Abstract
Objectives. We aimed to test the hypothesized role of shared body size norms in the social contagion of body size and obesity.
Methods. Using data collected in 2009 from 101 women and 812 of their social ties in Phoenix, Arizona, we assessed the indirect effect of social norms on shared body mass index (BMI) measured in 3 different ways.
Results. We confirmed Christakis and Fowler's basic finding that BMI and obesity do indeed cluster socially, but we found that body size norms accounted for only a small portion of this effect (at most 20%) and only via 1 of the 3 pathways.
Conclusions. If shared social norms play only a minor role in the social contagion of obesity, interventions targeted at changing ideas about appropriate BMIs or body sizes may be less useful than those working more directly with behaviors, for example, by changing eating habits or transforming opportunities for and constraints on dietary intake.
In recent years, health researchers have begun to explore how chronic, noninfectious disease might proliferate through social contagion, as people learn from and react to those around them.1 The idea that social ties serve as conduits for the spread of ill health (and conversely, health) has considerable implications for public health policy and practice; yet, the sociocultural mechanisms by which such types of social contagion might occur remain poorly specified.2
One of the most highly cited examples of this type of social contagion model appears in a study by Christakis and Fowler.3 Using longitudinal data from the 32-year Framingham Heart Study, they demonstrated that obesity spreads through social ties, especially mutual friendships, over time. As with other studies that have observed social clustering of obesity, Christakis and Fowler could not determine from the data the specific social, cultural, and psychological mechanisms by which such contagion occurred.3,4 However, they speculated about underlying pathways, including both socially shared norms about the acceptability of being overweight and socially shared behaviors.
According to the first social norm hypothesis, social affiliation fosters shared norms or ideals (e.g., about the acceptability of being overweight), which then lead to similarity in body mass index (BMI) through the actions of these ideals on diet and physical activity. Studies have found clustering of both body attitudes and eating behaviors.5–7 However, to our knowledge, Christakis and Fowler's3 proposition that shared norms account for the observed social contagion of obesity has not been empirically tested.
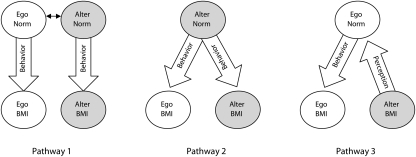
We specifically tested the proposed role played by norms of acceptable body size in observed patterns of clustering in obesity. Specifically, we examined 3 potential pathways for the influence of norms within social relationships (Figure 1). People may come to share a close friend's or other network member's norm for body size, which in turn influences their BMI-related behaviors (pathway 1). For example, through conversations about fatness and thinness people may come to share friends’ ideals of appropriate body size, ideals that may in turn influence how they eat and exercise. Second, people may not internalize their friends’ norms for body size, but they may still feel pressure to fit their friends’ norms and thus modify their BMI-related behaviors (pathway 2). Specifically, people may have a heavier ideal body size than do their friends, but because of subtle comments and shaming, they may feel compelled to lose weight. Finally, people may not necessarily share their friends’ ideals for body size. However, friends’ body size may shape people's own ideals, which could lead them to eat and exercise differently in an attempt to approximate that ideal (pathway 3).
FIGURE 1.
Three potential pathways by which norms might account for the observed relationship between ego and alter BMI.
Note. alter = respondent in Phase 2 sampled from an ego's social network; BMI = body mass index (defined as weight in kilograms divided by height in meters squared); ego = study respondents in Phase 1.
Although each of these pathways is theoretically plausible, several field studies have indicated that norms, beliefs, and ideals are rarely related to behaviors in such a direct manner.8–10 To assess these proposed pathways, we measured key variables—body size and 3 different assessments of body size–related norms—of women and their closest network members in Phoenix, Arizona (101 women and 812 of their social ties). After confirming clustering of obesity and BMI within social ties, we then assessed whether the observed social clustering of BMI could be accounted for by the indirect effect of these different norms about acceptable body size.
