Abstract
Objective
To describe the subjective pain and functional improvements of a patient with chronic Achilles tendinopathy following a treatment plan incorporating active and passive tissue warm-up, followed respectively by soft tissue mobilization utilizing both Graston Technique® and Active Release Techniques®, eccentric exercise, and static stretching in combination with cryotherapy.
Background
The primary characterization of chronic Achilles tendinopathy is gradual onset of pain and dysfunction focused in one or both Achilles tendons arising secondary to a history of repetitive use or excessive overload.
Intervention and Outcome
Conservative treatment is commonly the initial strategy for patient management. Tissue heating, soft tissue mobilization, eccentric training, and static stretching with cryotherapy were implemented to reduce pain and improve function.
Summary
A specific protocol of heat, soft tissue mobilization, eccentric exercise, stretching, and cryotherapy appeared to facilitate a rapid and complete recovery from chronic Achilles tendinopathy.
Keywords: Achilles, tendon pathology, tendinopathy, soft tissue therapy, thermotherapy, cryotherapy, eccentric exercise, Active Release Techniques, Graston Technique
Abstract
Objectif
décrire la douleur subjective et les améliorations fonctionnelles d’un patient souffrant de tendinopathie achilléenne chronique qui suit un traitement comprenant le réchauffement des tissus actifs et passifs, suivi respectivement de la mobilisation des parties molles à l’aide de la technique Graston® et des techniques Active Release®, de l’exercice excentrique, et de l’étirement statique jumelé à la cryothérapie.
Information de base
la tendinopathie achilléenne chronique se caractérise principalement par une douleur et une dysfonction qui évoluent graduellement dans l’un des tendons d’Achille, ou les deux, suite à un usage répétitif ou une surcharge excessive.
Intervention et résultat
le traitement conservateur constitue la stratégie initiale de gestion des patients. Le réchauffement des tissus, la mobilisation des parties molles, l’exercice excentrique et l’étirement statique avec cryothérapie furent utilisés pour atténuer la douleur et améliorer les fonctions.
Sommaire
un protocole spécifique de chaleur, la mobilisation des parties molles, l’exercice excentrique, l’étirement et la cryothérapie semblent faciliter la récupération rapide et complète d’une tendinopathie achilléenne chronique.
Keywords: Achille, pathologie des tendons, tendinopathie, thérapie des parties molles, thermothérapie, cryothérapie, exercice excentrique, techniques Active Release, technique Graston
Introduction
Chronic painful injuries of the Achilles tendon are relatively common in athletes, especially among runners.1–7 The annual incidence of Achilles disorders in top-level runners has been reported to be between 7% and 9%.2 In such cases, overuse is generally considered to be the inducing factor, however, the exact pathogenesis has not been demonstrated.1–4 Postulated alternative theories include poor vascularity, diminished flexibility, heredity, age, gender, as well as endocrine and/or metabolic factors.3,6 Realistically, the pathogenesis is likely a combination of multiple intrinsic and extrinsic factors.2 Alfredson (2005) theorizes that physical activity may be involved with provocation of symptoms as opposed to acting as the primary cause of the pathology.4
The lack of a conclusive pathogenesis for chronic achilles tendon disorders has resulted in considerable debate regarding the diagnostic terminology used in the literature.1–3,5,7,8 The terms “tendinitis” and “tendonitis” have been used, despite the absence of scientific evidence indicating inflammation.1–4 Under diagnostic ultrasound (DxUS) and magnetic resonance imaging (MRI), tendons exhibit a localized area of structural degeneration which has provoked the use of the term “degenerative tendinosis”.5 Recent investigations have indicated that the morphology of tendinosis involves changes in collagen fiber structure and arrangement, an increased amount of interfibrillar glycosaminoglycans (GAGs), and local vasculo-neural growth (neo-vascularisation) within the tendon structure.4,5,9 Alfredson (2003,2005), an authority on achilles pain disorders, states that it is now common opinion among investigators and clinicians that for chronic pain symptoms arising from a tender area of mid-substance tendon tissue, the term “tendinopathy” should be applied. Alternatively, when chronic pain symptoms are combined with diagnostic imaging showing changes in tendon fiber structure, arrangement, and/or evidence of local neo-vascularisation (via colour doppler ultrasound), the term utilized should be “tendinosis”.4,5,8 These terms could simply be interpreted as representing an academic continuum of severity and/or chronicity, with the former indicating a less progressed, and therefore less severe stage. This is an important distinction when developing a plan of management, as approaching treatment with the sole purpose of reducing inflammation is unlikely to resolve the condition as seen with the use of anti-inflammatory agents for chronic tendinopathies.10 Terminology aside, clinically determining the diagnosis of chronic Achilles tendinopathy via comprehensive patient history and physical exam is typically not difficult.
