Abstract
BACKGROUND
Associations of decline in functional performance with clinically-important outcomes in patients with peripheral arterial disease (PAD) are unknown.
OBJECTIVES
We hypothesized that greater two-year decline in office-based functional performance measures would be associated with greater mobility loss and mortality in people with PAD.
METHODS
440 men and women with PAD completed the six-minute walk test and measures of walking velocity at baseline and annually for two years. Participants were categorized into tertiles according to their functional decline between baseline and two-year follow-up and were followed annually after the functional change assessment. Cox proportional hazard models were used to assess relations between the two-year change in functional performance with later mortality and mobility loss, adjusting for age, sex, race, the ankle brachial index, comorbidities, and other confounders.
RESULTS
One hundred two participants (23.2%) died during a median follow-up of 44.5 months after functional change was assessed. Of 319 participants without baseline mobility disability, 60 (18.8%) developed mobility loss after functional change was assessed. Participants in the tertile with greatest six-minute walk decline had the highest subsequent mobility loss (Hazard Ratio (HR)=3.50, 95% Confidence Interval (CI)=1.56–7.85, p=0.002), all-cause mortality (HR=2.16, 95% CI=1.28–3.64, p=0.004), and cardiovascular disease (CVD) mortality (HR=2.45, 95% CI=1.08–5.54, p=0.031), compared to those with the smallest six-minute walk decline. Greater declines in fastest paced four-meter walking velocity were associated with higher mobility loss (P trend=0.018), all-cause mortality (P trend=0.01) and CVD mortality (P trend=0.004).
CONCLUSION
PAD participants with declining functional performance are at increased risk for later mobility loss and mortality.
Keywords: peripheral vascular disease, mortality, physical functioning
Men and women with lower extremity peripheral arterial disease (PAD) have greater functional impairment, faster functional decline, and higher all-cause and cardiovascular disease mortality, compare to individuals without PAD (1–3). Previous studies demonstrate that baseline performance on office-based functional measures predicts subsequent mobility loss and mortality in patients with PAD (4,5).
It is unknown whether greater declines in office-based functional performance measures predict increased subsequent mobility loss or mortality in PAD. Declining performance may indicate deteriorating health associated with increased risk of later outcomes. Among men and women with PAD, we studied associations between two-year change in lower extremity performance and subsequent mobility loss and mortality, after the functional change was assessed. Functional performance measures assessed included the six-minute walk test, walking velocity over four meters at usual and fastest pace, and the short physical performance battery (SPPB). We hypothesized that PAD participants with greater decline in these functional performance measures over a two-year period would have higher subsequent rates of mobility loss, all-cause mortality, and cardiovascular disease mortality, compared to PAD participants with less decline. In secondary analyses, we assessed the relative value of baseline functional performance vs. two-year change in functional performance for predicting later mobility loss and mortality in participants with PAD.
METHODS
Participant Identification
The institutional review boards of Northwestern University and Catholic Health Partners Hospital approved the protocol. Participants gave written informed consent.
Participants were part of the Walking and Leg Circulation Study (WALCS) and WALCS II prospective, observational studies designed to identify clinical characteristics associated with functional decline and mortality in PAD (2–7). PAD participants were identified from among consecutive patients in three Chicago-area non-invasive vascular laboratories. Participants in WALCS were enrolled between 1998 and 2000 and returned annually for up to eight follow-up visits. Newly identified participants with PAD were enrolled between 2002 and 2004 as part of the WALCS II cohort and returned annually for up to four follow-up visits. WALCS participants were age 55 or older at enrollment (2,3). Newly identified WALCS II participants, enrolled four years after the WALCS cohort, were age 59 and older at enrollment (6). PAD participants from WALCS and WALCS II were included in this study if they attended a baseline visit and at least two annual follow-up visits and continued to be followed for later mortality and/or mobility loss.
All participants had an ankle brachial index (ABI) < 0.90 at their baseline visit (2–7). Exclusion criteria have been previously reported (6,7). Briefly, nursing home residents, wheel-chair bound individuals, and lower-extremity amputees were excluded. Potential participants with dementia, non-English speakers, and those with recent major surgery were excluded. Participants who underwent lower extremity revascularization during the first two years of the study, when change in functional performance was evaluated, were excluded from all analyses. Participants who underwent lower extremity revascularization after the assessment of functional change were excluded from analyses of mobility loss.
Ankle Brachial Index Measurement
A hand-held Doppler probe (Nicolet Vascular Pocket Dop II; Nicolet Biomedical Inc, Golden, CO) was used to obtain systolic pressures in the right and left brachial, dorsalis pedis, and posterior tibial arteries (2–7). Each pressure was measured twice. The ABI was calculated by dividing the mean of the dorsalis pedis and posterior tibial pressures in each leg by the mean of the four brachial pressures (8). Average brachial pressures in the arm with the highest pressure were used when one brachial pressure was higher than the opposite brachial pressure in both measurement sets and the two brachial pressures differed by 10 mm Hg or more in at least one measurement set, since in such cases subclavian stenosis was possible (9). Zero values (N=17) for the dorsalis pedis or posterior tibial vessels were excluded from the ABI calculation. The lowest leg ABI was used in analyses.
Change in Functional Performance
All participants underwent baseline measures of functional performance and returned annually for two years for assessment of change in functional performance. Change in functional performance between baseline and two-year follow-up was studied for its association with subsequent mobility loss and mortality, occurring after the two-year change in functional performance assessment was assessed.
