Abstract
Context
The role of aerobic physical activity as a standalone treatment in decreasing adiposity in school-aged children and youth has not been well established.
Objective
To systematically search and assess the quality of the literature on the efficacy of aerobic physical activity to decrease adiposity in school-aged children and youth.
Methods
An electronic search strategy was conducted in EBSCO databases, including MEDLINE and CINAHL. Retrieved articles that met the eligibility criteria were rated for methodological quality by using the Downs and Black checklist.
Results
10 articles met the inclusion criteria in the form of RCTs. Results indicate that five articles had positive results in decreasing adiposity compared to controls and five articles had no change in adiposity compared to controls.
Conclusion
There is a paucity of evidence to support aerobic physical activity as a successful standalone treatment for decreasing adiposity. Despite the heterogeneity of the methods there is some evidence to support that school-aged children and youth benefit from aerobic physical activity to decrease adiposity and to limit weight gain.
Keywords: systematic review, physical activity, exercise, adiposity, body mass index, body composition, children, youth
Abstract
Contexte
le rôle de l’activité physique aérobique en tant que traitement autonome afin de réduire l’adiposité chez les enfants d’âge scolaire et les adolescents n’a pas été clairement établi.
Objectif
rechercher systématiquement et évaluer la qualité de la documentation sur l’efficacité de l’activité physique aérobique afin de réduire l’adiposité chez les enfants d’âge scolaire et les adolescents.
Méthodes
une recherche électronique fut menée dans les banques de données EBSCO, notamment MEDLINE et CINAHL. Les articles consultés qui répondaient aux critères d’admissibilité furent évalués en fonction de leur qualité méthodologique à l’aide de la liste de vérification Downs and Black.
Résultats
10 articles répondaient aux critères d’inclusion sous la forme d’essais cliniques aléatoires. Les résultats indiquent que cinq articles démontraient qu’il était possible de réduire l’adiposité par rapport aux contrôles, et que cinq articles démontraient qu’il n’y avait aucun changement par rapport aux contrôles.
Conclusion
il existe suffisamment de preuves solides démontrant que l’activité physique aérobique constitue un traitement autonome efficace pour réduire l’adiposité. Malgré l’hétérogénéité des méthodes, il existe des preuves démontrant que les enfants d’âge scolaire et les adolescents bénéficient de l’activité physique aérobique pour réduire l’adiposité et limiter la prise de poids.
Keywords: évaluation systématique, activité physique, exercice, adiposité, indice de masse corporelle, composition du corps, enfants, adolescents
Introduction
Physical inactivity is one of the leading causes of major chronic illness tracking from childhood into adulthood1. Overweight and obese children are four times more likely to become overweight adults, thus leading to major chronic illnesses such as type-two diabetes, heart disease, and cancer1. Physical inactivity is leading to a global epidemic of childhood obesity1. In 2010, The World Health Organization (WHO) stated that physical inactivity is the fourth leading risk factor for global mortality.1 There is a widespread concern in Canada that the prevalence of overweight and obese children and youth are reaching epidemic proportions.2 Obesity is on the rise in Canada with approximately 26% of Canadian children and youth between the ages of two and 17 years of age over the 90th percentile for body weight.3
Canada first set physical activity guidelines for children and youth in 2002 to promote healthy active living in the Canadian population.4,5 Health Canada, now the Public Health Agency of Canada (PHAC), in conjunction with the Canadian Society for Exercise Physiology (CSEP) developed basic guidelines to give physical activity guidance to Canadian children (5–11) and youth (12–17).4,5,6,7 The recommended target in 2002 was for children and youth to complete a minimum of 30 minutes of physical activity per day and progressively increase to 90 minutes per day of moderate to vigorous intensity activity.1,4,5
As of early 2011, the PHAC in conjunction with the CSEP changed their physical activity guidelines for children and youth.4,5,6,7 For health benefits, children (5–11) and youth (12–17) should accumulate at least 60 minutes of moderate to vigorous physical activity daily.4,5,6,7 Thus, there has been a decrease in the recommended amount for physical activity of Canadian children and youth. A common intervention for overweight and obese children is an aerobic physical activity program to decrease adiposity.
Reversing the trend of increasing adiposity in children has been proven to be an extremely difficult task. It has been widely acknowledged that increasing physical activity to increase total energy expenditure and reducing caloric intake may form the theoretical basis for the management of obesity.4,5,6,7 Thus, increasing aerobic physical activity may be the foundation for decreasing childhood obesity and a first step to behavioural change. Increasing physical activity has been supported in recent years by the WHO, PHAC, and CSEP.1,4,5,6,7 The objective of this systematic review was to determine the quality of current evidence forming the relationship between aerobic physical activity and adiposity changes in school-aged children and youth. We reviewed randomized controlled trials (RCTs) that assessed the efficacy of physical activity programs for decreasing adiposity in school-aged children and youth with sedentary controls.
Physical Activity Guidelines for Children and Youth
There are currently two separate guidelines published to give physical activity guidance to Canadian children and youth.4,5,6,7 These new guidelines recommend children and youth should accumulate at least 60 minutes of moderate to vigorous intensity physical activity daily.4,5,6,7 Moderate physical activity is defined as 3–6.9 metabolic equivalents (METS) for example brisk walking and bicycle riding.4,5,8 Vigorous physical activity is defined as >7 METS for example running, tennis, and jumping jacks.4,5,8 Children and youth should engage in vigorous physical activity at least three days per week and resistance training three days per week for health benefits. CSEP also developed the Canadian Sedentary Behaviour Guidelines. Children and youth should minimize the time spent being sedentary each day by limiting recreational screen time to no more than two hours per day which is now consistent with the guidelines published by the Canadian Pediatric Society.4,5,6,7 Screen time refers to the amount of time spent sedentary in front of electronic devices including televisions, computers, and video games.
In 2011 the Canadian physical activity guidelines changed significantly to reflect global harmonization in the guidelines.1,4,5,6,7 The guidelines now define physical activity participation in an absolute amount and no longer incorporate progression. Previously the physical activity guidelines stated that children and youth should increase the time spent being physically active by 30 minutes per day and progress to a minimum of 90 minutes per day.4,5,6 Now the guidelines recommend a minimum of 60 minutes per day everyday.4,5,6,7 Further, the guidelines used to recommend that children and youth should decrease screen time to less than 90 minutes per day.4,5 Today, it is recommended that screen time should be decreased to less than two hours per day.4,5,6,7
Canada’s physical activity guidelines formerly pertained to a limited age span of children between six to nine years of age and youth between 10–14 years of age, allowing for specific promotional and educational materials to be directed at different age groups.4–10 As of 2011 the guidelines have included five year olds up to 17 year olds to comprise a larger target.
