adoption | ||||
| Radonf | 70 (58.8) | 55 (47.4) | 2.4 (1.1, 5.2) | .03 |
| Carbon monoxide | 61 (51.3) | 35 (30.2) | 2.4 (1.4, 4.2) | .001 |
| Lead | 73 (61.3) | 40 (34.5) | 3.0 (1.8, 5.1) | < .001 |
| Water contaminants | 71 (59.7) | 53 (45.7) | 1.8 (1.1, 2.9) | .03 |
| In-wall humidity | 74 (62.2) | 46 (39.7) | 2.5 (1.5, 4.2) | .006 |
| Secondhand smoke | 29 (24.4) | 23 (19.8) | 1.3 (0.7, 2.4) | .4 |
Note. CI = confidence interval; EH = environmental health; OR = odds ratio.
Values are numbers (%) for precaution adoption at 3 months by EH measure. Precaution adoption at 3 months is defined as movement forward from the baseline stage by at least 1 step in the stages of the precaution adoption process model.
Full model including main effects for group, education (years), household income ($5000 increments), study site, and all corresponding interactions was evaluated. Group effect (OR [exp(b)]) reported is based on reduced model, such that effects are adjusted for any statistically significant confounders and interactions. Income and education were not associated with precaution adoption for any EH risk.
OR, CI, and χ2 P value from logistic generalized estimating equations model.
General EH precaution adoption is defined as ≥3 EH risks with precaution adoption.
The number and percentage of participants with precaution adoption for each EH subscale is reported.
Gallatin County participants showed an increased odds of precaution adoption for radon (OR = 3.0; 95% CI = 1.4,6.5; P = .004).
Income (increasing increments of $5000), education (years), and the interaction between these attributes and study group were not associated with precaution adoption. For radon, the odds of precaution adoption was 3 times higher for Gallatin County participants (P = .004). No other differences in precaution adoption between sites for subscales were identified.
DISCUSSION
The goal of this study was to determine if a multirisk environmental health intervention delivered by public health nurses increased parents’ self-efficacy and precaution adoption. The analyses provided evidence of an effect for both self-efficacy and precaution adoption: both general and risk-specific effects were found. The increases in self-efficacy between T1 and T2 were between 1.5 and 3 times greater for the intervention group than for the controls. Of 14 subscales examined (1 general and 6 risk-specific for each of the 2 outcomes), only the precaution adoption subscale addressing tobacco smoke failed to achieve statistical or clinical significance. A detailed examination of these data revealed a restriction of range, with 65% (n = 153) of participants reporting that they had already taken precautionary action for second-hand smoke. However, no difference was found even when those cases were excluded from analysis. From this finding it was surmised that parents may have viewed tobacco smoke differently from other environmental health risks. Although studies focusing on smoking abstinence generally supported the notion that social factors (e.g., marrying a nonsmoker, having parents who did not smoke) versus environmental factors were strong predictors of remaining smoke free, the evidence was mixed in regard to environmental versus social drivers of behavior.30 What was deduced from this finding was that from among all the risks addressed by the intervention, second-hand smoke was the risk least amenable to change. Although significant differences were observed for all the other subscales, the magnitude of the differences varied considerably across subscales. The largest effects were observed for both outcomes on the lead subscale. It is interesting to note that among the environmental health risks examined, the public health nurses had the greatest familiarity with lead versus other risks. Many nurses had previous experience with collecting and interpreting blood lead samples in WIC, well child, and immunization clinics. As a result, their previous experience with lead may have given them a more facile understanding of lead than the other risks. Lead results were also much more straightforward to interpret for parents compared with the other environmental health risks (i.e., water contaminants).
A differential effect for both self-efficacy and precaution adoption between the 2 study sites in regard to radon was also observed. Although nurses at both sites educated parents about radon and radon-related health problems, only those homes in Gallatin County were tested. Because our pilot testing procedures confirmed that radon risks were very low in Whatcom County, it was unnecessary to test the homes there during the full-scale randomized controlled trial. This decision was based simply on cost considerations. In retrospect, it would have been better to test all 235 homes, even knowing that those in Whatcom County were not at risk. Seeing the radon test kit in their home may have had a larger impact on parents’ self-efficacy than reading the radon information in the intervention book alone. The use of a differential radon protocol across the 2 performance sites was a significant limitation of the study.
Education and household income were both positively correlated with all but 1 of the self-efficacy scales. These variables were controlled for in the multivariate analyses; however, it is important to note that, all other things considered, participants with more education and/or higher incomes had better self-efficacy outcomes. Other investigators found self-efficacy to be differentially affected by socioeconomic status.31 Few studies examined the role that self-efficacy may have in promoting environmental risk reduction behaviors. In a study of adults caring for children living on or near a Superfund site, Bland et al. 32 found that among the concepts of subjective norms, perceived benefits, and self-efficacy, only self-efficacy was associated with adults’ reporting that their children played outside in lead-safe areas. The study findings related to self-efficacy will be further explored as tailored environmental health interventions for different populations are created.