Six-Minute Walk
Following a standardized protocol (10,11), participants walked up and down a 100-ft hallway for six minutes after instructions to cover as much distance as possible. The intra-class correlation coefficient for test re-test reliability of the six-minute walk was 0.90 (P<.001) in our laboratory among 156 PAD participants who completed the tests approximately one to two weeks apart (12).
Four-meter walking velocity
Walking velocity was measured with a four-meter walk performed at “usual” and “fastest” pace (2–4,7). For the “usual” paced walk, participants were instructed to walk at their usual pace, “as if going down the street to the store.” Each walk was performed twice. The faster walk in each pair was used in analyses (2–4,7,13,14).
Repeated chair rises
Participants sit in a straight-backed chair with arms folded across their chest and stand five times consecutively as quickly as possible. Time to complete five chair rises was measured (13,14).
Standing balance
Participants were asked to hold three increasingly difficult standing positions for ten seconds each: standing with feet together side-by-side and parallel (side-by-side stand), standing with feet parallel with the toes of one foot adjacent to and touching the heel of the opposite foot (semi-tandem stand), and standing with one foot directly in front of the other (tandem stand) (13,14).
Short Physical Performance Battery
The Short Physical Performance Battery (SPPB) combines data from the usual paced four-meter walking velocity, time to rise from a seated position five times, and standing balance. Individuals receive a zero score for each task they are unable to complete. Scores of one to four are assigned for remaining tasks, based upon quartiles of performance for over 6,000 participants in the Established Populations for the Epidemiologic Study of the Elderly (13,14). Scores are summed to obtain the SPPB, ranging from 0 to 12.
Mobility Measures
At baseline and subsequent follow-up visits, participants were asked whether they were able to walk ¼ mile and whether they could climb up and down one flight of stairs, selecting one of the following three response options for each measure: a) “yes, on my own”; b) ”yes, with help”; or c) ”no, not at all.” Participants eligible for analyses of mobility loss were those who reported the ability to walk ¼ mile and climb up and down one flight of stairs on their own at the baseline, first annual follow-up, and second annual follow-up visits. Mobility loss was defined as becoming unable to walk ¼ mile or walk up and down one flight of stairs without assistance after the second annual follow-up visit (5,15,16).
Death
We used the Social Security Administration Death Index to search for deaths through 5/23/2009. Information on deaths was also obtained from family members, proxies, and primary care physicians. Death certificates were obtained from the state in which death occurred or from the patients' medical record. Cardiovascular disease deaths were those with International Classification of Disease-10 codes in the range I01.0 through I99.9, including deaths due to coronary heart disease, stroke, peripheral vascular disease, and other cardiovascular disease (4).
Comorbidities
Comorbidities assessed included diabetes, angina, myocardial infarction, heart failure, cancer, chronic lung disease, lower extremity arthritis, spinal stenosis, spinal disk disease, and stroke. Disease-specific algorithms that combine data from patient report, medical record review, medications, laboratory values, and a questionnaire completed by the participant's primary care physician were used to verify and document baseline comorbidities, based on criteria previously developed (17). American College of Rheumatology criteria were used to diagnose knee and hip osteoarthritis (18,19).
Medication Identification
The study principal investigator (MMM), blinded to all other patient data, reviewed lists of medications at the baseline visit and identified presence vs. absence of statin use and use of PAD-related medications (cilostazol or pentoxifylline).
Other Measures
Body mass index (BMI) was calculated as weight (kilograms)/(height (meters))2. Cigarette smoking history was determined from patient report. To measure physical activity, participants were asked, “During the last week, how many city blocks or their equivalent did you walk?” (20). This measure of patient-reported physical activity is highly correlated with vertical accelerometer-measured physical activity in PAD participants (20).
Statistical Analyses
Baseline characteristics between PAD participants with and without mobility loss and between survivors and decedents were compared using general linear models for continuous variables and chi-square tests for categorical variables, adjusting for age. We assumed a linear association of age with continuous study variables. We used logistic regression to adjust for age for categorical variables.
We did not observe a threshold effect for the associations of change in functional performance measures with each study outcome. Therefore, participants were categorized into tertiles according to their change in each functional performance measure between baseline and two-year follow-up. The decision to classify participants into tertiles was made in an a priori fashion. Proportional hazards analyses were used to compare differences in mobility loss, all-cause mortality, and cardiovascular disease mortality across tertiles of two-year change in functional performance. The third tertile represented the least functional decline and the first tertile represented the greatest functional decline. Proportional hazards analyses were performed to determine associations of each tertile with mobility loss, all-cause mortality, and cardiovascular disease mortality, adjusting for age, sex, race, and baseline functional performance (Model I). These proportional hazards analyses were repeated with additional adjustment for comorbidities, cigarette smoking (pack-years), BMI, ABI, physical activity, relevant medications, and study cohort (WALCS vs. WALCS II) (Model II). Ordinal values (i.e. 1,2,3) were entered for each tertile in the analyses. For the models relating change in functioning to mobility loss, comorbidities included in Model II were diabetes, angina, myocardial infarction, heart failure, cancer, chronic lung disease, lower extremity arthritis, spinal stenosis, spinal disk disease, and stroke. For models relating change in functioning to mortality, comorbidities included in Model II were diabetes, angina, myocardial infarction, heart failure, cancer, chronic lung disease, and stroke. For the models relating change in functioning to mobility loss, relevant medications included in Model II were cilostazol, pentoxifylline, and statins. For the models relating change in functioning to mortality, relevant medications included in Model II were statins. Proportional hazards models were repeated in which a standardized regression coefficient was used in place of tertile measurements for the change in functioning variable. These analyses using standardized regression coefficients allowed us to compare the magnitude of the association of the change in functioning variable to the variable for baseline functional performance. For all proportional hazards models, we tested for the proportional hazards assumption (21). The proportional hazards assumption was valid through the first 72 months of follow-up after baseline testing. Therefore, our models were truncated at 72 month follow-up. Analyses were performed using SAS statistical software (PHREG procedures, Version 9.1, SAS Institute Inc, Cary, NC).
