Abstract
Despite the clinical importance of readiness to change in predicting treatment outcomes among adults, no studies have examined this construct among pediatric pain patients. Because parents play a key role in adolescent pain management, both adolescent and parent readiness to adopt a self-management approach to pain merit further study. The primary goal of the current study was to validate adolescent and parent-report adaptations of the adult Pain Stages of Change Questionnaire (PSOCQ). Participants included 259 adolescent patients with chronic pain syndromes and their parents presenting to two pediatric pain management clinics. Using confirmatory factor analytic techniques, a four-factor solution was supported for the parent (PSOCQ-P) version that included Precontemplation, Contemplation, Action and Maintenance factors, while the adolescent (PSOCQ-A) version supported a three-factor model that combines the Action and Maintenance scales. Within both versions, each of the factors was found to be internally consistent. The PSOCQ-A and PSOCQ-P showed evidence of criterion validity through significant correlations with coping strategies and pain catastrophizing. Stability findings at four and eight weeks following a multidisciplinary pain clinic evaluation are reported. Associations between pediatric PSOCQ scores and demographic, pain and functional domains were explored to inform future research. Further validation of the PSOCQ-A and PSOCQ-P measures with new, separate samples of pediatric pain patients and parents are needed before use in clinical contexts.
Keywords: PSOCQ-A, PSOCQ-P, assessment, child, pain management
Interdisciplinary treatment programs for children and adolescents with chronic pain are growing in number, with promising results of reduced pain and disability [9; 26; 28]. As this treatment model has proliferated, there is increased emphasis on understanding predictors of successful treatment outcomes. Individuals' level of motivation, or readiness to change, has emerged in adult pain research as a potentially important factor for successful pain self-management [16]. The readiness to change concept aligns with the transtheoretical model (TTM) of behavioral change [31]. Four TTM-based “stages of change” have been conceptualized and measured for chronic pain: Precontemplation (little perceived personal responsibility for pain control, no interest in implementing behavioral changes), Contemplation (awareness of personal responsibility for pain control, considering behavioral change), Action (active involvement in learning self-management strategies), and Maintenance (sense of personal responsibility for pain control and routine application of self-management strategies) [21; 23].
The Pain Stages of Change Questionnaire (PSOCQ) [23], a well-known tool measuring adult readiness to adopt a self-management approach to pain, integrates the TTM framework with cognitive-behavioral pain management theory. Measure development studies yielded four factors representing the TTM-based pain stages of change with good internal consistency, temporal stability, and discriminant and criterion-related validity [23; 35]. Subsequent studies have further investigated the PSOCQ's psychometric properties [3; 12; 17; 22] and explored its utility cross-culturally [8; 27; 38] and in a community setting [14]. Although some variability exists for PSOCQ subscales across studies, there is general support that the measure is a useful tool.
Despite the clinical importance of readiness to change in predicting adult treatment outcomes [19; 22], no studies have examined this construct among pediatric pain patients. With a significant portion of pediatric patients with chronic pain demonstrating nonadherence to pain management recommendations [34], examining factors contributing to this struggle is essential. Because parents play a key role in pediatric pain management, it is also important to consider parental readiness to change, i.e., the extent to which parents perceive themselves ready to endorse the self-management philosophy.
The goal of the current study is to validate adolescent and parent-report adaptations of the PSOCQ. In the context of pediatric pain, the readiness to change construct refers to degree of willingness to adopt and maintain a self-management approach to pain. Specific hypotheses include: (1) the four-factor structure of the original PSOCQ (i.e. precontemplation, contemplation, action, maintenance) will be replicated using the adolescent (PSOCQ-A) and parent (PSOCQ-P) adaptations; (2) PSOCQ-A and PSOCQ-P will each demonstrate internal consistency, and (3) PSOCQ-A and PSOCQ-P will show evidence of criterion-related validity through significant correlations with coping strategies (i.e, positive correlations for action/maintenance with accommodative coping and between precontemplation and passive coping) and pain catastrophizing (i.e, lower action/maintenance scores and higher precontemplation scores will associate with more catastrophizing). In addition, we will explore associations between PSOCQ-P and PSOCQ-A scores and demographic (age, gender, SES), pain-related (location, duration, intensity), and physical functioning variables to inform future studies. Lastly, we examine stability of PSOCQ-A and PSOCQ-P scores four and eight weeks following multidisciplinary pain clinic evaluation.
Method
Participants
Participants were 259 patients and their parents presenting for initial (Time 1 – “T1”) evaluation to two large pediatric institutions (Children's Hospital Boston (CHB) and The Children's Hospital of Philadelphia (CHOP) that provide specialized tertiary care for the management of chronic pain between September 2007 and December 2009. Patients were ineligible for participation if they had significant impairments or developmental delays that affected their ability to respond to self-report measures. Inclusion criteria for the current study included: 1) primary presenting complaint of ongoing pain, 2) identified patient ages 12–18 years, and 3) patient and parent ability to read and comprehend questionnaires written in English. Patients were referred from a variety of medical subspecialties (e.g., orthopedics, rheumatology, neurology) and primary care pediatricians, usually after other treatment attempts failed to substantially reduce symptoms or if pain was more severe than expected given the medical condition. Institutional Review Board (IRB) approval was obtained at both institutions for data collected at each site and to combine de-identified data across sites.
Sample 1 (CHB site)
Sample 1 consisted of 162 patient-parent dyads participating in a larger ongoing IRB approved study examining attitudes toward pain. Self-report measures were collected at two time points: 1) the patient's initial multidisciplinary clinic evaluation (Time 1 – “T1”), and 2) 4-weeks after the initial evaluation via mailed questionnaires. As follow-up data collection of the PSOCQ was initiated after the onset of the study, 130 of the 162 participant families were asked to complete the PSOCQ at follow-up. Among those invited, 97 completed 4-week follow up measures, resulting in a 75% response rate. Additional demographic characteristics for Sample 1 are presented in Table 1.
Table 1.
Demographic Characteristics for Samples 1, 2 and Combined
| Sample 1 (n=162) | Sample 2 (n=97) | Combined (N=259) | |
|---|---|---|---|
| Adolescent sex: Females (%) | 76.5 | 79.4 | 77.6 |
|
| |||
| Race: Caucasian (%) | 94.4 | 89.7 | 92.7 |
|
| |||
| Age (Mean, SD) | 14.74 (1.67) | 15.71 (1.41) | 15.10 (1.64) |
|
| |||
| Pain duration in months (Mean, SD) | 24.36 (27.28) | 21.76 (19.96) | 23.43 (24.88) |
|
| |||
| Parent reporter: Mothers (%) | 88.9 | 90.7 | 89.6 |
|
| |||
| Mother education* | 5.73 (1.09) | 5.60 (1.03) | 5.68 (1.07) |
|
| |||
| Father education* | 5.64 (1.19) | 5.62 (1.13) | 5.63 (1.17) |
|
| |||
| Family SES* (Mean, SD) | 52.23 (8.98) | 49.75 (10.77) | 51.25 (9.77) |
|
| |||
| Primary pain location (%) | |||
| Limb | 38.3 | 44.3 | 40.5 |
| Diffuse musculoskeletal pain | 10.5 | 36.1 | 20.1 |
| Flank | 0.6 | 3.1 | 1.5 |
| Back/neck | 19.8 | 11.3 | 16.6 |
| Abdomen | 11.7 | 2.1 | 8.1 |
| Pelvic area(male or female) | 10.5 | 0 | 6.6 |
| Head | 3.7 | 1.0 | 2.7 |
| Chest | 3.7 | 2.1 | 3.1 |
Parent education and Family socioeconomic status (SES) coding is based on the four-factor index of social status [15]. Parent education scores ranged from 1 (“less than 7th grade”) to 7 (“graduate professional training-graduate degree”). All mean education values fell within the 5= “partial college (at least one year) or specialized training” category, between categories 4 = “High school graduate” and 6 = “Standard college or university graduate”. SES scores ranged from 26 (“machine operators, semiskilled workers”) to 66 (“major business, professional”). All mean SES values fell within the “medium business owner, minor professional, technical” category of social strata.