Implications and Practice
By focusing the study on parents’ cognitive/behavioral outcomes, we opted not to relate the intervention to specific health or health care utilization outcomes as had been the case in several other studies (e.g., asthma, pesticides).33,34 Given the heterogeneity of the risks examined and the brief timeline, it did not make sense to examine the intervention's impact on household measures or biomarkers. Focusing on the parents’ cognitive/behavioral outcomes was consistent with the conceptual approach4 and made sense given the number and complexity of the risks examined.
In regard to the secondary aim of reporting household and biomarker data, this study was unique in collecting data addressing a wide range of physical, chemical, and biologic risks. These risks were selected based on local housing conditions, especially those obtaining water data. Overall, more than 64% of households were found to have at least 1 risk, and 23% of households had more than 1 risk. It was surprising to see that no single risk or pattern of risk predominated across households or across the 2 study locations. Rather, “no one thing” was found. In a few cases, we entered homes and encountered situations that posed immediate life-threatening risks to a family (e.g., significantly elevated CO levels); such cases were few and far between. The only a priori measure found that presumptively predicted household risks at baseline (i.e., no risks vs ≥ 1 risk) was the data collector's perception of the overall condition of the home (OR = 1.21, 95% CI = 1.06, 1.38; P = .003). However, it is important to note that the study was powered to test the effectiveness of the intervention rather than to identify factors predictive of baseline risk. This is an important differentiation.
Adults in the study were overwhelmingly well-educated, non-Hispanic White females. These characteristics reflected the demographics of the study sites, both of which are college towns. The tailored intervention was designed commensurate with local population, climate, and lifestyle characteristics in mind; thus, the intervention book focused on single unit housing (e.g., mobile homes) as well as information addressing wood stoves and weatherization practices. Future research in other settings should be preceded by an assessment of the physical–spatial, economic resources, and cultural–ideologic characteristics of the study population.4 Caution against generalizing these findings to ethnically diverse populations as well as those with other patterns of environmental health risk (e.g., multiunit dwellings) should be considered. The study addressed a narrow socioeconomic strata of parents living in rural areas in 2 economically stable counties; generalizing these findings even to rural dwellers with other characteristics would be unsound. A related limitation pertains to unique attributes of the 2 performance sites for the study. Although the counties were similar in regard to housing costs, household income, and homeownership rates, they differed appreciably in regard to population density and temperature extremes (which significantly impacted home heating and weatherization practices). Both counties are known as popular places to vacation and many of our participants worked in service industries associated with tourism. Both counties have local economies influenced by gentrification and population influx. Poverty in these counties may be substantively different than the characterization of poverty in many other rural communities. It is also important to note that the public health nurses delivering the study intervention differed from rural public health nurses as a whole in regard to educational status; all the intervention nurses in the study had at least a bachelor's degree. In contrast, a study by Bigbee et al.12 found that only 47% of solo office public health nurses in Idaho had a bachelor's degree. It is likely that the high educational status of the public health nurses was a reflection of the communities’ close proximity to state universities. An additional limitation was the inability to offer the intervention to non-English speakers/readers; subsequent research will replicate the study with rural Hispanic and/or Native American families.
Overall, findings from this study complement the foundational work of Olds et al.35–37 regarding the benefits of home visits on child and maternal health outcomes. These findings suggest that in addition to home visits addressing parenting and personal development, public health nurses can favorably influence parents’ environmental risk reduction practices. This study also provided evidence that public health nurses were able to successfully follow a complex set of risk communication protocols and delivered a environmental health tailored intervention.
Conclusions
Although this study focused exclusively on the effectiveness of the intervention, it has implications for the public health nurse workforce overall and the rural workforce in particular. Hill et al38 queried Montana public health nurses to assess their current involvement in environmental health and their perceptions regarding a broader inclusion of environmental health into their practice. The majority of nurses did not work on environmental health activities or initiatives within the health department; however, even within their existing responsibilities, they were often called upon to respond to environmental health questions. Fifty-six percent of public health nurses reported fielding questions about the health effects of environmental hazards; 9% reported that they were often (vs never, rarely, or sometimes) asked such questions. It was clear that rural public health nurses were already providing environmental health information to the families and communities they served. What was not clear from the Montana survey was whether the information provided by public health nurses had the requisite and intended health response. In this context, findings from this study began to provide the evidence base, albeit preliminary, that public health nurse delivered environmental health interventions have the potential to effectively guide parents in the adoption of precautionary actions.