RESULTS
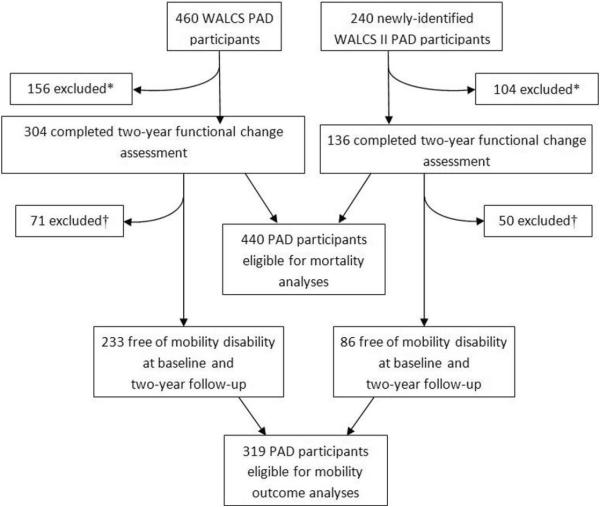
A total of 440 PAD participants were eligible for the mortality outcome analyses and 319 were eligible for the mobility loss analyses (see Figure 1). There were no differences in the prevalence of males (55.0% vs. 56.8%) or African-Americans (18.5% vs. 16.6%) between potential participants who were ineligible vs. eligible, respectively. However, ineligible participants had poorer six-minute walk performance (1,017 vs. 1,174 feet, p<0.001), slower usual paced four-meter walking velocity (0.83 vs. 0.89 meters/second, P<0.01), slower fast-paced four-meter walking velocity (1.12 vs. 1.21 meters/second, P<0.01), lower SPPB scores (9.26 vs. 9.83, p<0.01), and lower ABI values (0.62 vs. 0.66, p<0.01), compared to eligible participants.
Figure 1. Depiction of eligible participants from the WALCS and WALCS II cohorts.
*Excluded because they did not return annually for 2 years for functional assessment after baseline (N=198), they underwent lower extremity revascularization during the first 2 years of follow-up (N=48), they were lost to follow-up after their two-year functional change assessment (N=8) or they had missing variables in the fully adjusted models (N=6).
†Excluded because they met criteria for mobility disability between baseline and 2-year follow-up (N=76) or they were missing data on their mobility status during follow-up (N=45) WALCS – Walking and Leg Circulation Study
Overall median follow-up after baseline measures was 72.0 months (inter-quartile range 50.0 to 97.0 months). Median follow-up for study outcomes after assessment of two-year change in functioning was 44.5 months (inter-quartile range-26.0 to 73.0 months). Death certificates were obtained for 92 (90.2%) decedents. Thirty-nine deaths (38.2%) were due to cardiovascular disease and 20 (19.6%) were due to cancer.
Table 1 shows baseline characteristics of PAD participants according to the outcomes of mobility loss and mortality. Adjusting for age, PAD participants who developed mobility loss included higher proportions of women and participants with diabetes mellitus. PAD participants who developed mobility loss had poorer baseline functional performance compared to those who remained free of mobility disability during follow-up. Adjusting for age, participants who died during follow-up included higher proportions of participants with history of angina, heart failure, and diabetes mellitus compared to survivors. At baseline, decedents had poorer baseline functional performance compared to survivors (Table 1).
Table 1.
Age-adjusted Associations of Study Characteristics with Mortality and Mobility Loss among Participants with Peripheral Arterial Disease.
