Abstract
Objectives. The indoor environment has not been fully incorporated into the environmental justice dialogue. To inform strategies to reduce disparities, we developed a framework to identify the individual and place-based drivers of indoor environment quality.
Methods. We reviewed empirical evidence of socioeconomic disparities in indoor exposures and key determinants of these exposures for air pollutants, lead, allergens, and semivolatile organic compounds. We also used an indoor air quality model applied to multifamily housing to illustrate how nitrogen dioxide (NO2) and fine particulate matter (PM2.5) vary as a function of factors known to be influenced by socioeconomic status.
Results. Indoor concentrations of multiple pollutants are elevated in low-socioeconomic status households. Differences in these exposures are driven by the combined influences of indoor sources, outdoor sources, physical structures, and residential activity patterns. Simulation models confirmed indoor sources’ importance in determining indoor NO2 and PM2.5 exposures and showed the influence of household-specific determinants.
Conclusions. Both theoretical models and empirical evidence emphasized that disparities in indoor environmental exposure can be significant. Understanding key determinants of multiple indoor exposures can aid in developing policies to reduce these disparities.
The persistence of racial/ethnic and socioeconomic health disparities in the United States remains a significant public health problem. One focus of the environmental justice (EJ) movement has been the contribution of the physical and social environments in shaping adverse health outcomes among poor communities of color. The emphasis of EJ has historically been on outdoor pollution sources such as industry or traffic, in part because of EJ's origins in addressing historical and continued institutional racism through the siting of industrial facilities, illegal and regulated dumping, and land use planning in communities lacking the political capital that would promote a more equitable distribution of risk.1–5
Although these outdoor sources can clearly influence health disparities given uneven distributions across communities,6,7 an underappreciated EJ issue relates to disparities in indoor residential environmental quality. The direct effect of dilapidated housing and poor sanitation on health has been documented since the 19th century,8–12 because good public policy did not develop in step with rapid urbanization and population growth. Over the past century, understanding of the connections between housing and health has expanded beyond sanitation, infectious disease, and safety to include a broad list of agents associated with morbidity and mortality, such as radon; asbestos; lead; insect and pet allergens; chemicals in wall coatings, furnishings, and consumer products; penetrating outdoor toxics; pesticides; and secondhand smoke, combustion byproducts, and fungi.13–15 Although the linkage between housing and health has been firmly established, it has occurred largely outside of the EJ movement.
As researchers attempt to inform activities which may eliminate known and emerging disparities in environmental risks, addressing indoor environmental exposures will be critical, and doing so will require an understanding of the root causes of these uneven distributions. Addressing indoor exposures is challenging because they include contributions from both indoor and outdoor sources and because they may be influenced by variables that are socioeconomically patterned (e.g., dwelling size) and by institutional factors that define housing quality and neighborhood attributes (e.g., ambient pollution).
However, residential indoor exposures are shaped by specific physical and chemical mechanisms that can be described and modeled. Physical models describing emissions, air exchange, dynamic partitioning, deposition, and other critical processes can aid in the evaluation of risk-reduction strategies. These models can also help identify underlying determinants of exposures, including root causes related to socioeconomic and demographic characteristics that add to the overall burden of health disparities. For example, indoor concentrations of airborne pollutants may be driven by the design or condition of the home's physical structure; resident behaviors; product use profiles; characteristics of household furnishings; presence, condition, and use of mechanical ventilation; air infiltration pathways (especially in multifamily settings); and outdoor pollutant concentrations.
We describe the empirical evidence of socioeconomic disparities in indoor environmental exposures and exposure-related factors and discuss how a framework that identifies the dominant individual, place-based, and institutional drivers of these observed exposure disparities can inform interventions and risk reduction. Although exposure disparities may be observed in multiple settings, we focus our discussion and case study on urban, multifamily households to highlight some general principles and the unique challenges in these settings.
FACTORS CONTRIBUTING TO INDOOR ENVIRONMENTAL DISPARITIES
Indoor environmental exposures, and therefore exposure disparities, are driven by key determinants that vary by route of exposure. For air pollutants, these determinants can be best understood through the structure of a simple box model often used to describe indoor steady-state concentrations in the presence of both indoor and outdoor sources:
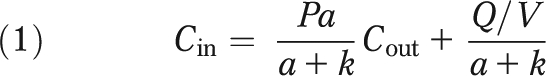 |
where Cin is the indoor steady-state concentration (mg/m3); Cout is the outdoor steady-state concentration (mg/m3); a is the air exchange rate of the home (1/h); P is the penetration efficiency of the pollutant (unitless); k represents loss terms, including deposition or reaction (1/h); Q is the source emission rate (mg/h), and V is home volume (m3).
Examining this simple model makes it easy to understand how differential patterns of 1 or more model parameters could create exposure disparities, as well as how the magnitude of the terms influence the relative importance of indoor versus outdoor sources. Any outdoor exposure disparities would be manifested in the first term of this equation, but other influential factors are socioeconomically patterned.