Both the American Nurses Association and the Public Health Nursing Section of the American Public Health Association (APHA) released policy statements calling for research addressing environmental health actions by nurses. The American Public Health Association document listed a specific mandate for research addressing the effectiveness and public health impact of nursing interventions.39,40 The present study will contribute to this science base and inform future research addressing the scope of public health nurse activities in both rural and urban health departments.
Acknowledgments
This study was supported by the National Institute of Nursing Research (NIH R01NR009239 to P.G. Butterfield and K01NR009984 to W. Hill). The authors would like thank the health officers, public health nurses, and the environmental health staff at Gallatin City County Health Department (Montana) and Whatcom County Health Department (Washington).
Human Participant Protection
Study protocols were reviewed and approved by the institutional review boards at Montana State University, the University of Washington, and Washington State University.
References
- 1.Harnish KE, Butterfield P, Hill WG. Does Dixon's integrative environmental health model inform an understanding of rural parents’ perceptions of local environmental health risks? Public Health Nurs. 2006;23(5):465–471 [DOI] [PubMed] [Google Scholar]
- 2.Larsson LS, Butterfield P, Christopher S, Hill W. Rural community leaders’ perceptions of environmental health risks: improving community health. AAOHN J. 2006;54(3):105–112 [PMC free article] [PubMed] [Google Scholar]
- 3.Barnes G, Fisher B, Postma J, et al. Incorporating environmental health into nursing practice: a case study on indoor air quality. Pediatr Nurs. 2010;36(1):33–40 [PubMed] [Google Scholar]
- 4.Butterfield P, Postma J. The TERRA framework: conceptualizing rural environmental health inequities through an environmental justice lens. ANS Adv Nurs Sci. 2009;32(2):107–117 [DOI] [PubMed] [Google Scholar]
- 5.Moodie SM, Tsui EK, Silbergeld EK. Community- and family-level factors influence care-giver choice to screen blood lead levels of children in a mining community. Environ Res. 2010;110(5):484–496 [DOI] [PubMed] [Google Scholar]
- 6.Quandt SA, Doran AM, Rao P, et al. Reporting pesticide assessment results to farmworker families: development, implementation, and evaluation of a risk communication strategy. Environ Health Perspect. 2004;112(5):636–642 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rao P, Quandt SA, Doran AM, et al. Pesticides in the homes of farmworkers: Latino mothers’ perceptions of risk to their children's health. Health Educ Behav. 2007;34(2):335–353 [DOI] [PubMed] [Google Scholar]
- 8.Severtson DJ, Henriques JB. The effect of graphics on environmental health risk beliefs, emotions, behavioral intentions, and recall. Risk Anal. 2009;29(11):1549–1565 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.McCaule LA, Travers R, Lasarev M, et al. Effectiveness of cleaning practices in removing pesticides from home environments. J Agromed. 2006;11(2):81–88 [DOI] [PubMed] [Google Scholar]
- 10.Centers for Disease Control and Prevention, National Center for Environmental Health CDC's Healthy Homes Initiative. Atlanta, GA: CDC; 2009 [Google Scholar]
- 11.American Nurses Association Public Health Nursing: Scope & Standards of Practice. Silver Springs, MD: Nursebooks.org; 2007 [Google Scholar]
- 12.Bigbee JL, Gehrke P, Otterness N. Public health nurses in rural/frontier one-nurse offices. Rural Remote Health. 2009;9(4):1282. [PubMed] [Google Scholar]
- 13.Bigbee JL, Lind B. Methodological challenges in rural and frontier nursing research. Appl Nurs Res. 2007;20(2):104–106 [DOI] [PubMed] [Google Scholar]
- 14.Moules NJ, MacLeod ML, Thirsk LM, Hanlon N. “And then you'll see her in the grocery store”: the working relationships of public health nurses and high-priority families in northern Canadian communities. J Pediatr Nurs. 2010;25(5):327–334 [DOI] [PubMed] [Google Scholar]
- 15.Anderson ES, Winett RA, Wojcik JR. Self-regulation, self-efficacy, outcome expectations, and social support: social cognitive theory and nutrition behavior. Ann Behav Med. 2007;34(3):304–312 [DOI] [PubMed] [Google Scholar]
- 16.Borrelli B, McQuaid E, Novak S, et al. Motivating Latino caregivers of children with asthma to quit smoking: a randomized trial. J Consult Clin Psychol. 2010;78(1):34–43 [DOI] [PubMed] [Google Scholar]
- 17.Gielen AC, McKenzie LB, McDonald EM, et al. Using a computer kiosk to promote child safety: results of a randomized, controlled trial in an urban pediatric emergency department. Pediatrics. 2007;120(2):330–339 [DOI] [PubMed] [Google Scholar]