| MOBILITY DISABILITY OUTCOME | ||||
|---|---|---|---|---|
| Participants free of mobility disability at baseline (N=319) | Participants remaining free of mobility disability during follow-up (N=259) | Participants who developed mobility loss during follow-up (N=60) | P Value comparing participants with vs. without mobility disability during follow-up | |
| Ankle brachial index | 0.67 (0.14) | 0.66 (0.01) | 0.68 (0.02) | 0.399 |
| Body mass index (kg/M2) | 27.23 (4.96) | 26.87 (0.31) | 28.12 (0.64) | 0.081 |
| Male Gender (%) | 60.82 | 64.28 | 42.85 | 0.003 |
| African American (%) | 15.99 | 14.35 | 17.42 | 0.562 |
| Current smoker (%) | 19.12 | 15.87 | 15.67 | 0.972 |
| Angina (%) | 29.47 | 30.36 | 27.54 | 0.67 |
| Myocardial Infarction (%) | 22.88 | 21.07 | 31.34 | 0.097 |
| Pulmonary disease (%) | 28.21 | 25.85 | 31.34 | 0.405 |
| PAD Participants free of mobility disability at baseline (N=319) | Participants remaining free of mobility disability during follow-up (N=259) | Participants who developed mobility loss during follow-up (N=60) | P Value comparing participants with vs. without mobility disability during follow-up | |
|---|---|---|---|---|
| Cancer (%) | 15.67 | 16.75 | 12.1 | 0.369 |
| Heart Failure (%) | 18.18 | 17.99 | 17.05 | 0.867 |
| Diabetes Mellitus (%) | 28.84 | 21.73 | 43.14 | 0.002 |
| Six minute walk (feet) | 1258.46 (323.57) | 1307.84 (19.16) | 1023.53 (39.05) | <.001 |
| Usual pace four-meter walking velocity (meters/second) | 0.94 (0.19) | 0.97 (0.01) | 0.80 (0.02) | <.001 |
| Fastest pace four meter walking velocity (meters/second) | 1.28 (0.25) | 1.32 (0.01) | 1.07 (0.03) | <.001 |
| SPPB (0–12 score, 12=best) | 10.34 (1.87) | 10.66 (0.10) | 8.58 (0.22) | <.001 |
| ALL-CAUSE MORTALITY OUTCOME | ||||
|---|---|---|---|---|
| Baseline Characteristics (N=440) | Survivors (N=338) | Decedents (N=102) | P Value comparing decedents and survivors | |
| Ankle brachial index | 0.66 (0.15) | 0.67 (0.01) | 0.64 (0.01) | 0.084 |
| Body mass index (kg/M2) | 27.52 (5.49) | 27.62 (0.29) | 27.21 (0.54) | 0.508 |
| Male Gender (%) | 56.82 | 54.5 | 65.07 | 0.064 |
| African American (%) | 16.59 | 15.39 | 19.39 | 0.352 |
| Current smoker (%) | 15.68 | 12.8 | 14.67 | 0.635 |
| Angina (%) | 31.14 | 26.77 | 45.09 | 0.001 |
| Myocardial Infarction (%) | 23.64 | 21.4 | 30.74 | 0.055 |
| Pulmonary disease (%) | 32.73 | 30.81 | 38.95 | 0.132 |
| Cancer (%) | 15.45 | 16.04 | 13.01 | 0.456 |
| Heart Failure (%) | 21.36 | 17.71 | 33.51 | 0.001 |
| Diabetes Mellitus (%) | 32.05 | 25.95 | 47.83 | <0.001 |
| Six minute walk (feet) | 1173.61 (369.02) | 1199.57 (19.48) | 1086.74 (35.88) | 0.006 |
| Usual pace four-meter walking velocity (meters/second) | 0.89 (0.21) | 0.91 (0.01) | 0.86 (0.02) | 0.040 |
| Fastest pace four meter walking velocity (meters/second) | 1.21 (0.29) | 1.22 (0.01) | 1.18 (0.03) | 0.257 |
| SPPB (0–12 score, 12=best) | 9.83 (2.36) | 9.98 (0.12) | 9.26 (0.23) | 0.005 |
Data shown are means (standard errors)
Adjusting for age, sex, race, and baseline functional performance (Model I), greater declines between baseline and two-year follow-up in the usual-paced walking velocity (P trend<0.001), fast-paced walking velocity (P trend=0.014), and the SPPB (P trend<0.001) were each associated with higher rates of mobility loss after the functional change assessment (Table 2). After additional adjustment for comorbidities, BMI, relevant medications, smoking, study cohort (WALCS vs. WALCS II), physical activity, and the ABI, greater two-year declines in the six-minute walk, usual and fast-paced four-meter walking velocity, and the SPPB score were associated with a higher rate of subsequent mobility loss (Table 2).
Table 2.
Adjusted Associations of Two- Year Change in Functional Performance Measures with Mortality and Mobility Loss among Participants with Peripheral Arterial Disease
| Model I | Model II | ||||
|---|---|---|---|---|---|
| Functional performance measures | Tertiles | Standardized Hazard Ratio (95% Confidence Interval) | P Trend Value | Standardized Hazard Ratio (95% Confidence Interval) | P Trend Value |
| Mobility Loss (N=324) | |||||
| Six minute walk | Tertile 1 | 1.85 (0.99–3.47) | 0.051 | 3.50 (1.56–7.85)1 | 0.003 |
| Tertile 2 | 1.79 (0.88–3.63) | 3.03 (1.28–7.15)2 | |||
| Tertile 3 | 1.00 (Reference) | 1.00 (Reference) | |||
| Four meter velocity, usual pace | Tertile 1 | 3.40 (1.64–7.05)1 | <0.001 | 3.67 (1.59–8.48)1 | 0.001 |
| Tertile 2 | 1.95 (1.07–3.54) | 2.45 (1.23–4.88)2 | |||
| Tertile 3 | 1.00 (Reference) | 1.00 (Reference) | |||
| Four meter velocity, fast pace | Tertile 1 | 2.35 (1.17–4.74)4 | 0.014 | 2.45 (1.15–5.23)3 | 0.018 |
| Tertile 2 | 1.87 (0.98–3.57) | 2.80 (1.32–5.91)1 | |||
| Tertile 3 | 1.00 (Reference) | 1.00 (Reference) | |||
| Short Physical Performance Battery | Tertile 1 | 4.43 (1.97–9.96)1 | <0.001 | 5.57 (2.20–14.12)1 | 0.0002 |