The PHAC and CSEP have created physical activity guidelines for the Canadian population to increase healthy active living.4,5,6,7 A sedentary lifestyle is one of the leading causes of obesity. According to a systematic review performed by Janssen and LeBlanc the relationship between physical activity and obesity in school-aged children and youth has been extensively studied via observational studies.11 Low-level physical activity studies have reported that there is a weak to modest relationship between physical activity and obesity.11 Interestingly, studies that have looked at moderate to vigorous physical activity have reported a stronger correlation than low-level physical activity.11 These studies have reported that there is a dose-response relationship between physical activity and obesity.11–25 Thus, with an increase in physical activity in school-aged children and youth there will be a decrease in adiposity leading to a decrease in obesity.
We hypothesize that aerobic physical activity, as a standalone intervention will decrease measures of total adiposity in response to an increase in aerobic training in school-aged children and youth.
Methods
Search Strategy
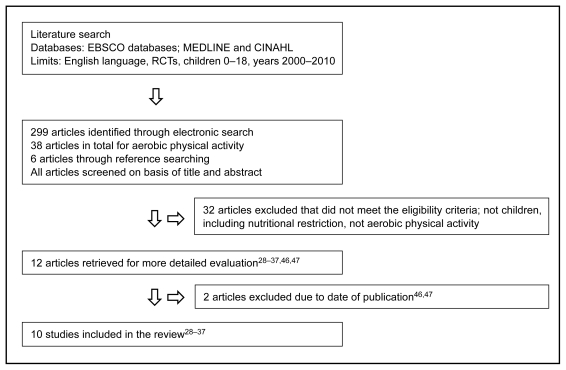
Figure 1 depicts the flow of trials through the review. Studies were identified by searching electronic databases and scanning reference lists of articles identified. The electronic literature search was conducted by one independent reviewer in the EBSCO databases in MEDLINE and CINAHL up to and including December 2010. The MeSH terms used were [“Exercise”, “Leisure Activities”, “Physical Endurance” OR], [“Body Mass Index”, “Body Fat Distribution”, “Overweight”, “Skinfold Thickness”, “Adipose Tissue”, “Obesity”, and “Body Composition” OR]. Text words were used [“Physical activity”, “fitness”, “exercise”, “energy expenditure” OR] and [“obese”, “obesity”, “overweight”, “body composition”, body mass index”. All MeSH terms and text words were combined with aerobic* and the following limiters: English language; from 2000–2010; age related: All children and adolescents 0–18 years; and Publication Type: Randomized Controlled Trials. The reference lists from all retrieved papers were reviewed for further relevant articles that may not have been included in the initial electronic search.
Figure 1.
Literature Search Flow
Screening of citations
The authors independently examined the electronic search results. The titles and abstracts of the 38 articles found in the search strategy were examined to determine which full-text manuscripts met the eligibility criteria to be included in the review. The eligibility criteria used is indicated in Table 1. The eligibility criteria were applied to all of the obtained full text manuscripts and consisted of studies that were RCTs conducted on children between 0–18 years of age. Interventions included aerobic physical activity with no co-interventions of caloric restriction allowed; these could be compared to a sedentary control group, an active controlled group, or a sedentary control with lifestyle education only. Studies must have had an outcome measure for determining adiposity. Only articles published in a peer-reviewed journal in the English language within the past 10 years (2000–2010) were considered. These criteria were applied to all of the obtained manuscripts. The eligibility assessment was performed independently by two reviewers and if disagreement between reviewers was identified it was resolved by consensus.
Table 1.
Review of eligibility criteria
| Inclusion Criteria | Exclusion Criteria |
|---|---|
| RCTs | Cross-sectional studies, case-control studies, case studies, prospective or retrospective cohort studies, reviews, or personal narratives |
| Published in peer-reviewed journal | Published in a non-peer reviewed journal |
| Published in the English language | Not published in the English language |
| All children between 0–18 years of age | Adult subjects |
| Published between January 2000 and December 2010 | Published before January 2000 |
| Studies must have used some outcome measure for determining adiposity (body composition, percent body fat, weight, body mass index (BMI), skinfold thickness, trunk and visceral fat composition, and adiponectin levels) | Studies without an outcome measure |
| Intervention group provided with aerobic physical activity | Intervention group did not perform any aerobic physical activity or included nutrition in the intervention |
| Control group consisting of sedentariness, maintaining current levels of physical activity, or sedentariness with lifestyle counseling | No control group |
For the purpose of this review fitness and exercise are considered proxy measures for physical activity
Data collection process
The authors independently reviewed the published studies meeting the inclusion criteria and conducted a critical appraisal of the studies. The following items were extracted: objectives, interventions, outcome measures used, results, adverse events, and drop-outs. The specific design of the study was extracted to ensure it was a RCT. Details of the population used including all baseline characteristics and samples sizes for the intervention groups and the control groups were recorded. Specific details of the intervention groups and control groups were extracted including the frequency, intensity, and duration of the intervention, the number of sessions per week, and the format for each intervention (group training sessions, supervised sessions, or individual sessions). (See Table 2 and 3). In addition, the method of randomization, blinding procedures, statistical analysis, sample sizes, and power were extracted and recorded. To ascertain the validity of eligible RCTs, the two reviewers worked independently. With adequate reliability the two reviewers determined the adequacy of the randomization process, the concealment of randomized allocation to groups, blinding of the participants in the study, blinding of the authors and data collectors.