This report will describe the clinical presentation and treatment of a case of chronic Achilles tendinopathy which resulted from repetitive athletic activity (running). This case is of particular interest due to the rapid and successful patient response to a treatment plan incorporating an active and passive tissue warm-up, followed respectively by soft tissue mobilization utilizing both Graston Technique® (GT®) and Active Release Techniques® (ART®), eccentric training, and static stretching in combination with cryotherapy. The report will provide an overview of symptomatology, rationale supporting the management strategy, and expected outcomes associated with the diagnosis of chronic Achilles tendinopathy.
Case Presentation
A 40-year-old physically active male presented with intermittent bilateral Achilles pain of approximately 3.5 years duration which initially was felt in the right Achilles following a 7-minute dash in street shoes. Later, the patient began to notice an achy stiffness first thing in the morning, when starting to walk after prolonged sitting, and during the beginning of a regular fitness jog (10 km). The symptoms started out relatively mild and intermittent depending on activity level. Approximately six months later, the patient began training for a marathon and greatly increased the volume of running. During this period, the symptoms in the right Achilles gradually worsened, and the left Achilles began to exhibit similar symptoms. Approximately four months later, the stiffness and discomfort progressed to the point where the patient was limping while walking and was unable to continue training for the marathon. The patient then felt it was necessary to seek care. Orthotics were obtained from a chiropractor, a topical anti-inflammatory from a primary care physician, and physical therapy which included rest, therapeutic ultrasound, general massage, basic calf stretching, and needle acupuncture. The patient attended 10–15 physiotherapy sessions, 10 massage treatments and stated that the sessions provided only temporary relief, as the symptoms would re-occur with even light physical activity. Six months after the initiation of treatment the patient no longer pursued the goal of running a marathon, had greatly reduced his physical activity, and discontinued the physiotherapy sessions due to no evidence of long term improvements.
After almost a year of reduced activity and self-care, during which time the symptoms lessened but did not resolve, the patient then attended the author’s clinic. The patient characterized the pain (present in both achilles tendons but slightly worse on the left) as a bothersome “stiff, achy painful” sensation, with an intensity rating of 6–7 out of 10 as reported on a numeric pain rating scale (zero indicating “no pain” and 10 equalling the “worst pain ever”). Pain was described to be worse in the morning, and after prolonged inactivity, but too much activity also aggravated the pain. Based on self-report, the patient was able to run short distances of not greater than 5 km, but both Achilles were always very painful afterward. The patient had no previous history of significant foot or ankle injuries, related surgeries or traumas, medication or supplement use, and was a non-smoker and non-drinker. As an information technology manager, the daily job demands involved sedentary activities. Systems review and illness history was non-contributory.
Gait and postural observation were unremarkable. Physical examination revealed bilateral Achilles tendon pain induced by palpation which was slightly worse on the left. Upon visual inspection, the left tendon was mildly red, showed no evidence of ecchymosis and also exhibited a visual and palpable enlargement of the mid-substance tendon, just proximal to its insertion at the calcaneus. Mild pain in both tendons was provoked with resisted plantar flexion, passive dorsiflexion, and with bodyweight heel raises. Bilateral palpation of the posterior calf muscle complex subjectively revealed tightness and tenderness in the following muscles; soleus, flexor hallucis longus, flexor digitorum longus, and tibialis posterior. Orthopedic lower limb joint provocative testing indicated normal ligament structure and joint function. Chiropractic evaluation of lumbar, sacroiliac, knee, ankle mortis, subtalar, and tarsal joint motion were within normal limits. Neurological and vascular functions were likewise determined as normal.
Following the examination, the patient was diagnosed with chronic bilateral Achilles tendinopathy. The plan of management included two in-office treatments per week for three weeks, followed by one session every seven to ten days for an additional three sessions. Therefore, the patient received a total of nine sessions over an eight week period. The treatment plan (see Table 1) began with active and passive tissue heating accomplished by five minutes of heat pack application in combination with stationary cycling (see Figure 1). This was followed respectively by GT® (see Figure 2) and ART® (see Figure 3) applied to the affected muscles of the posterior leg (gastrocnemius, soleus, plantaris, flexor digitorum, tibialis posterior, and flexor hallucis longus). Slow eccentric calf lowering exercises (see Figure 4) were performed after the soft tissue mobilizations utilizing the sets and repetitions prescription consistent with previously published protocols.17–22 Finally, static gastrocnemius and soleus stretching was utilized in conjunction with ice pack application (see Figure 5). The patient was also required to follow a specific protocol of home therapy which included ice application, calf stretching, and eccentric heel lowering exercises (See Table 2). The patient was instructed to maintain his current level of physical activity, but not to increase it. During re-evaluation on the sixth visit, the pain level was reduced to 3–4 out of 10 (a 50% improvement), and Achilles discomfort was experienced less often in the mornings, as well as during and after running. Upon conclusion of the plan of management, the patient reported minimal discomfort in the Achilles tendons when squeezing or rubbing them, little to no discomfort with running, no pain with activities of daily living, and a pain level of 0–1 out of 10. Resisted plantar flexion and passive ankle dorsiflexion was non-painful. The patient considered the condition to be almost completely resolved and was thus discharged with instructions to continue with the home therapy protocol for an additional three weeks and to incorporate the eccentric calf lowering exercises into a regular training routine.