| Tertile 2 | 1.70 (0.66–4.37) | 1.99 (0.71–5.57) | |||
| Tertile 3 | 1.00 (Reference) | 1.00 (Reference) | |||
| Model I | Model II | ||||
|---|---|---|---|---|---|
| Functional performance measures | Tertiles | Hazard Ratio (95% Confidence Interval) | P Trend Value | Hazard Ratio (95% Confidence Interval) | P Trend Value |
| All-Cause Mortality (N=445) | |||||
| Six minute walk | Tertile 1 | 2.28 (1.37–3.80)1 | <0.001 | 2.16 (1.28–3.64)1 | 0.001 |
| Tertile 2 | 1.18 (0.67–2.08) | 0.93 (0.51–1.70) | |||
| Tertile 3 | 1.00 (Reference) | 1.00 (Reference) | |||
| Four meter velocity, usual pace | Tertile 1 | 1.54 (0.94–2.53) | 0.098 | 1.31 (0.77–2.23) | 0.001 |
| Tertile 2 | 1.02 (0.62–1.67) | 1.01 (0.61–1.67) | |||
| Tertile 3 | 1.00 (Reference) | 1.00 (Reference) | |||
| Four meter velocity, fast pace | Tertile 1 | 2.60 (1.51–4.48)1 | <0.001 | 2.14 (1.20–3.79)1 | 0.010 |
| Tertile 2 | 1.85 (1.07–3.19)2 | 1.61 (0.91–2.85) | |||
| Tertile 3 | 1.00 (Reference) | 1.00 (Reference) | |||
| Short Physical Performance Battery | Tertile 1 | 1.62 (0.93–2.81) | 0.055 | 1.42 (0.79–2.54) | 0.170 |
| Tertile 2 | 0.95 (0.51–1.76) | 0.87 (0.46–1.65) | |||
| Tertile 3 | 1.00 (Reference) | 1.00 (Reference) | |||
| Model I | Model II | ||||
|---|---|---|---|---|---|
| Functional performance measures | Tertiles | Hazard Ratio (95% Confidence Interval) | P Trend Value | Hazard Ratio (95% Confidence Interval) | P Trend Value |
| Cardiovascular Mortality (N=445) | |||||
| Six minute walk | Tertile 1 | 2.21 (1.01–4.85)5 | 0.174 | 2.45 (1.08–5.54)4 | 0.012 |
| Tertile 2 | 0.54 (0.19–1.53) | 0.48 (0.16–1.44) | |||
| Tertile 3 | 1.00 (Reference) | 1.00 (Reference) | |||
| Four meter velocity, usual pace | Tertile 1 | 1.91 (0.85–4.24) | 0.111 | 1.92 (0.78–4.73) | 0.176 |
| Tertile 2 | 0.90 (0.38–2.11) | 1.01 (0.41–2.44) | |||
| Tertile 3 | 1.00 (Reference) | 1.00 (Reference) | |||
| Four meter velocity, fast pace | Tertile 1 | 6.97 (2.31–21.05)1 | <0.001 | 4.86 (1.53–15.47)1 | 0.004 |
| Tertile 2 | 2.94 (0.92–9.42) | 2.51 (0.76–8.30) | |||
| Tertile 3 | 1.00 (Reference) | 1.00 (Reference) | |||
| Short Physical Performance Battery | Tertile 1 | 2.67 (1.08–5.54) | 0.041 | 1.67 (0.56–5.02) | 0.346 |
| Tertile 2 | 1.51 (0.47–4.78) | 1.33 (0.40–4.39) | |||
| Tertile 3 | 1.00 (Reference) | 1.00 (Reference) | |||
P < 0.01
P=0.01
P=0.02
P=0.03
P=0.047
In analyses adjusting for age, sex, race, and baseline functional performance (Model I), greater declines between baseline and two-year follow-up in six-minute walk performance (P trend<0.001) and fast-paced walking velocity (P trend<0.004) were associated with higher all-cause mortality during subsequent follow-up (Table 2, Model I). After additional adjustment for comorbidities, relevant medications, BMI, smoking, study cohort, physical activity, and the ABI (Model II), greater declines in the six-minute walk test (P trend=0.001), usual-paced four-meter walking velocity (P trend=0.001), and fast-paced four-meter walking velocity (P trend=0.010), were associated with higher all-cause mortality (Table 2, Model II).
Adjusting for age, sex, race, and baseline functional performance (Model I), greater declines between baseline and two-year follow-up in the fast-paced walking velocity (P trend=0.049) and SPPB (P trend=0.041) were each associated with higher rates of subsequent cardiovascular disease mortality (Table 2). After additional adjustment for comorbidities, BMI, smoking, relevant medications, study cohort, physical activity, and the ABI, greater declines in the six-minute walk (P trend=0.012) and fast-paced walking velocity (P trend=0.004) were each associated with higher rates of cardiovascular disease mortality during follow-up after the functional change was assessed (Table 2, Model II).
Table 3 shows standardized hazard ratios from statistical models including associations of both baseline functional performance measures and change in each functional performance measure with study outcomes. These analyses, using standardized hazard ratios, allow direct comparison of baseline functional performance measures and change in functional performance as predictors of study outcomes. Adjusting for age, sex, race, comorbidities, ABI, BMI, smoking, physical activity, relevant medications, and study cohort, poorer baseline six-minute walk performance (P<0.001) and greater decline in six-minute walk performance (P=0.007) were each associated with increased rates of mobility loss during follow-up after the functional change assessment (Table 3, Model II). Similarly, for the remaining functional measures, poorer baseline performance and greater declines in performance were each associated independently and significantly with higher rates of mobility loss in fully adjusted analyses (Table 3, Model II).
Table 3.