Sample 2 (CHOP site)
Sample 2 consisted of 97 patient-parent dyads. All participants were enrolled in an IRB approved research project that collected self-report measures at two time points: 1) the patient's initial multidisciplinary clinic evaluation (Time 1 – “T1”), and 2) 8-weeks after the initial evaluation via telephone follow up calls. A total of 92 patient-parent dyads completed the 8 week follow-up measures. See Table 1 for additional demographic characteristics for Sample 2.
Combined Sample
The total sample included 259 patients from both sites and was primarily female (77.6%) and Caucasian (92.7%; 1.9% Hispanic, 2.7% Black, 1.9% Asian, 0.4% American Indian, 0.4% other), reflective of the population of adolescents seen in these tertiary care clinic settings. The mean age was 15.12 years (SD = 1.66). Refer to Table 1 for additional demographic characteristics for the Combined Sample.
Measures
Demographic and Pain-Relevant Descriptive Information
Parents completed a demographic information form including the adolescents' age, sex, race and ethnicity, family SES [15], as well as information regarding the onset and duration of pain. The location of the primary pain problem was collected from the patient's chart.
Concurrent validity measures
Pain Intensity
At T1, patients in Sample 1 stated their most, usual and least pain intensity levels using a verbally reported numeric rating scale (NRS)[40] ranging from 0=”no pain” to 10=”worst pain imaginable”. Sample 2 utilized a written 10 cm visual analog scale (VAS)[29] ranging from 0=”no pain” to 10=”unbearable pain” to report their most, usual and least intensity for the presenting pain problem at T1. Both samples also assessed the adolescent's verbal report of the current pain intensity on the day of the initial evaluation using a verbal NRS report, anchored at 0=”no pain” and 10=”worst pain you can imagine”.
Functional Disability Inventory (FDI)
Patient self-reports were collected at T1 for both samples using the FDI [6; 20; 42] which assesses children's self-reported difficulty in physical and psychosocial functioning due to their physical health. The instrument consists of 15 items concerning perceptions of activity limitations during the past two weeks that are rated 0=”no trouble”, 1=”a little trouble”, 2=”some trouble”, 3=”a lot of trouble”, and 4=”impossible”. A total summary score was used in analyses (range 0–60). The FDI has demonstrated reliability and validity in adolescents ages 8–18[6; 20; 42]. Alpha reliability for the combined sample was .89.
Criterion-related validity measures
The Pain Catastrophizing Scale for Children (PCS-C) and for Parents (PCS-P)
For both samples, patients and parents provided reports regarding beliefs about the patient's pain at T1. The PCS-C [7] and PCS-P [7; 13] are reliable and validated 13 item parallel measures that assess threatening beliefs about actual or anticipated painful experiences on a 5-point scale (both rated 0=”not at all”, 1=”mildly”, 2=”moderately”, 3=”severely”, and 4=”extremely”). A total score, which reflects tendencies to ruminate, magnify and/or feel helpless about pain, was examined. Higher scores reflect greater pain catastrophizing. Alpha reliabilities for pain catastrophizing total scores in the combined sample were .91 for PCS-C and .91 for PCS-P.
The Pain Response Inventory (PRI)
Patients in Sample 1 provided pain coping reports at T1 using the reliable and validated PRI [43]. A total of 60 items are rated on a 5-point scale (0=”never”, 1=”once in a while”, 2=”sometimes”, 3=”often”, and 4=”always”) with higher scores indicating greater use of that coping style. The PRI generates 3 primary pain coping styles: passive, active, and accommodative. Passive coping approaches include self-isolation, activity restriction, and catastrophizing. These strategies indicate a coping style that assumes little self-control over pain. Accommodative coping approaches, including acceptance, self-encouragement, and distraction, are most in line with the self-management approach to pain and have been linked with the most positive outcomes [41]. Thus, passive coping scores were used to represent a non-adaptive approach to coping with pain that suggests little readiness to change, and accommodative coping scores were used to represent an adaptive coping style consistent with greater readiness to change. The active coping subscale (which includes divergent strategies including rest, massaging/guarding, and social support seeking) was not used in analyses, given inconsistent patterns of associations found with this PRI subscale in previous studies[33]. Alpha reliabilities for the scales for the combined sample were .91 for Passive Coping and .90 for Accommodative Coping.
Core measures to be validated
The Pain Stages of Change Questionnaire for Adolescents (PSOCQ-A) and Parents (PSOCQ-P)
The 30-item adult Pain Stages of Change Questionnaire [21; 23] was modified to assess patient self-reports of readiness to adopt a self-management approach to chronic pain and parent reports of their own mindset regarding motivation to change with respect to their adolescent's current behavior. Multiple revisions were pursued based on input from 3 pediatric psychologists with expertise in pain management (LM, DL, JG) and were piloted with patients to examine acceptability and utility of the measures. Items included in the PSOCQ-A were adapted from the original adult measure to primarily include more developmentally appropriate and understandable terminology, while the PSOCQ-P items were specifically adapted to reflect the parent's motivation and readiness to change his/her own mindset and behaviors based on perceptions of their adolescent's current behavior. Instructions for completing the measure and individual items appear in Table 7. The resulting readability [32] for the adapted adolescent measure was at a 6th grade level (Flesch-Kincaid grade level = 6.3; Flesch-Kincaid reading ease = 79.4) and at a 7th grade level for the adapted parent measure (Flesch-Kincaid grade level = 7.1; Flesch-Kincaid reading ease = 73.1). The PSOCQ-A 6th grade readability level roughly corresponds to the age of ≥ 12 years. This age was considered to be a developmentally appropriate lower end for the concepts being assessed with respect to the literature focusing on the development of children's concepts of pain and illness [2; 10–11] which suggests that approximately 11 years of age is when an appreciation of “psychophysiologic” factors begins to emerge as relevant to children's understanding of the pain experience.
Table 7.
PSOCQ-A and PSOCQ-P instructions and item text.