We used data collected as part of the American Housing Survey16 to highlight the associations between socioeconomic status (SES) and housing characteristics that are directly linked to indoor exposure to pollutants (Table 1). Lower income populations have smaller homes (as anticipated), which would tend to enhance the influence of indoor sources. Moreover, by having a greater occupant density, these homes will tend to have a greater source density (although the absolute source strength may be lower given a smaller number of occupants) and an increased potential for particle resuspension.17 Low SES populations also tend to live closer to mobile and stationary sources, enhancing the influence of the outdoor source term. The most challenging parameter to characterize in the box model is air exchange rate. Low-income homes tend to be older, which may be associated with “leakier” homes that increase infiltration from the outdoors but reduce the influence of indoor sources.18 The presence of holes and other structural deficiencies may also lead to increased infiltration from outdoors. However, research has demonstrated that some multifamily units may have low air exchange rates and inadequate ventilation, which would enhance the effect of indoor sources.19 Concentrations of volatile compounds related to vapor intrusion from the subsurface would be influenced by home volume and air exchange rate but would also be enhanced in single-family dwellings with basements located near contaminated sites, leading to potential differences in exposure patterns.20
TABLE 1.
Representative Housing Variables Associated With Indoor Environmental Exposures, by Household Income: American Housing Survey, United States, 1999
| Income Category |
|||||
| Housing Variable | < $30 K/Year (n = 25 647) | $30 < $60 K/Year (n = 25 840) | $60 < $100 K/Year (n = 24 000) | ≥ $100 K/Year (n = 22 842) | Associated Exposures and Hazards |
| Built before 1980, % | 71.56 | 65.82 | 57.77 | 48.63 | Lead paint; structural integrity |
| Area of peeling paint larger than 8 × 11 in, % | 3.11 | 2.04 | 1.41 | 0.99 | Lead paint |
| Any inside water leaks in past 12 mo, % | 9.14 | 8.67 | 8.24 | 7.98 | Mold and moisture; structural integrity |
| Neighborhood with heavy street noise or traffic, % | 28.19 | 25.42 | 21.95 | 16.69 | Outdoor air sources—mobile |
| Industry or factory within half block, % | 6.90 | 5.50 | 3.54 | 1.74 | Outdoor air sources—stationary |
| Unit uncomfortably cold for ≥ 24 h, % | 10.70 | 9.67 | 7.33 | 6.71 | Supplemental heating; comfort |
| Evidence of rodents in unit, % | 17.77 | 16.81 | 16.98 | 16.26 | Allergen exposure; pesticide exposure |
| Mean floor area of unit, ft2 | 1524 | 1762 | 2098 | 2853 | Exposure to indoor air pollutants |
| Mean occupant density, no./1000 ft2 | 2.78 | 2.59 | 2.31 | 1.82 | Indoor source strength—various |
| Homes with cracks in floor, wall, or ceiling, % | 7.13 | 5.10 | 3.88 | 3.31 | Allergen exposure (pests) |
| Homes with holes in floor, % | 1.85 | 1.03 | 0.58 | 0.37 | Allergen exposure (pests) |
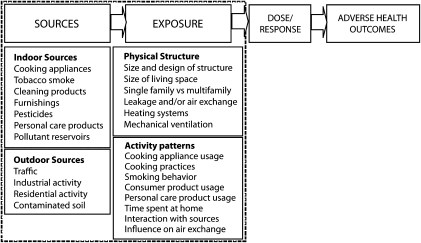
For hazards other than air pollutants, exposure disparities cannot be readily explained through the application of a simple box model, but structural attributes may be socioeconomically patterned and could be root causes of multiple exposures. For example, the homes of low SES populations are more likely to have peeling paint (Table 1), a predictor of lead exposures in older homes; inside water leaks, a predictor of mold and moisture development; and structural deficiencies that may provide points of entry for cockroaches and other pests. Similar trends have been observed if homes and households are categorized by neighborhood characteristics (as urban or rural) or ownership status (rent or own; results not shown). In these cases, the prevalence of characteristics traditionally associated with environmental exposures is generally higher in urban homes and rental households. In general, this evidence from the American Housing Survey reinforces the fact that multiple factors that can influence indoor exposures are more common in low SES populations (Figure 1).
FIGURE 1.
Conceptual framework—contributors to indoor environmental exposure.
EMPIRICAL EVIDENCE OF DISPARITIES IN KEY INDOOR EXPOSURES
We now focus on the empirical evidence for several important classes of indoor pollutants—air pollutants, lead, allergens, and semivolatile organic compounds (SVOCs)—to determine whether studies have previously documented either socioeconomic disparities in exposure or in the root causes of such disparities.
Air Pollutants
Numerous air pollutants are found in the indoor environment and are related to combustion processes or other defined sources. In developed countries, key contributing sources of combustion byproducts, such as carbon monoxide, nitrogen dioxide (NO2), and fine particulate matter (PM2.5), include gas stoves,21,22 cooking,23–25 smoking,24 and natural gas combustion used for heating.22 Studies have shown that low-income households in multifamily buildings have elevated concentrations of NO2, given smaller unit size, elevated source strength, and often inadequate ventilation.19 These root causes would also influence other combustion byproducts (e.g., PM2.5).