METHODS
We used a 2-phase design. In phase 1, we recruited 112 women aged 18–45 years from the Phoenix, Arizona (referred to as “egos”), area using a purposive sampling design to ensure half the sample was overweight or obese. In 2009, each woman was interviewed face to face (social network interview) and asked for the names of as many as 20 people that she knew and was in regular contact with (referred to as “alters”). We excluded alters younger than 18 years. In phase 2, we contacted, recruited, and interviewed alters in order of closeness to the ego. As a check on the social network elicitation technique, we assessed 2 methods for collecting social ties. In half of the cases, we contacted the 5 alters listed as closest to the ego; in the other half, we attempted to contact and recruit all 20. The number of alters participating for each ego thus ranged from 0 to 20. The average number of recruited alters per ego was 7.25 (participation rate = 77.7% for the 5-alter participants and 66.0% for the 20-alter participants); participation was 71.2% of all those approached. Data for at least 1 alter were available for 101 egos, which provided a sample of 812 ego–alter pairs that formed the basis of our analysis.
The interviewers were senior global health students at Arizona State University who went through an extensive training process over several weeks (> 20 hr before the start of the interviews). To further ensure data quality, we met with interviewers at least twice weekly and had 2 senior assistants check the data at collection and at data entry points.
Our study design differed in several notable respects from that of Christakis and Fowler.3 First, it was cross-sectional rather than longitudinal. The design is not relevant for the particular findings of this study because the cross-sectional pattern is sufficient to show that social norms are in many cases unlikely to account for the observed pattern of obesity clustering in networks. We should note that if we had found strong evidence that shared norms accounted for shared BMI (defined as weight in kilograms divided by height in meters squared), then we would have needed to explore other confounding variables—such as shared neighborhood environment or work conditions—in a longitudinal design to assess whether norms really were underlying causal factors. Second, we focused only on female egos, which makes theoretical sense given the relative importance of weight and body size to women's social identity.11 This focus also increased the power of tests because we did not need to control for the ego's gender. Third, the Christakis and Fowler study was a secondary analysis that relied on the participant tracking protocols from the Framingham Heart Study, rather than a standard social network elicitation tool, to generate the social network ties. Finally, Christakis and Fowler focused specifically on siblings in their analyses of family members, whereas we focused more generally on family members, given the small proportion of siblings in our sample.
Measures of Social Ties
We elicited from the ego an open-ended descriptor of the type of relationship she had with each alter. In coding relationship type, we differentiated friends, family members, and romantic partners or spouses, understanding that each may create a quite different set of influences.12 For example, people appear to react very differently to an obese family member than to an obese friend, and many obese people have reported significantly greater teasing from family members, including their spouses.13
In the Christakis and Fowler study,3 the weight status of same-sex friends and siblings had the greatest influence on weight gain over time. To examine this increased effect of same-sex relationships, we differentiated data for male and female alters. Finally, Christakis and Fowler examined 2 definitions of friendship: (1) ego-perceived friendship, in which only the ego needed to recognize the relationship, and (2) mutual friendship, in which both ego and alter identified each other. They found the strongest effects in mutual friendships. To this end, we applied measures of closeness from the egos and alters to assess mutuality of perceived closeness. We considered a mutual relationship to be one in which both members rated the closeness of the relationship as 4 or more on a 7-point inclusion-of-other-in-self scale (on which 7 = closest and 1 = not at all close).14
Measures of Social Norms
We operationalized social norms on the basis of Christakis and Fowler's3 proposal that social norms regarding the acceptability of obesity are a mechanism that can account for the clustering of obesity over time. This definition of social norms as ideals of acceptable behavior or appearance is consistent with social psychological definitions of social norms as socially shared standards of behavior.15 Such standards may be enforced through social interactions, such as shaming, discrimination, or subtle slights, or through learned and internalized personal preferences.15 The proposed pathways reflect some of these mechanisms of influence and enforcement. For example, a person may learn an alter's personal standards, which in turn guide behavior. A person may not hold an alter's personal standard but nonetheless be compelled to conform to it because of shaming, discrimination, or some other form of social interaction. A person may also form a personal standard of appropriate appearance or behavior on the basis of observations of an alter's appearance or behavior. In each of these cases, either the person's own standard or another's standard forms the proximate mechanism of enforcement or influence. To assess the personal standards of egos and their alters, we used 3 different measures of how people rate acceptable body size, how they rate obesity compared with other socially devalued conditions, and how they stigmatize obesity.