Adjusted Comparisons of Baseline Functional Performance Measures and Two-Year Change in Functional Performance Measures with Mortality and Mobility Loss Among Participants with Peripheral Arterial Disease (N=446)
| Model I | Model II | ||||
|---|---|---|---|---|---|
| Functional performance measures | Measurement | Standardized Hazard Ratio (95% Confidence Interval) | P value | Standardized Hazard Ratio (95% Confidence Interval) | P value |
| Mobility Loss (N=324) | |||||
| Six minute walk | Two-year change in performance. | 0.86 (0.76 – 0.96) | 0.01 | 0.82 (0.71 – 0.95) | 0.007 |
| Baseline value | 0.39 (0.30 – 0.51) | <0.001 | 0.31 (0.21 – 0.47) | <0.001 | |
| Four meter velocity, usual pace | Two-year change in performance. | 0.74 (0.63 – 0.87) | <0.001 | 0.77 (0.66 – 0.92) | 0.003 |
| Baseline value | 0.23 (0.15 – 0.35) | <0.001 | 0.21 (0.12 – 0.35) | <0.001 | |
| Four meter velocity, fast pace | Two-year change in performance. | 0.78 (0.67 – 0.89) | <0.001 | 0.80 (0.69 – 0.92) | 0.002 |
| Baseline value | 0.31 (0.22 – 0.43) | <0.001 | 0.29 (0.19 – 0.46) | <0.001 | |
| Short Physical Performance Battery | Two-year change in performance. | 0.73 (0.64 – 0.85) | <0.001 | 0.70 (0.59 – 0.82) | <0.001 |
| Baseline value | 0.34 (0.27 – 0.44) | <0.001 | 0.28 (0.20 – 0.40) | <0.001 | |
| Model I | Model II | ||||
|---|---|---|---|---|---|
| Functional performance measures | Measurement | Standardized Hazard Ratio (95% Confidence Interval) | P value | Standardized Hazard Ratio (95% Confidence Interval) | P value |
| All-Cause Mortality (N=446) | |||||
| Six minute walk | Two-year change in performance. | 0.88 (0.81 – 0.97) | 0.007 | 0.89 (0.81 – 0.97) | 0.011 |
| Baseline value | 0.61 (0.49 – 0.76) | <0.001 | 0.69 (0.53 – 0.90) | 0.005 | |
| Four meter velocity, usual pace | Two-year change in performance. | 0.89 (0.80 – 0.99) | 0.026 | 0.93 (0.84 – 1.03) | 0.166 |
| Baseline value | 0.68 (0.54 – 0.86) | 0.001 | 0.86 (0.66 – 1.11) | 0.237 | |
| Four meter velocity, fast pace | Two-year change in performance. | 0.82 (0.74 – 0.91) | <0.001 | 0.85 (0.77 – 0.95) | 0.003 |
| Baseline value | 0.69 (0.55 – 0.87) | 0.001 | 0.84 (0.64 – 1.09) | 0.179 | |
| Short physical performance battery | Two-year change in performance. | 0.87 (0.79 – 0.97) | 0.011 | 0.88 (0.79 – 0.99) | 0.032 |
| Baseline value | 0.68 (0.55 – 0.85) | <0.001 | 0.80 (0.62 – 1.04) | 0.094 | |
| Model I | Model II | ||||
|---|---|---|---|---|---|
| Functional performance measures | Measurement | Standardized Hazard Ratio (95% Confidence Interval) | P value | Standardized Hazard Ratio (95% Confidence Interval) | P value |
| Cardiovascular Disease Mortality (N=446) | |||||
| Six minute walk | Two-year change in performance. | 0.86 (0.75 – 0.99) | 0.035 | 0.88 (0.75 – 1.02) | 0.096 |
| Baseline value | 0.58 (0.41 – 0.83) | 0.003 | 0.72 (0.45 – 1.14) | 0.161 | |
| Four meter velocity, usual pace | Two-year change in performance. | 0.83 (0.71 – 0.97) | 0.016 | 0.86 (0.72 – 1.02) | 0.090 |
| Baseline value | 0.69 (0.47 – 1.02) | 0.062 | 0.93 (0.60 – 1.43) | 0.738 | |
| Four meter velocity, fast pace | Two-year change in performance. | 0.73 (0.63 – 0.85) | 0.062 | 0.75 (0.63 – 0.90) | 0.001 |
| Baseline value | 0.70 (0.48 – 1.00) | 0.052 | 0.96 (0.60 – 1.54) | 0.875 | |
| Short physical performance battery | Two-year change in performance. | 0.81 (0.69 – 0.96) | 0.013 | 0.87 (0.72 – 1.05) | 0.144 |
| Baseline value | 0.71 (0.49 – 1.02) | 0.067 | 0.95 (0.60 – 1.49) | 0.809 | |
In analyses adjusting for age, sex, and race, and including both baseline performance measures and changes in performance measures, poorer baseline performance on each functional measurement and greater decline in performance in each functional measure were each associated significantly with higher all-cause mortality (Table 3, Model I). After additional adjustment for comorbidities, ABI, BMI, smoking, relevant medications, study cohort, and physical activity, poorer baseline six-minute walk performance (P=0.005) and greater decline in six-minute walk performance (P=0.011) were each associated independently with higher all-cause mortality (Table 3, Model II). In fully adjusted analyses, greater decline in the fast-paced four-meter walking velocity (P=0.003) and greater decline in the SPPB (P=0.032) between baseline and two-year follow-up were associated with increased all-cause mortality (Table 3, Model 2). In contrast, slower baseline walking velocity and lower baseline SPPB were not associated with higher mortality in fully adjusted analyses (Table 3, Model II).