Secondhand smoke exposure within residences is also influenced by multiple factors that correlate with SES (Table 2). Source strength is primarily driven by the intensity and time course of indoor smoking behaviors among household members, and evidence has consistently shown higher smoking rates in low SES populations.26,27 Dwelling size and air exchange rates also contribute to these exposures.28,29 Secondhand smoke exposures may be particularly susceptible to a phenomenon observed in multifamily buildings in which infiltrating air may not originate outdoors. Unintended air pathways between apartments or between common areas and apartments can transfer exposures to individuals uninvolved in the polluting activity. In this case, the likelihood of both transfer of air between dwellings and that this air contains elevated pollutant concentrations is increased.28
TABLE 2.
Representative Studies That Inform the Links Between Exposure Disparities and Determinants in Indoor Environments
| Pollutant Environmental Media | Hypothesized Determinant |
||||
| Indoor Source | Outdoor Source | Physical Structure | Activity Pattern | References | |
| Combustion byproducts | |||||
| Nitrogen dioxide | X | X | X | X | Zota et al.19 |
| Secondhand smoke | X | X | X | Wilson et al.29 | |
| Kraev et al.28 | |||||
| VOCs | |||||
| 1,4-dichlorobenzene | X | X | X | Wang et al.30 | |
| Hun et al.33 | |||||
| Churchill et al.32 | |||||
| BTEX | X | X | X | X | Wang et al.30 |
| Chloroform | X | X | X | Wang et al.30 | |
| Hun et al.33 | |||||
| Metals: lead | X | X | X | Gaitens et al.37 | |
| Levin et al.36 | |||||
| SVOCs | |||||
| PBDEs | X | Zota et al.39 | |||
| Pesticides | X | X | Julien et al.40 | ||
| Julien et al.41 | |||||
| Asthma triggers: allergens | X | X | Simons et al.42 | ||
| Wilson et al.43 | |||||
| Bradman et al.44 | |||||
| Peters et al.45 | |||||
Note. BTEX = benzene, toluene, ethylbenzene, and xylenes; PBDEs = polybrominated diphenyl ethers; SVOCs = semivolatile organic compounds; VOCs = volatile organic compounds.
Exposures to volatile organic compounds (VOCs), which may originate outdoors or indoors, have been associated with SES and race/ethnicity, as well as directly with household characteristics. When Wang et al.30 examined personal exposures to VOCs in the National Health and Nutrition Examination Survey, they found higher benzene exposures among those with lower education, those with higher poverty income ratios, and Mexican Americans. They also documented similar exposure patterns for 3 other chlorinated compounds: chloroform, 1,4-dichlorobenzene (1,4-DCB), and tetrachloroethene. In these cases, low-income and non-White households had higher exposures. Wang et al. presented evidence that these associations were driven by individual associations between race/ethnicity and urban residence (chloroform) and race/ethnicity and use of air fresheners in cars (1,4-DCB). Examining the same dataset, D'Souza et al.31 reported that race/ethnicity had the strongest effect on these exposures, with higher exposures among Hispanic and Black participants. Similarly, non-White race has been associated with 1,4-DCB in blood.32 In a study of cumulative cancer risks from exposure to VOCs, the dominant contributors to these risks were exposures to formaldehyde, 1,4-DCB, acetaldehyde, chloroform, and benzene.33 Except for benzene, exposure to all compounds was driven by indoor residential sources, and Hispanics had higher cumulative cancer risks from these compounds, primarily because of exposure to 1,4-DCB, likely from increased air freshener use.
Lead
Perhaps the most notable example of the link between disparities in indoor exposure to an environmental toxicant and health effects is childhood lead poisoning attributed to deteriorating lead paint and lead-contaminated soil. In this case, the connections between SES and poor housing conditions and the ingestion of household dust containing elevated lead concentrations are clear.34–36 In a recent analysis of lead concentrations in household dust, associations were found with income, race/ethnicity, floor surface or condition, and year of construction.37 Lead is also a pollutant that has historically had significant indoor and outdoor sources. Before its removal from gasoline, exposure disparities would likely have been linked to roadway proximity, whereas present exposure disparities are more strongly associated with housing age and quality. Intervention efforts focused on the home environment have reduced disparities in lead poisoning,38 potentially changing the dominant pathways once again.
Allergens
Household pests are common worldwide; residential infestation, however, is strongly linked to low SES. This problem, potentially linked to disease transmission and allergic sensitization, can also affect quality of life. Allergen exposures within the home have been associated with housing disrepair43–45 as well as with SES and race/ethnicity.46–48 For example, Peters et al.45 showed that holes in the wall or ceiling were associated with a 6- to 11-fold increase in kitchen cockroach allergen concentrations. Of note, some allergens do not show clear-cut trends with SES, and for others, high-income populations may be more highly exposed, such as with dust mites.49
Semivolatile Organic Compounds
Over the past decade, numerous studies have documented the presence of SVOCs in indoor air and dust, with known or suspected health effects.50–52 For example, animal studies have suggested that phthalates, pesticides, polybrominated diphenyl ethers (PBDEs), and polychlorinated biphenyls can act as developmental toxicants, endocrine disruptors, or both. Residential environments have the potential to be critical sources of these chemical exposures through their release from building materials, household furnishings, and a wide range of consumer products.53 Unlike standard air pollutants, SVOC exposures are not well described by simple models because they can partition from the air to dust and can contribute to persistent residues.52 SVOCs are particularly challenging to characterize or remediate because once these compounds are introduced into indoor spaces, they are not easily removed by ventilation.54 Socioeconomic patterning would therefore be driven not only by the factors in the standard box model but also by home characteristics that may influence partitioning and removal behaviors.