| Adolescent Measure | Parent Measure | |
|---|---|---|
| Instructions: This questionnaire is to help us understand the way you look at your pain. Each statement describes how you may feel about this problem. Please decide how much you agree or disagree with each statement. In each example, make sure your choice is based on how you feel right now, not how you have felt in the past or how you would like to feel. Circle the response that best described how much you agree or disagree RIGHT NOW with each statement. | Instructions: This questionnaire is to help us better understand the way you view your child's pain problem. Each statement describes how you may feel about this particular problem. Please indicate the extent to which you tend to agree or disagree with each statement. In each example, please make sure your choice is based on how you feel right now, not how you have felt in the past or how you would like to feel. Circle the response that best described how much you agree or disagree with each statement. | |
| Item | Item Text | Item Text |
| Precontemplation | ||
| 11 | I have tried everything that people have recommended to manage my pain and nothing helps. | We have tried everything that people have recommended to manage his/her pain and nothing helps. |
| 12 | My pain is a medical problem and I should be dealing with medical doctors about it. | My child's pain is a medical problem and s/he should be dealing with physicians about it. |
| 16 | Everybody I speak with tells me that I have to learn to live with my pain, but I don't see why I should have to. | Everybody I speak with tells me that my child has to learn to live with his/her pain, but I don't see why s/he should have to. |
| 22 | I still think despite what doctors tell me, there must be some surgery or medicine that would get rid of my pain. | I still think that despite what doctors tell us, there must be some surgical procedure or medication that would get rid of the pain. |
| 24 | The best thing I can do is find a doctor who can figure out how to get rid of my pain once and for all. | The best thing I can do is find a doctor who can figure out how to get rid of my child's pain once and for all. |
| 25 | Why can't someone just do something to take away my pain? | Why can't someone just do something to take away my child's pain? |
| 29 | All of this talk about how to cope better is a waste of my time. | All of this talk about how to cope better is a waste of our time. |
| Contemplation | ||
| 1 | I have been thinking that the way I cope with my pain could get better. | I have been thinking that the way my child copes with pain could improve. |
| 7 | I have recently realized that there is no medical cure for my pain condition, so I want to learn some ways to cope with it. | I have recently realized that there is no medical cure for my child's pain condition, so I would like him/her to learn some ways to cope with it. |
| 8 | Even if my pain doesn't go away, I am ready to start changing how I deal with it. | Even if my child's pain doesn't go away, I am ready to help him/her to start changing how s/he deals with it. |
| 9 | I realize now that it's time for me to come up with a better plan to cope with my pain problem. | I realize now that it's time to come up with a better plan to cope with my child's pain problem. |
| 14 | I am beginning to wonder if I need to get some help to develop skills for dealing with my pain. | I am beginning to wonder if my child needs to get some help to develop skills for dealing with his/her pain. |
| 15 | I have recently figured out that it's up to me to deal better with my pain. | I have recently figured out that it's up to my child to deal better with his/her pain. |
| 19 | I have recently come to the conclusion that it's time for me to change how I cope with my pain. | I have recently come to the conclusion that it's time for my child to change how s/he copes with his/her pain. |
| 21 | I'm starting to wonder whether it's up to me to manage my pain rather than relying on doctors. | I am starting to wonder whether it's up to my child to manage his/her pain rather than relying on physicians. |
| 23 | I have been thinking that doctors can only help so much in managing my pain and that the rest is up to me. | I have been thinking that doctors can only help so much in managing my child's pain and that the rest is up to my child. |
| 28 | I have been wondering if there is something I could do to manage my pain better. | I have been wondering if there is something my child could do to manage his/her pain better. |
| Action | ||
| 2 | I am developing new ways to cope with my pain. | I am encouraging my child to develop new ways to cope with his/her pain. |
| 6 | I have started to come up with strategies to help myself control my pain. | I am encouraging my child to come up with strategies to help him/her control pain. |
| 20 | I'm getting help learning some strategies for coping better with my pain. | I am encouraging my child to get help with learning some strategies for coping better with his/her pain. |
| 26 | I am learning to help myself control my pain without doctors. | I am encouraging my child to learn to help him/herself control his/her pain without doctors. |
| 27 | I am testing out some coping skills to manage my pain better. | I am encouraging my child to test out some coping skills to manage his/her pain better. |
| 30 | I am learning ways to control my pain other than with medicines or surgery. | I am encouraging my child to learn ways to control his/her pain other than with medications or surgery. |
| Maintenance | ||
| 3 | I have learned some good ways to keep my pain problem from getting in the way of my life. | My child has learned some good ways to keep his/her pain problem from interfering with life. |
| 4 | When my pain flares up, I find myself using coping strategies that have worked in the past, such as a relaxation exercise or distractions. | When my child's pain flares up, s/he is automatically using coping strategies that have worked in the past, such as a relaxation exercise or a mental distraction technique. |
| 5 | I am using some strategies that help me better deal with my pain on a day-to-day basis. | My child is using some strategies that help him/her better deal with his/her pain problem on a day-to-day basis. |
| 10 | I use what I have learned to help keep my pain under control. | My child uses what s/he has learned to help keep his/her pain under control. |
| 13 | I am currently using some suggestions people have made about how to live with my pain. | My child is currently using some suggestions people have made about how to live with his/her pain problem. |
| 17 | I have built strategies for dealing with my pain into my everyday life. | My child has incorporated strategies for dealing with pain into his/her everyday life. |
| 18 | I have made a lot of progress in coping with my pain. | My child has made a lot of progress in coping with his/her pain. |
The final 30 item parallel PSOCQ-A and –P measures assess readiness to adopt a self-management approach to pain coping, with individual items rated on a 5-point scale rated 1=”Strongly Disagree”, 2=”Disagree”, 3=”Undecided or Unsure”, 4=”Agree”, 5=”Strongly Agree” (refer to Table 7 for item text). Initial scoring of the PSOCQ-A and PSOCQ-P followed the criteria for the 4 adult subscale scores: Precontemplation, Contemplation, Action, and Maintenance. In addition, patients are categorized as being in one stage of change based on the highest subscale score value. When two subscale score values are equal, the patient is categorized into the stage of change representing more progression towards self-management (e.g., if Precontemplation and Contemplation subscale scores are equal, the patient is categorized into the contemplation stage). This is consistent with previous research (Jensen et al. 2000). Both samples provided patient and parent data at T1. Follow-up reports were completed for Sample 1 at 4 weeks and for Sample 2 at 8 weeks after the initial T1 evaluation.
Procedures
Institutional Review Board approval was obtained at both locations for the study and to share de-identified data between the two sites and close communication occurred between sites to ensure compatibility of the pooled data. The PSOCQ and additional measures were administered at the time of the initial evaluation for specialized pain management services. Administration of questionnaires occurred by mail in advance of the visit or in person during the initial evaluation. Families self-selected the parent to report on the measures. Across sites, patients received a multidisciplinary evaluation by a treatment team including a clinical psychologist and pain specialist physician at both sites as well as a physical therapist at the Children's Hospital Boston site. Follow up data were collected from participants via mailed surveys at 4 weeks (Sample 1) and via telephone at 8 weeks (Sample 2).
Data Analytic Plan
Descriptive Statistics
Descriptive statistics were used to characterize the population and compare the demographic and diagnostic information from the two sites to ensure similarity in the two samples.
Factor Analysis
Confirmatory factor analysis (CFA) was conducted on the combined T1 data using SEM via the Mplus software [30] to test the four-factor solution reported by Kerns et al [23] for the original PSOCQ. Based on recommendations by Bentler and Bonett [1], the following statistics were used to evaluate model fit: chi square, Comparative Fit Index (CFI; >.90 acceptable, >.95 excellent), and Root Mean Square Error of Approximation (RMSEA; <.08 acceptable, <.05 excellent). Fit of nested models were tested by comparing the difference in chi-square values between the two models to a chi-square statistic with degrees of freedom equal to the difference in degrees of freedom between the two models. A significant difference indicates that the more complex model better fits the data [37]. In order to further assess the appropriateness of the current model, the proposed 4-Factor solutions were compared to alternative models including 3-Factor solutions and model respecifications based on modification indices [36] related to within factor correlations between items.
Scale Reliability and Stability
Following assessment of the factor structure we tested the reliability of the PSOCQ-A and PSOCQ-P measures by computing inter-item correlation coefficients. We also examined measure stability at 4- and 8-weeks after initial assessment (for Sample 1 and Sample 2, respectively).
Validity analyses
Validity of the adolescent and parent measures was examined through correlations with adolescent-reported pain coping strategies (measured by the PRI) and pain catastrophizing (measured by the PCS-C and PCS-P, respectively). Consistent with a conceptual framework and process employed by Kerns and colleagues in the initial validation of the PSOCQ[23], it was hypothesized that Action/Maintenance scores would be positively associated with accommodative coping scores and negatively correlated with pain catastrophizing, while Precontemplation scores would be significantly positively correlated with measures of passive coping and pain catastrophizing.
Exploratory analyses
Exploratory analyses were performed to test for associations between PSOCQ-A and PSOCQ-P subscales and demographics, pain scores, pain location, and functional disability. Chi-square tests were used to compare categorical variables to stage of change. Pearson correlation coefficients were used to assess the association between continuous measures and continuous subscale scores.
Results
Descriptive statistics
Across the two site samples, no differences were detected for sex, pain duration, SES, and race. Participants in Sample 1 (M=13.74 years, SD=1.67) were somewhat younger than Sample 2 (M=15.71 years, SD=1.41) t= 4.78, p < 0.001) and there was a significant difference in the proportion of patients reporting specific primary pain locations between the samples. More patients in Sample 1 reported abdominal pain (Pearson Chi-square = 7.61, p < 0.01) and pelvic pain (Pearson Chi-square = 10.89, p < 0.001), while more patients in Sample 2 reported diffuse pain (Pearson Chi-square = 24.76, p < 0.001). See Table 1. With no contraindication to combine site participants, all subsequent analyses were conducted with the combined sample.
Table 2 presents the Combined Sample means and standard deviations for validity measures. Table 3 presents the Combined Sample means, standard deviations, and internal consistencies for the final PSOCQ-A and PSOCQ-P subscales at T1 as well as the 4-week and 8-week samples.