- 18.U.S. Census Bureau State & County Quickfacts. Washington, DC: US Census Bureau; 2010 [Google Scholar]
- 19.American Public Health Association Standard Methods for the Examination of Water and Wastewater. 20th ed. Washington, DC: American Public Health Association, the American Water Works Association, and the Water Environment Federation; 1998 [Google Scholar]
- 20.Tinker E, Postma J, Butterfield P. Barriers and facilitators in the delivery of environmental risk reduction by public health nurses in the home setting. Public Health Nurs 2010;28(1):35–42 [DOI] [PubMed] [Google Scholar]
- 21.Bandura A. Health promotion by social cognitive means. Health Educ Behav. 2004;31(2):143–164 [DOI] [PubMed] [Google Scholar]
- 22.Bandura A. Guide for Constructing Self-Efficacy Scales. Palo Alto, CA: Stanford University; 2001 [Google Scholar]
- 23.Hill W. Development and Early Evaluation of the Self-Efficacy for Environmental Risk Reduction Instrument. Meeting of the American Public Health Association; November 4-8, 2006; Boston, MA [Google Scholar]
- 24.Weinstein ND, Sandman PM, The Precaution Adoption Process Model. San Francisco, CA: Jossey-Bass; 2002 [Google Scholar]
- 25.Weinstein ND, Lyon JE, Sandman PM, Cuite CL. Experimental evidence for stages of health behavior change: the precaution adoption process model applied to home radon testing. Health Psychol. 1998;17(5):445–453 [DOI] [PubMed] [Google Scholar]
- 26.Prochaska JO. Decision making in the transtheoretical model of behavior change. Med Decis Making. 2008;28(6):845–849 [DOI] [PubMed] [Google Scholar]
- 27.Prochaska JO, Velicer WF, et al. Stage-based expert systems to guide a population of primary care patients to quit smoking, eat healthier, prevent skin cancer, and receive regular mammograms. Prev Med. 2005;41(2):406–416 [DOI] [PubMed] [Google Scholar]
- 28.U.S. Census Bureau Whatcom County. : U.S. Census Bureau. WA: State and County QuickFacts; 2009 [Google Scholar]
- 29.U.S. Census Bureau U.S. Census Bureau State and County QuickFacts: Gallatin County. Montana: U.S. Census Bureau; 2009 [Google Scholar]
- 30.Macy JT, Seo DC, Chassin L, et al. Prospective predictors of long-term abstinence versus relapse among smokers who quit as young adults. Am J Public Health. 2007;97(8):1470–1475 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Begley CE, Shegog R, Iyagba B, et al. Socioeconomic status and self-management in epilepsy: comparison of diverse clinical populations in Houston, Texas. Epilepsy Behav. 2010;19(3):232–238 [DOI] [PubMed] [Google Scholar]
- 32.Bland AD, Kegler MC, Escoffery C, Halinka Malcoe L. Understanding childhood lead poisoning preventive behaviors: the roles of self-efficacy, subjective norms, and perceived benefits. Prev Med. 2005;41(1):70–78 [DOI] [PubMed] [Google Scholar]
- 33.Krieger J, Takaro TK, Song L, et al. A randomized controlled trial of asthma self-management support comparing clinic-based nurses and in-home community health workers: the Seattle-King County Healthy Homes II Project. Arch Pediatr Adolesc Med. 2009;163(2):141–149 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Postma J, Karr C, Kieckhefer G. Community health workers and environmental interventions for children with asthma: a systematic review. J Asthma. 2009;46(6):564–576 [DOI] [PubMed] [Google Scholar]
- 35.Olds D, Henderson CR, Jr, Cole R, et al. Long-term effects of nurse home visitation on children's criminal and antisocial behavior: 15-year follow-up of a randomized controlled trial. JAMA. 1998;280(14):1238–1244 [DOI] [PubMed] [Google Scholar]
- 36.Olds DL, Eckenrode J, Henderson CR, Jr, et al. Long-term effects of home visitation on maternal life course and child abuse and neglect. Fifteen-year follow-up of a randomized trial. JAMA. 1997;278(8):637–643 [PubMed] [Google Scholar]
- 37.Olds DL, Robinson J, O'Brien R, et al. Home visiting by paraprofessionals and by nurses: a randomized, controlled trial. Pediatrics. 2002;110(3):486–496 [DOI] [PubMed] [Google Scholar]
- 38.Hill WG, Butterfield P, Kuntz S. Barriers and facilitators to the incorporation of environmental health into public health nursing practice. Public Health Nurs. 2010;27(2):121–130 [DOI] [PubMed] [Google Scholar]
- 39.American Public Health Association, Public Health Nursing Section Environmental Health Principles and Recommendations for Public Health Nursing. Washington, DC: American Public Health Associaton; 2006 [Google Scholar]
- 40.American Nurses Association Principles of Environmental Health for Nursing Practice With Implementation Strategies. Silver Spring, MD: American Nurses Association; 2007 [Google Scholar]