Disparities in residential exposure to pesticides illustrate the combined impact of deficiencies in housing conditions on household exposure. The regular application of chemical pesticides, including banned and restricted products, is used to combat severe infestation, yet these methods are often ineffective in the ultimate control of pest populations. Consistent with disparities in infestation, exposure to pesticides within the home has been associated with SES55,56 and race/ethnicity.41 The latter case is an interesting example of the subtleties of housing-related EJ issues, in which Hispanic households in a Boston study had elevated exposures to cyfluthrin, a restricted-use pesticide, because of the availability of off-label products at local bodegas. In addition, recent evidence has shown that pesticide residues persist for years beyond application, as evidenced by the presence of banned compounds, such as DDT and some organophosphates, in residential dust and wipe samples.40,57
Several studies have found that non-White racial and ethnic groups, as well as populations with lower household income and lower educational attainment, have significantly higher PBDE body burdens.39,58–60 The root causes of these disproportionate exposures have not been well researched, but 1 potential pathway linking elevated PBDE body burden to low SES populations may involve differences in housing stock and furniture quality, which in turn influences PBDE levels in house dust. Indeed, the levels of PBDE compounds found in house dust in low SES homes in California were among the highest ever reported.39 The physical weathering and crumbling of PBDE-treated foam in older furniture, more often found in lower income homes, may release greater amounts of pentabromodiphenyl ether compounds. SES differences in housing factors, such as air exchange rates, may further modify exposure.39
MODELING CASE STUDY
One of the challenges of the empirical literature is that disentangling the various contributing factors and quantifying the tradeoffs between indoor and outdoor sources is difficult. At the same time, the simple box model may be inadequate to characterize the complexities of multifamily housing. To more accurately describe indoor residential exposures and their determinants in multifamily buildings, we created a detailed simulation of resident activity, emissions, and airflow. We used CONTAM 2.4c, a multizonal indoor air-quality simulation model developed by the National Institute of Standards and Technology (Gaithersburg, MD), to estimate NO2 and PM2.5 concentrations in a low-rise multifamily building. We created a set of scenarios that simulated how changes in household characteristics known to vary by SES influence indoor concentrations of these pollutants.
A full description of modeling parameters is provided in a supplement to the online version of this article at http://www.ajph.org. All CONTAM simulations used a National Institute of Standards and Technology template (apartment building 26) to simulate a building typical of Boston public housing—4 stories, constructed in 1940 to 1969, and naturally ventilated. We simulated a family of 2 adults and 2 children living in each apartment, which included a bedroom, bathroom, living room, and kitchen. Sources of NO2 included gas stoves used for cooking and outdoor NO2; sources of PM2.5 included smoking, outdoor PM2.5, and cooking. Although another significant source of NO2 can be the use of gas stoves for supplemental heating, we did not consider this in our core simulations to focus on more typical exposure scenarios. Emission and removal rates are provided in the online supplement. Cases were simulated by varying gas stove use, smoking rate, house leakiness, outdoor air pollution, and apartment size. Note that these cases are not meant to capture a population distribution of exposure but rather to illustrate how different parameters can act to influence exposures.
All cases were simulated for 7 days in winter, to focus on the season in which indoor exposures are generally most significant. We used simulation results to calculate 24-hour average indoor concentrations per source and pollutant across all apartment rooms and over 7 days. Overall, we computed 162 combinations and categorized each pollutant by the quartile of its mean level. We estimated indoor and outdoor fractions for each pollutant across these quartiles.
SIMULATION RESULTS AND IMPLICATIONS
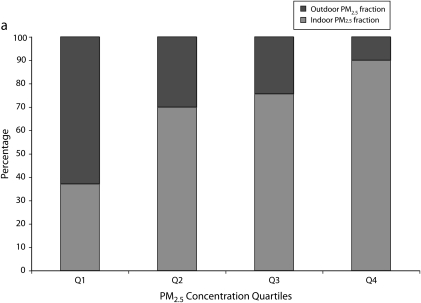
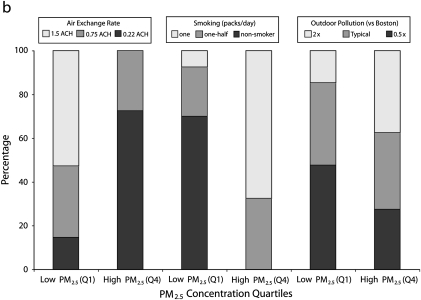
As shown in Figure 2a, at low PM2.5 exposure levels (quartile 1), outdoor sources contributed a higher fraction of indoor concentrations than indoor sources—63% versus 37%. At the higher concentrations (quartile 4), this trend was reversed—90% of exposure was from indoor sources. We observed the same trend for NO2; in the highest exposure quartile, 61% of the exposure was from indoor sources, compared with 0% in the lowest exposure quartile (data are available as a supplement to the online version of this article at http://www.ajph.org).