Table 1.
Office Therapy Protocol
| Patient: ___________________________ |
| Plan of Management: |
| _____/Week for _____ Weeks. |
In Office Protocol:
|
Figure 1.
Active and passive tissue warm-up utilizing a heat pack in combination with stationary cycling.
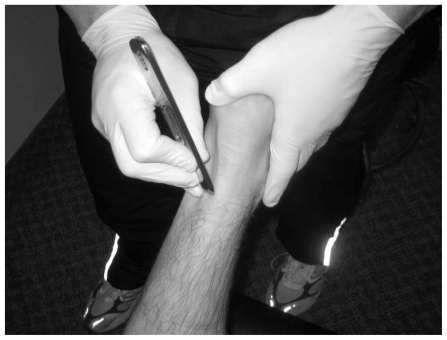
Figure 2.
Graston Technique® performed on the Achilles tendon.
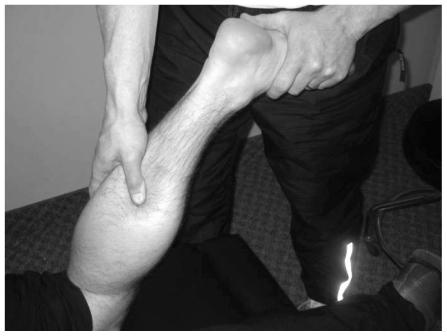
Figure 3.
Active Release Techniques® performed on the gastrocnemius muscle.
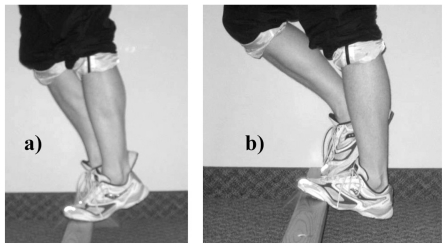
Figure 4.
Eccentric calf strengthening exercise. a) Start position, b) End Position.
Figure 5.
Static stretching with ice pack application. a) Gastrocnemius stretch, b) Soleus stretch.
Table 2.
Patient Home Therapy Protocol
| Patient: __________________ |
| In Office Management: |
| _______/Week for ______ Weeks. |
| Home Care: |
Day of Treatment:
|
1stDay after Treatment:
|
2ndDay after Treatment: (and up to next office visit)
|
During follow up seven months later, the patient reported equal or perhaps slight improvement over the discharged status. Orthopaedic and manual muscle testing were non-provocative and the patient reported a pain level of 0–1 out of 10. It was also noted that the weekly training routine was altered to include cross-training activities (cycling, swimming, circuit training, weights, yoga), and therefore the load on the Achilles was perhaps less than when training for a marathon, but significantly more loading than when the patient initially presented for therapy. The change in exercise pattern to include alternative forms of exercise may have also contributed to the overall improvement in symptoms. In summary, the patient reported to be at, or near, pre-injured physical status with the only residual symptom being a non-painful thickening of the Achilles tendons which was more pronounced on the left compared to the right.