Table 2.
Validity Measure Means and SDs for Time 1, 4-week and 8-week follow-up data
| Mean (SD) Time 1 (Combined Sample) | |
|---|---|
| Pain Intensity | |
| Most | 8.82 (1.58) |
| Least | 3.18 (2.48) |
| Usual | 6.06 (2.08) |
| Current | 5.35 (2.82) |
|
| |
| Pain Catastrophizing Scale for Children (PCS-C) | 27.97 (10.86) |
|
| |
| Pain Catastrophizing Scale for Parents (PCS-P) | 26.85 (10.39) |
|
| |
| Pain Coping (PRI) (n=144) | |
| Passive Coping | 1.15 (.78) |
| Active Coping | 1.66 (.61) |
| Accomodative Coping | 1.83 (.74) |
|
| |
| Functional Disability (FDI) | 24.53 (11.62) |
Table 3.
Pain Stages of Change Questionnaire for Adolescents (PSOCQ-A) and for Parents (PSOCQ-P) Means and SDs for Time 1, 4-week and 8-week follow-up data
| PSOCQ Subscales | Time 1 (Combined Sample, N=259) | 4-weeks (Sample 1, n=97) | 8-weeks (Sample 2, n=92) |
|---|---|---|---|
| Mean (SD), α | Mean (SD), α | Mean (SD), α | |
| Pain Stages of Change Questionnaire for Adolescents (PSOCQ-A) | |||
|
| |||
| Precontemplation | 3.58 (.85), .71 | 3.29 (1.02), .82 | 3.14 (.83), .69 |
| Contemplation | 3.36 (.68), .85 | 3.23 (.68), .85 | 3.52 (.60), .82 |
| Action/Maintenance | 3.22 (.72), .91 | 3.42 (.82), .93 | 3.77 (.58), .90 |
|
| |||
| Pain Stages of Change Questionnaire for Parents (PSOCQ-P) | |||
|
| |||
| Precontemplation | 3.08 (.72), .72 | 2.97 (.77), .71 | 2.74 (.63), .67 |
| Contemplation | 3.49 (.65), .84 | 3.35 (.64), .84 | 3.44 (.51), .75 |
| Action | 3.69 (.61), .79 | 3.82 (.58), .79 | 3.80 (.52), .74 |
| Maintenance | 3.24 (.70), .83 | 3.62 (.65), .85 | 3.78 (.51), .79 |
Factor Analysis
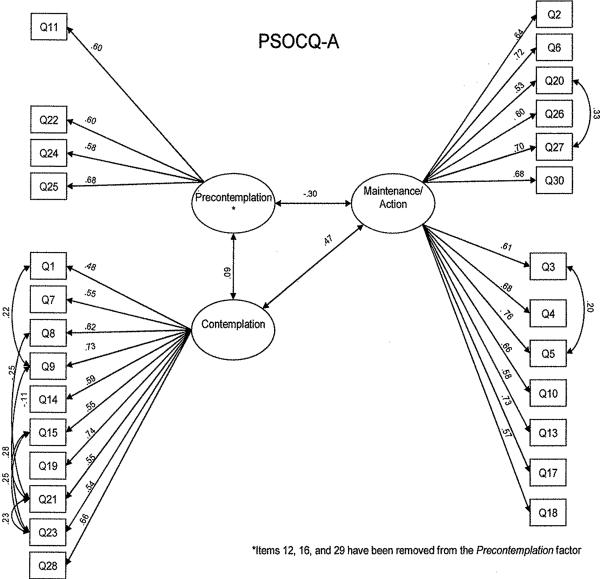
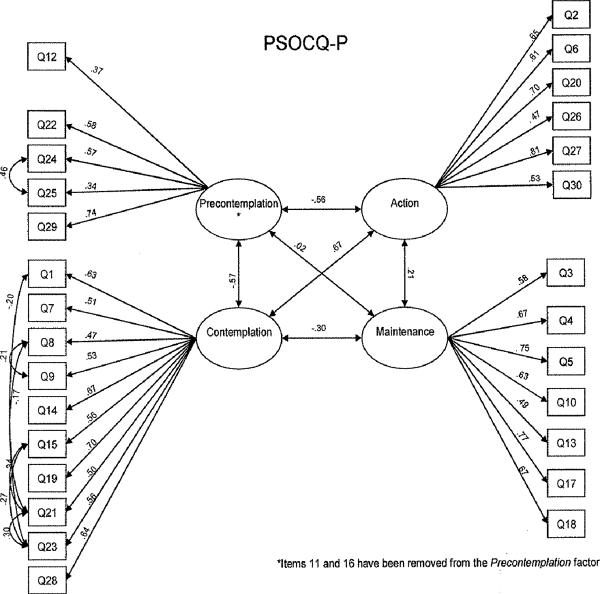
The results of all factor analyses run are summarized in Tables 4a (PSOCQ-A) and 4b (PSOCQ-P). In keeping with the Kerns et al. original factor structure, the following 4-factors were specified in the initial models: Precontemplation (7 items), Contemplation (10 items), Action (6 items) and Maintenance (7 items). See Figures 1 (PSOCQ-A) and 2 (PSOCQ-P) for final factor models, showing item assignment and coefficients.
Table 4a.
Confirmatory factor analysis model fit index comparison for the Pain Stages of Change Questionnaire for Adolescents (PSOCQ-A; N=258) at Time 1
| Model Tested | χ2 (d.f.) significance | CFI | TLI | RMSEA | AIC |
|---|---|---|---|---|---|
| Fit index guidelines | lower χ2 value is better | higher value is better | 1.0 is best | <0.08 is acceptable fit | lower value is better |
| 4-Factor Model (Unmodified) | |||||
| PSOCQ-A | 961.885 (399) p<0.0001 | 0.805 | 0.787 | 0.074 | 20618.898 |
| PSOCQ-A With Q12,Q16,Q29 removed | 784.584 (318) p<0.0001 | 0.828 | 0.810 | 0.075 | 18,364.041 |
| 3-Factor Model (Unmodified) | |||||
| PSOCQ-A | 973.086 (402) p<0.0001 | 0.802 | 0.786 | 0.074 | 20624.099 |
| 4-Factor Model (Modified) | |||||
| PSOCQ-A* | 866.401 (392) p<0.0001 | 0.836 | 0.818 | 0.068 | 20537.414 |
| 3-Factor Model (Modified) | |||||
| PSOCQ-A | 868.281 (394) p<0.0001 | 0.836 | 0.819 | 0.068 | 20535.294 |
| PSOCQ-A With Q12,Q16,Q29 removed | 690.757 (313) p<0.0001 | 0.861 | 0.844 | 0.068 | 18,280.214 |
Notes: Final model is shown in bold. Modified models allow for correlation between items within the same subscale, while unmodified do not.
Factor correlation of >1 found between Maintenance and Action scale, therefore this model was deemed unacceptable.
Table 4b.
Confirmatory factor analysis model fit index comparison for the Pain Stages of Change Questionnaire for Parents (PSOCQ-P; N=259) at Time 1
| Model Tested | χ2 (d.f.) significance | CFI | TLI | RMSEA | AIC |
|---|---|---|---|---|---|
| Fit index guidelines | lower χ2 value is better | higher value is better | 1.0 is best | <0.08 is acceptable fit | lower value is better |
| 4-Factor Model (Unmodified) | |||||
| PSOCQ-P | 941.096 (399) p<0.0001 | 0.789 | 0.770 | 0.072 | 19756.958 |
| 3-Factor Model (Unmodified) | |||||
| PSOCQ-P | 1514.495 (402) p<0.0001 | 0.566 | 0.531 | 0.103 | 20324.358 |
| 4-Factor Model (Modified) | |||||
| PSOCQ-P | 801.580 (391) p<0.0001 | 0.840 | 0.822 | 0.064 | 19633.443 |
| PSOCQ-P With Q11 and Q16 removed | 692.898 (337) p<0.0001 | 0.855 | 0.838 | 0.064 | 18,049.294 |
Notes: Final model is shown in bold. Modified models allow for correlation between items within the same subscale, while unmodified do not.