Ideal Body Size.
We assessed people's judgments about ideal body size with a commonly used scale, the Figural Rating Scale developed by Stunkard et al.16 The Figural Rating Scale is composed of 9 line-drawn figures that participants rate in terms of their desired body size.17,18 Egos and alters selected the bodies they would most like to have from among these 9 choices. A higher score indicates a larger ideal body size.
Antiobesity Preference.
We used a matched-pairs technique to assess the relative degree to which respondents rated obesity as more or less desirable than other stigmatized conditions. Egos and alters were asked whether they would prefer to be obese or whether they would rather have each of 12 randomly ordered, socially stigmatized conditions, such as herpes and alcoholism. On a scale ranging from 0 to 12, high scores indicated that respondents preferred to have more of the other socially stigmatized conditions than obesity. The comparison items were suggested in part by Schwartz et al.19 As in their study, we found that a reasonably high percentage of respondents would rather have severe depression (25.1%) or even be completely blind (14.5%) than be obese. The scale we created had good reliability (Cronbach's α = .80).
Antifat Stigma.
We also assessed the degree to which an individual agreed with 6 stigmatizing statements about obesity. We developed statements from inductive and deductive sources (focus groups, content searches on interview transcripts, literature searches) and extensive piloting. The statements were “People are overweight because they are lazy,” “People who are overweight are the ones who don't like exercising,” “Obese people should be ashamed of their bodies,” “Fat people are lazy,” “Obesity happens when people don't have self control,” and “You can tell a lot about someone by the size of their body.” A greater number of “true” responses to the 6 statements indicated a more stigmatizing view of obesity. The scale has acceptable reliability (Cronbach's α = .70–.78) in 3 samples from Phoenix, Arizona.
Body Mass Index Measures
We determined the BMI of all alters and egos by self-reported height and weight, and we classified it using standard cutpoints of 25 to 29.9 as overweight and 30 or more as obese. We calculated network BMI as the average value across each ego's alters.
BMI estimates based on self-reports are a reasonable proxy for anthropometric measures of between-individual differences in BMI with correlations between 0.90 and 0.95 in US populations.20,21
Analysis
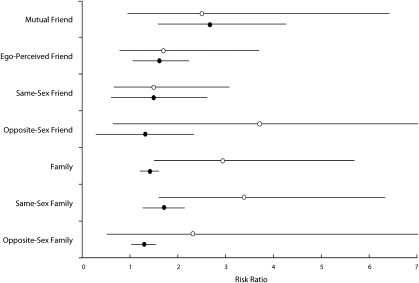
First, we examined whether BMI was indeed more similar among individuals who shared social ties, by examining (1) the relationship between ego BMI and the average BMI of an ego's alters and (2) the increased risk of the ego's being obese when each alter was obese. Following Christakis and Fowler,3 we also conducted the analysis within specific kinds of social ties (e.g., friends, same-sex friends, family members). Spouse or partner ties were insufficient for the relationship-specific analysis (n = 22). For the relative risk of being obese, we adjusted the standard errors to account for clustering within egos (Figure 2), using a design effect based on the formula 1 + (n − 1)ρ, where n is the average number of alters per ego and ρ is the intraclass correlation coefficient. Because our data were cross-sectional, the purpose of this analysis was simply to check for consistency with Christakis and Fowler's primary findings.
FIGURE 2.
Relative risk of ego being obese when an alter is obese, by relationship type.