In analyses adjusting for age, sex, and race and including both baseline performance measures and changes in performance measures, poorer baseline six-minute walk performance (P=0.003) was associated significantly with higher cardiovascular disease mortality (Table 3, Model I). In these analyses, greater decline in six-minute walk performance (P=0.035), usual-paced four-meter walking velocity (P=0.016), and the SPPB (P=0.013) were each associated significantly with higher cardiovascular disease mortality. In fully adjusted analyses, only greater decline in fast-paced four meter walking velocity (P=0.001) was associated with higher cardiovascular disease mortality (Table 3, Model II).
DISCUSSION
Results reported here demonstrate that decline in any one of four office-based functional performance measures over a two-year period is associated with an increased rate of subsequent mobility loss in participants with PAD, even after controlling for age, comorbidities, medications, ABI, physical activity, and other potential confounders. Greater decline in six-minute walk performance and fastest-paced four-meter walking velocity were also associated with increased all-cause mortality, compared to lesser declines in these functional performance measures. Finally, greater decline in six-minute walk performance was associated with higher cardiovascular mortality.
Functional performance measures, such as the six-minute walk test and walking velocity over four meters, are reliable, objective measures of lower extremity performance that can be administered in the office setting. They require a short amount of time and only a stopwatch to administer. Based on findings reported here, clinicians can potentially use serial, annual measures of functional performance over two years of follow-up to identify people with PAD who are at increased risk for mobility loss and mortality.
To our knowledge, no prior studies have assessed associations of change in functional performance with subsequent mobility loss or mortality in participants with PAD. We previously reported that poorer baseline six-minute walk performance, slower baseline usual and fastest paced four-meter walking velocity, and lower baseline SPPB scores were associated with higher rates of mobility loss among participants with PAD over 50-month follow-up (5). We also reported that poorer baseline six-minute walk performance and slower usual and fastest paced four-meter walking velocity were associated with higher mortality among participants with PAD (4). The current study demonstrates that for all functional performance measures evaluated, both poorer baseline functional performance and greater decline in functional performance are associated significantly and independently with increased rates of mobility loss, even after adjusting for potential confounders including comorbidities, the ABI, and physical activity. Similarly, both poorer baseline six-minute walk performance and greater decline in six-minute walk performance are associated with higher all-cause mortality in participants with PAD. However, our results suggest that declines in fast-paced walking velocity and the SPPB are more predictive of all-cause mortality than baseline measures of fast-paced walking velocity and the SPPB, respectively.
Decline in functional performance is likely to predict mobility loss and mortality if it is a more sensitive measure of deteriorating global health than measures such as comorbidities or the ABI. Declines in functional performance measures may be sensitive to progression of comorbid diseases and/or progression of systemic atherosclerosis, which in turn may influence risk of mobility loss and mortality. Further study is needed to determine whether preventing functional decline can protect against mobility loss and mortality among individuals with PAD.
In unadjusted analyses, men with PAD had higher rates of mobility loss than women with PAD (Table 1). However, we did not observe any interactions of gender on the associations of decline in functional performance with mobility loss or mortality (data not shown). Further study is needed to establish gender differences in functional decline among men and women with PAD. in analyses adjusting for both baseline fast-paced walking velocity and change in fast-paced walking velocity, only greater decline in fast-paced walking velocity, but not baseline fast-paced walking velocity, predicted higher all-cause mortality or cardiovascular disease mortality, respectively. Similarly, in analyses adjusting for both baseline SPPB and change in the SPPB, only change in the SPPB predicted higher all-cause mortality. Together, these
This study has limitations. First, data are observational. Associations of decline in functional performance with adverse outcomes should not be construed as causal. Second, a priori we selected functional performance over two-year follow-up as the independent variable of interest for these analyses. Our findings may not be generalizable to PAD participants without two years of functional performance measures. Third, based on our exclusion criteria, our findings are not generalizable to PAD participants who undergo lower extremity revascularization during the two-year measurement of change in functioning. Fourth, we used death certificates to ascertain cardiovascular death, which may be associated with some mis-classification as compared to adjudicated cause of death (22).
In conclusion, two-year declines in six-minute walk, usual and fast paced walking velocity, and the SPPB score predicted mortality and/or mobility loss in participants with PAD. Further study is needed to determine whether exercise and other interventions that prevent functional decline are protective against mobility loss and mortality in patients with PAD.