FIGURE 2.
Contribution of a) indoor (smoking, cooking) and outdoor sources to simulated PM2.5 concentrations, across 162 scenarios in CONTAM and (b) indoor PM2.5 between the lowest and highest quartile for categories of air exchange rate, smoking, and outdoor air pollution.
Note. PM2.5 = fine particulate matter.
We can explain these trends by further analyzing pollutant exposure according to household characteristics such as source strength, physical characteristics of the home, and source use patterns. For example, among the homes in the highest quartile of simulated PM2.5 concentrations, none were in the highest category of house leakiness and air exchange rate, compared with 53% of homes in the lowest quartile (Figure 2b), and 68% had a heavy smoker, compared with 8% in the lowest exposure quartile, thus reinforcing the significant contribution of indoor sources to the most highly exposed individuals. For NO2 simulations, trends were similar to those for PM2.5 (information available as a supplement to the online version of this article). Of note, when we compared models with and without the use of a gas stove to provide supplemental heat, the indoor NO2 source contribution to total pollutant levels was substantially elevated (Supplemental Figure 1, available as a supplement to the online version of this article).
IMPLICATIONS FOR MOVEMENT STRATEGIES AND PRIORITIES
The framework we have presented can be used as a tool to incorporate indoor exposures into EJ considerations and ultimately to guide policies that can address health disparities. Both theoretical models and empirical evidence have emphasized that indoor environmental exposures can exceed outdoor concentrations and, coupled with the amount of time individuals spend indoors versus outdoors, can dominate personal exposures to multiple pollutants known to influence health. Understanding the determinants of these exposures allows one to understand the origins of exposure disparities. In some cases, physical models of pollutant emission and transport in the indoor environment can be used to gain insight and quantify relationships between exposures and household characteristics, as shown for PM2.5 and NO2. In other settings, empirical modeling may identify key determinants, as in the case of exposure to lead, asthma triggers, and some SVOCs.
Once the dominant drivers are identified, efforts can be focused on those that are amenable to intervention. For example, although housing size is closely linked to SES and can directly influence indoor environmental exposures, it is not a likely target for intervention. Source usage patterns and air exchange rates may, however, be suitable targets for action. Gaining a more structural understanding of how indoor exposure disparities originate and propagate can also identify pathways associated with multiple exposures. Actions that target these critical pathways may provide opportunities to address cumulative risks efficiently.
It is worth noting that some exposures in the home are persistent and would thus require different interventions than for short-lived air pollutants, for which source removal will confer immediate benefits. The deposition of particle-bound pollutants and the adsorption to surfaces of semivolatile contaminants can provide long-lasting reservoirs that may confer health risk long after the polluting activity has ceased. Understanding chemical characteristics such as half-life or partition coefficients may be crucial in the design of appropriate and meaningful interventions.
RESEARCH NEEDS
Although many studies have characterized either indoor exposure disparities or their root causes, the need for more research on this topic is clear. For example, future studies could further examine individual pollutants (Table 2), with an increased emphasis on either comparisons between populations or characterization of root causes. A second research direction might take a wider perspective; for example, more community-based participatory exposure research is needed, with researchers partnering with EJ groups, thus combining creative scientific approaches with local knowledge, to characterize indoor environmental conditions in affected communities and stimulate local action. Many successful examples of these efforts exist.61–63
Systematic data collection on physical and chemical exposures in indoor environmental media (e.g., radon in air or pesticides in dust) from different socioeconomic and geographic communities is also needed. Although these efforts involve substantial human and financial resources, EJ activists and researchers could leverage existing large-scale, federally funded surveys (e.g., National Health and Nutrition Examination Survey) to collect and analyze information on indoor exposures, housing, and health. Efforts to track changes in housing characteristics to gain insight into their relationship to health trends38 are also worthwhile endeavors. Research has provided strong evidence that housing-related factors contribute to health outcomes such as asthma and lead poisoning, and efforts to take action within the home have been effective in reducing adverse health outcomes.
Finally, exposure is not the sole determinant of health risk; other individual and neighborhood characteristics with strong ties to SES will influence how environmental exposures will affect health and may heighten the influence of indoor environmental exposures.13 For example, studies have shown that children with elevated exposure to violence are more likely to exhibit the effects of NO2 on asthma development.64 Children living in communities with high rates of violence would not only exhibit greater psychosocial stress (a key effect modifier), but might, depending on their age and other household and neighborhood factors, spend more time indoors,65 which would heighten exposures to elevated indoor concentrations. Future studies should capture attributes of susceptibility, in terms of preexisting disease status and other risk factors such as nutritional status, to consider concurrently with indoor exposure patterns. The links between housing and mental health have also become evident in recent years,66,67 and these effects may also be relevant in understanding disease patterns and the relationship to population characteristics.