Table 2.
| Reference | N | Power | Age | Sex | Subjects | Total Score | Intervention outcome |
|---|---|---|---|---|---|---|---|
| Aguilar et al.37 | 1044 | 5/5 | 9–10 | Both | Average weight children and adolescents | 23/32 | Decreased BMI |
| McMurray et al.29 | 1140 | 5/5 | 11–14 | Both | Average weight children and adolescents | 22/32 | No change in BMI or body composition |
| Farpour-Lambert et al.30 | 44 | 0/5 | 6.5–10 | Both | Pre-pubertal obese children | 21/32 | Decreased BMI, body composition, abdominal fat, & triglycerides |
| Meyer et al.32 | 67 | 0/5 | 11–16 | Both | Obese adolescents | 19/32 | Decreased BMI, waist/hip ratio, triglycerides |
| Kelly et al.33 | 20 | 0/5 | Mean 10.9 | Both | Over-weight children and adolescents | 18/32 | No significant difference in body weight, BMI, percent body fat, triglycerides |
| Gutin et al.34 | 80 | 0/5 | 13–16 | Both | Obese adolescents | 17/32 | Decreased total body composition |
| Heyman et al.28 | 16 | 0/5 | Mean 16.1 | Female | Type 1 Diabetes | 16/32 | Unchanged body fatness Increased body fatness on controls |
| Hagstromer et al.35 | 31 | 0/5 | 13–15 | Both | Obese adolescents | 16/32 | No change in BMI & total body weight |
| Kelly et al.31 | 19 | 0/5 | Mean 10.8 | Both | Over-weight | 15/32 | No change in total body weight, adipocytes, or adipokines |
| Tan et al.36 | 60 | 0/5 | 9–10 | Both | Obese children | 14/32 | No difference between BMI, skinfolds & waist girth |
Results listed in order of methodological quality based on the Downs and Black checklist.22
All study designs are RCTs.
Table 3.
| Reference | Frequency d/wk | Duration mins/d | Length Wks/mos | Intensity |
|---|---|---|---|---|
| ^Aguilar et al.37 | 3 d/wk | 90 mins/d | 28 wks | Unknown |
| McMurray et al.29 | 3 d/wk | 30 mins/d | 8 wks | Unknown |
| ^ Farpour-Lambert et al.30 | 3 d/wk | 60 min/d | 3 mos | 55–60 max HR |
| ^ Meyer et al.32 | 3 d/wk | 60–90 mins/d | 6 mos | unknown |
| Kelly et al.33 | 4 d/wk | 30–50 mins/d | 8 wks | 50–80% V02max |
| ^ Gutin et al.34 | 5 d/wk | Unknown | 8 mos | Grp 2: 55–60% V02max Grp 3: 75–80% V02max |
| Heyman et al.28 | 2 d/wk | 90 mins/d | 6 mos | 80–90% max HR |
| Hagstromer et al.35 | 1 d/wk | 60 mins/d | 13 wks | unknown |
| Kelly et al.31 | 4 d/wk | 30–50 mins/d | 8 wks | 50–80% V02max |
| Tan et al.36 | 5 d/wk | 50 mins/d | 8 wks | Lactate Threshold |
Results listed in order of methodological quality based on the Downs and Black checklist.24
Denotes significant change in outcome for intervention group.
Quality of the Studies
The methodological quality of all studies that met the eligibility criteria were assessed independently by the authors using the Downs and Black checklist.26 The checklist is considered a reliable and valid tool to report on the methodological quality of randomized and non-randomized studies.26 (See Table 4).
Table 4.
Methodological quality scoring method
| No. | Item Description | Hagstromer et al.35 | Kelly et al.31 | Meyer el al.32 | Gutin et al.34 | Heyman et al.28 | McMurray et al.29 | Kelly et al.33 | Tan et al.36 | Aguilar et al.37 | Farpour- Lambert et al.30 |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Hypothesis/aim/objective described? | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| 2 | Main outcomes to be measured described?1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| 3 | Characteristcs of patients described? | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 0 | 0 | 1 |
| 4 | Interventions of interests clearly described? | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 |
| 5 | Distributions of confounders described? | 2 | 2 | 2 | 1 | 2 | 0 | 2 | 0 | 2 | 2 |
| 6 | Main findings clearly described? | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| 7 | Estimates of random variability in data? | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| 8 | Important adverse events reported? | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 9 | Described patients lost to follow-up? | 0 | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 10 | Actual probability values reported except where P values <.001? | 0 | 0 | 1 | 1 | 0 | 1 | 1 | 0 | 1 | 1 |
| 11 | Subjects asked to participate representative of entire population? | 0 | 0 | 0 | 1 | 1 | 0 | 1 | 0 | 1 | 1 |
| 12 | Subjects prepared to participate representative of population? | 0 | 0 | 0 | 0 | 1 | 1 | 0 | 1 | 1 | 1 |
| 13 | “Staff, places, facilities representative of treatment majority of patients receive?” | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 |
| 14 | Attempt made to blind subjects? | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| 15 | Attempt made to blind those measuring the outcomes to intervention? | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 |
| 16 | “Any of the results based on “”data dredging,”” was this made clear?” | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| 17 | “Analysis adjust for different lengths of follow-up of patients, or is this time period between the intervention and outcome the same for cases and controls?” | 1 | 0 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 1 |
| 18 | Statistical tests appropriate | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 0 | 1 |
| 19 | Compliance with treatments reliable? | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 |
| 20 | Outcomes measures valid/reliable? | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| 21 | Patients in intervention groups or cases and controls recruited from the same population? | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 |
| 22 | Subjects in different intervention groups or cases and controls recruited over same time period? | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 1 |
| 23 | Subjects randomized to groups? | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| 24 | Randomized assignments concealed until recruitment was complete? | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 1 |
| 25 | Adjustment for confounding in analyses? | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| 26 | Losses to follow-up accounted for? | 0 | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 27 | Sufficient power to detect clinically important effect where P value for differences due to chance is <5% | 0 | 0 | 0 | 0 | 0 | 5 | 0 | 0 | 5 | 0 |
| Total Score out of 32 | 16/32 | 15/32 | 19/32 | 17/32 | 16/32 | 21/32 | 18/32 | 15/32 | 23/32 | 22/32 |
Due to the extreme heterogeneity in the study results we hypothesized that the effect size may differ between studies according to the methodological quality of the studies analyzed. The Downs and Black assessment of power is provided in Table 5. There are 27 questions with a total score out of 32.26 Scores above 20 were considered of high methodological quality; 11–20 moderate quality; and below 11 were considered of poor methodological quality. All scoring can be found in Table 4. No attempts were made at meta-analysis as there was too much heterogeneity between the studies to allow for a suitable synthesis.
Table 5.
