Abstract
Background
The inability to speak during critical illness is a source of distress for patients, yet nurse-patient communication in the intensive care unit has not been systematically studied or measured.
Objectives
To describe communication interactions, methods, and assistive techniques between nurses and nonspeaking critically ill patients in the intensive care unit.
Methods
Descriptive observational study of the nonintervention/usual care cohort from a larger clinical trial of nurse-patient communication in a medical and a cardiothoracic surgical intensive care unit. Videorecorded interactions between 10 randomly selected nurses (5 per unit) and a convenience sample of 30 critically ill adults (15 per unit) who were awake, responsive, and unable to speak because of respiratory tract intubation were rated for frequency, success, quality, communication methods, and assistive communication techniques. Patients self-rated ease of communication.
Results
Nurses initiated most (86.2%) of the communication exchanges. Mean rate of completed communication exchange was 2.62 exchanges per minute. The most common positive nurse act was making eye contact with the patient. Although communication exchanges were generally (>70%) successful, more than one-third (37.7%) of communications about pain were unsuccessful. Patients rated 40% of the communication sessions with nurses as somewhat difficult to extremely difficult. Assistive communication strategies were uncommon, with little to no use of assistive communication materials (eg, writing supplies, alphabet or word boards).
Conclusions
Study results highlight specific areas for improvement in communication between nurses and nonspeaking patients in the intensive care unit, particularly in communication about pain and in the use of assistive communication strategies and communication materials.
More than 2.7 million patients in intensive care units (ICUs) in the United States each year are unable to speak, in large part because of the presence of artificial airways and assisted ventilation (ie, mechanical ventilation).1,2 Communication ability may be further impaired during critical illness by sedation, fatigue, delirium, or neurological disease.3 Communication difficulty is the most commonly reported distressing symptom for ICU patients receiving mechanical ventilation4–7 and is associated with anxiety, panic, anger, frustration, sleeplessness, and distress.4,5,8–11 Nurses also report frustration when patients are unable to verbally report their symptoms, pain levels, and needs.12,13
Problems associated with the inability to speak during critical illness are well-known; however, the actual process of nurse-patient communication in the ICU has not been well studied or systematically measured. Without these data, it is difficult to construct appropriate and evidence-based standards for communication with nonspeaking critically ill patients.3 Efforts to improve communication with ICU patients should be built on a clear understanding of existing strengths and weaknesses in the communication process. In this article, we report findings from the first (usual care) phase of a larger 3-phase clinical trial of nurse-patient communication in the ICU.14 The purpose of this prospective substudy is to describe (1) the frequency, success, quality, and ease of nurse-patient communication interactions and (2) the communication methods and assistive strategies used between nurses and nonspeaking patients in the ICU during usual care.
Background and Significance
Much of the data on communication problems experienced by patients in the ICU are from qualitative studies of the patient’s experience of mechanical ventilation15–17 and/or being unable to speak.18–24 Additional survey research shows communication difficulty is associated with greater severity of illness and feelings of anger,10 frustration,11 panic, anxiety, and sleeplessness.4,5,8
Most observational studies of nurse-patient communication in the ICU were conducted more than 10 years ago. Ashworth’s classic 1980 study25 of nurse-patient communication in 5 British ICUs showed that nurses’ communication was positively correlated with patients’ ability to communicate and provide feedback. Overall, 71% of communication consisted of short-term, task-related information, commands, or brief questions.25 Most (76%–96%) of the verbal interactions between staff and patients in each unit lasted less than 1 minute.25 Other observational studies26–28 confirmed and extended Ashworth’s findings. Salyer and Stuart27 used observations of 20 patients to construct a measure of nurse-patient interaction content. The Categories of Nurse-Patient Interaction Content tool included positive (ie, acknowledgment, reassurance, acceptance, approval, or affirmation) and negative (ie, expressions of rejection, refusal, denial, negation, or prohibition) action and reaction categories for nurses and patients. Positive actions of nurses were correlated with positive reactions of patients. Relatively few interactions (34/217; 15.7%) were initiated by patients.27 Ten years later, Hall28 employed the Categories of Nurse-Patient Interaction Content tool to examine the interactions between nurses and patients receiving mechanical ventilation and the relationships between nurse characteristics and their communication patterns. Higher scores on the Glasgow Coma Scale (indicating greater responsiveness of patients) were associated with more positive reactions and fewer negative actions from the nurse to the patient (r = 0.38, P < .05). The amount of time the nurse actually spent with the patient correlated positively with the number of positive reactions from nurse to patient (r = 0.37, P < .05). However, no association was found between length of time the nurse was assigned to the patient or amount of ICU experience that the nurse had and positive or negative actions by the nurse. Additionally, no association was found between educational level of the nurse and interactions with the patient.28
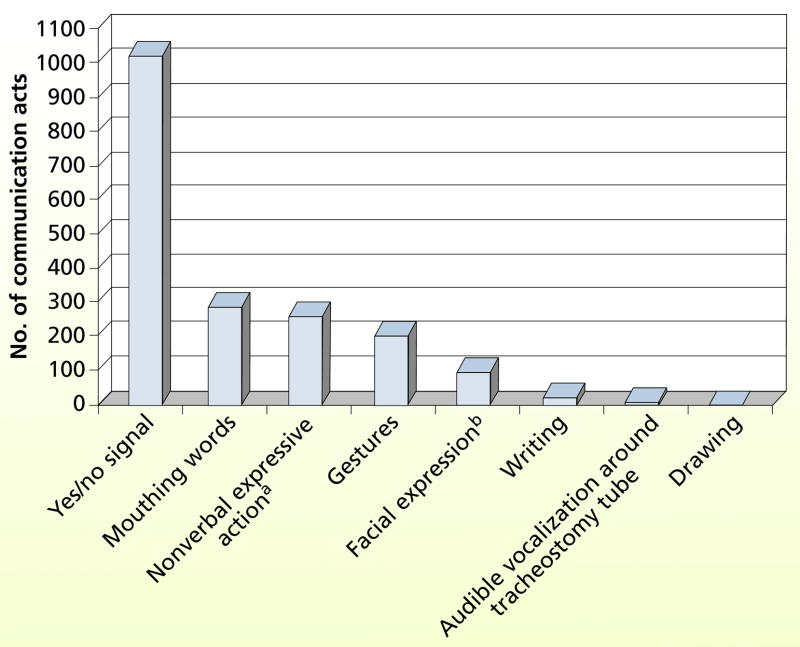
The primary methods of communication used by nonspeaking ICU patients in prior studies were head nods, gesture, mouthing words, and, less frequently, writing.25,26,29,30 The use of alphabet or word communication boards or other forms of augmentative and assistive communication aids was described as “rare” in these studies.25,26,30 In a descriptive observational study that used video recordings of nurse-patient communication, Connolly31 described and categorized common gestural communication used by ICU patients receiving mechanical ventilation. Gestures generated by the patient represented basic needs (eg, pain medication, suctioning, thirst, sleep) and were easily interpreted within the context of the ICU. In some successful interactions, “mirroring,” or nurses’ replication of gestures initiated by patients to affirm their meaning, was a technique that led to increased frequency of gestural communication by nonspeaking patients.31
In general, study results suggest that communication interactions between ICU patients and nurses are influenced by the patient’s severity of illness, level of consciousness, and degree of responsiveness. In previous studies, researchers have described typical communication between patients and nurses as brief, nurse-initiated, informative statements about physical care, yes/no questions, reassurances, or commands. However, most observational studies of nurse-patient communication in the ICU have been limited to single observations of nurse-patient dyads with observation times of various lengths.25–28,32 In addition, measurement parameters of “interaction” were not well defined and communication measurement has consisted primarily of lists and categorizations of communication behaviors. To our knowledge, the successfulness of communication attempts and interpretation of nonvocal communication has not been systematically evaluated in the critical care setting.