Discussion
As illustrated by the above case presentation, patients with chronic Achilles tendinopathy typically present with a gradual onset of pain and dysfunction focused in one or both Achilles tendons.11 In athletic patients (competitive or recreational), symptoms generally arise secondary to a history of repetitive use or excessive overload.1–6,11 Factors included in the clinical presentation may include sudden increases in training volume or intensity, or both, a change of terrain (for example, hill running), an increase in interval training, or a solitary intense run.7 However, as mentioned previously, overuse is not always associated with the diagnosis.1–4 The pain associated with Achilles tendinopathy can range from mild to severe, depending on the phase of injury at initial presentation.11
Physical examination may reveal pain with resisted plantar flexion and passive dorsiflexion, and the patient will typically find it difficult to stand on tiptoe and/or to perform repeated single leg heel raises.11 Tenderness may be localized or diffuse, possibly extending several centimeters along the tendon, starting just proximal (2 to 6 centimeters) to the insertion of the Achilles onto the calcaneus.1–3, 11 The area of tenderness may be accompanied by tendon swelling, fibrous or nodular thickening, and possibly crepitus.3,11 If the diagnosis of Achilles tendinopathy is still in debate after a careful and thorough history and physical examination, medical imaging including diagnostic ultrasound or magnetic resonance imaging may be warranted.11
Most sources of information on the treatment of chronic Achilles tendinopathy suggest a conservative treatment protocol as the initial strategy for patient management, however, evidence is sparse in regards to which conservative treatment method and/or modality is most effective.1–5,11–13 Conservative treatment options include; eccentric strength training, therapeutic modalities, soft tissue mobilization, rest, corticosteroids, cryotherapy, heat, non-steroidal anti-inflammatory drugs (NSAIDs), deep friction massage, stretching, acupuncture, and podiatry.1,9,12–32 Among these treatments, calf muscle eccentric strength training, either alone or in combination with one or more of the other therapies, has the most supportive evidence.12,14–22 It is cost effective and low risk which makes it an ideal first-line therapy.12,14–22 In patients that have failed first-line conservative therapy, alternative treatments including extracorporeal shockwave therapy (ESWT), ultrasound-guided sclerosing agent injections and platelet-rich plasma (PRP) injections show promise in early studies, however, significant additional research is needed.9,32,33 Most commonly, the conservative therapy approach consists of some combination of the available therapies.1 Considering that the pathology of chronic Achilles tendinopathy is due to tissue overload and degeneration rather than inflammation, the rationale behind the plan of management developed for the presented patient was to reduce pain and to improve function. The aim was to re-initiate a state of healing and promote new tissue synthesis along lines of function-induced stress, while avoiding re-aggravation. The presented plan of management sought to achieve these outcomes via a specific treatment protocol incorporating an active and passive tissue warm-up, followed respectively by soft tissue mobilization (GT®, ART®), eccentric strength training, and static calf stretching in combination with cryotherapy. A brief review of the evidence in support of each of these specific interventions is presented.
Thermotherapy
Thermotherapy or heat application in a clinical setting has traditionally been used for the management of pain, joint stiffness and/or soft tissue stiffness associated with chronic conditions.34 Heat therapy application has also been thought to relieve muscle spasms, increase local blood flow, and assist in the resolution of inflammatory infiltrates, edema, and chemical exudates.35 Evidence on whether heat application can increase the extensibility of collagen fibers and therefore improve the elasticity of muscle, fascia, and tendon tissue remains inconclusive.36–38 Some evidence does support the use of heat therapy to create vasodilation, increased blood flow, warming of superficial tissues, and an increase in cellular metabolism.34–37
Graston Technique®
GT®, otherwise known as “Graston Technique Instrument-Assisted Soft Tissue Mobilization”, is a patented form of augmented soft tissue mobilization (ASTM).28,39,40 The therapy involves the utilization of custom designed stainless steel instruments to augment a clinician’s ability to perform soft tissue mobilization (see Figure 2).39 Essentially, the technique is an instrument assisted form of deep transverse friction massage (DTFM) as proposed by Cyriax in 1975.25,28 DTFM is theorized to reduce abnormal post injury fibrous adhesions, to make scar tissue more mobile in sub-acute and chronic injury, and to facilitate healing in chronically degenerated soft tissues by inducing controlled micro-trauma and facilitating the normal alignment of soft tissue fibers.3,25–29 This therapy creates a state of touch induced analgesia, inflammation, hyperemia, and increased fibroblast recruitment and activation, which contribute to the repair and regeneration of damaged collagen.3,25–29 Experimental animal investigations and human case reports support the above theories.26–29,39 Although there have been no controlled human studies, GT® and ASTM therapies have been reported to produce positive clinical benefits in the treatment of chronic ankle pain, sub-acute lumbar compartment syndrome, and trigger thumb.28,29,39
Active Release Techniques®
ART® is perhaps the most popular of the soft tissue therapy/mobilization techniques utilized by chiropractors and other manual therapists.40 It is proposed that repetitive or constant micro-trauma in the form of pressure, tension, and/or friction can lead to chronically tight and weak muscles, which eventually progresses to tissue injury, degeneration, and/or inflammation.38,41,42 If this situation is sustained, tissue adhesions and fibrosis can lead to chronically dysfunctional and painful tissue injuries.38 This theory is in line with the repetitive overuse pathogenesis theory of chronic Achilles tendinopathy.3 During ART® therapy, the clinician applies deep digital tension (utilizing either the thumb or fingers) to the affected site as the tissue is moved both actively and passively from a shortened position to a lengthened position (see Figure 3).38,41 The goal is to improve tissue function by reducing tissue stiffness, fibrosis, and/or adhesion.38,41 Numerous recent case reports suggest that ART®, in combination with active rehabilitation, is effective in the treatment of conditions including chronic lateral epicondylosis, external coxa sultans and for increasing the strength in a post-operative shoulder.40,43,44 Future research involving randomized control trials will more conclusively determine the efficacy of ART® in the treatment of musculoskeletal injuries.