Downs and Black assessment of power27
| Downs and Black | Size of smallest intervention grp | Power | Score |
|---|---|---|---|
| A | <58 | .70 | 0 |
| B | 59–72 | .80 | 1 |
| C | 73–82 | .85 | 2 |
| D | 83–96 | .90 | 3 |
| E | 97–118 | .95 | 4 |
| F | >119 | .99 | 5 |
Results
A total of 10 RCTs were identified for inclusion in the review.28–37 The search of EBSCO databases in MEDLINE and CINAHL using all MeSH terms and search terms combined with limiters produced a total of 299 articles. To specify only aerobic physical activity aerobic* was added as a text word and resulted in 399 articles. Adding all the MeSH terms with all search terms, including aerobic*, and limiters resulted in 38 articles. Of these, 32 studies were discarded because after reviewing the titles and abstracts it appeared that these papers did not meet the inclusion criteria of the review. These studies were primarily discarded due to inclusion of a nutritional intervention or exclusion of aerobic physical activity in the intervention group. The full-text of the remaining six citations were examined in more detail. It appeared that all six studies met the inclusion criteria and were included in this review. An additional six studies met the criteria for inclusion and were identified by checking the references of relevant papers. Two of the additional studies were excluded because they did not meet the inclusion criteria. No unpublished preliminary studies were included in this review. (See Figure 1) Appendix 1 provides a summary of the results for each of the 10 studies.
Appendix 1.
Results Table
| Author(s) | Score | Population | Sample Size | Intervention | Outcome |
|---|---|---|---|---|---|
| Hagstromer et al., 2008 | 16/32 | 10–18 year old adolescents | 31 subjects; Exercise grp n = 16 Control grp n = 15 |
Exercise; 1hr/wk for 13wks Session 1 brisk walking, 2–5 spinning, 6–9 strength training 50–70% 1RM, 10–13 swimming |
No change in BMI, total body weight, or BMI SD-score |
| Kelly et al., 2007 | 15/32 | Overweight children (BMI >85th percentile) Exercise grp 10.0 ± 0.67 Control grp 11.0 ± 0.71 |
20 children randomly assigned to exercise or control grp | 4d/wk for 8wks of stationary cycling wks 1–3 50–60% V02 max for 30 mins wk 4–7 60–70% V02 max for 40 mins wk 8 70–80% V02 max for 50 mins Control grp – maintain normal physical activity |
No change in total body weight, adipocytes, or adipokines |
| Meyer et al., 2006 | 19/32 | 11–16 year old obese children Exercise grp 13.7 ± 2.1 Control grp 14.1 ± 2.4 |
67 obese children randomly assigned to control (34; 17 boys and 17 girls) and exercise grp (33; 17 boys, 16 girls) | 3 d/wk for 6 months (Mon: swimming, aqua aerobic class for 60 mins; Wed: Sports for 90 mins; Fri: Walking for 60 mins). | decreased BMI, waist/hip ratio, insulin, insulin resistance, triglycerides, low-density lipoproteins, fibrinogen, and C reactive protein |
| Gutin et al., 2002 | 17/32 | Obese 13–16 year old youth | 80 obese youth were randomly assigned to 1 of 3 grps group 1; lifestyle ed group 2; moderate physical exercise + lifestyle ed group 3; vigorous physical training + lifestyle ed | 5 d/wk for 8 months; target HR >170 bpm; mod PA 55–60% V02max, vigorous PA 75–80% V02max | Moderate and vigorous PA decreases total body composition. Vigorous PA is more effective than moderate PA for cardiovascular health. PA enhances body composition in obese children but intensity is unknown |
| Heyman et al., 2007 | 16/32 | Diabetic girls 13–18.5 | 16 diabetic girls were randomly assigned to 6 months training program (n = 9) and 6 months non training program (n = 7) | 3hrs/wk for 6 months at 80–90% max HR | Body fatness remained the same in the PA grp and increased in the control grp |
| *McMurray et al., 2002 | 21/32 | 11–14 year old children and youth | 1140 children and youth were randomly assigned to into 4 grps
|
30 mins aerobic exercise 3 d/wk for 8 wks | No change in BMI or body composition but decrease in skinfold thickness after 8 wks |
| Kelly et al., 2004 | 16/32 | Overweight and obese children (10.9 ± 0.4) | 20 overweight and obese children were randomly assigned to exercise grp or control grp | Exercise grp – 4 d/wk for 8 wks of stationary cycling for 30mins 50– 60% V02max and increasing over 8 wks to 50 mins 70–80% Control – maintain current levels of PA |
No significant difference btwn grps over 8wks in body weight, BMI, percent body fat, LDL, or triglycerides |
| Tan et al., 2010 | 15/32 | Obese children 9–10 years of age | 60 obese children; 26 girls and 34 boys were randomly assigned to 8wk training program at lactate threshold and a control grp | Exercise grp – 5 d/wk for 8wks 50 mins per session for a total of 40 sessions maintaining HR at lactate threshold | No difference between BMI, skinfolds, and waist girth |
| *Aguilar et al., 2010 | 23/32 | 1044 4th–5th grade children from 20 different schools | 1044 10 schools were randomly assigned to a 28 week training program and 10 schools to a control group | Exercise group – 3 d/wk for 28 wks 90minutes each session | Significant decrease in BMI in exercise group |
| *Farpour-Lambert et al., 2009 | 22/32 | Obese children 8.9 ± 1.5 years old | 44 pre-pubertal obese children were randomly assigned to an exercise grp (n = 22) or a control grp (n = 22) | 3 d/wk 60 mins/d for 3 months at 55–65% V02 max | Exercise grp had a significant decrease in BMI, body composition, abdominal fat, and triglycerides |
highest methodological quality.
Methodological quality
Table 4 depicts the quality score of each of the included studies. The Downs and Black checklist was used to adequately evaluate the methodological quality of all 10 of the reviewed studies and allowed for greater objectivity in the results.26 All 10 of the RCTs reviewed contained several significant methodological limitations. Many of the intervention group sizes were too small and not fully representative of the entire population. The lack of power was a significant issue for most studies and few studies addressed this deficiency.28,30,31–36 Aguilar at al.37 and McMurray et al.29 had the largest intervention groups and thus ultimately had significant power ratings.