In this article, we present descriptive findings from a systematic analysis of video-recorded observations of nonspeaking ICU patients interacting with their nurses during usual care conditions. This prospective observational study aims to generate baseline measures of frequency, success, quality, and ease of nurse-patient communication in the ICU. Secondarily, differences between units were explored.
Research Questions
The following research questions are addressed:
What are the frequency, successfulness, and quality of communications between nurses and temporarily nonspeaking ICU patients?
What are patients’ ratings of communication ease (difficulty) after nurse-patient communication interactions?
What communication methods and assisted communication strategies are used during communication interactions between nurses and temporarily nonspeaking ICU patients?
Methods
Design
This observational study applied descriptive analysis on data from the nonintervention (usual care) cohort of a larger quasi-experimental clinical trial, the Study of Patient-Nurse Effectiveness with Assisted Communication Strategies (SPEACS). The design and methods of the SPEACS study are described in detail elsewhere.14 The study was approved by the University of Pittsburgh’s institutional review board. Patients, or their surrogates if the patient was incapable of decision making, provided written informed consent. Methods are presented in brief here.
Setting
The study was conducted in the 32-bed medical intensive care unit (MICU) and 22-bed cardiovascular-thoracic intensive care unit (CTICU) of a large academic medical center. Few assistive communication materials were available during this preintervention (usual care) phase of the investigation: primarily paper and, less commonly, alphabet letter boards. Family members occasionally brought in other communication aids such as dry erase boards or homemade flash cards or, very rarely, electronic keyboard devices.
Sample
Nurse Participants
Ten registered nurses (RNs), 5 from each unit, were randomly selected from a sampling pool of 44 eligible RNs. All RNs who met the following inclusion criteria are included in the sampling pool: (1) At least 1 year of critical care nursing experience, (2) permanent staff in MICU or CTICU working at least 2 consecutive weekday shifts on a regular basis, and (3) English-speaking. Nurses with a diagnosed hearing or speech impairment were excluded, given the likelihood that these individuals would have previously been exposed to communication services or training. No nurses had previous training in augmentative or assistive communication.
Patient Participants
Thirty patients, 15 from each ICU, who met study eligibility criteria were enrolled in the study. Patients were approached and enrolled in the study depending on the availability of an enrolled nurse participant, which was determined from the daily staffing schedule. Three nonspeaking ICU patients were assigned to each study nurse for 2 consecutive observation days, forming 30 nurse-patient dyads. Patient participants met the following entry criteria: (1) age at least 18 years, (2) nonspeaking because of oral endotracheal tube or tracheostomy, (3) likely to remain intubated for 48 hours after study enrollment according to the clinician’s judgment, (4) able to understand English, and (5) scored 13 or higher on the Glasgow Coma Scale,33 which was applied by using a “verbal” score that represented ability to communicate words by using non-vocal methods. We provided this adaptation of the Glasgow Coma Scale verbal score because nonvocal communication ability was essential to participation in the study. Patients who were reported by family to have a diagnosed hearing, speech, or language disability that significantly interfered with communication before hospitalization were excluded from this study.
This sample was considered adequate for the descriptive purposes (mean, proportions) of this study. For descriptive statistics, means and proportions may be estimated with precision (in terms of the total width of a 95% confidence interval) of 0.746σ and 0.374 for the total cohort and 1.104σ and 0.522 for a unit, respectively. When we limited the investigation of changes over time on selected communication performance measures between the 2 hospital units (MICU vs CTICU) to only the usual care control cohort (n=30), unit by time interactions as small as f =0.390 could be detected when repeated measures analyses were used at a significance level of .05, assuming a maximum intracluster correlation of about 0.1 as in the 3-cohort SPEACS trial.14
Procedures and Data Collection
Communication Observation
Data on communication between the nurse and patient were obtained by video recording 4 separate sessions of naturally occurring nurse-patient communication. Trained data collectors collected the observational data twice daily (morning and afternoon/evening) on 2 consecutive days while the nurse participant was assigned to the care of the enrolled ICU patient. Three minutes of nurse-patient interaction per session were recorded, either continuously or in additive increments, to ensure adequate and equal opportunities for communication interaction. On the basis of previous studies,25–28,34,35 this time unit was selected to be a functional time frame for observation of sending, receiving, confirmation, and follow-up of messages in the ICU.
To minimize participants’ reactivity, such as the “Hawthorne effect,” one desensitizing session was videotaped for each dyad on the morning of the first observation day.36,37 These data were not included in the analysis, but participants were unaware that the first of 5 sessions was “sham.” To supplement observational recordings, the data collector used field notes to document salient events pertaining to the setting, patient, nurse, hospital environment or routine, interruptions in the nurse-patient interaction, and the use of assistive communication equipment, such as writing pads or communication boards.
Demographics and Clinical Descriptive Data
Standard demographic information about the patients and general items pertaining to communication and hospitalization were collected to describe the sample by using a demographic data form standardized by the Center for Research in Chronic Disorders at the University of Pittsburgh School of Nursing.
Severity of illness was measured by using the Acute Physiology and Chronic Health Evaluation (APACHE) III, a well-accepted measure of illness severity in critical care populations, with higher scores indicating greater severity of illness.38,39 APACHE III scores were calculated on enrollment and daily for 2 consecutive days during observation data collection, with values obtained through review of the electronic medical record. Scores were independently calculated by 2 trained research assistants to ensure accuracy.
Delirium was measured by the Confusion Assessment Method-ICU (CAM-ICU), the most widely used instrument for diagnosing delirium.40 The instrument shows high interrater reliability (κ= 0.79–0.96), sensitivities of 93% to 100%, and specificities of 89% to 100% when compared with a reference standard (psychiatrist) diagnosis of delirium.41 CAM-ICU was administered to patients when they enrolled in the study and after each video-recorded session by trained research assistants. Patients who tested positive for delirium were not excluded from observation in order to best represent the population of intubated nonspeaking ICU patients and their communication challenges.