Acknowledgments
The project was supported by the National Institute of Environmental Health Sciences (award number R21ES017522).
Note. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Environmental Health Sciences or the National Institutes of Health.
Human Participant Protection
No protocol approval was needed for this study because no human participants were involved.
References
- 1.Evans GW, Kantrowitz E. Socioeconomic status and health: the potential role of environmental risk exposure. Annu Rev Public Health. 2002;23:303–331 [DOI] [PubMed] [Google Scholar]
- 2.Gee GC, Payne-Sturges DC. Environmental health disparities: a framework integrating psychosocial and environmental concepts. Environ Health Perspect. 2004;112(17):1645–1653 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.IOM Toward environmental justice:research, education, and health policy needs. Washington, D.C.: National Academy Press; 1999 [PubMed] [Google Scholar]
- 4.Morello-Frosch R, Pastor M, Sadd J. Integrating environmental justice and the precautionary principle in research and policymaking: the case of ambient air toxics exposures and health risks among school children in Los Angeles. Ann Am Acad Pol Soc Sci. 2002;584:47–68 [Google Scholar]
- 5.Szasz A, Meuser M. Environmental inequalities: literature review and proposals for new directions in research and theory. Curr Sociol. 1997;45(3):99–120 [Google Scholar]
- 6.Lopez R. Segregation and black/white differences in exposure to air toxics in 1990. Environ Health Perspect. 2002;110(Suppl 2):289–295 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Morello-Frosch R, Jesdale BM. Separate and unequal: residential segregation and estimated cancer risks associated with ambient air toxics in U.S. metropolitan areas. Environ Health Perspect. 2006;114(3):386–393 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Crisci M. Public Health in New York City in the Late Nineteenth Century. Bethesda, MD: National Library of Medicine, History of Medicine Division; 1990 [Google Scholar]
- 9.Griscom JH. The Sanitary Condition of the Laboring Population of New York. New York: Harper & brothers; 1845 [Google Scholar]
- 10.Riis JA. How the other half lives: studies among the tenements of New York. New York: Charles Scribner's Sons; 1890 [Google Scholar]
- 11.Von Hoffman A. The origins of American housing reform. Cambridge, MA: Joint Center for Housing Studies: Harvard University; 1998 [Google Scholar]
- 12.Wile IS. Sociological aspects of housing. Am J Public Health (N Y). 1920;10(4):327–331 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rauh VA, Landrigan PJ, Claudio L. Housing and health: intersection of poverty and environmental exposures. Ann N Y Acad Sci. 2008;1136:276–288 [DOI] [PubMed] [Google Scholar]
- 14.Samet JM, Spengler JD. Indoor environments and health: moving into the 21st century. Am J Public Health. 2003;93(9):1489–1493 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Shaw M. Housing and public health. Annu Rev Public Health. 2004;25:397–418 [DOI] [PubMed] [Google Scholar]
- 16.HUD American Housing Survey for the United States 1999: Current Housing Reports. In; 2000 [Google Scholar]
- 17.Baxter LK, Clougherty JE, Laden F, Levy JI. Predictors of concentrations of nitrogen dioxide, fine particulate matter, and particle constituents inside of lower socioeconomic status urban homes. J Expo Sci Environ Epidemiol. 2007;17(5):433–444 [DOI] [PubMed] [Google Scholar]
- 18.Chan W, Nazaroff W, Price M, Sohn M, Gadgil A. Analyzing a Database of Residential Air Leakage in the United States. Atmos Environ. 2005;29:3445–3455 [Google Scholar]
- 19.Zota A, Adamkiewicz G, Levy JI, Spengler JD. Ventilation in public housing: implications for indoor nitrogen dioxide concentrations. Indoor Air. 2005;15(6):393–401 [DOI] [PubMed] [Google Scholar]
- 20.Hers I, Zapf-Gilje R, Li L, Atwater J. The use of indoor air measurements to evaluate intrusion of subsurface VOC vapors into buildings. J Air Waste Manag Assoc. 2001;51(9):1318–1331 [DOI] [PubMed] [Google Scholar]
- 21.Levy JI, Lee K, Spengler JD, Yanagisawa Y. Impact of residential nitrogen dioxide exposure on personal exposure: an international study. J Air Waste Manag Assoc. 1998;48(6):553–560 [DOI] [PubMed] [Google Scholar]
- 22.Yang W, Lee K, Chung M. Characterization of indoor air quality using multiple measurements of nitrogen dioxide. Indoor Air. 2004;14(2):105–111 [DOI] [PubMed] [Google Scholar]
- 23.Evans GJ, Peers A, Sabaliauskas K. Particle dose estimation from frying in residential settings. Indoor Air. 2008;18(6):499–510 [DOI] [PubMed] [Google Scholar]
- 24.He C, Morawska L, Hitchins J, Gilbert D. Contributions from indoor sources to particle number and mass concentrations in residential houses. Atmos Environ. 2004;38(21):3405–3415 [Google Scholar]