The majority of the studies (n = 7) included in this review were of moderate methodological quality.28,31–36 Aguilar et al.,37 McMurray et al.,29 and Farpour-Lambert et al.30 were all considered to be of high methodological quality.29,30,37 The highest score on the Downs and Black scoring system was 23/32 achieved by the Aguilar et al. study.37
All 10 of the studies failed in reporting the important adverse events that may have been a consequence of the intervention.28–37 Adverse events such as musculoskeletal injuries may occur in physical activity programs. Also, the majority (n = 8) of the studies failed in reporting the characteristics of the subjects that were lost to follow-up.28–30,33–37 Four of the studies reviewed achieved a score of zero for external validity highlighting that the authors failed to describe if the subjects were representative of the entire population.31–33,35 Four of the studies reviewed achieved a score of two for external validity highlighting that some of the reviewed studies did report if the subjects, staff, and facilities were representative of the entire population.28,30,34,37
The majority of the studies (n = 9) failed in reporting the blinding procedures and if there was compliance with the intervention.28,29,31–37 Shortcomings in selection bias were also evident in the majority of the studies that were reviewed. Eight of the studies failed to report if the randomization process was concealed from both parents and health care staff until recruitment was complete.28,29,31–36
Only two of the studies reviewed had significant power to detect a clinically important effect of physical activity on adiposity according to the Downs and Black checklist.29,37 A small intervention group will not have significant power to see a decrease in adiposity with a physical activity intervention. Two of the studies revealed a power rating of 5/5 on the Downs and Black checklist, although this is due to large intervention groups.29,37 Conversely, eight of the other studies reviewed had a rating of 0/5 on the Downs and Black checklist due to small intervention groups.28,30–36 It may be possible to rate question 27 on the Downs and Black checklist as 1/1 for significant power and 0/1 insufficient power. This review did not change the Downs and Black checklist but there have been recent papers that have changed question 27.29,38 Thus, it is important to bring to the readers’ attention the potential flaw of question 27 on the Downs and Black checklist.
Participants
The sample sizes in the 10 studies ranged from 16 to 1140.28–37 Five of the studies included sample sizes that ranged from 44 to 90.30,31 All the studies had participants that ranged in age from 6.5 to 18.5 years old.28–37 Six of the studies included subjects that were considered to be over the 90th percentile in weight.30–34,36 Three of the studies used normal healthy weight children.29,35,37 Only one study looked at subjects that were previously diagnosed with diabetes and were considered to be overweight or obese.28
Primary Outcome
It is important to note that of all the RCTs examined, obesity was not always the primary health outcome measured. In many of the experimental studies the primary aim of the study was to improve other health measures and not specifically measures of adiposity.28–33 All 10 of the studies looked at different methods of measuring obesity including weight, body mass index, skinfolds, percentage of body fat, waist circumference, trunk and visceral fat composition.28–37 The most common control intervention used within the studies was a sedentary control group (n = 5). Four of the studies maintained current levels of physical activity as a control intervention and one study used a sedentary control group with lifestyle counseling. The time of the exercise session varied between all 10 studies in this review. The length of each intervention ranged from eight weeks to eight months in duration. The results show that interventions of longer duration can have beneficial effects on adiposity in children and youth.30,32,34,37 The frequency of exercise prescription also ranged significantly from one day per week to five days per week of aerobic exercise. The duration of each session varied between studies from 30 minutes per day to 90 minutes per day. (See Table 3).
Five of the exercise intervention studies showed no change in body composition, percentage of fat, or body mass index in response to a training program.29,31,33,35,36 Four of the exercise intervention studies showed a decrease in body mass index, hip to waist ratio, or body fat composition in response to the training program.30,32,34,37 Heyman et al. showed an increase in body fat composition in response to an aerobic training program of six months duration however less weight gain compared to controls.28 Only Hagstromer et al. employed more than aerobic physical activity by incorporating strength training into the intervention.35 However, Hagstromer et al. did not show a change in body mass index after 13 weeks of exercise compared to the control group.35
According to Aguilar et al., the study with the highest methodological quality, aerobic physical activity three days per week for 90 minutes for 28 weeks in duration can significantly decrease body mass index.37 The intensity of exercise in the intervention group in Aguilar et al. study is unknown.37
Discussion
Overall, the evidence is not sufficiently strong to determine the efficacy of aerobic physical activity as a standalone treatment for decreasing adiposity of school-aged children and youth. Only five RCTs showed positive results of aerobic physical activity as a standalone treatment for decreasing adiposity.28,30,32,34,37 There is a paucity of evidence to suggest that aerobic physical activity should be used as a standalone treatment for obesity.28,30,32,34,37 Thus, chiropractors and other healthcare practitioners should potentially use a combined approach of diet and exercise to decrease adiposity in school-aged children and youth.
There is considerable evidence on the health benefits of physical activity in children and youth.8,11,40 Leading a physically active lifestyle is an extremely important part of healthy living for children and youth.8 Strong et al. performed a systematic review of the literature to evaluate the evidence linking physical activity to health and behavioural outcomes in school-aged children and youth.40 The results showed that physical activity has beneficial effects on adiposity, musculoskeletal health and fitness, cardiovascular health, blood pressure, plasma lipids, lipoprotein levels, and on several components of mental health.40 Thus, prescribing physical activity as part of a healthy lifestyle is an important component of clinical practice.
Due to variation in the age, sex, exercise frequency, exercise intensity, and exercise duration, limited conclusions can be made on recommendations of aerobic physical activity frequency, duration, and intensity. Also, due to the lack of adequate intervention sizes and power in the majority of the studies (n = 8) it is difficult to draw any definite conclusions regarding whether or not aerobic physical activity effects adiposity in school aged children and youth.