Agitation-sedation was measured on the Richmond Agitation and Sedation Scale (RASS), a 10-point scale for assessing mental status that has demonstrated excellent interrater reliability and validity in a wide range of critically ill medical and surgical patients.42,43 RASS scores were determined on patient enrollment and after each observational session via assessment by a trained data collector.
Communication Measures
To measure nurse-patient communication, 4 (3-minute) video recordings for each nurse-patient dyad were transcribed for verbal and nonverbal behaviors and then segmented into communication acts and exchanges. A communication act is a unit of communicative behavior, nonvocal or verbal, that is directed from one conversational participant to another in an attempt to convey a message. An exchange is a cluster of contiguous communication acts related to the communication of a single idea.44 Trained coders transcribed each communication act within a communication exchange and then coded it for initiation, communication function, and specific communication method or assistive strategy use. Raters maintained an interrater agreement of 0.80 on determinations of acts, delineation of exchanges, initiator of communication exchanges, and ratings of success and quality. This cut point (>0.80) is commonly used as acceptable inter-rater reliability in research involving observational coding from videos.32,45,46 The following example of nurse-patient communication illustrates the determination of communication acts, where each line is a communication act (6 acts) in a single exchange. This is a nurse-initiated exchange because the nurse was the first communicator.
-
(Act 1)
Nurse: “Mary, do you need some pain meds?”
-
(Act 2)
Patient: [grimacing facial expression]
-
(Act 3)
Nurse: “Mary, you look like you’re in pain...” [pause]
-
(Act 4)
Patient: [shakes head up and down]
-
(Act 5)
Nurse: “…do you want some medicine?” [makes gesture for “injection”]
-
(Act 6)
Patient: [nods yes]
Frequency was measured by tallying the number of communication exchanges per session. The mean number of acts per exchange in each 3-minute video-recorded observation was an additional indicator of frequency. Acts per exchange is an approximate index of the amount of message co-construction for each exchange. In addition, a mathematical measure of communication rate or density of communication was derived by dividing the total number of exchanges per session by 3 minutes, resulting in the number of exchanges per minute.
Initiation
The ratio of patient-initiated to nurse-initiated exchanges provided further description of communication exchanges. Patient initiation of communication is measured as a proportion of exchanges initiated by patients through any means (eg, gesture, signal, facial expression, writing, mouthing words).
Successfulness
Coders applied a 5-point ordinal rating for success to each exchange, judging how much of the intended message had been understood by the recipient (see Table 1). The numbers of exchanges for each of the success rating categories were summed and divided by the total number of exchanges to obtain mean proportion of success ratings across sessions and phases. The preceding example of nurse-patient communication was rated as successful because the message was received and understood.
Table 1.
Communication measurement glossary
| Variable | Operational definition |
|---|---|
| Frequencya | (a) Mean number of communication acts/exchanges, (b) mean number of communication exchanges per 3-minute session, (c) mean number of exchanges per minute |
| Act | Unit of communicative behavior, nonvocal or verbal, that is directed from one conversational participant to another in an attempt to convey a message |
| Exchange | Cluster of continuous communication acts related to the communication of a single idea |
| Successa | 1 = No communication response when one is obligated 2 = Message attempted but not conveyed or abandoned 3 = Message partially conveyed (partner has to interpret to obtain partial meaning, partner has to clarify) 4 = Message conveyed with adequate partner response indicating comprehension of basic meaning 5 = Message conveyed with elaborated partner response (action or verbal) indicating complete comprehension of entire message (basic idea plus details) NA = Message did not obligate a response |
| Level of partner assistance | 0 = No support provided despite patient’s need for it 1 = Maximal physical and or verbal assistance required 2 = Moderate physical and/or verbal assistance required 3 = Minimal physical and/or verbal assistance required 4 = Patient responded or initiated communication independently NA = patient was not assisted, but partner’s message did not obligate a response |
| Qualitya | Sum of positive, facilitative communication behaviors by nurse during communication acts versus sum of negative, communication-inhibiting nurse behaviors for 3-minute session |
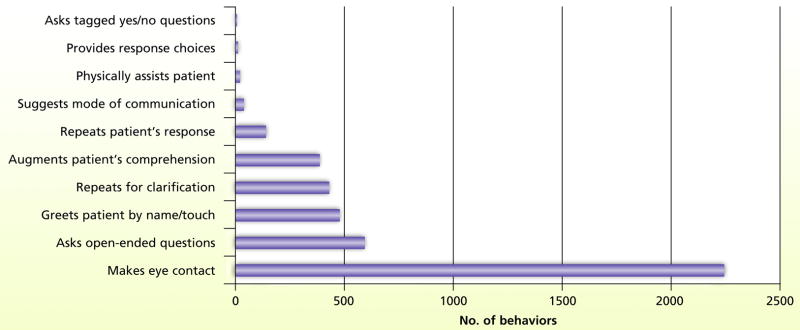
| Positive nurse behaviors | (1) Asks tagged yes-no questions, (2) provides response choices, (3) physically assists patients, (4) suggests mode of communication, (5) repeats patient’s response, (6) augments comprehension, (7) repeats for clarification, (8) greets patient by name/touch, (9) asks open-ended questions when patient has method to respond, (10) makes eye contact |
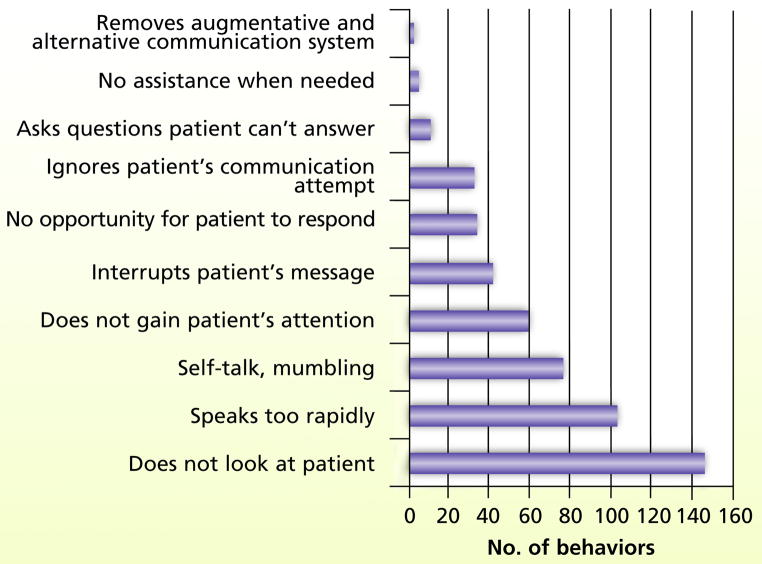
| Negative nurse behaviors | (1) Removes augmentative and alternative communication system inappropriately, (2) does not gain patient’s attention before interaction, (3) does not provide assistance when needed, (4) asks questions that patient cannot answer, (4) ignores patient’s communication attempt, (5) does not provide opportunity for patient’s response (pause time), (6) interrupts patient’s message, (7) does not gain patient’s attention, (8) self-talk, mumbling (9) speaks too rapidly, (10) does not look at patient during interaction |
Main outcome variable.