Figure 1.
Confirmatory factor analysis for PSOCQ-A, 3-factor modified model
Figure 2.
Confirmatory factor analysis of PSOCQ-P, 4-factor modified model
The first model tested was the 4-factor adolescent report version (PSOCQ-A) assessed at T1, which generated an RMSEA value (0.074) indicating an adequate fit to the data, but other fit indices suggested poorer fit (CFI = 0.805; χ2(399) = 961.885, p < .0001). Factor correlations for the PSOCQ-A were as follows: Contemplation with Precontemplation: 0.048 (p=0.552), Action with Precontemplation: −0.308 (p<0.001), Action with Contemplation: 0.547 (p<0.001), Maintenance with Precontemplation: −0.317 (p<0.001), Maintenance with Contemplation: 0.418 (p<0.001), Maintenance with Action: 0.997 (p<0.001).
A similar pattern of findings occurred for the 4-factor parent report version (PSOCQ-P) fit indices assessed at T1. Specifically, results showed that the RMSEA value (0.072) indicated an adequate fit of the model to the data, yet the CFI = 0.789 and χ2(399) = 941.096 (p < .0001) both suggested poorer model fit. Factor correlations for the PSOCQ-P sample were as follows: Contemplation with Precontemplation: −0.387 (p<0.001), Action with Precontemplation: −0.368 (p<0.001), Maintenance with Precontemplation: 0.059 (p=0.442), Action with Contemplation: 0.650 (p<0.001), Maintenance with Contemplation: −0.291 (p<0.001), and Maintenance with Action: 0.209 (p=0.004).
Based on the high level of correlation between the Maintenance and Action factors on the PSOCQ-A, we next examined a 3-Factor model in which the Maintenance and Action factors were combined to determine if fit would be improved. This 3-factor model with the combined Maintenance/Action scale showed poorer fit based on all fit statistics for both the adolescent (PSOCQ-A) and parent (PSOCQ-P) versions assessed at T1 (see Tables 4a&b). Furthermore, comparing the chi-square values between the 4-factor and 3-factor models indicate significantly worse fit among the 3-factor model in both the adolescent and parent measures (χ2 (3)=11.201, p=0.011 for adolescent measure and χ2 (3)=573.399, p<0.001 for the parent measure). Collectively, these findings did not support that the 3-factor model was a better fit than the 4-factor model for both the adolescent and parent measures.
After examination of the modification indices for 4-Factor models, we explored whether modified 4-Factor models which allowed for correlations between items within the existing PSOCQ subscales (factors in the CFA) would improve model fit. We selected items to be correlated based on modification indices. Results for the 4-Factor modified parent version (PSOCQ-P) model showed improvement beyond the previously tested parent models (i.e., the initial 4-Factor and 3-Factor models) across all fit indices (see Table 4b). Specifically, results showed that the RMSEA value of 0.064, CFI = 0.840 and χ2(391) = 801.580 (p < .0001). The factor correlations for the 4-Factor modified PSOCQ-P model were as follows: Contemplation with Precontemplation: −0.519 (p<0.001), Action with Precontemplation: −0.490 (p<0.001), Maintenance with Precontemplation: 0.047 (p=0.559), Action with Contemplation: 0.670 (p<0.001), Maintenance with Contemplation: −0.304 (p<0.001), Maintenance with Action: 0.207 (p=0.004).
We then tested a 4-Factor adolescent version (PSOCQ-A) model modified to allow for correlations between items within the existing PSOCQ scales to determine if this would improve model fit. Results for this model showed improvement beyond the previously tested adolescent models (i.e., the initial 4-Factor [unmodified] and 3-Factor models) across all fit indices (see Table 4a). However, the resulting factor correlations for the 4-Factor modified PSOCQ-A model resulted in an unacceptably high correlation (>1) between the Action and Maintenance scale. The unacceptably high correlation between the Action and Maintenance factors suggest that they are indistinguishable from each other and should be combined into one factor. We therefore ran a final exploratory model to test whether a modified 3-Factor adolescent version (PSOCQ-A) model that allowed for correlations between items within the existing PSOCQ scales would improve model fit. Fit indices for this exploratory 3-Factor model were quite similar to the modified 4-Factor adolescent version (PSOCQ-A) model (RMSEA value of 0.068, CFI = 0.836 and χ2(394) = 868.281, p < .0001). In addition, there was a significant improvement over the 4-Factor unmodified PSOCQ-A model (χ 2(5)=93.604, p<0.001). The resulting factor correlations were: Contemplation with Precontemplation: 0.057 (p=0.482), Maintenance/Action with Precontemplation: −0.314 (p<0.001), Maintenance/Action with Contemplation: 0.470 (p<0.001).
An examination of the individual items reveals that most items loaded strongly onto their assigned factors. However, for both adolescent and parent reports, the Precontemplation subscale appeared relatively less stable than the other subscales, with several items loading less strongly onto this subscale. Specifically, on the adolescent report version, items 29 (“All of this talk about how to cope better is a waste of my time”), 12 (“My pain is a medical problem and I should be dealing with medical doctors about it”) and 16 (“Everybody I speak with tells me that I have to learn to live with my pain but I don't see why I should have to”) had poor factor loadings of 0.32, 0.39 and 0.39, respectively. On the parent report version, items 12 and 16 also had poor loadings (Item 12 = 0.41 and Item 16 = 0.16). Additionally, Items 11 (“We have tried everything that people have recommended to manage his/her pain and nothing helps”) and 25 (“Why can't someone just do something to take away my child's pain?”) had relatively low factor loadings of 0.38 and 0.41, respectively. All other factor loadings on all subscales ranged from 0.47 to 0.81 (see Figures 1 & 2). Removing items 12, 16, and 29 from the adolescent (PSOCQ-A) 3-factor modified model, further improved the fit over the model including all items (RMSEA value of 0.068, CFI = 0.861 and χ2(313) = 690.757, p < .0001). Likewise, removing items 11 and 16 from the parent (PSOCQ-P) 4-factor modified model also further improved fit over the model including all items (RMSEA value of 0.064, CFI = 0.855 and χ2(337) = 692.898, p < .0001). These models represent the best fit to the PSOCQ-A and PSOCQ-P in our data.
PSOCQ Scale reliability and stability
To assess the measure's internal consistency and stability over time in the adolescent and parent samples, we computed Cronbach's alpha coefficients for the Combined Sample at T1 (alpha range 0.71–0.91) and at the 4-week (Sample 1 alpha range 0.71–0.93) and 8-week (Sample 2 alpha range 0.67–0.90) follow ups (see Table 3). The Combined Sample reflects adequate reliability for all of the subscales. Relatively lower alpha coefficients were consistently found for the Precontemplation scale across the samples.
Table 5 reports intraclass correlation coefficients for each PSOCQ subscale by respondent. Separate analyses were conducted for Sample 1 (4-week window) and Sample 2 (8-week window) given the difference in test-retest time frames. Overall results show acceptable stability of the measure at the 4 week follow up time period collected for Sample 1. The 8 week follow up data from Sample 2 shows a decrease in the strength of the correlations relative to correlations between T1 and 4-week follow up, including a non-significant correlation for the Maintenance subscale on the parent report. Overall, findings show good stability but also some change over time, as would be expected after an initial multidisciplinary evaluation which is often followed with initiation of new treatment approaches.
Table 5.
Intraclass correlation coefficients (ICC) indicating stability of PSOCQ subscales over time, by subsample
| Reporter/Subscale | Sample 1 ICC | Sample 2 ICC |
|---|---|---|
| Adolescent Precontemplation | 489*** | .233* |
| Adolescent Contemplation | .570*** | .374*** |
| Adolescent Action/Maintenance | .588*** | .351*** |
|
| ||
| Parent Precontemplation | .507*** | .423*** |
| Parent Contemplation | .589*** | .448*** |
| Parent Action | .506*** | .494*** |
| Parent Maintenance | .436*** | .081 |
p < 0.05,
p< 0.01,
p< 0.001
PSOCQ validity analyses
We tested the hypothesis that higher Action and Maintenance scores for parents and higher Action/Maintenance scores for adolescents would be associated with adolescents' reports of greater use of accommodative coping strategies, and higher Precontemplation scores would associate with greater reliance on passive coping strategies. Use of accommodative coping strategies correlated significantly with the PSOCQ-A Action/Maintenance subscale (r = .37, p<.001). Adolescent report of use of accommodative coping was moderately correlated with the PSOCQ-P Maintenance subscale (r = .17, p<.05). Use of passive coping strategies was significantly correlated with the Precontemplation score on the PSOCQ-A (r = .37, p<.001), but no significant correlation emerged on the parent report of Precontemplation.