Eccentric Exercise
Rehabilitative exercise has long been included in the conservative treatment approach to chronic Achilles ten-dinopathy.1–5,11,12,14–16 Although clinical research appears to support the efficacy of eccentric calf loading for the treatment of chronic Achilles tendinopathy, evidence regarding the mechanism of action is still unclear.17–22 Theories include a direct mechanical effect on tendon pathology in terms of tissue shape and alignment, an improvement in strength which relates to improved function, an improvement in muscle-tendon stiffness, a reduction in tendon volume, or a reduction or reversal of local tendon neovascularisation.17–19,45,46 Shalabi et al. (2004) found that eccentric training of the gastrocnemiussoleus complex in chronic Achilles tendinopathy resulted in decreased tendon volume and decreased intratendinous signal as evaluated by MRI.17 In another study, Öhberg and Alfredson (2004) found that painful Achilles tendinosis is associated with a local neovascularisation within the tendon structure, as demonstrated by colour doppler US.19 Furthermore, after 12-weeks of eccentric calf exercise, 34/36 subjects had decreased pain and improved function and 32/36 subjects had US evidence showing resolution of the neovascularisation. Öhberg and Alfredson concluded that positive clinical results after eccentric calf muscle training in patients with chronic Achilles tendinopathy seem to be associated with a more normal tendon structure and no remaining evidence of local tendon neovascularisation.19 A recent systematic review by Kingma et al. (2007), examined the efficacy of eccentric overload training on outcome measures of pain and physical functioning in patients with chronic Achilles tendinopathy.47 The study included three randomized control trials and six controlled trials. All were prospective in nature and had a mean duration of symptoms between 3.6 and 22 months. Six of the studies used the protocol described by Alfredson et al., while the other three used eccentric exercises with other co-interventions such as stretching, and cryotherapy.47,48 The duration of the eccentric training was 6 or 12 weeks and was compared to concentric training (three studies), surgery (one study), with a night splint or combined with a night splint (one study) and four studies did not include a control group. The results revealed a mean reduction in pain of 60% with eccentric overload training compared to 33% among controls.47 Although the effects of eccentric training are promising for reducing pain in chronic Achilles tendinopathy, the full magnitude of its effect cannot be determined due to the lack of satisfactory methodological quality of the studies. The results of the abovementioned findings offer strong support for the inclusion of eccentric calf muscle training in the management of chronic Achilles tendinopathy.
Cryotherapy and Stretching
Ice application (cryotherapy) and stretching are generally considered to be staple components of most injury management plans.49 In fact, ice is the most often applied therapeutic modality, despite the fact that there is minimal understanding regarding the actual physiological effects on soft tissue.49 Generally speaking, the effects associated with the application of cryotherapy include a reduction in cell metabolism and blood flow, decreased nerve conduction velocity, and decreased muscle spindle activity.34 Together, these physiological responses lead to the therapeutic effects of decreased secondary cell hypoxic injury, decreased pain, and decreased muscle spasm.34 Although evidence is not conclusive, the ideal method of ice application may be to apply real ice (as opposed to gel packs or chemical packs) through a wet towel interface to the injured area utilizing a protocol of 10 minutes on, 10 minutes off, 10 minutes on.49 Static gastrocnemius and soleus muscle stretching was included in the plan of management to improve ankle range of motion, isometric force production, stretch tolerance, and to promote a focused Achilles stress during the theorized tissue remodelling phase induced by soft tissue mobilization. Improvements in joint range of motion, isometric force production, and stretch tolerance following regular static stretching are supported by recent evidence.50–52
Prognosis
The natural history of Achilles tendinopathy is largely unknown.3 However, it is known that 24% to 45% of patients presenting with a chronic Achilles pain problem will fail to respond to conservative therapies and will choose operative management.3,53 No studies have reported the prognosis of patients with chronic Achilles tendinopathy treated conservatively with soft tissue mobilization either alone or in combination with a regime of eccentric calf strengthening. Considering that the best prognosis reported in the available literature is a return to full activity within 12 weeks, regardless of the therapeutic intervention, the response to treatment of the presented patient is notable.24 The patient obtained a near complete resolution of symptoms and a complete return to physical activity after a total of nine therapy sessions over an eight week period. Upon follow-up, seven months later, the patient had maintained the positive therapeutic result.