Level of Assistance Required
Coders applied a 5-point ordinal rating for level of assistance to each exchange on the basis of judgments about degree of independence in communication on the part of the patient (Table 1). These ratings were used descriptively to evaluate successful and unsuccessful exchanges further.
Quality was measured by the presence or absence of 10 possible positive communication behaviors and 10 possible negative communication behaviors assigned by raters to each nurse communication act. These behaviors may recur in a 3-minute communication session between nurse and patient. Quality was computed by summing the number of positive communication behaviors and the number of negative communication behaviors by the nurse. These behaviors were selected from publications on ICU nurse communication25–28,32 and best practice in augmentative and assistive communication. Several positive nurse behaviors are evident in the preceding example of nurse-patient communication: use of pause time, confirming meaning of patient’s nonverbal grimace, and the nurse’s gesture. Assessment of positive nurse behaviors required some judgment. For example, the use of open-ended questions by the nurse is a positive behavior, moving communication beyond yes-no questions controlled by the nurse, but only if the patient has the means (cognitively and/or motorically) to answer open-ended questions. Raters maintained good (85.4%–95.3%) interrater agreement on the identification of positive behaviors.
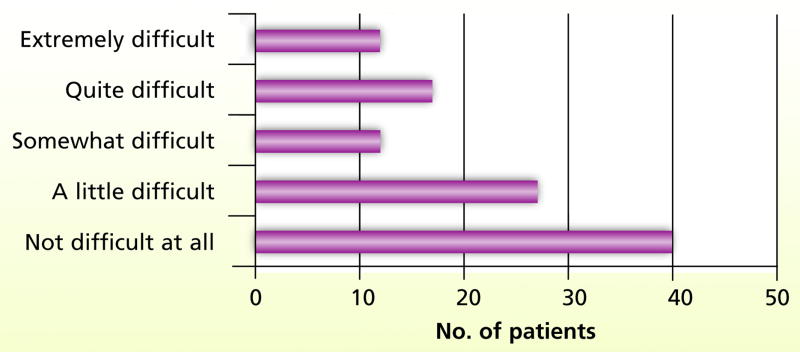
Ease of communication was measured by patient self-report, wherein patients used a simplified single-item self-rating (on a scale of 1 to 5) after each observation session to report their communication difficulty during that nurse-patient interaction, with 5 representing greatest difficulty. The wording of this item is consistent with items on Menzel’s Ease of Communication Scale10; however, we asked patients to reflect only on their difficulty in communicating with the nurse during the previously observed interaction rather than “during the last day or two” as in Menzel’s scale.
Data Analysis
Analyses were conducted by using SAS for Windows Version 9.2 (SAS Institute, Inc, Cary, North Carolina). In addition to automated integrity checks on the data during data entry, the range of response and contingency table analyses were used to identify data inconsistencies. Descriptive statistics (eg, means, medians, standard deviations, interquartile ranges) were computed to summarize continuous-type descriptors of patients (eg, age) and nurses (eg, years of critical care practice) as well as communication outcomes (eg, number of communication exchanges in a 3-minute session, number of acts in a single communication exchange). Frequencies, percentages, and (as appropriate) modes and ranges were calculated to describe categorical patient and nurse characteristics and communication measurements (eg, patient’s and nurse’s sex, initiator of communication exchange, level of partner assistance of exchange).
The numbers of acts per exchange were computed and subsequently averaged across the exchanges occurring for each nurse-patient dyad across the 4 observation sessions. Linear mixed effects modeling was used to analyze this communication frequency outcome. This repeated measures model included a fixed between-subjects effect for intensive care unit (MICU vs CTICU) and fixed within-subjects effects for session and the 2-way interaction of intensive care unit and session. Random effects were included in models for dyad as well as nurse to address the clustering of patients within nurses. Autoregressive structure was chosen as the best fitting covariance structure for the repeated session assessments based on information criteria (AIC, AICc, and BIC).
Results
Demographic Characteristics
One-hundred twenty observation sessions were completed on 30 patients ranging in age from 29 to 82 years (mean, 56.30 years; SD, 15.72 years); 16 (53%) were women. Twelve patients (40%) were orally intubated during the period of observation, and the remainder (n = 18, 60%) had tracheotomy tubes that were not routinely capped or valved to enable speech. Table 2 lists patients’ clinical and demographic characteristics. Nurses, 2 men and 8 women, ranged in age from 24 to 55 years (mean, 41.80 years; SD, 8.68 years) with a mean of 11.30 years (SD, 9.1 years) in critical care practice. Table 3 shows characteristics of the 10 nurse participants.
Table 2.
Characteristics of patients (N = 30)
| Characteristic | Value |
|---|---|
| Age, y | |
| Mean (SD) | 56.30 (15.72) |
| Range | 29–82 |
| Median | 56 |
|
| |
| Score on APACHE III | |
| Mean (SD) | 49.47 (13.23) |
| Range | 12–79 |
| Median | 51 |
|
| |
| Days intubated before enrollment | |
| Mean (SD) | 12.60 (11.73) |
| Range | 1–54 |
| Median | 9 |
|
| |
| Airway, No. (%) of patients | |
| Intubation | 12 (40) |
| Tracheotomy | 18 (60) |
|
| |
| Sex, No. (%) of patients | |
| Male | 14 (47) |
| Female | 16 (53) |
|
| |
| Race, No. (%) of patients | |
| White | 23 (77) |
| African American | 7 (23) |
|
| |
| Visual acuity, No. (%) of patients | |
| Impaired | 2 (7) |
| Accurate | 3 (10) |
| Adequate with correction + lenses available | 10 (33) |
| Adequate with correction + lenses not available | 15 (30) |
|
| |
| Hearing acuity, No. (%) of patients | |
| Impaired | 1 (3) |
| Adequate/unimpaired | 28 (93) |
| Uses hearing aid + aid not available | 1 (3) |
Abbreviation: APACHE, Acute Physiology and Chronic Health Evaluation.
Table 3.