The hypothesis that pain catastrophizing (i.e., PCS total score) would associate positively with Precontemplation and negatively with Action and Maintenance scores was partially confirmed. On the PSOCQ-A, significant correlations were noted in the expected directions between adolescent PCS scores and the Precontemplation (r = .33, p < .001), and Action/Maintenance (r = −.15, p <.05) subscales. A positive correlation also emerged between adolescent catastrophizing and the Contemplation subscale (r = .22, p < .001). On the PSOCQ-P, a significant positive correlation emerged between parent reports of catastrophizing and the Precontemplation subscale (r = .20, p <.01), but no other significant associations were observed.
Categorization into a primary PSOCQ stage of change
For adolescents, we found that a total of 139 (54.3%) could be categorized into a Precontemplation stage, while the Contemplation stage included 53 (20.7%), and the Action/Maintenance stage included 64 (25%). A somewhat different pattern emerged for parents, with each primary stage represented at the following rates: Precontemplation 41 (15.9%), Contemplation 65 (25.2%), Action 100 (38.8%), and Maintenance 52 (20.2%). A Chi-square test comparing the distributions of the four primary stages of change indicates significant differences between reporters (χ2(6) = 17.56, p < .01). Specifically, 147/255 (58%) of parents reported a higher stage than the adolescent, 118 (46%) of the dyads were categorized into the same stage, while only 24 (9%) of the adolescents reported a higher stage than their parent.
PSOCQ exploratory correlational analyses
With the exception of adolescent age and PSOCQ-A Contemplation (r=.15, p<0.02), there were no significant correlations between adolescent sex, age, pain duration, or family SES and the PSOCQ-A or –P scales. Chi-square tests revealed no significant associations between pain location (i.e. head, back/neck, limb, etc.) and primary stage of change on either PSOCQ-A or PSOCQ-P.
Table 6 presents correlations between PSOCQ-A and –P with pain intensity and functional measures. PSOCQ-A and PSOCQ-P reports for parallel subscales were all significantly positively correlated. As would be anticipated, adolescent reports of pain and disability were positively correlated with PSOCQ-A Precontemplation scores.
Table 6.
Correlations for Combined Sample PSOCQ-A and −P scales with pain intensity and functional measures
| 1. | 2. | 3. | 4. | 5. | 6. | 7. | 8. | 9. | |
|---|---|---|---|---|---|---|---|---|---|
| 1. PSOCQ-A Precontemplation | - | .041 | −.246** | .356** | −.010 | −.121 | −.114 | .259** | .181** |
| 2. PSOCQ-A Contemplation | - | .431** | −.070 | .313** | .320** | .033 | .006 | .166** | |
| 3. PSOCQ-A Action/Maintenance | - | −.120 | .033 | .256** | .411** | −.122 | .003 | ||
| 4. PSOCQ-P Precontemplation | - | −.345** | −.319** | .050 | .052 | .123* | |||
| 5. PSOCQ-P Contemplation | - | .540** | −.217** | .081 | .033 | ||||
| 6. PSOCQ-P Action | - | .206** | .000 | .026 | |||||
| 7. PSOCQ-P Maintenance | - | −.063 | −.049 | ||||||
| 8. Adolescent's Usual Pain | - | .296** | |||||||
| 9. FDI – Disability Total | - |
p < 0.05,
p < 0.01
Discussion
In the absence of a current validated measure of readiness to adopt a self management approach to pain among adolescents, the primary goal of the current study was to validate adolescent and parent-report adaptations of the PSOCQ. Findings provide initial support for PSOCQ-Adolescent and PSOCQ-Parent versions, which were modified from the original PSOCQ to be developmentally appropriate for adolescent patient self-report and to assess readiness to change in parents of these adolescents. Using confirmatory factor analytic techniques, several models were tested, and based on these analyses a three-factor model for the PSOCQ-A and a four-factor model for the PSOCQ-P were supported. For the PSOCQ-A, a modified 3-factor model that includes a combined Action/Maintenance scale and excludes items 12, 16, and 29 from the Precontemplation scale was ultimately supported as the final model based on overall fit in our sample. For the PSOCQ-P, the modified 4-factor model, where selected items within the existing PSOCQ scales were allowed to correlate, was a clear stand-out, having the strongest support among all models tested. Further examination of the item loadings supported removing items 11 and 16 from the PSOCQ-P Precontemplation scale to improve model fit. This factor structure closely replicates the original PSOCQ [23].
Internal consistency estimates for all subscales of the PSOCQ-A and PSOCQ-P were adequate. Among these estimates, the Precontemplation subscale was less stable than other subscales. Across both measures, item 16 on the Precontemplation scale had low factor loadings. Item 16 may be difficult to interpret, as some respondents may focus more on the phrase, “Everybody I speak with tells me I have to learn to live with my pain,” while others may focus on the more precontemplative aspect of the item, “…I don't see why I should have to.” For adolescents, we found that there was a poor factor loading for item 12, “My pain is a medical problem and I should be dealing with medical doctors about it.” We found that less than 10% of adolescent (and parents) respondents reported any disagreement with this statement. This might suggest that respondents either strongly believe this statement or may not infer a distinction between “medical” (e.g., physicians) and “psychological” (e.g., psychologists, psychiatrists) doctors from this statement. Few adolescents reported agreement with item 29 (“All of this talk about how to cope better is a waste of my time”), while few parents reported disagreement with items 11 (“We have tried everything that people have recommended to manage his/her pain and nothing helps”). Response patterns to these statements may reflect some degree of social desirability bias [25] as well as hopefulness that the current clinical encounter will meet previously unmet needs. Finally, respondents who are more precontemplative may also potentially be less knowledgeable about pain management and/or less motivated to answer items overall. Additional refinement of these poorly loading Precontemplation scale items to generate alternate items that better capture the intent of this scale may prove beneficial in future research. Despite having dropped these items from the Precontemplation subscales for calculating subscale scores, we presently recommend collecting and retaining all 30 items pending replication of these findings in other samples.
In general, parents in our sample appeared further along the stage of change continuum than the adolescents. Approximately one half of adolescents were classified in the Precontemplation stage in our sample, compared to only 16% of parents. Conversely, many more parents (59%) than adolescents (25%) were in the Action/Maintenance phases. This pattern suggests that parents may have a better understanding and appreciation for the value of a multidisciplinary and self-management approach to chronic pain treatment. This is not surprising, as it is typically the parent who takes the initiative to seek out the multidisciplinary evaluation. Further studies are needed to determine how much “buy in” to the self-management approach is necessary from adolescents in order to truly make use of this type of pain treatment. In addition, future research is needed to examine the extent to which timing of PSOCQ-P administration for parents may help to explain the absence of a significant negative factor correlation between the PSOCQ-P Precontemplation and Maintenance scales. This finding may be related to the small number of parents falling into the Precontemplation stage when assessed in the context of an initial pain clinic evaluation. A stronger pattern of factor correlations may be found among samples that include parents who have not yet committed to making an appointment for their child at a specialized multidisciplinary pain clinic and are thus more likely to fall in the precontemplation stage. It also might be the case that parents hold equally strong beliefs that are consistent with both “stages” of readiness. That is, it is conceivable that some parents may perceive that they are committed to a self-management approach and uninterested in making further changes to improve coping. Kerns and colleagues[24] labeled this pattern as “non-contemplative action”. Clearly, further exploration of parents' beliefs may prove important in understanding their perceived roles in promoting optimal pain management and adjustment of their children.