This review shows that there is a paucity of evidence to support that aerobic physical activity has beneficial effects on adiposity of those with normal body mass and those with a body mass in the 90th percentile of weight.30,32,34,37 However, fifty percent of the studies did not find a decrease in adiposity. Thus, for the practicing chiropractor there is limited evidence to support the sole use of aerobic physical activity to treat obesity based on the results of five positives studies and five studies with no change and all with varying quality. This review shares similar results to a meta-analysis on the effects of school based physical activity programs on BMI in children.41 The results of the meta-analysis performed by Harris et al. showed that school-based physical activity programs may not be sufficient to decrease BMI in school-aged children.41 The author further concluded that a combined approach of diet and exercise may be the appropriate treatment measure for increased adiposity in young children and youth.41
A recent study analyzing sedentariness, screen time, physical activity, and nutrition found that all may be significant contributors to decreasing body composition in children and youth and should be incorporated into any intervention.40,45 The role of proper nutrition and caloric restriction combined with a physical activity program may play a role in decreasing adiposity in school-aged children and youth. Knopfli et al.42 performed a study on the effects of an eight-week multidisciplinary inpatient program on body weight, body composition, aerobic fitness, and quality of life in obese children and youth. The results showed that a multidisciplinary inpatient treatment program including moderate calorie restriction to 1200–1400k/cal per day, daily physical activity of 60 to 90 minutes in duration two times per day, and behaviour modification can significantly decrease adiposity in school-aged children and youth.42
There are currently no intervention studies that have reviewed the health effects of the previous or current Canadian physical activity guidelines.4,5,6,7 Based on Janssen and LeBlanc’s systematic review on the health benefits associated with physical activity, there is strong evidence to suggest as little as two to three hours per week of moderate to vigorous physical activity are associated with health benefits.11 Thus, it seems appropriate to set a minimal target of 30 minutes per day of physical activity that reflect the low levels of physical activity in inactive and sedentary children and youth.11 However, a recommendation of at least 60 minutes per day is more appropriate for overall health benefits.1,11 Implementing an average of 60 minutes per day instead of 60 minutes everyday has been recommended because physical activity on a daily basis has not been validated within the current literature.11 It is known that physical activity should be at least moderate intensity but more consideration on the impact of low intensity activities on health benefits for children and youth is needed.11 Aerobic activities should make up the majority of the physical activities performed by children and youth because of its effects on body mass index, cardiovascular health, blood lipid profiles, and metabolic syndrome.11
This review has some possible limitations including the limitations in the original literature itself; there may be inherent bias in the original studies. Another possible limitation in this review is the language bias as we only permitted articles published in the English language. The studies reviewed predominately involved young children who may not have appreciated the importance of not breaching protocol from their assigned groups, thus corrupting the study to some content. We did not search EMBASE, MANTIS, or Cochrane libraries. However, we did conduct a thorough search strategy using two electronic databases with hand reference searching of obtained articles, thus measures were taken to evaluate the current state of literature. It could be argued that a weakness in this review was the inclusion criteria. This systematic review only included RCTs according to the eligibility criteria employed to review the highest quality of evidence. Only reviewing RCTs can exclude other clinical studies that may change the results of this review.
The primary limitation amongst the selected studies was the lack of homogeneity of the study designs and thus definitive conclusions in regard to frequency, intensity and duration of aerobic physical activity to decrease adiposity is difficult to make. There are no studies in the current literature that utilize the current or previous guidelines created by CSEP for their intervention strategies. In particular, future research on physical activity interventions should consider utilizing the Canadian physical activity guidelines for children and youth outlined by CSEP to determine exact exercise prescription.
Future research in this area should take place to determine the rates at which chiropractors recommend or prescribe physical activity to decrease adiposity in children and youth. Future systematic reviews should be conducted to assess the value of only caloric restriction on childhood obesity. Moreover, the combination of both physical activity and caloric restriction should be addressed in a systematic review of the literature. The current body of literature on physical activity and obesity in children is lacking evidence for a combined approach of increased physical activity and decreased caloric intake for weight loss or overall changes in body composition and adiposity. It may be hypothesized that a combined approach of caloric restriction and physical activity may essentially be an effective method for decreasing adiposity in school-aged children and youth.
Chiropractors and other healthcare practitioners need to educate themselves, parents, and children on the benefits of regular physical activity and sport participation. A combined approach of physical activity and caloric restriction may be the most effective method to combat childhood obesity. Chiropractors and other healthcare practitioners should promote a healthy lifestyle by emphasizing proper nutrition and following the physical activity guidelines. Parents can strongly influence physical activity behaviours in children through role-modeling and direct involvement in physical activities.43,44 Parental influence on physical activity may also track into adulthood leading to more physically active adults and less health complications.43,44 There is a growing need for chiropractors to play a more influential role in the community when it comes to physical activity and sport participation in young school-aged children and youth.
Conclusion
The childhood obesity epidemic is rapidly growing and affects all socioeconomic levels and ethnicities.44 Excessive weight in children and youth is linked to cardiovascular disease, orthopedic problems, and psychosocial constraints that track into adulthood.44 The increase in sedentary behaviour and decrease in aerobic fitness may cause an increase risk of obesity in school-aged children and youth.45 A focus on early physical activity intervention is thus urgently needed. There is a paucity of evidence to support aerobic physical activity as a successful standalone treatment for decreasing adiposity. Despite the heterogeneity of the methods there is some evidence to support that school-aged children and youth benefit from aerobic physical activity to decrease adiposity and to limit weight gain. Results of this systematic review make it difficult for chiropractors and other healthcare providers to justify the recommendation of aerobic physical activity as a standalone treatment for decreasing adiposity. Further, an effective approach to weight loss may be a combination of physical activity and caloric restriction. Further research is necessary before any definitive statements can be made with regards to the recommendation of only aerobic physical activity and its effects on adiposity in young children and youth.