Note. alter = respondent in Phase 2 sampled from an ego's social network; ego = study respondents in Phase 1; Clear circles and solid lines represent estimates from our study (with 95% confidence intervals). Solid circles and solid lines are estimates from Christakis and Fowler's3 figure 4 for increased risk of the ego's becoming obese if an alter becomes obese. Estimates for same-sex friends and family members from Christakis and Fowler are for women only for comparison with this study's results. For this study, the upper bound for the 95% confidence interval was 21.2 for opposite-sex friend and 8.5 for opposite-sex family member.
Second, we considered 3 potential pathways by which norms might account for observed social influence on obesity (Figure 1). This process involved assessing the indirect effect of a third variable—in this case, 1 kind of social norm—on the observed association between 2 other variables—in this case, ego BMI and average network BMI.22 First, to examine how well the data supported each proposed causal link, we examined the crude correlations between pairs of variables that were linked in at least 1 of the proposed causal pathways (Figure 1), which was a crucial first check of whether a third variable might account for the observed correlation between ego and average network BMI. Second, we tested whether this reduction was statistically significant, using a well-established bootstrapping technique for assessing the degree to which a third variable accounts for the association between 2 variables. Bootstrapping is superior to a Sobel test, which assumes normality of the indirect effect and can be overly conservative.23 This procedure bootstrapped the point estimate and 95% confidence intervals for the reduction in main effect given the third variable (based on 1000 iterations). We also calculated the proportion of variance in the ego's BMI attributable to the indirect effect (R2med), and we report regression coefficients, both unadjusted and adjusted for the indirect effect (c anc c′).24
In all cases, we treated the ego's BMI as the dependent variable and the average alter BMI as the independent variable. We used either ego's social norm measures or average alter social norm measures as the third intermediary variable. The first proposed pathway involves a 3-step indirect path, whereby pairs of individuals come to share body norms, which in turn influence BMI through eating and exercise behaviors. To test this pathway, we collapsed the 2-step path between ego BMI and social norm to a single step in the analysis. Overall, exhausting the 3 different measures of norms and the 3 proposed pathways involved 9 tests.
In these analyses, we were interested in a substantial indirect effect, and the sample size (n = 101) was sufficient to detect such an indirect effect (power = .8, α = .05) if the correlations along the 2 indirect pathways were greater than or equal to 0.37.25
RESULTS
Seventy-four egos listed at least 1 family member for a total of 209 ties (69% female). Family members included parents (43 ties), siblings (45 ties), children (5 ties), in-laws (17 ties), and extended family (99 ties). Eighty-nine egos listed at least 1 friend, for a total of 449 ties (72% female; Table 1) . The remaining ties were distributed among spouses, coworkers, roommates, and acquaintances from common activities (e.g., sports, church). In 398 of the 812 relationships, both the ego and alter rated the relationship as 4 or more on the inclusion-of-other-in-self scale (mutually close relationship).
TABLE 1.
Descriptive Statistics for Egos With at Least 1 Alter and for Alters: Phoenix, Arizona, 2009
| Ego (n = 101), Mean (SD) or % | Alters (n = 812) , Mean (SD) or % | |
| Age, y | 26.2 (8.0) | 31.0 (12.9)* |
| BMI | 24.5 (5.5) | 25.3 (5.5) |
| Reported closeness | 4.5 (1.8) | 4.1 (1.8)* |
| Ideal body size (1–9 scale) | 3.4 (0.7) | 3.7 (0.8)* |
| Stigma paired comparisons (0–12 scale) | 4.2 (2.8) | 4.1 (3.0) |
| Stigmatizing statements (0–6 scale) | 1.9 (1.7) | 1.9 (1.7) |
| Proportion overweight | 0.35 | 0.42* |
| Proportion obese | 0.18 | 0.17 |
| Proportion female | 1.0 | 0.70 |
Note. alter = respondent in Phase 2 sampled from an ego's social network; BMI = body mass index (defined as weight in kilograms divided by height in meters squared); ego = study respondents in Phase 1; network = all alters sampled for a given ego.
*Significant differences with α = 05.