Over a 4-week time period, PSOCQ scores were generally stable, suggesting that this measure reliably assesses readiness to change over this briefer time period. While the 8-week follow up data ICC's were significant, there was an expected decrease in the strength of the correlations for each subscale from T1 to T2 for all subscales. These findings are considered to be consistent with the stage of change model given that patients make progress with treatment and grow more committed to a self-management approach to pain over time[18–19; 21–22].
The correlational findings provide initial support for the validity of the PSOCQ with significant associations between readiness to change and coping and pain catastrophizing. Relationships between these variables were in the predicted directions and consistent with findings for adults [18], but were noted to be stronger for adolescent self-reports for which all hypotheses were supported. Specifically, adolescent reports of accommodative coping were correlated with adolescent Action/Maintenance subscale scores as well the PSOCQ-P Maintenance subscale score, while adolescent passive coping was correlated with adolescent, but not parent, Precontemplation. Relationships between adolescent and parent pain catastrophizing, as assessed by the PCS-C and PCS-P measures, and readiness to change showed strongest associations at the extreme ends of the staging model. In particular, greater adolescent pain catastrophizing was related to higher levels of PSOCQ-A Precontemplation and lower Maintentance, while parental pain catastrophizing was only related to PSOCQ-P Precontemplation. These findings suggest that pain catastrophizing has a more robust relationship with PSOCQ Precontemplation across reporters.
Some limitations to the study are important to consider. Although a strength of our cross-site collaboration was a sample size of at least 5 subjects to each variable[4], we acknowledge that a larger sample size yielding a 10:1 or greater ratio would strengthen these findings [39]. Site-specific differences in procedures and the types and formats of information collected from patients may have influenced our findings in non-specific ways. Findings may not generalize to pediatric pain patients treated in primary care or community settings and there is limited ethnic/racial diversity in our sample of primarily female adolescents and mothers. Finally, we acknowledge that the 3-factor solution for the adolescent version of the PSOCQ raises questions regarding replicability, as it differs from the 4-factor model we hypothesized. Research using the PSOCQ with adults has occasionally identified alternate factor structures, including 2-factor [38] and a 3-factor solution similar to the PSOCQ-A where the Action and Maintenance subscales appeared to be a unitary dimension [5]. From a developmental perspective it may be more difficult for adolescents to distinguish between actively learning self-management strategies and continuing to practice these approaches. Further validation of the PSOCQ model structure across chronic pain populations, including adolescent and parent reporters, is warranted.
Despite these challenges, this project represents initial support for a validated measure of readiness to change for use with pediatric chronic pain patients and has utility in future research contexts. We advise caution regarding use of the measure in clinical contexts at this early stage of development with respect to determining recommendations for clinical care. Within a research context, examining relationships with measures of anxiety, depression, and parental responses to pain will provide a fuller understanding of how the PSOCQ-A and –P function. Future studies are needed to examine the measure as an outcome as well as a potential moderator or mediator of the success of interventions. Questions for further research include whether parent or adolescent readiness for change is more predictive of seeking and, perhaps more importantly, benefiting from pain management services and whether parental readiness to change may influence adolescent readiness to change over time. Future research to develop strategies for tailoring or matching self-management treatment approaches to adolescent and parent readiness to change using the PSOCQ may prove particularly useful. In addition, longitudinal investigations of relationships among measures of readiness to change, treatment adherence, and outcomes within chronic pediatric pain populations are needed to determine the value of adopting a self-management approach to chronic pediatric pain and in the development of more effective treatment approaches.
Summary.
This project represents the initial validation of adolescent (PSOCQ-A) and parent (PSOCQ-P) measures of readiness to adopt a self-management approach to pediatric chronic pain.
Acknowledgements
The authors thank Lisa Meltzer for input on initial development of the PSOCQ-A and -P; Elizabeth Carpino for help with data management at the CHB site; and the staff of the Pediatric Pain Management Clinic at CHOP. Jessica Guite's work on this project was supported in part by Grant No. R03HD054596 from the Eunice Kennedy Shriver National Institute of Child Health and Human Development. Laura Simons' work was supported by Award Number K23HD067202 from the Eunice Kennedy Shriver National Institute Of Child Health & Human Development. Robert Kerns' contributions were supported by the Department of Veterans Affairs, Veterans Health Administration, Office of Research and Development, Health Services Research and Development Service (REA 08-266). The content is solely the responsibility of the authors and does not necessarily represent the official views of the Eunice Kennedy Shriver National Institute of Child Health and Human Development, the National Institutes of Health, or the Department of Veterans Affairs.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest There are no conflicts of interest to report.
References
- [1].Bentler PM, Bonnett DG. Significance tests and goodness of fit in the analysis of covariance structures. Psychol Bull. 1980;88(3):588–606. [Google Scholar]
- [2].Bibace R, Walsh ME. Development of children's concept of illness. Pediatrics. 1980;66:912–917. [PubMed] [Google Scholar]
- [3].Biller N, Arnstein P, Caudill MA, Federman CW, Guberman C. Predicting completion of a cognitive-behavioral pain management program by initial measures of a chronic pain patient' s readiness for change. Clin J Pain. 2000;16(4):352–359. doi: 10.1097/00002508-200012000-00013. [DOI] [PubMed] [Google Scholar]
- [4].Bryant FB, Yarnold PR. Principal components analysis and exploratory and confirmatory factor analysis. In: Grimm LG, Yarnold RR, editors. Reading and understanding multivariale statistics. American Psychological Association; Washington, DC: 1995. pp. 99–136. [Google Scholar]
- [5].Carr JL, Klaber Moffett JA, Sharp DM, Haines DR. Is the Pain Stages of Change Questionnaire (PSOCQ) a useful tool for predicting participation in a self-management programme? Further evidence of validity, on a sample of UK pain clinic patients. BMC Musculoskeletal Disorders. 2006;7(101):1–7. doi: 10.1186/1471-2474-7-101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Claar RL, Walker LS. Functional assessment of pediatric pain patients: Psychometric properties of the Functional Disability Inventory. Pain. 2006;121(1–2):77–84. doi: 10.1016/j.pain.2005.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Crombez G, Bijttebier P, Eccleston C, Mascagni T, Mertens G, Goubert L, Verstraeten K. The child version of the pain catastrophizing scale (PCS-C): A preliminary validation. Pain. 2003;104(3):639–646. doi: 10.1016/S0304-3959(03)00121-0. [DOI] [PubMed] [Google Scholar]
- [8].Dijkstra A, Vlaeyen JW, Rijnen H, Nielson W. Readiness to adopt the self-management approach to cope with chronic pain in fibromyalgic patients. Pain. 2001;90(1–2):37–45. doi: 10.1016/s0304-3959(00)00384-5. [DOI] [PubMed] [Google Scholar]