References
- 1.World Health Organization. Global Strategy on Diet, Physical Activity, and Health. The World Health Organization; 2010. [Google Scholar]
- 2.Tremblay MS, Willms JD. Is the Canadian childhood obesity epidemic related to physical inactivity? International J Obesity. 2003;27:1100–1105. doi: 10.1038/sj.ijo.0802376. [DOI] [PubMed] [Google Scholar]
- 3.Lau DCW, Douketis JD, Morrison KM, Hramiak IM, Sharma AM, Ur E. Canadian clinical practice guidelines on the management and prevention of obesity in adults and children [summary] Can Med Assoc J. 2006;176(8):1–13. doi: 10.1503/cmaj.061409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Health Canada, Canadian Society for Exercise Physiology. Canada’s Physical Activity Guide for Youth. Ottawa: Minister of Public Works and Government Services Canada; 2002. [Google Scholar]
- 5.Health Canada, Canadian Society for Exercise Physiology. Canada’s Physical Activity Guideline for Children. Ottawa: Minister of Public Works and Government Services Canada; 2002. [Google Scholar]
- 6.Tremblay MS, Warburton DER, Janssen I, Paterson DH, Latimer AE, Rhodes RE, Kho ME, Hicks A, LeBlanc AG, Zehr L, Murumets K, Duggan M. New physical activity guidelines. Appl Physiol Nutr Metab. 2011;36:36–46. doi: 10.1139/H11-009. [DOI] [PubMed] [Google Scholar]
- 7.Tremblay MS, LeBlanc AG, Janssen !, Kho ME, Hicks A, Murumets K, Colley RC, Duggan M. Canadian sedentary behaviour guidelines for children and youth. Appl Physiol Nutr Metab. 2011;36:59–64. doi: 10.1139/H11-012. [DOI] [PubMed] [Google Scholar]
- 8.Janssen I. Physical activity guidelines for children and youth. Appl Physiol Nutr Metab. 2007;32:109–121. [Google Scholar]
- 9.Timmons B, Naylor P, Pfeiffer K. Physical activity for preschool children – how much and how? Can J Public Health. 2007;98:122–134. [PubMed] [Google Scholar]
- 10.Hearst W, Sharratt M. Canada’s physical activity guides: background, development, and process. Appl Physiol Nutr Metab. 2007;32:9–13. [Google Scholar]
- 11.Janssen I, Leblanc A. Systematic review of the health benefits of physical activity and fitness in school-aged children and youth. International J Behav Nutr Phys Activity. 2010;7(40):1–16. doi: 10.1186/1479-5868-7-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Eisenmann JC, Bartee RT, Wang MQ. Physical activity, TV viewing, and weight in U.S. youth: 1999 Youth Risk Behavior Survey. Obes Res. 2002;10(5):379–385. doi: 10.1038/oby.2002.52. [DOI] [PubMed] [Google Scholar]
- 13.Dencker M, Thorsson O, Karlsson MK, Linden C, Eiberg S, Wollmer P, Andersen LB. Daily physical activity related to body fat in children aged 8–11 years. J Pediatr. 2006;149(1):38–42. doi: 10.1016/j.jpeds.2006.02.002. [DOI] [PubMed] [Google Scholar]
- 14.Laxmaiah A, Nagalla B, Vijayaraghavan K, Nair M. Factors affecting prevalence of overweight among 12- to 17-year-old urban adolescents in Hyderabad, India. Obesity (Silver Spring) 2007;15(6):1384–1390. doi: 10.1038/oby.2007.165. [DOI] [PubMed] [Google Scholar]
- 15.Hernandez B, Gortmaker SL, Colditz GA, Peterson KE, Laird NM, Parra-Cabrera S. Association of obesity with physical activity, television programs and other forms of video viewing among children in Mexico city. Int J Obes Relat Metab Disord. 1999;23(8):845–854. doi: 10.1038/sj.ijo.0800962. [DOI] [PubMed] [Google Scholar]
- 16.Janssen I, Katzmarzyk PT, Boyce WF, King MA, Pickett W. Overweight and obesity in Canadian adolescents and their associations with dietary habits and physical activity patterns. J Adolesc Health. 2004;35(5):360–367. doi: 10.1016/j.jadohealth.2003.11.095. [DOI] [PubMed] [Google Scholar]
- 17.Veugelers PJ, Fitzgerald AL. Prevalence of and risk factors for childhood overweight and obesity. CMAJ. 2005;173(6):607–613. doi: 10.1503/cmaj.050445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Smith BJ, Phongsavan P, Havea D, Halavatau V, Chey T. Body mass index, physical activity and dietary behaviours among adolescents in the Kingdom of Tonga. Public Health Nutr. 2007;10(2):137–144. doi: 10.1017/S1368980007226060. [DOI] [PubMed] [Google Scholar]
- 19.Guerra S, Teixeira-Pinto A, Ribeiro JC, Ascensao A, Magalhaes J, Andersen LB, Duarte JA, Mota J. Relationship between physical activity and obesity in children and adolescents. J Sports Med Phys Fitness. 2006;46(1):79–83. [PubMed] [Google Scholar]
- 20.Eisenmann JC, Laurson KR, Wickel EE, Gentile D, Walsh D. Utility of pedometer step recommendations for predicting overweight in children. Int J Obes (Lond) 2007;31(7):1179–1182. doi: 10.1038/sj.ijo.0803553. [DOI] [PubMed] [Google Scholar]
- 21.McMurray RG, Harrell JS, Deng S, Bradley CB, Cox LM, Bangdiwala SI. The influence of physical activity, socioeconomic status, and ethnicity on the weight status of adolescents. Obes Res. 2000;8(2):130–139. doi: 10.1038/oby.2000.14. [DOI] [PubMed] [Google Scholar]
- 22.O’Loughlin J, Paradis G, Renaud L, Meshefedjian G, Gray-Donald K. Prevalence and correlates of overweight among elementary school children in multiethnic, low income, inner-city neighbourhoods in Montreal, Canada. Ann Epidemiol. 1998;8(7):422–432. doi: 10.1016/s1047-2797(98)00009-x. [DOI] [PubMed] [Google Scholar]
- 23.Fiore H, Travis S, Whalen A, Auinger P, Ryan S. Potentially protective factors associated with healthful body mass index in adolescents with obese and nonobese parents: a secondary data analysis of the third national health and nutrition examination survey, 1988–1994. J Am Diet Assoc. 2006;106(1):55–64. doi: 10.1016/j.jada.2005.09.046. quiz 76–59. [DOI] [PubMed] [Google Scholar]
- 24.Hanley AJ, Harris SB, Gittelsohn J, Wolever TM, Saksvig B, Zinman B. Overweight among children and adolescents in a Native Canadian community: prevalence and associated factors. Am J Clin Nutr. 2000;71(3):693–700. doi: 10.1093/ajcn/71.3.693. [DOI] [PubMed] [Google Scholar]