Within individuals, the 3 social norm measures showed moderate to low correlations with each other in the expected directions. The strongest association was between antiobesity preference and antifat stigma (among egos, r = 0.40; P < .01; among alters, r = 0.27; P < .01), with much weaker associations between desired body size and antiobesity preference (among egos, r = −0.27; P < .01; among alters, r = −0.19; P < .01) or antifat stigma (among egos, r = −0.09; ç; among alters, r = −0.09; Eligible (n=33 199) 90.7% of potential participants).
Our data confirmed Christakis and Fowler's3 observation that having heavier and obese alters makes it statistically more likely that a person will be heavier and obese and that this relationship is stronger when alters are closer. We confirmed this finding in this data set by means of a simple correlation of BMI between egos and the average BMI of their social network (r = 0.59; P < .01). This correlation increased when we considered only mutually close relationships (r = 0.64; P < .01) and decreased when we considered nonmutually close relationships (r = 0.40; P < .01). The risk of being obese increased if a woman's alters were obese (rate ratio [RR] = 2.4; 95% confidence interval [CI] = 1.51, 3.84). This effect increased when we considered only mutually close alters (RR = 3.6; 95% CI = 1.94, 6.92) and decreased to being nonsignificant among nonmutually close alters (RR = 1.5; 95% CI = 0.83, 2.82).
We examined the relative risk when examining specific types of social ties (e.g., family, friends) and found a positive effect across all these types of relationships. However, the effect was only statistically significant for family members in general and for same-sex family members. None of the friendship categories showed significant effects, which may be a result of low statistical power. Consistent with Christakis and Fowler,3 the effect increased, although not significantly, when considering mutual as opposed to ego-perceived friendships.
Estimates from the Christakis and Fowler3 study of the increased risk of the ego's becoming obese if an alter of a specific type also becomes obese are not directly comparable to cross-sectional relative risks, but they provide a point of comparison for the relative magnitude of effects for these different relationships. The most noticeable difference between our estimates and those of Christakis and Fowler is our finding of a greater effect among family members. This greater effect may be a result of the different kinds of family members sampled; Christakis and Fowler focused only on siblings, and we included a much wider range of possible family ties.
We then investigated whether the proposed causal links were supported statistically. The strongest correlations (Table 2) are between ego's BMI and ego's norms and between ego's network's average BMI and ego's networks’ average norms. We found moderate to low correlations between ego's norms and ego's average network norms. In all cases, however, these correlations were insufficiently strong to account for the large observed correlation between ego and network BMIs (r = 0.59).
TABLE 2.
Bivariate Correlations Among Ego BMI, Ego Norm, Average Network Norm, and Average Network BMI for 3 Social Norms: Phoenix, Arizona, 2009
| Ego |
Network |
|||||||
| Respondent and Social Norm | BMI | IBS | AOP | AFS | BMI | IBS | AOP | AFS |
| Ego | ||||||||
| BMI | 1.00 | 0.52** | −0.41** | −0.21* | 0.59** | 0.20* | −0.15 | −0.14 |
| IBS | 1.00 | −0.27** | −0.09 | 0.33** | 0.25* | −0.12 | −0.11 | |
| AOP | 1.00 | 0.40** | −0.20* | −0.01 | 0.37** | 0.26** | ||
| AFS | 1.00 | −0.10 | 0.09 | 0.11 | 0.14 | |||
| Network | ||||||||
| BMI | 1.00 | 0.45** | −0.37** | −0.18 | ||||
| IBS | 1.00 | −0.19 | −0.09 | |||||
| AOP | 1.00 | 0.29** | ||||||
| AFS | 1.00 | |||||||
Note. AFS = antifat stigma; AOP = antiobesity preference; BMI = body mass index (defined as weight in kilograms divided by height in meters squared); IBS = ideal body size; ego = study respondent in Phase 1; network = all alters sampled for a given ego.
*P < .05; **P < .01.