Characteristics of nurses (N = 10)
| Characteristic | Value |
|---|---|
| Age, y | |
| Mean (SD) | 41.80 (8.68) |
| Range | 24–55 |
| Median | 43 |
|
| |
| Years of nursing practice | |
| Mean (SD) | 15.60 (9.34) |
| Range | 2–33 |
| Median | 14 |
|
| |
| Years of critical care practice | |
| Mean (SD) | 11.30 (9.09) |
| Range | 2–33 |
| Median | 11 |
|
| |
| Sex, No. (%) of nurses | |
| Male | 2 (20) |
| Female | 8 (80) |
|
| |
| Race, No. (%) of nurses | |
| White | 10 (100) |
|
| |
| Highest educational level, No. (%) of nurses | |
| Associate’s degree | 1 (10) |
| Diploma | 0 (0) |
| Bachelor’s degree | 8 (80) |
| Other | 1 (10) |
| CCRN certified, No. (%) of nurses | 3 (30) |
In the 120 observation sessions, patients were restrained via single or bilateral wrist restraints during 20 (16.7 %) sessions of nurse-patient communication. They tested positive for delirium on the CAM-ICU in 25 sessions (20.8%). Patients were calm and cooperative during most (n=84; 70%) sessions, with sedation-agitation scores falling in the sedated range during 28 sessions (23.3%), but rarely in the restless-agitated range (n = 8; 7%).
Communication Interactions
Frequency
A total of 5140 communication acts were recorded and coded during 360 minutes of video-recorded interaction. Almost all (n = 5015; 97.6%) of these interactions were between nurses and patients. These communication acts clustered into 943 topical message units or communication exchanges. The mean rate of completed communication exchanges between nurses and nonspeaking patients was 2.62 exchanges per minute. The number of communication exchanges in a 3-minute session ranged from 1 to 21 exchanges (mean, 9.32; SD, 4.3), with a median of 8.5 communication exchanges per session.
The number of acts in a single communication exchange ranged from 1 to 38 (mean, 5.45; SD, 5.1). The median number of acts in an exchange was 4.0. Nearly one-third (31.8%) of the 943 communication exchanges in this sample were composed of 1 or 2 acts. Another one-third (34%) of the observed exchanges were composed of 3 to 5 communication acts. Most communication acts were performed by the nurse (3322 acts; 64.6%). Patients performed 1693 (32.9%) of the communication acts, and family members and others in the room contributed the remainder (125 acts; 2.4%) as third parties in a nurse-patient communication.
Further analyses were performed to determine whether session, unit, or nurse had an effect on the number of acts per exchange (averaged across exchanges within a session for each dyad). The only significant main effect was for intensive care unit (F1,104 = 11.74, P = .001). The CTICU dyads had a mean of 2.71 acts per exchange across the sessions, which was significantly less than the MICU mean of 3.81 acts per exchange across the sessions. No significant interaction was found between type of intensive care unit and session (F3,104 = 0.34, P = .79) and no significant effects for session (F3,104 = 1.34, P = .27).
Initiations
Communication exchanges were most often (86.2%) initiated by nurses. Patients initiated 12%, and third parties initiated another 2% of exchanges. Most nurse-patient exchanges were about care, focusing on nurse assessment, care provision, and patients’ care needs. The topics of nurse-patient communication in the control group (usual care) will be described in greater detail in a separate article.47
Success
Of the 943 nurse-patient communication exchanges, a total of 747 exchanges (79.2%) were able to be rated for successfulness. Approximately one-fifth of the communication exchanges (n = 191; 20.3%) were statements, such as “I have a couple of your medications here,” that did not obligate a response; thus, success determinations were not possible. A few (n=5) exchanges were incomplete or could not be fully understood by raters. Of the 747 rated exchanges, most (71.8%) were transmitted successfully with adequate understanding or acknowledgment. An additional 14 exchanges (1.9%) achieved the highest rating for being transmitted successfully with elaboration by the responder as in the following example.
Nurse: “Would you like to get out of bed to a chair?”
Patient: (slight nod of head) “No.” (mouths) “The chair is so uncomfortable.”
Nurse: “The chair is so uncomfortable.”
Patient: (nods head yes)
In more than one-quarter of the nurse-patient communication exchanges (n = 197; 26.4%), the message was partially conveyed, not conveyed, or abandoned. Messages about pain were in this “unsuccessful” range 37.7% of the time, whereas 25.0% of messages about other topics were unsuccessful. When the dichotomized categorization of success described earlier was used, patient-initiated communication exchanges were successful slightly less often than nurse-initiated exchanges (63.6% vs 74.9%). All 75 communication exchanges in which patients were judged to have not received needed assistance to communicate were rated as partially or completely unsuccessful. Communication exchanges in which patients were independent or required minimal physical or verbal assistance to communicate had the highest success rates, 90.6% and 72.0%, respectively.
Quality
Each of the 3322 communication acts performed by the nurse were rated for positive and negative behaviors. More than 1 behavior could be demonstrated in a single act. Figures 1 and 2 detail the positive and negative behaviors of nurses, respectively. Making eye contact, asking open-ended questions, greeting by name or touch, and the use of gesture or pointing were the most common positive communication behaviors used by nurses. Conversely, lack of eye contact for an entire exchange was the most common negative communication behavior, followed by speaking too rapidly and not gaining the patient’s attention before beginning a communication exchange. Self-talk or mumbling was another fairly common negative nurse behavior observed in this group. On average, nurses demonstrated 4.9 as many positive communication behaviors as negative communication behaviors. The mean number of positive nurse acts per exchange (averaged across exchanges within a session for each dyad) was 0.73, whereas the mean number of negative nurse acts per exchange (averaged across exchanges within a session for each dyad) was 0.15. Unit had a significant effect on positive nurse behaviors: CTICU nurses exhibited fewer positive communication behaviors than did MICU nurses (F = 7.38, P = .008). Negative acts did not differ by unit or by day in the study or time of observation (morning vs afternoon).
Figure 1.
Quality of communication acts: positive nurse behaviors.
Figure 2.
Quality of communication acts: negative nurse behaviors.
Ease of Communication
Patients were able to respond to the question, “Overall, how difficult was it for you to communicate with the nurse?” after 108 out of 120 observation sessions (90%). The histogram in Figure 3 shows the distribution of communication ratings on a 5-point Likert-type scale. Most (62%) rated the observed nurse-patient communication sessions as not-at-all to a little difficult, whereas 38% rated communication as somewhat to extremely difficult.
Figure 3.
Patients’ ratings of ease of communication (N = 108).
Patient Communication Methods
Figure 4 shows communication methods used by patients. Little to no alternative communication was used other than natural methods (ie, head nod, gesture, mouthing words, and facial expression). Head nods and yes/no gestures were the most common communication technique used, followed by mouthing words and communicative nonverbal actions and gestures. Writing was minimal (n = 20 acts). No communication boards, alphabet boards, or picture boards were observed in use during these video-recorded observations.
Figure 4.
Patients’ communication methods (N = 1693 patient communication acts).
a Such as a purposeful look or hand squeeze.
b Such as a smile, frown, grimace.
Discussion
This study is the first published observational study in which nurse-patient communication in the ICU is comprehensively rated beyond positive and negative behaviors.27,28,32 The study results present an overall picture in which nonspeaking ICU patients were able to communicate and receive basic messages about care with relatively good success and a moderate degree of difficulty reported by patients. However, a more discriminate analysis and interpretation of each communication performance variable shows critical areas for improvement.