- 25.Olson DA, Burke JM. Distributions of PM2.5 source strengths for cooking from the Research Triangle Park particulate matter panel study. Environ Sci Technol. 2006;40(1):163–169 [DOI] [PubMed] [Google Scholar]
- 26.Giovino GA, Schooley MW, Zhu BP, et al. Surveillance for selected tobacco-use behaviors–United States, 1900-1994. MMWR CDC Surveill Summ. 1994;43(3):1–43 [PubMed] [Google Scholar]
- 27.Nelson DE, Emont SL, Brackbill RM, Cameron LL, Peddicord J, Fiore MC. Cigarette smoking prevalence by occupation in the United States. A comparison between 1978 to 1980 and 1987 to 1990. J Occup Med. 1994;36(5):516–525 [PubMed] [Google Scholar]
- 28.Kraev TA, Adamkiewicz G, Hammond SK, Spengler JD. Indoor concentrations of nicotine in low-income, multi-unit housing: associations with smoking behaviours and housing characteristics. Tob Control. 2009;18(6):438–444 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wilson SE, Kahn RS, Khoury J, Lanphear BP. The role of air nicotine in explaining racial differences in cotinine among tobacco-exposed children. Chest. 2007;131(3):856–862 [DOI] [PubMed] [Google Scholar]
- 30.Wang S, Majeed M, Chu P, Lin H. Characterizing Relationships between Personal Exposures to VOCs and Socioeconomic, Demographic, Behavioral Variables. Atmos Environ. 2009;43:2296–2302 [Google Scholar]
- 31.D'Souza J, Jia C, Mukerjee B, Batterman S. Ethnicity, housing and personal factors as determinants of VOC Exposures. Atmos Environ. 2009;43:2884–2892 [Google Scholar]
- 32.Churchill JE, Ashley DL, Kaye WE. Recent chemical exposures and blood volatile organic compound levels in a large population-based sample. Arch Environ Health. 2001;56(2):157–166 [DOI] [PubMed] [Google Scholar]
- 33.Hun DE, Siegel JA, Morandi MT, Stock TH, Corsi RL. Cancer risk disparities between hispanic and non-hispanic white populations: the role of exposure to indoor air pollution. Environ Health Perspect. 2009;117(12):1925–1931 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.CDC Blood lead levels in young children–United States and selected states, 1996-1999. MMWR Morb Mortal Wkly Rep. 2000;49(50):1133–1137 [PubMed] [Google Scholar]
- 35.Jacobs DE, Clickner RP, Zhou JY, et al. The prevalence of lead-based paint hazards in U.S. housing. Environ Health Perspect. 2002;110(10):A599–A606 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Levin R, Brown MJ, Kashtock ME, et al. Lead exposures in U.S. children, 2008: implications for prevention. Environ Health Perspect. 2008;116(10):1285–1293 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Gaitens JM, Dixon SL, Jacobs DE, et al. Exposure of U.S. children to residential dust lead, 1999-2004: I. Housing and demographic factors. Environ Health Perspect. 2009;117(3):461–467 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Jacobs DE, Wilson J, Dixon SL, Smith J, Evens A. The relationship of housing and population health: a 30-year retrospective analysis. Environ Health Perspect. 2009;117(4):597–604 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Zota AR, Rudel RA, Morello-Frosch RA, Brody JG. Elevated house dust and serum concentrations of PBDEs in California: unintended consequences of furniture flammability standards? Environ Sci Technol. 2008;42(21):8158–8164 [DOI] [PubMed] [Google Scholar]
- 40.Julien R, Adamkiewicz G, Levy JI, Bennett D, Nishioka M, Spengler JD. Pesticide loadings of select organophosphate and pyrethroid pesticides in urban public housing. J Expo Sci Environ Epidemiol. 2008;18(2):167–174 [DOI] [PubMed] [Google Scholar]
- 41.Julien R, Levy JI, Adamkiewicz G, et al. Pesticides in urban multiunit dwellings: hazard identification using classification and regression tree (CART) analysis. J Air Waste Manag Assoc. 2008;58(10):1297–1302 [PubMed] [Google Scholar]
- 42.Simons E, Curtin-Brosnan J, Buckley T, Breysse P, Eggleston PA. Indoor environmental differences between inner city and suburban homes of children with asthma. J Urban Health. 2007;84(4):577–590 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Wilson J, Dixon SL, Breysse P, et al. Housing and allergens: a pooled analysis of nine US studies. Environ Res. 2010;110(2):189–198 [DOI] [PubMed] [Google Scholar]
- 44.Bradman A, Chevrier J, Tager I, et al. Association of housing disrepair indicators with cockroach and rodent infestations in a cohort of pregnant Latina women and their children. Environ Health Perspect. 2005;113(12):1795–1801 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Peters JL, Levy JI, Rogers CA, Burge HA, Spengler JD. Determinants of allergen concentrations in apartments of asthmatic children living in public housing. J Urban Health. 2007;84(2):185–197 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Phipatanakul W, Gold DR, Muilenberg M, Sredl DL, Weiss ST, Celedon JC. Predictors of indoor exposure to mouse allergen in urban and suburban homes in Boston. Allergy. 2005;60(5):697–701 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Leaderer BP, Belanger K, Triche E, et al. Dust mite, cockroach, cat, and dog allergen concentrations in homes of asthmatic children in the northeastern United States: impact of socioeconomic factors and population density. Environ Health Perspect. 2002;110(4):419–425 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Sarpong SB, Hamilton RG, Eggleston PA, Adkinson NF., Jr Socioeconomic status and race as risk factors for cockroach allergen exposure and sensitization in children with asthma. J Allergy Clin Immunol. 1996;97(6):1393–1401 [DOI] [PubMed] [Google Scholar]