Summary
Chronic Achilles tendinopathy is a common injury, especially among distance runners.1–7 The diagnosis is relatively straightforward, and can be made from a thorough history and physical examination. The onset of pain and dysfunction are typically gradual and progressive, associated with overuse or high levels of physical activity.1–4,11 Early recognition and initiation of conservative therapies typically allow patients to return to their previous levels of activity anywhere between 12 weeks and 1 year, however, recovery can be long and frustrating as re-aggravation is possible.24
Although a conservative management approach is recommended, there is a considerable lack of evidence supporting a specific conservative management strategy. General treatment guidelines supported by the literature include methods to relieve pain, avoid re-aggravation, and treat injured tissues from the perspective of affecting the conditions pathology of angiofibroblastic degeneration and functional impairment.1–5,11–13 Current literature suggests that the conservative management of chronic Achilles tendinopathy should include an eccentric calf muscle strength training protocol.12,14–22 Whether or not the inclusion of some other conservative therapy intervention in combination with eccentric training improves the prognosis is not known. As seen in this case report, the implementation of a specific treatment protocol incorporating both an active and passive tissue warm-up, followed respectively by GT® and ART® soft tissue mobilization, eccentric calf muscle strength training, and static calf stretching in combination with cryotherapy appears to have resolved a case of chronic Achilles tendinopathy quite rapidly compared to the prognosis of 12 weeks reported by the literature.24 It is hypothesized that a specific treatment plan involving in-office and home based focused soft tissue therapy and tissue rehabilitation which relates directly to the current understanding of the pathology of chronic Achilles tendinopathy is the possible reason as to why this patient responded so positively, when previous passive treatment efforts failed. Consequently the conservative treatment protocol used in this case report may be beneficial for patients experiencing symptoms arising from chronic Achilles tendinopathy; however significant additional study is clearly necessary.
Footnotes
Disclaimer: Written consent was obtained from the patient for publication of this case report. No funding was received for this report. The author has no commercial associations that might pose a conflict of interest in connection with the submitted article.
References
- 1.Alfredson H, Lorentzon R. Chronic achilles tendinosis: Recommendations for treatment and prevention. Sports Med. 2000;29(2):135–46. doi: 10.2165/00007256-200029020-00005. [DOI] [PubMed] [Google Scholar]
- 2.Paavola M, Kannus P, Jarvinen T, Khan K, Jozsa L, Jarvinen M. Current concepts review: Achilles tendinopathy. J Bone Joint Surg. 2002;84A(11):2062–2076. doi: 10.2106/00004623-200211000-00024. [DOI] [PubMed] [Google Scholar]
- 3.Kader D, Saxena A, Movin T, Maffulli N. Achilles tendinopathy: Some aspects of basic science and clinical management. Br J Sports Med. 2002;36(4):239–49. doi: 10.1136/bjsm.36.4.239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Alfredson H. The chronic painful achilles and patellar tendon: Research on basic biology and treatment. Scand J Med Sci Sports. 2005;15(4):252–9. doi: 10.1111/j.1600-0838.2005.00466.x. [DOI] [PubMed] [Google Scholar]
- 5.Alfredson H. Chronic mid-portion achilles tendinopathy: An update on research and treatment. Clin Sports Med. 2003;22:727–741. doi: 10.1016/s0278-5919(03)00010-3. [DOI] [PubMed] [Google Scholar]
- 6.Huang TF, Perry SM, Soslowsky LJ. The effect of overuse activity on achilles tendon in an animal model: A biomechanical study. Ann Biomed Eng. 2004;32(3):336–41. doi: 10.1023/b:abme.0000017537.26426.76. [DOI] [PubMed] [Google Scholar]
- 7.Schepsis AA, Jones H, Haas AL. Achilles tendon disorders in athletes. Am J Sports Med. 2002;30(2):287–305. doi: 10.1177/03635465020300022501. [DOI] [PubMed] [Google Scholar]
- 8.Magnussen RA, Dunn WR, Thomson AB. Nonoperative treatment of midportion achilles tendinopathy: A systematic review. Clin J Sport Med. 2009;19(1):54– 64. doi: 10.1097/JSM.0b013e31818ef090. [DOI] [PubMed] [Google Scholar]