ABBREVIATIONS
- ABI
ankle brachial index
- BMI
body mass index
- CI
confidence interval
- CVD
cardiovascular disease
- HR
hazard ratio
- PAD
peripheral arterial disease
- SPPB
short physical performance battery
- WALCS
Walking and Leg Circulation Study
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Ankle Brachial Index Collaboration. Fowkes FG, Murray GD, et al. Ankle brachial index combined with Framingham Risk Score to predict cardiovascular events and mortality: a meta-analysis. JAMA. 2008;300:197–208. doi: 10.1001/jama.300.2.197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.McDermott MM, Greenland P, Liu K, et al. Leg symptoms in peripheral arterial disease: associated clinical characteristics and functional impairment. JAMA. 2001;286:1599–1606. doi: 10.1001/jama.286.13.1599. [DOI] [PubMed] [Google Scholar]
- 3.McDermott MM, Liu K, Greenland P, et al. Functional decline in peripheral arterial disease: associations with the ankle brachial index and leg symptoms. JAMA. 2004;292:453–61. doi: 10.1001/jama.292.4.453. [DOI] [PubMed] [Google Scholar]
- 4.McDermott MM, Tian L, Liu K, et al. Prognostic value of functional performance for mortality in patients with peripheral artery disease. J Am Coll Cardiol. 2008;51:1482–1489. doi: 10.1016/j.jacc.2007.12.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.McDermott MM, Guralnik JM, Tian L, et al. Baseline functional performance predicts the rate of mobility loss in persons with peripheral arterial disease. J Am Coll Cardiol. 2007;50:974–982. doi: 10.1016/j.jacc.2007.05.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.McDermott MM, Hoff F, Ferrucci L, et al. Lower extremity ischemia, calf skeletal muscle characteristics, and functional impairment in peripheral arterial disease. J Am Geriatr Soc. 2007;55:400–6. doi: 10.1111/j.1532-5415.2007.01092.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.McDermott MM, Greenland P, Liu K, et al. The ankle brachial index as a measure of leg functioning and physical activity in peripheral arterial disease: the walking and leg circulation study. Ann Intern Med. 2002;136:873–83. doi: 10.7326/0003-4819-136-12-200206180-00008. [DOI] [PubMed] [Google Scholar]
- 8.McDermott MM, Criqui MH, Liu K, et al. The lower ankle brachial index calculated by averaging the dorsalis pedis and posterior tibial arterial pressures is most closely associated with leg functioning in peripheral arterial disease. J Vasc Surg. 2000;32:1164–1171. doi: 10.1067/mva.2000.108640. [DOI] [PubMed] [Google Scholar]
- 9.Shadman R, Criqui MH, Bundens WP, et al. Subclavian artery stenosis: prevalence, risk factors, and association with cardiovascular diseases. J Am Coll Cardiol. 2004;44:618–23. doi: 10.1016/j.jacc.2004.04.044. [DOI] [PubMed] [Google Scholar]
- 10.Montgomery PS, Gardner AW. The clinical utility of a six-minute walk test in peripheral arterial occlusive disease patients. J Am Geriatr Soc. 1998;46:706–711. doi: 10.1111/j.1532-5415.1998.tb03804.x. [DOI] [PubMed] [Google Scholar]
- 11.McDermott MM, Ades PA, Dyer A, et al. Corridor-based functional performance measures correlate better with physical activity during daily life than treadmill measures in persons with peripheral arterial disease. J Vasc Surg. 2008;48:1231–7. doi: 10.1016/j.jvs.2008.06.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.McDermott MM, Ades P, Guralnik JM, et al. Treadmill exercise and resistance training in patients with peripheral arterial disease with and without intermittent claudication: a randomized controlled trial. JAMA. 2009 Jan 14;301(2):165–74. doi: 10.1001/jama.2008.962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Guralnik JM, Ferrucci L, Simonsick E, Salive ME, Wallace RB. Lower extremity function in persons over 70 years as a predictor of subsequent disability. N Engl J Med. 1995;332:556–561. doi: 10.1056/NEJM199503023320902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Guralnik JM, Simonsick EM, Ferrucci L, et al. A short physical performance battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol. 1994;49:M85–M94. doi: 10.1093/geronj/49.2.m85. [DOI] [PubMed] [Google Scholar]
- 15.Patel KV, Coppin AK, Manini TM, et al. Midlife physical activity and mobility in older age. The InCHIANTI study. Am J Prev Med. 2006;31:217–224. doi: 10.1016/j.amepre.2006.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Fried LP, Guralnik JM. Disability in older adults: evidence regarding significance, etiology, and risk. J Am Geriatr Soc. 1997;45:92–100. doi: 10.1111/j.1532-5415.1997.tb00986.x. [DOI] [PubMed] [Google Scholar]
- 17.Guralnik JM, Fried LP, Simonsick EM, Kasper JD, Lafferty ME, editors. The Women's Health and Aging Study: health and social characteristics of older women with disability. National Institute on Aging; Bethesda, MD: 1995. NIH publication 95-4009, Appendix E. [Google Scholar]
- 18.Altman R, Alarcon G, Appelrouth D, et al. The American College of Rheumatology criteria for the classification and reporting of osteoarthritis of the hip. Arthritis Rheum. 1991;34:505–514. doi: 10.1002/art.1780340502. [DOI] [PubMed] [Google Scholar]
- 19.Altman R, Asch E, Bloch D, et al. Development of criteria for the classification and reporting of osteoarthritis. Arthritis Rheum. 1986;29:1039–1049. doi: 10.1002/art.1780290816. [DOI] [PubMed] [Google Scholar]
- 20.Garg PK, Tian L, Criqui MH, et al. Physical activity during daily life and mortality in patients with peripheral arterial disease. Circulation. 2006;114:242–8. doi: 10.1161/CIRCULATIONAHA.105.605246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lin DY, Wei LJ, Ying Z. Checking the Cox model with cumulative sums of martingale-based residuals. Biometrika. 1993;80:557–572. [Google Scholar]
- 22.Coady SA, Sorlie PD, Cooper LS, et al. Validation of death certificate diagnosis for coronary heart disease: the Atherosclerosis Risk in Communities (ARIC) Study. J Clin Epidemiol. 2001;54:40–50. doi: 10.1016/s0895-4356(00)00272-9. [DOI] [PubMed] [Google Scholar]