Finally, we determined whether social norms had an indirect effect on ego–alter similarity in BMI. In only 1 of the proposed pathways (pathway 3) did social norms account for a statistically significant proportion of the BMI clustering effect. Specifically, ego's desired body size accounted for 20% of the effect of network members’ BMI on ego's BMI (95% CI = 10%, 46%; R2med = 0.15; unadjusted regression coefficient c = 0.99; adjusted regression coefficient c′ = 0.79). Ego's antiobesity preference accounted for 10% of the effect of network members’ BMI on ego's BMI (95% CI = 1%, 20%; R2med = 0.08; c = 0.99; c′ = 0.88).
Ego's antifat stigma did not significantly account for any of the observed social clustering. Moreover, for none of the 3 measures of body size norms did network members’ norms account for the effect of network members’ BMI on ego's BMI. Thus, pathways 1 and 2 were not supported. Our results did not change when we restricted the sample to mutually close relationships.
DISCUSSION
On the basis of the responses of 101 women and 812 of their social alters, we can confirm that people who are heavier have alters who are also heavier. However, by incorporating direct measures of social norms about acceptable body size into the analysis, we found minimal support for the proposition that similarity in BMI can be accounted for by shared social norms. Specifically, we found no evidence that pathways 1 and 2 accounted for the observed social clustering of BMI. We did find some evidence for pathway 3, by which a network member's BMI may influence ego's desired body size, which in turn influences ego's BMI. However, in this data set, pathway 3 accounted for at most 20% of the observed relationship between alters’ and ego's BMI. Moreover, this moderate indirect effect may be the result of unmeasured confounders, such as shared neighborhood environment or work conditions, or reverse causation, by which one's body composition influences one's norms of acceptable body size.
If shared social norms are not responsible for most social clustering, then what other possible pathways might explain this observed clustering of obesity within social ties? Christakis and Fowler3 also suggested that common activities (e.g., eating, exercising, dieting) might play a role, which has received some limited support.5–7 We hope that future studies similar to ours that incorporate data on diet and exercise will be able to identify what role common activities play in the social clustering of obesity. Much similarity in BMI results may possibly result from choosing to affiliate with people who have similar BMIs, although in their analysis Christakis and Fowler used techniques intended to identify social influence over and above selective affiliation.26–28 Another possibility is that body norms are in fact important, but we either measured the wrong domain or measured it without suitable reliability. If that is the case, the development of better measures for social norms relevant to BMI and obesity may ultimately show a greater role for norms in the social contagion of body size.
Limitations
The most obvious limitation of the study is that the inability to detect an indirect effect of norms may have resulted from unreliable or inappropriate measures of social norms regarding body size, unreliability of self-reported measurement of BMI, and interobserver measurement error. For example, other scales intended to measure antiobesity attitudes might possibly provide more reliable or valid estimates of social norms and thus permit detection of mediation.8,28,29 Moreover, self-reports may not reflect implicit feelings or thoughts about acceptable body size, and so other methods for assessing such norms may provide different results.31
We hope that future work will assess whether these other measures show that norms do indeed account for the relationship between social proximity and similarity in BMI. Also, although we took considerable effort to recruit alters through multiple means (phone, in person, Internet) and presented the goals of the study in a relatively neutral way, a selection bias based on the types of alters agreeing to participate in the study is possible. Finally, we considered BMI rather than obesity in assessing the indirect effect of social norms. In the future, we hope that studies with sufficient power to examine the same pathways on shared obesity will provide a further test of the role of social norms in social clustering of body size.
Conclusions
These analyses provide only limited support for the proposition that social norms of acceptable body size account for observed patterns of social clustering in obesity. If shared social norms are not the primary culprit, then this finding has implications for the kinds of interventions that would be most effective at reversing current obesity trends. Specifically, interventions targeted at changing ideas about appropriate BMIs or body sizes may be less useful than those working more directly with behaviors, for example, by changing eating habits or transforming opportunities for and constraints on dietary intake.