Frequency
The findings demonstrate a relatively low frequency of communication between nurses and nonspeaking ICU patients as evidenced by fewer than 3 completed communication exchanges per minute on average between nurses and nonspeaking patients. Moreover, communication exchanges were brief, with nearly one-third (31.8%) of exchanges comprising only 1 or 2 acts and another third (34%) comprising 3 to 5 acts. The first 3 minutes of the nurse-patient interaction, used here for consistency of measurement, may be more task-oriented than subsequent interactions or this pattern may be typical of nurse-patient interaction in the ICU. Prior studies do not provide detail about when nurse-patient observations were conducted. This is the first study to record consistent timing (morning and afternoon) and number (4) of observations equally applied to all nurse-patient dyads.
Initiations
The finding that nurses initiated the majority (82.6%) of communication exchanges and performed twice as many communication acts as patients is consistent with results of prior studies of communication in the ICU as well as studies of patient-provider communication in other settings.25,27,28,32 Clearly, nurses control the timing, topic, and method of communication with patients in the ICU. As such, nurses bear a unique responsibility to engage non-speaking patients in communication and enable the patient’s message to be effectively transmitted and understood.
Success
Overall, this group of experienced critical care nurses demonstrated mostly (73.7%) successful communication exchanges. Nevertheless, more than one-quarter of the nurse-patient communication exchanges that obligated a response were either partially understood, abandoned, or entirely ignored. All (100%) of the communication exchanges in which patients required, but did not receive, assistance from the nurse failed. Nurse-patient dyads performed best when little to no assistance was required. Untrained in augmentative and alternative communication techniques, these critical care nurses lack a set of skills in assistive communication strategies that could improve communication where the need is greatest. Nurses admit to becoming frustrated, giving up, and avoiding contact with patients with whom communication is difficult.12,13,26,34 Relatively few successful communication exchanges achieved the highest level of success, which entails an elaborated response. This area also is in need of improvement. Normal, meaningful human communication is more than yes-no answers or acknowledgments. Enabling a patient to add a brief explanation or a humorous comment to a yes-no answer can restore the patient’s sense of self or personhood. The finding that 37.7% of communications about pain were unsuccessful is disturbing and points to the need for improved pain-symptom communication.
The good news is that nurses are asking patients about pain and engaging in communication with the patients about pain. Unfortunately, these communication exchanges are often unclear and unresolved. Breakdowns occur when patients become confused with or inattentive to the nurses’ queries about symptoms of pain and when nurses have difficulty interpreting patients’ responses. Critical care clinicians use physiological cues (eg, heart rate, blood pressure, ventilator asynchrony) in addition to nonvocal behaviors (facial grimaces, gestures) as indicators of pain or discomfort.20 In a classic investigation of pain among ICU patients, ICU survivors reported attempting to communicate pain by signaling with their eyes, grabbing or holding onto the nurse’s arm, and moving their legs up and down.48 Although communicating about pain, discomfort, and other symptoms is a common need for intubated ICU patients,24 few data show that nurses consistently or accurately interpret nonverbal signals as symptom communication.49
Quality
Negative communication behaviors were few, especially when compared with the incidence of positive communication behaviors. The list of positive behaviors, however, shows room for improvement and areas that are potentially fruitful for instruction. Nurses in this sample rarely repeated or mirrored the patient’s response or communication attempt, suggested a method of assistive communication to the patient, physically assisted a patient to communicate, or provided verbal choices even for yes/no questions. These simple facilitative communication skills can be taught to nursing students and practicing nurses. Similarly, through communication skills training, nurses may be able to identify and discontinue common negative communication behaviors, such as failure to make eye contact, speaking too fast or with too much information, and self-talk. Unlike previous observational studies,27,28,32 silence during care was not recorded as a negative behavior unless the nurse failed to gain the patient’s attention before providing care or ignored a patient’s communication attempt.
Ease
Patient self-ratings of communication difficulty in this study differ markedly from such ratings in other studies that included communication difficulty as a distressing symptom.6,7,10 Patients’ ratings may have been affected by social desirability or the Hawthorne effect. Nevertheless, nearly 40% of patients’ responses rated communication with the nurse as somewhat to extremely difficult, suggesting room for improvement.
Communication Methods
The communication methods used by patients in this study are similar to those documented in previous research.18,25,26,30 Patients’ communication methods in the ICU have not changed in the past 3 decades since Ashworth’s original study25 in which the problem of impairment of patients’ communication during critical illness was documented. In fact, the incidence of writing was minimal in this cohort—less than in previous reports—and, unfortunately, no communication boards or other assistive communication devices were observed in use. Clearly, access to assistive communication materials and devices is needed in this population.
Systematic development and testing of interventions to improve communication with non-speaking ICU patients has been limited. Funded by the National Institute of Child Health and Human Development, the SPEACS study14 was designed to test 2 levels of intervention including communication skills training for nurses, assistive communication materials, electronic communication devices, and specialty consultation on communication outcomes (frequency, quality, success, and ease). The results, to be published subsequently, will provide valuable information on the effectiveness of multilevel interventions to improve communication between nurses and nonspeaking patients in the ICU.
Limitations
This study was limited to 2 ICUs in 1 hospital and may not reflect nurse-patient communication performance in other locales or settings. Potential generalizability of the results was, however, increased by random selection of nurses for participation in the study. Patients and nurses may have been influenced by the camera and the presence of observers. Although a desensitizing, unrated video-recording session conducted with all patient-nurse dyads was intended to reduce the Hawthorne effect, the unavoidable visibility of the camera and recording team increased the likelihood that “best” behavior was observed. Our measure of communication success is limited in that data about outcomes of communication exchanges about pain, symptoms, or care needs (ie, provision of requested care) were not collected.
Additionally, these results must be considered within the context of the nurses’ level of experience. Although randomly selected, the nurses in this sample were an experienced group of critical care nurses; 30% had CCRN certification. As such, they most likely represented the best of a naive group of nurses who had not received specialized training, consultation services, or access to communication aids. Their mean age (41.8 years) is, however, reflective of the mean age of nurses across the country (45 years).50 Patients were representative of mixed cardiothoracic surgical and medical ICU populations.
Conclusion
This study provides a unique and detailed description of nurse-patient communication when patients in the ICU are unable to speak. The findings point to areas for practice improvement in the use of assistive communication strategies and communication materials with critically ill patients. Evidence-based interventions are needed to improve critical care nurses’ skill with assisted communication, access to communication materials (eg, writing tools, communication boards), and success in communicating about pain and other symptoms. Future research should include systematic testing of interventions to improve communication with ICU patients and a closer examination of symptom communication and treatment of identified symptoms as the full measure of successful communication about pain or other distressing symptoms.
Acknowledgments
The authors thank Xiao (Shirley) Lu, MS, for early statistical support and Michael Donahoe, MD, for clinical support.