- 25.Kuriyan R, Bhat S, Thomas T, Vaz M, Kurpad AV. Television viewing and sleep are associated with overweight among urban and semi-urban South Indian children. Nutr J. 2007;6:25. doi: 10.1186/1475-2891-6-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Downs SH, Black N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J Epidemiol Community Health. 1998;52:377–384. doi: 10.1136/jech.52.6.377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Malcomson KS, Dunwoody I, Lowe-Strong AS. Psychosocial interventions in people with multiple sclerosis: A review. J Neurol. 2007;254:1–13. doi: 10.1007/s00415-006-0349-y. [DOI] [PubMed] [Google Scholar]
- 28.Heyman E, Toutain C, Delamarche P, Berthon P, Briard D, Youssef H, Dekerdanet M, Gratas-Delamarche A. Exercise training and cardiovascular risk factors in type 1 diabetic adolescent girls. Pediatr Exerc Sci. 2007;19(4):408–419. doi: 10.1123/pes.19.4.408. [DOI] [PubMed] [Google Scholar]
- 29.McMurray RG, Harrell JS, Bangiwala SI, Bradley CB, Deng S, Levine A. A school-based intervention can reduce body fat and blood pressure in young adolescents. J Adoles Health. 2002;31:125–132. doi: 10.1016/s1054-139x(02)00348-8. [DOI] [PubMed] [Google Scholar]
- 30.Farpour-Lambert NJ, Aggoun Y, Marchand LM, Martin XE, Herrmann FR, Beghetti M. Physical activity reduces systemic blood pressure and improves early markers of atherosclerosis in pre-pubertal obese children. J Am Coll Cardiol. 2009;54:2396–406. doi: 10.1016/j.jacc.2009.08.030. [DOI] [PubMed] [Google Scholar]
- 31.Kelly AS, Steinberger J, Olson TP, Dengel DR. In the absence of weight loss, exercise training does not improve adipokines or oxidative stress in overweight children. Metabolism. 2007;56(7):1005–1009. doi: 10.1016/j.metabol.2007.03.009. [DOI] [PubMed] [Google Scholar]
- 32.Meyer AA, Kundt G, Lenschow U, Schuff-Werner P, Kienast W. Improvement of early vascular changes and cardiovascular risk factors in obese children after a six-month exercise program. J Am Coll Cardiol. 2006;48(9):1865–1870. doi: 10.1016/j.jacc.2006.07.035. [DOI] [PubMed] [Google Scholar]
- 33.Kelly AS, Weitzteon RJ, Kaiser DR, Steinberger J, Bank AJ, Dengel DR. Inflammation, insulin, and endothelial function in overweight children and adolescents: The role of exercise. J Pediatr. 2004;145:731–6. doi: 10.1016/j.jpeds.2004.08.004. [DOI] [PubMed] [Google Scholar]
- 34.Gutin B, Barbeau P, Owens S, Lemmon CR, Bauman M, Allison J, Kang HS, Litaker MS. Effects of exercise intensity on cardiovascular fitness, total body composition, and visceral adiposity of obese adolescents. Am J Clin Nutr. 2002;75(5):818–826. doi: 10.1093/ajcn/75.5.818. [DOI] [PubMed] [Google Scholar]
- 35.Hagstromer M, Elmberg K, Marid S, Sjostrom M. Participation in organized weekly physical exercise in obese adolescents reduced daily physical activity. Acta Pediatrica. 2008;98:352–354. doi: 10.1111/j.1651-2227.2008.01116.x. [DOI] [PubMed] [Google Scholar]
- 36.Tan S, Yang C, Wang J. Physical training of 9-to-10-year-old children with obesity to lactate threshold intensity. Pediatr Exerc Sci. 2010;22:477–485. doi: 10.1123/pes.22.3.477. [DOI] [PubMed] [Google Scholar]
- 37.Aguilar FS, Martinez-Vizcaino V, Lopez MS, Martinez MS, Gutierrez RF, Martinez SS, Lopez-Garcia E, Rodriguez-Artalejo F. Impact of after school physical activity program on obesity in children. J Pediatr. 2010;157:36–42. doi: 10.1016/j.jpeds.2009.12.046. [DOI] [PubMed] [Google Scholar]
- 38.Kaminskyj A, Frazier M, Johnstone K, Gleberzon BJ. Chiropractic care for patients with asthma: A systematic review of the literature. J Can Chiropr Assoc. 2010;54(1):24–32. [PMC free article] [PubMed] [Google Scholar]
- 39.Takito MY, D’Aquino Benicio MH, Lopes Nevri LdC. Physical activity by pregnant women and outcomes for newborns: A systematic review. Rev Saude Publica. 2009;43(6):1–10. doi: 10.1590/s0034-89102009005000074. [DOI] [PubMed] [Google Scholar]
- 40.Strong WB, Malina RM, Blimkie CJ, Daniels SR, Dishman RK, Gutin B, et al. Evidence based physical activity for school-aged youth. J Pediatr. 2005;146:732–737. doi: 10.1016/j.jpeds.2005.01.055. [DOI] [PubMed] [Google Scholar]
- 41.Harris KC, Kuramoto LK, Schulzer MS, Retallack JE. Effect of school-based physical activity interventions on body mass index in children: a meta-analysis. CMAJ. 2009;180(7):719–26. doi: 10.1503/cmaj.080966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Knopfli BH, Radtke T, Lehmann M, et al. Effects of a multidisciplinary inpatient intervention on body composition, aerobic fitness, and quality of life in severely obese girls and boys. J Adoles Health. 2008;42:119–127. doi: 10.1016/j.jadohealth.2007.08.015. [DOI] [PubMed] [Google Scholar]
- 43.O’Connor TM, Jago R, Baranowski T. Engaging parents to increase youth physical activity: A systematic review. Am J Prev Med. 2009;37(2):141–157. doi: 10.1016/j.amepre.2009.04.020. [DOI] [PubMed] [Google Scholar]
- 44.Norton DE, Froelicher ES, Waters CM, Carrieri-Kohlman V. Parental influence in models of primary prevention of cardiovascular disease in children. Eur J Cardiovasc Nurs. 2003;2:311–322. doi: 10.1016/S1474-5151(03)00072-0. [DOI] [PubMed] [Google Scholar]
- 45.Kriemier S, Zahner L, Schindler C, et al. Effect of school based physical activity programme (KISS) on fitness and adiposity in primary school children: cluster randomized controlled trial. BMJ. 2010;340:785–794. doi: 10.1136/bmj.c785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Owens S, Gutin B, Allison J, Riggs S, Ferguson M, Litaker M, Thompson W. Effect of physical training on total and visceral fat in obese children. Med Sci Sports Exerc. 1999;31(1):143–148. doi: 10.1097/00005768-199901000-00022. [DOI] [PubMed] [Google Scholar]
- 47.Ferguson MA, Gutin B, Le NA, Karp W, Litaker M, Humphries M, Okuyama T, Riggs S, Owens S. Effects of exercise training and its cessation on components of the insulin resistance syndrome in obese children. Int J Obes Relat Metab Disord. 1999;23(8):889–895. doi: 10.1038/sj.ijo.0800968. [DOI] [PubMed] [Google Scholar]