- [9].Eccleston C, Malleson PN, Clinch J, Connell H, Sourbut C. Chronic pain in adolescents: Evaluation of a programme of interdisciplinary cognitive behaviour therapy. Arch Dis Child. 2003;88:881–885. doi: 10.1136/adc.88.10.881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Gaffney A, Dunne EA. Children's understanding of the causality of pain. Pain. 1987;29:91–104. doi: 10.1016/0304-3959(87)90182-5. [DOI] [PubMed] [Google Scholar]
- [11].Gaffney AA, Dunne EA. Developmental aspects of children's definitions of pain. Pain. 1986;26:105–117. doi: 10.1016/0304-3959(86)90177-6. [DOI] [PubMed] [Google Scholar]
- [12].Glenn B, Burns JW. Pain self-management in the process and outcome of multidisciplinary treatment of chronic pain: Evaluation of a stage of change model. J Behav Med. 2003;26(5):417–433. doi: 10.1023/a:1025720017595. [DOI] [PubMed] [Google Scholar]
- [13].Goubert L, Eccleston C, Vervoort T, Jordan A, Crombez G. Parental catastrophizing about their child's pain. The parent version of the Pain Catastrophizing Scale (PCS-P): a preliminary validation. Pain. 2006;123(3):254–263. doi: 10.1016/j.pain.2006.02.035. [DOI] [PubMed] [Google Scholar]
- [14].Habib S, Morrissey SA, Helmes E. Readiness to adopt a self-management approach to pain: evaluation of the pain stages of change model in a non-pain-clinic sample. Pain. 2003;104(1–2):283–290. doi: 10.1016/s0304-3959(03)00016-2. [DOI] [PubMed] [Google Scholar]
- [15].Hollingshead AB. Four-factor index of social status. Yale University, Department of Sociology; New Haven: 1975. [Google Scholar]
- [16].Jensen MP, Nielson WR, Kerns RD. Toward the development of a motivational model of pain self-management. J Pain. 2003;4:477–492. doi: 10.1016/s1526-5900(03)00779-x. [DOI] [PubMed] [Google Scholar]
- [17].Jensen MP, Nielson WR, Romano JM, Hill ML, Turner JA. Further evaluation of the Pain Stages of Change Questionnaire: Is the transtheoretical model of change useful for patients with chronic pain? Pain. 2000;86(3):255–264. doi: 10.1016/S0304-3959(00)00257-8. [DOI] [PubMed] [Google Scholar]
- [18].Jensen MP, Nielson WR, Turner JA, Romano JM, Hill ML. Readiness to self-manage pain is associated with coping and with psychological and physical functioning among patients with chronic pain. Pain. 2003;104(3):529–537. doi: 10.1016/S0304-3959(03)00092-7. [DOI] [PubMed] [Google Scholar]
- [19].Jensen MP, Nielson WR, Turner JA, Romano JM, Hill ML. Changes in readiness to self-manage pain are associated with improvement in multidisciplinary pain treatment and pain coping. Pain. 2004;111(1–2):84–95. doi: 10.1016/j.pain.2004.06.003. [DOI] [PubMed] [Google Scholar]
- [20].Kashikar-Zuck S, Flowers SR, Claar RL, Guite JW, Logan DE, Lynch-Jordan AM, Palermo TM, Wilson AC. Clinical utility and validity of the Functional Disability Inventory (FDI) among a multicenter sample of youth with chronic pain. Pain. 2011;152:1600–1607. doi: 10.1016/j.pain.2011.02.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Kerns RD, Habib S. A critical review of the pain readiness to change model. J Pain. 2004;5(7):357–367. doi: 10.1016/j.jpain.2004.06.005. [DOI] [PubMed] [Google Scholar]
- [22].Kerns RD, Rosenberg R. Predicting responses to self-management treatments for chronic pain: application of the pain stages of change model. Pain. 2000;84(1):49–55. doi: 10.1016/S0304-3959(99)00184-0. [DOI] [PubMed] [Google Scholar]
- [23].Kerns RD, Rosenberg R, Jamison RN, Caudill MA, Haythornthwaite J. Readiness to adopt a self-management approach to chronic pain: the Pain Stages of Change Questionnaire (PSOCQ) Pain. 1997;72(1–2):227–234. doi: 10.1016/s0304-3959(97)00038-9. [DOI] [PubMed] [Google Scholar]
- [24].Kerns RD, Wagner J, Rosenberg R, Haythornthwaite J, Caudill-Slosberg M. Identification of subgroups of persons with chronic pain based on profiles on the pain stages of change questionnaire. Pain. 2005;116(3):302–310. doi: 10.1016/j.pain.2005.04.022. [DOI] [PubMed] [Google Scholar]
- [25].Logan DE, Claar RL, Scharff L. Social desirability response bias and self-report of psychological distress in pediatric chronic pain patients. Pain. 2008;136:366–372. doi: 10.1016/j.pain.2007.07.015. [DOI] [PubMed] [Google Scholar]
- [26].Maillard SM, Davies K, Khubchandani R, Woo PM, Murray KJ. Reflex sympathetic dystrophy: a multidisciplinary approach. Arthritis Rheum. 2004;51(2):284–290. doi: 10.1002/art.20249. [DOI] [PubMed] [Google Scholar]
- [27].Maurischat C, Harter M, Auclair P, Kerns RD, Bengel J. Preliminary validation of a German version of pain stages of change questionnaire. Eur J Pain. 2002;6(1):43–48. doi: 10.1053/eujp.2001.0271. [DOI] [PubMed] [Google Scholar]
- [28].Maynard CS, Amari A, Wieczorek B, Christensen JR, Slifer KJ. Interdisciplinary behavioral rehabilitation of pediatric pain-associated disability: Retrospective review of an inpatient treatment protocol. J Pediatr Psychol. 2010;35(2):128–137. doi: 10.1093/jpepsy/jsp038. [DOI] [PubMed] [Google Scholar]
- [29].McGrath PA. Pain in Children: Nature, Assessment, and Treatment. Guilford Press; New York, NY: 1990. [Google Scholar]
- [30].Muthen M. Mplus Version 5.21: Muthen & Muthen. 2009 Copyright 1998–2009, Available from: http://www.statmodel.com/
- [31].Prochaska JO, DiClemente CC. The transtheoretical approach; crossing traditional boundaries of therapy. Dow Jones-Irwin; Homewood, IL: 1984. [Google Scholar]
- [32].RFP-Evaluations Centers. What are readability statistics. 2010 Available from: http://rfptemplates.technologyevaluation.com/What-are-Readability-Statistics.html#Flesch_Reading_Ease_Formula.
- [33].Simons LE, Claar RL, Logan DL. Chronic pain in adolescence: Parental responses, adolescent coping, and their impact on adolescent's pain behaviors. J Pediatr Psychol. 2008;33(8):894–904. doi: 10.1093/jpepsy/jsn029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Simons LE, Logan DE, Chastain L, Cerullo M. Engagement in multidisciplinary interventions for pediatric chronic pain: Parental expectations, barriers, and child outcomes. The Clinical Journal of Pain. 2010;26:291–299. doi: 10.1097/AJP.0b013e3181cf59fb. [DOI] [PubMed] [Google Scholar]
- [35].Snow MG, Kerns RD, Rosenberg R, Jarvis JA, McCourt MS, Prochaska JO. Stages of change for chronic pain patients: Development of a questionnaire to assess readiness to change. Paper presented at the Society of Behavioral Medicine; San Francisco, CA. 1993. [Google Scholar]
- [36].Sorbom D. Model modification. Psychometrika. 1989;54:371–384. [Google Scholar]
- [37].Steiger JH, Shapiro A, Browne MW. On the multivariate asymptotic distribution of sequential chi-square statistics. Psychometrika. 1985;50:253–264. [Google Scholar]
- [38].Strong J, Westbury K, Smith G, McKenzie I, Ryan W. Treatment outcome in individuals with chronic pain: Is the Pain Stages of Change Questionnaire (PSOCQ) a useful tool? Pain. 2002;97(1–2):65–73. doi: 10.1016/s0304-3959(01)00493-6. [DOI] [PubMed] [Google Scholar]
- [39].Velicer WF, Fava JL. Effects of variable and subject sampling on factor pattern recovery. Psychological Methods. 1998;3:231–251. [Google Scholar]
- [40].von Baeyer CL, Spagrud LJ, McCormick JC, Choo E, Neville K, Connelly MA. Three new datasets supporting use of the Numerical Rating Scale (NRS-11) for children's self-reports of pain intensity. Pain. 2009;143:223–227. doi: 10.1016/j.pain.2009.03.002. [DOI] [PubMed] [Google Scholar]
- [41].Walker LS. Psychological factors in the development and natural history of functional gastrointestinal disorders. J Pediatr Gastroenterol Nutr. 2008;47(5):687–688. doi: 10.1097/01.mpg.0000338960.40055.4d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [42].Walker LS, Greene JW. The Functional Disability Inventory: Measuring a neglected dimension of child health status. J Pediatr Psychol. 1991;16(1):39–58. doi: 10.1093/jpepsy/16.1.39. [DOI] [PubMed] [Google Scholar]
- [43].Walker LS, Smith CA, Garber J, Van Slyke DA. Development and validation of the pain response inventory for children. Psychological Assessment. 1997;9(4):392–405. [Google Scholar]