Footnotes
FINANCIAL DISCLOSURES
This work was supported by a grant (R01-HD043988) from the National Institute of Child Health and Human Development.
eLetters
Now that you’ve read the article, create or contribute to an online discussion on this topic. Visit www.ajcconline.org and click “Respond to This Article” in either the full-text or PDF view of the article.
SEE ALSO
For more about nurse-patient communication, visit the Critical Care Nurse Web site, www.ccnonline.org, and read the article by Grossbach et al, “Promoting Effective Communication for Patients Receiving Mechanical Ventilation” (August 2010).
To purchase electronic or print reprints, contact The InnoVision Group, 101 Columbia, Aliso Viejo, CA 92656. Phone, (800) 899-1712 or (949) 362-2050 (ext 532); fax, (949) 362-2049; reprints@aacn.org.
References
- 1.Angus DC, Barnato AE, Linde-Zwirble WT, et al. Robert Wood Johnson Foundation ICU End-Of-Life Peer Group. Use of intensive care at the end of life in the United States: An epidemiologic study. Crit Care Med. 2004;32(3):638–643. doi: 10.1097/01.ccm.0000114816.62331.08. [DOI] [PubMed] [Google Scholar]
- 2.Angus DC, Shorr AF, White A, Dremsizov TT, Schmitz RJ, Kelley MA Committee on Manpower for Pulmonary and Critical Care Societies (COMPACCS) Critical care delivery in the United States: distribution of services and compliance with Leapfrog recommendations. Crit Care Med. 2006;34(4):1016–1024. doi: 10.1097/01.CCM.0000206105.05626.15. [DOI] [PubMed] [Google Scholar]
- 3.Happ MB. Communicating with mechanically ventilated patients: State of the science. AACN Clin Issues. 2001;12(2):247–258. doi: 10.1097/00044067-200105000-00008. [DOI] [PubMed] [Google Scholar]
- 4.Pennock BE, Crawshaw L, Maher T, Price T, Kaplan PD. Distressful events in the ICU as perceived by patients recovering from coronary artery bypass surgery. Heart Lung. 1994;23(4):323–327. [PubMed] [Google Scholar]
- 5.Rotondi AJ, Chelluri L, Sirio C, et al. Patients’ recollections of stressful experiences while receiving prolonged mechanical ventilation in an intensive care unit. Crit Care Med. 2002;30(4):746–752. doi: 10.1097/00003246-200204000-00004. [DOI] [PubMed] [Google Scholar]
- 6.Nelson JE, Meier DE, Litke A, Natale DA, Siegel RE, Morrison RS. The symptom burden of critical illness. Crit Care Med. 2004;32:1527–1534. doi: 10.1097/01.ccm.0000129485.08835.5a. [DOI] [PubMed] [Google Scholar]
- 7.Nelson JE, Meier DE, Oei EJ, et al. Self-reported symptom experience of critically ill cancer patients receiving intensive care. Crit Care Med. 2001;29(2):277–282. doi: 10.1097/00003246-200102000-00010. [DOI] [PubMed] [Google Scholar]
- 8.Bergbom-Engberg I, Haljamae H. Assessment of patients’ experience of discomforts during respirator therapy. Crit Care Med. 1989;17(10):1068–1072. doi: 10.1097/00003246-198910000-00021. [DOI] [PubMed] [Google Scholar]
- 9.Carroll SM. Nonvocal ventilated patients’ perceptions of being misunderstood. Western J Nurs Res. 2004;26:85–103. doi: 10.1177/0193945903259462. [DOI] [PubMed] [Google Scholar]
- 10.Menzel LK. Factors related to the emotional responses of intubated patients to being unable to speak. Heart Lung. 1998;27(4):245–252. doi: 10.1016/s0147-9563(98)90036-x. [DOI] [PubMed] [Google Scholar]
- 11.Patak L, Gawlinski A, Fung NI, Doering L, Berg J. Patients’ reports of health care practitioner interventions that are related to communication during mechanical ventilation. Heart Lung. 2004;33:323–327. doi: 10.1016/j.hrtlng.2004.02.002. [DOI] [PubMed] [Google Scholar]
- 12.Leathart AJ. Communication and socialisation (2): Perceptions of neophyte ITU nurses. Intensive Crit Care Nurs. 1994;10(2):142–154. doi: 10.1016/0964-3397(94)90011-6. [DOI] [PubMed] [Google Scholar]
- 13.Alasad J, Ahmad M. Communication with critically ill patients. J Adv Nurs. 2005;50(4):356–362. doi: 10.1111/j.1365-2648.2005.03400.x. [DOI] [PubMed] [Google Scholar]
- 14.Happ MB, Sereika S, Garrett K, Tate J. Use of quasi-experimental sequential cohort design in the Study of Patient-Nurse Effectiveness with Assisted Communication Strategies (SPEACS) Contemp ClinTrials. 2008;29(5):801–808. doi: 10.1016/j.cct.2008.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Fitch M. The patient’s reaction to ventilation. Can Crit Care Nurs J. 1989;6(2):13–16. [PubMed] [Google Scholar]
- 16.Gries ML, Fernsler J. Patient perceptions of the mechanical ventilation experience. Focus Crit Care. 1988;15(2):52–59. [PubMed] [Google Scholar]
- 17.Jablonski RS. The experience of being mechanically ventilated. Qual Health Res. 1994;4(2):186–207. [Google Scholar]
- 18.Wojnicki-Johansson G. Communication between nurse and patient during ventilator treatment: Patient reports and RN evaluations. Intensive Crit Care Nurs. 2001;17(1):29–39. doi: 10.1054/iccn.2000.1547. [DOI] [PubMed] [Google Scholar]
- 19.Robillard AB. Communication problems in the intensive care unit. Qual Soc. 1994;17(4):383–395. [Google Scholar]
- 20.Happ MB. Interpretation of nonvocal behavior and the meaning of voicelessness in critical care. Soc Sci Med. 2000;50(9):1247–1255. doi: 10.1016/s0277-9536(99)00367-6. [DOI] [PubMed] [Google Scholar]
- 21.Magnus VS, Turkington L. Communication interaction in ICU: patient and staff experiences and perceptions. Intensive Crit Care Nurs. 2006;22:167–180. doi: 10.1016/j.iccn.2005.09.009. [DOI] [PubMed] [Google Scholar]
- 22.McCabe C. Nurse-patient communication: an exploration of patients’ experiences. J Clin Nurs. 2004;13:41–49. doi: 10.1111/j.1365-2702.2004.00817.x. [DOI] [PubMed] [Google Scholar]
- 23.Carroll SM. Silent, slow lifeworld: the communication experience of nonverbal patients. Qual Health Res. 2007;17(9):1165–1177. doi: 10.1177/1049732307307334. [DOI] [PubMed] [Google Scholar]
- 24.Fowler SB. Impaired verbal communication during short-term oral intubation. Nurs Diagn. 1997;8(3):93–98. doi: 10.1111/j.1744-618x.1997.tb00317.x. [DOI] [PubMed] [Google Scholar]