- 49.Kitch BT, Chew G, Burge HA, et al. Socioeconomic predictors of high allergen levels in homes in the greater Boston area. Environ Health Perspect. 2000;108(4):301–307 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Rudel RA, Dodson RE, Perovich LJ, et al. Semivolatile endocrine-disrupting compounds in paired indoor and outdoor air in two northern California communities. Environ Sci Technol. 2010;44(17):6583–6590 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Rudel RA, Perovich LJ. Endocrine disrupting chemicals in indoor and outdoor air. Atmos Environ. 2009;43(1):170–181 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Weschler C, Nazaroff W. Semivolatile organic compounds in indoor environments. Atmos Environ. 2008;42(40):9018–9040 [Google Scholar]
- 53.Weschler C. Changes in indoor pollutants since the 1950s. Atmos Environ. 2009;43:153–169 [Google Scholar]
- 54.Xu Y, Hubal EA, Clausen PA, Little JC. Predicting residential exposure to phthalate plasticizer emitted from vinyl flooring: a mechanistic analysis. Environ Sci Technol. 2009;43(7):2374–2380 [DOI] [PubMed] [Google Scholar]
- 55.Griffith M, Tajik M, Wing S. Patterns of agricultural pesticide use in relation to socioeconomic characteristics of the population in the rural U.S. South. Int J Health Serv. 2007;37(2):259–277 [DOI] [PubMed] [Google Scholar]
- 56.Stehr-Green PA. Demographic and seasonal influences on human serum pesticide residue levels. J Toxicol Environ Health. 1989;27(4):405–421 [DOI] [PubMed] [Google Scholar]
- 57.Stout DM, 2nd, Bradham KD, Egeghy PP, et al. American Healthy Homes Survey: a national study of residential pesticides measured from floor wipes. Environ Sci Technol. 2009;43(12):4294–4300 [DOI] [PubMed] [Google Scholar]
- 58.Rose M, Bennett DH, Bergman A, Fangstrom B, Pessah IN, Hertz-Picciotto I. PBDEs in 2-5 year-old children from California and associations with diet and indoor environment. Environ Sci Technol. 2010;44(7):2648–2653 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Windham GC, Pinney SM, Sjodin A, et al. Body burdens of brominated flame retardants and other persistent organo-halogenated compounds and their descriptors in US girls. Environ Res. 2010;110(3):251–257 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Zota AR, Adamkiewicz G, Morello-Frosch RA. Are PBDEs an environmental equity concern? Exposure disparities by socioeconomic status. Environ Sci Technol. 2010;44(15):5691–5692 [DOI] [PubMed] [Google Scholar]
- 61.Brody JG, Morello-Frosch R, Zota A, Brown P, Perez C, Rudel RA. Linking exposure assessment science with policy objectives for environmental justice and breast cancer advocacy: the northern California household exposure study. Am J Public Health. 2009;99(Suppl 3):S600–S609 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Hynes HP, Brugge D, Osgood ND, Snell J, Vallarino J, Spengler J. Investigations into the indoor environment and respiratory health in Boston public housing. Rev Environ Health. 2004;19(3-4):271–289 [PubMed] [Google Scholar]
- 63.Perera FP, Illman SM, Kinney PL, et al. The challenge of preventing environmentally related disease in young children: community-based research in New York City. Environ Health Perspect. 2002;110(2):197–204 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Clougherty JE, Levy JI, Kubzansky LD, et al. Synergistic effects of traffic-related air pollution and exposure to violence on urban asthma etiology. Environ Health Perspect. 2007;115(8):1140–1146 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Levy JI, Welker-Hood LK, Clougherty JE, Dodson RE, Steinbach S, Hynes HP. Lung function, asthma symptoms, and quality of life for children in public housing in Boston: a case-series analysis. Environ Health. 2004;3:13 Available at: http://www.ehjournal.net/content/3/1/13. Accessed June 22, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Evans GW. The built environment and mental health. J Urban Health. 2003;80(4):536–555 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Weich S, Blanchard M, Prince M, Burton E, Erens B, Sproston K. Mental health and the built environment: cross-sectional survey of individual and contextual risk factors for depression. Br J Psychiatry. 2002;180:428–433 [DOI] [PubMed] [Google Scholar]