- 9.Alfredson H, Ohberg L. Sclerosing injections to areas of neo-vascularisation reduce pain in chronic achilles tendinopathy: A double-blind randomised controlled trial. Knee Surg Sports Traumatol Arthrosc. 2005;13(4):338–44. doi: 10.1007/s00167-004-0585-6. [DOI] [PubMed] [Google Scholar]
- 10.Rees JD, Maffulli N, Cook J. Management of tendinopathy. Am J Sports Med. 2009;37(9):1855–67. doi: 10.1177/0363546508324283. [DOI] [PubMed] [Google Scholar]
- 11.Sorosky B, Press J, Plastaras C, Rittenberg J. The practical management of achilles tendinopathy. Clin J Sport Med. 2004;14(1):40–4. doi: 10.1097/00042752-200401000-00007. [DOI] [PubMed] [Google Scholar]
- 12.Murray IR, Murray SA, MacKenzie K, Coleman S. How evidence based is the management of two common sports injuries in a sports injury clinic? Br J Sports Med. 2005;39(12):912–916. doi: 10.1136/bjsm.2004.017624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.McLauchlan GJ, Handoll HH. Interventions for treating acute and chronic achilles tendinitis. Cochrane Database Syst Rev. 2001;2:1–11. doi: 10.1002/14651858.CD000232. [DOI] [PubMed] [Google Scholar]
- 14.Kongsgaard M, Aagaard P, Kjaer M, Magnusson SP. Structural achilles tendon properties in athletes subjected to different exercise modes and in achilles tendon rupture patients. J Appl Physiol. 2005;99(5):1965–71. doi: 10.1152/japplphysiol.00384.2005. [DOI] [PubMed] [Google Scholar]
- 15.Ng GY, Ng CO, See EK. Comparison of therapeutic ultrasound and exercises for augmenting tendon healing in rats. Ultrasound Med Biol. 2004;30(11):1539–43. doi: 10.1016/j.ultrasmedbio.2004.08.030. [DOI] [PubMed] [Google Scholar]
- 16.Beneka AG, Malliou PC, Benekas G. Water and land based rehabilitation for achilles tendinopathy in an elite female runner. Br J Sports Med. 2003;37(6):535–7. doi: 10.1136/bjsm.37.6.535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Shalabi A, Kristoffersen-Wilberg M, Svensson L, Aspelin P, Movin T. Eccentric training of the gastrocnemiussoleus complex in chronic achilles tendinopathy results in decreased tendon volume and intratendinous signal as evaluated by MRI. Am J Sports Med. 2004;32(5):1286–96. doi: 10.1177/0363546504263148. [DOI] [PubMed] [Google Scholar]
- 18.Roos EM, Engstrom M, Lagerquist A, Soderberg B. Clinical improvement after 6 weeks of eccentric exercise in patients with mid-portion achilles tendinopathy – a randomized trial with 1-year follow-up. Scand J Med Sci Sports. 2004;14(5):286–95. doi: 10.1111/j.1600-0838.2004.378.x. [DOI] [PubMed] [Google Scholar]
- 19.Ohberg L, Alfredson H. Effects on neovascularisation behind the good results with eccentric training in chronic mid-portion achilles tendinosis? Knee Surg Sports Traumatol Arthrosc. 2004;12(5):465–70. doi: 10.1007/s00167-004-0494-8. [DOI] [PubMed] [Google Scholar]
- 20.Fahlstrom M, Jonsson P, Lorentzon R, Alfredson H. Chronic achilles tendon pain treated with eccentric calf-muscle training. Knee Surg Sports Traumatol Arthrosc. 2003;11(5):327–33. doi: 10.1007/s00167-003-0418-z. [DOI] [PubMed] [Google Scholar]
- 21.Mafi N, Lorentzon R, Alfredson H. Superior short-term results with eccentric calf muscle training compared to concentric training in a randomized prospective multicenter study on patients with chronic achilles tendinosis. Knee Surg Sports Traumatol Arthrosc. 2001;9(1):42–7. doi: 10.1007/s001670000148. [DOI] [PubMed] [Google Scholar]
- 22.Silbernagel KG, Thomee R, Thomee P, Karlsson J. Eccentric overload training for patients with chronic achilles tendon pain--a randomised controlled study with reliability testing of the evaluation methods. Scand J Med Sci Sports. 2001;11(4):197–206. doi: 10.1034/j.1600-0838.2001.110402.x. [DOI] [PubMed] [Google Scholar]
- 23.Speed CA. Fortnightly review: Corticosteroid injections in tendon lesions. BMJ. 2001;323(7309):382–6. doi: 10.1136/bmj.323.7309.382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Paoloni JA, Appleyard RC, Nelson J, Murrell GA. Topical glyceryl trinitrate treatment of chronic noninsertional achilles tendinopathy. A randomized, double-blind, placebo-controlled trial. J Bone Joint Surg Am. 2004;86-A(5):916–22. doi: 10.2106/00004623-200405000-00005. [DOI] [PubMed] [Google Scholar]