- 25.Ashworth P. RCN Research Series. London: Whitefriars Press; 1980. Care to Communicate: An Investigation Into Problems of Communication Between Patients and Nurses in Intensive Therapy Units. [Google Scholar]
- 26.Leathart AJ. Communication and socialisation (1): An exploratory study and explanation for nurse-patient communication in an ITU. Intensive Crit Care Nurs. 1994;10(2):93–104. doi: 10.1016/0964-3397(94)90004-3. [DOI] [PubMed] [Google Scholar]
- 27.Salyer J, Stuart BJ. Nurse-patient interaction in the intensive care unit. Heart Lung. 1985;14(1):20–24. [PubMed] [Google Scholar]
- 28.Hall DS. Interactions between nurses and patients on ventilators. Am J Crit Care. 1996;5(4):293–297. [PubMed] [Google Scholar]
- 29.Happ MB, Roesch TK, Garrett K. Electronic voice-output communication aids for temporarily nonspeaking patients in a medical intensive care unit: a feasibility study. Heart Lung. 2004;33(2):92–101. doi: 10.1016/j.hrtlng.2003.12.005. [DOI] [PubMed] [Google Scholar]
- 30.Happ MB, Tuite P, Dobbin K, DiVirgilio-Thomas D, Kitutu J. Communication ability, method, and content among non-speaking nonsurviving patients treated with mechanical ventilation in the intensive care unit. Am J Crit Care. 2004;13(3):210–218. [PubMed] [Google Scholar]
- 31.Connolly M. doctoral dissertation. Chicago, Ill: Rush University; 1992. Temporarily Nonvocal Trauma Patients and Their Gestures:A Descriptive Study. [Google Scholar]
- 32.de los Rios Castillo S-SJ. Well-being and medical recovery in the critical care unit: the role of the nurse-patient interaction. Salud Mental. 2002;25(2):21–31. [Google Scholar]
- 33.Teasdale G, Jennett B. Assessment of coma and impaired consciousness: a practical scale. Lancet. 1974;2(7872):81–84. doi: 10.1016/s0140-6736(74)91639-0. [DOI] [PubMed] [Google Scholar]
- 34.Bergbom-Engberg I, Haljamae H. The communication process with ventilator patients in the ICU as perceived by the nursing staff. Intensive Crit Care Nurs. 1993;9(1):40–47. doi: 10.1016/0964-3397(93)90008-l. [DOI] [PubMed] [Google Scholar]
- 35.Ashworth PM. Staff-patient communication in coronary care units. J Adv Nurs. 1984;9(1):35–42. doi: 10.1111/j.1365-2648.1984.tb00341.x. [DOI] [PubMed] [Google Scholar]
- 36.Paterson BL. A framework to identify reactivity in qualitative research. Western J Nurs Res. 1994;16(3):301–316. doi: 10.1177/019394599401600306. [DOI] [PubMed] [Google Scholar]
- 37.Haidet KK, Tate J, Divirgilio-Thomas D, Kolanowski A, Happ MB. Methods to improve reliability of video-recorded behavioral data. Res Nurs Health. 2009;32(4):465–474. doi: 10.1002/nur.20334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Knaus WA, Wagner DP, Draper EA, et al. The APACHE III prognostic system: risk prediction of hospital mortality for critically ill hospitalized adults. Chest. 1991;100(6):1619–1636. doi: 10.1378/chest.100.6.1619. [DOI] [PubMed] [Google Scholar]
- 39.Wagner DP, Knaus WA, Harrell FE, Zimmerman JE, Watts C. Daily prognostic estimates for critically ill adults in intensive care units: results from a prospective, multicenter, inception cohort analysis. Crit Care Med. 1994;22(9):1359–1372. doi: 10.1097/00003246-199409000-00004. [DOI] [PubMed] [Google Scholar]
- 40.Inouye SK, van Dyck CH, Alessi CA, Balkin S, Siegal AP, Horwitz RI. Clarifying confusion: the confusion assessment method—a new method for detection of delirium [see comment] Ann Intern Med. 1990;113(12):941–948. doi: 10.7326/0003-4819-113-12-941. [DOI] [PubMed] [Google Scholar]
- 41.Ely EW, Inouye SK, Bernard GR, et al. Delirium in mechanically ventilated patients: validity and reliability of the confusion assessment method for the intensive care unit (CAM-ICU) JAMA. 2001;286(21):2703–2710. doi: 10.1001/jama.286.21.2703. [DOI] [PubMed] [Google Scholar]
- 42.Sessler CN, Gosnell MS, Grap MJ, et al. The Richmond Agitation-Sedation Scale: validity and reliability in adult intensive care unit patients. Am J Respir Crit Care Med. 2002;166(10):1338–1344. doi: 10.1164/rccm.2107138. [DOI] [PubMed] [Google Scholar]
- 43.Ely EW, Truman B, Shintani A, et al. Monitoring sedation status over time in ICU patients: reliability and validity of the Richmond Agitation-Sedation Scale (RASS) JAMA. 2003;289(22):2983–2991. doi: 10.1001/jama.289.22.2983. [DOI] [PubMed] [Google Scholar]
- 44.Calculator S, Luchko CD. Evaluating the effectiveness of a communication board training program. J Speech Hearing Disorders. 1983;48(2):185–191. doi: 10.1044/jshd.4802.185. [DOI] [PubMed] [Google Scholar]
- 45.Morse JM, Beres MA, Spiers JA, Mayan M, Olson K. Identifying signals of suffering by linking verbal and facial cues. Qual Health Res. 2003;13(8):1063–1077. doi: 10.1177/1049732303256401. [DOI] [PubMed] [Google Scholar]
- 46.Topf M. Three estimates of inter-rater reliability for nominal data. Nurs Res. 1986;35:253–255. doi: 10.1097/00006199-198607000-00020. [DOI] [PubMed] [Google Scholar]
- 47.Garrett K. Topics of nurse-patient communication in the ICU. Paper presented at: CANS 2008, National State of the Science Congress on Nursing Research; October 2–4, 2008; Washington, DC. [Google Scholar]
- 48.Puntillo KA. Pain experiences of intensive care unit patients. Heart Lung. 1990;19(5 Pt 1):526–533. [PubMed] [Google Scholar]
- 49.Puntillo KA, Smith D, Arai S, Stotts N. Critical care nurses provide their perspectives of patients’ symptoms in intensive care units. Heart Lung. 2008;37(6):466–475. doi: 10.1016/j.hrtlng.2008.02.002. [DOI] [PubMed] [Google Scholar]
- 50.Critical Care Workforce Partnership. [Accessed December 15, 2010];Critical Care Workforce Partnership Position Statement: The Aging of the US Population and Increased Need for Critical Care Services. 2001 www.aacn.org/WD/.../Critical_Care_Workforce_Position_Statement.pdf.