By specifying and testing pathways of influence in social networks, we have also contributed to a growing body of research in public health demonstrating the importance of social relationships and networks in the spread of disease, the diffusion of public health messages, the adoption of health behaviors, and the provision of social support.1,32,33 As a complement to increasing evidence that social networks matter for health, more studies that examine in detail how social networks matter for health will help researchers discriminate among numerous plausible social, cultural, biological, and psychological mechanisms for their effects.34
Acknowledgments
The project was supported by funding from the Late Lessons From Early History Initiative at Arizona State University.
We thank the Arizona State University undergraduate global health students who generously assisted in alter recruitment, including Joseph Kling for his thorough analysis of that process. We also thank our graduate students, Deborah Williams, Ashlan Falletta-Cowden, Sveinn Sigurdsson, and Isa Rodriguez-Soto, for their generous assistance with data management.
Human Participant Protection
Institutional oversight for this research was provided by Arizona State University Institutional Review Board under protocol 0907004178.
References
- 1.Smith KP, Christakis NA. Social networks and health. Annu Rev Sociol. 2008;34(1):405–429 [Google Scholar]
- 2.Hruschka DJ. Culture as an explanation in population health. Ann Hum Biol. 2009;36(3):235–247 [DOI] [PubMed] [Google Scholar]
- 3.Christakis NA, Fowler JH. The spread of obesity in a large social network over 32 years. N Engl J Med. 2007;357(4):370–379 [DOI] [PubMed] [Google Scholar]
- 4.Trogdon JG, Nonnemaker J, Pais J. Peer effects in adolescent overweight. J Health Econ. 2008;27(5):1388–1399 [DOI] [PubMed] [Google Scholar]
- 5.Crandall CS. Social contagion of binge eating. J Pers Soc Psychol. 1988;55(4):588–598 [DOI] [PubMed] [Google Scholar]
- 6.Eisenberg ME, Neumark-Sztainer D, Story M, Perry C. The role of social norms and friends’ influences on unhealthy weight-control behaviors among adolescent girls. Soc Sci Med. 2005;60(6):1165–1173 [DOI] [PubMed] [Google Scholar]
- 7.Paxton SJ, Schutz HK, Wertheim EH, Muir SL. Friendship clique and peer influences on body image concerns, dietary restraint, extreme weight-loss behaviors, and binge eating in adolescent girls. J Abnorm Psychol. 1999;108(2):255–266 [DOI] [PubMed] [Google Scholar]
- 8.Allison D, Basile V, Yuker H. The measurement of attitudes toward and beliefs about obese persons. Int J Eat Disord. 1991;10(5):599–607 [Google Scholar]
- 9.Cancian F. What Are Norms? A Study of Beliefs and Actions in a Maya Community. Cambridge, UK: Cambridge University Press; 1975 [Google Scholar]
- 10.Farmer P. AIDS and Accusation: Haiti and the Geography of Blame. Berkeley: University of California Press; 2006 [Google Scholar]
- 11.Carryer JB. Embodied largeness: A feminist exploration. : De Ras M, Grace V, Bodily Boundaries, Sexualized Genders, Medical Discourses. Wellington, New Zealand: Dunmore Press; 1997:99–109 [Google Scholar]
- 12.Hruschka DJ. Friendship: Development, Ecology and Evolution of a Relationship. Berkeley: University of California Press; 2010 [Google Scholar]
- 13.Puhl RM, Brownell KD. Confronting and coping with weight stigma: an investigation of overweight and obese adults. Obesity (Silver Spring). 2006;14(10):1802–1815 [DOI] [PubMed] [Google Scholar]
- 14.Aron A, Aron EN, Smollan D. Inclusion of other in self scale and the structure of interpersonal closeness. J Pers Soc Psychol. 1992;63(4):596–612 [Google Scholar]
- 15.Cialdini RB, Trost MR. Social influence: social norms, conformity, and compliance. : Gilbert DT, Fiske ST, Lindzey G, Handbook of Social Psychology. Oxford, UK: Oxford University Press; 1998:151–192 [Google Scholar]
- 16.Stunkard AJ, Sorensen T, Schulsinger F. Use of the Danish adoption register for the study of obesity and thinness. : Kety SS, Rowland LP, Sidman RL, Matthysse SW, Genetics of Neurological and Psychiatric Disorder. New York: Raven Press; 1983:115–120 [PubMed] [Google Scholar]
- 17.Demarest J, Allen R. Body image: gender, ethnic and age differences. J Soc Psychol. 2000;140(4):465–472 [DOI] [PubMed] [Google Scholar]
- 18.Perry AC, Rosenblatt EB, Wang X. Physical, behavioral, and body image characteristics in a tri-racial group of adolescent girls. Obes Res. 2004;12(10):1670–1679 [DOI] [PubMed] [Google Scholar]
- 19.Schwartz MB, Vartanian LR, Nosek BA, Brownell KD. The influence of one's own body weight on implicit and explicit anti-fat bias. Obesity (Silver Spring). 2006;14(3):440–447 [DOI] [PubMed] [Google Scholar]
- 20.Elgar FJ, Stewart J. Validity of self-report screening for overweight and obesity. Evidence from the Canadian Community Health Survey. Can J Public Health. 2008;99(5):423–427 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.McAdams MA, Van Dam RM, Hu FB. Comparison of self-reported and measured BMI as correlates of disease markers in U.S. adults. Obesity (Silver Spring). 2007;15(1):188–196 [DOI] [PubMed] [Google Scholar]
- 22.MacKinnon DP, Krull JL, Lockwood CM. Equivalence of the mediation, confounding and suppression effect. Prev Sci. 2000;1(4):173–181 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Preacher KJ, Hayes AF. SPSS and SAS procedures for estimating indirect effects in simple mediation models. Behav Res Methods Instrum Comput. 2004;36(4):717–731 [DOI] [PubMed] [Google Scholar]
- 24.Fairchild AJ, MacKinnon DP, Taborga MP, Taylor AB. R2 effect-size measures for mediation analysis. Behav Res Methods. 2009;41(2):486–498 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Fritz MS, MacKinnon DP. Required sample size to detect the mediational effect. Psychol Sci. 2007;18(3):233–239 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Cohen-Cole E, et al. Detecting implausible social network effects in acne, height, and headaches: a longitudinal analysis. BMJ. 2008;337:a2533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cohen-Cole E, et al. Is obesity contagious? Social networks vs. environmental factors in the obesity epidemic. J Health Econ. 2008;27(5):1382–1387 [DOI] [PubMed] [Google Scholar]
- 28.Fowler JH, et al. Estimating peer effects on health in social networks: a response to Cohen-Cole and Fletcher. J Health Econ. 2008;27(5):1400–1405 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Yuker H, Allison D, Faith MS. Methods for measuring attitudes and beliefs about obese people. : Allison DB, Handbook of Assessment Methods for Eating Behaviors and Weight-Related Problems: Measures, Theory, and Research. Thousand Oaks, CA: Sage; 1995: pp. 81–105 [Google Scholar]
- 30.Crandall CS. Prejudice against fat people: ideology and self-interest. J Pers Soc Psychol. 1994;66(5):882–894 [DOI] [PubMed] [Google Scholar]
- 31.Greenwald AG, McGhee DE, Schwartz JLK. Measuring individual differences in implicit cognition: the Implicit Association Test. J Pers Soc Psychol. 1998;74(6):1464–1480 [DOI] [PubMed] [Google Scholar]
- 32.Luke DA, Harris JK. Network analysis in public health: History, methods and applications. Annu Rev Public Health. 2007;28:69–73 [DOI] [PubMed] [Google Scholar]
- 33.Valente T, Hoffman BR, Ritt-Olson A, Lichtman K, Johnson CA. Effects of social-network method for group assignment strategies on peer-led tobacco prevention programs in schools. Am J Public Health. 2003;93(11):1837–1843 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Cohen S, Doyle WJ, Skoner DP, Rabin BS, Gwaltney JM. Social ties and susceptibility to the common cold. JAMA. 1997;277(24):1940–1944 [PubMed] [Google Scholar]