- 25.Brosseau L, Casimiro L, Milne S, Robinson V, Shea B, Tugwell P, Wells G. Deep transverse friction massage for treating tendinitis. Cochrane Database Syst Rev. 2002;4:1–8. [Google Scholar]
- 26.Gehlsen GM, Ganion LR, Helfst R. Fibroblast responses to variation in soft tissue mobilization pressure. Med Sci Sports Exerc. 1999;31(4):531–5. doi: 10.1097/00005768-199904000-00006. [DOI] [PubMed] [Google Scholar]
- 27.Davidson CJ, Ganion LR, Gehlsen GM, Verhoestra B, Roepke JE, Sevier TL. Rat tendon morphologic and functional changes resulting from soft tissue mobilization. Med Sci Sports Exerc. 1997;29(3):313–9. doi: 10.1097/00005768-199703000-00005. [DOI] [PubMed] [Google Scholar]
- 28.Hammer WI, Pfefer MT. Treatment of a case of subacute lumbar compartment syndrome using the graston technique. J Manipulative Physiol Ther. 2005 Mar;28(3:):199–204. doi: 10.1016/j.jmpt.2005.02.010. [DOI] [PubMed] [Google Scholar]
- 29.Melham TJ, Sevier TL, Malnofski MJ, Wilson JK, Helfst RH. Chronic ankle pain and fibrosis successfully treated with a new non-invasive augmented soft tissue mobilization technique (ASTM): A case report. Med Sci Sports Exerc. 1997:801–804. doi: 10.1097/00005768-199806000-00004. [DOI] [PubMed] [Google Scholar]
- 30.Yeung CK, Guo X, Ng YF. Pulsed ultrasound treatment accelerates the repair of achilles tendon rupture in rats. J Orthop Res. 2006;24(2):193–201. doi: 10.1002/jor.20020. [DOI] [PubMed] [Google Scholar]
- 31.Demir H, Menku P, Kirnap M, Calis M, Ikizceli I. Comparison of the effects of laser, ultrasound, and combined laser + ultrasound treatments in experimental tendon healing. Lasers Surg Med. 2004;35(1):84–9. doi: 10.1002/lsm.20046. [DOI] [PubMed] [Google Scholar]
- 32.Rompe JD, Nafe B, Furia JP, Maffulli N. Eccentric loading, shock-wave treatment, or a wait-and-see policy for tendinopathy of the main body of tendo achillis: A randomized controlled trial. Am J Sports Med. 2007;35(3):374–83. doi: 10.1177/0363546506295940. [DOI] [PubMed] [Google Scholar]
- 33.Alsousou J, Thompson M, Hulley P, Noble A, Willett K. The biology of platelet-rich plasma and its application in trauma and orthopaedic surgery: A review of the literature. J Bone Joint Surg Br. 2009;91(8):987–96. doi: 10.1302/0301-620X.91B8.22546. [DOI] [PubMed] [Google Scholar]
- 34.Bélanger A. Evidence-based guide to therapeutic physical agents. Philadelphia: Lippincott Williams & Wilkins; 2002. pp. 263–98. [Google Scholar]
- 35.Lehmann JF. Therapeutic heat and cold. 4th ed. Vol. 417. Baltimore: Williams & Wilkins; 1990. pp. 590–591. [Google Scholar]
- 36.Kubo K, Kanehisa H, Fukunaga T. Effects of cold and hot water immersion on the mechanical properties of human muscle and tendon in vivo. Clin Biomech (Bristol, Avon) 2005;20(3):291–300. doi: 10.1016/j.clinbiomech.2004.11.005. [DOI] [PubMed] [Google Scholar]
- 37.Kumamoto T, Ito T, Kubota K, Yamamoto I, Abe K, Fujiwara T. The influence of thermotherapy on muscle elasticity: Measurement of pennation angle with the use of ultrasound images. J Phys Ther Sci. 2006;18:193–199. [Google Scholar]
- 38.Leahy PM. Active Release Techniques®, soft-tissue management system for the lower extremity. 2000 [Google Scholar]
- 39.Howitt S, Wong J, Zabukovec S. The conservative treatment of trigger thumb using graston techniques and active release techniques. J Can Chiropr Assoc. 2006;50(4):249–54. [PMC free article] [PubMed] [Google Scholar]
- 40.Howitt SD. Lateral epicondylosis: A case study of conservative care utilizing ART and rehabilitation. J Can Chiropr Assoc. 2006;50(3):182–9. [PMC free article] [PubMed] [Google Scholar]
- 41.Schiottz-Christensen B, Mooney V, Azad S, Selstad D, Gulick J, Bracker M. The role of active release manual therapy for upper extremity overuse syndromes – a preliminary report. J Occup Rehabil. 1999;9(3):201– 211. [Google Scholar]
- 42.Drover JM, Forand DR, Herzog W. Influence of active release technique on quadriceps inhibition and strength: A pilot study. J Manipulative Physiol Ther. 2004;27(6):408–13. doi: 10.1016/j.jmpt.2004.05.006. [DOI] [PubMed] [Google Scholar]
- 43.Spina AA. External coxa saltans (snapping hip) treated with active release techniques: A case report. J Can Chiropr Assoc. 2007;51(1):23–9. [PMC free article] [PubMed] [Google Scholar]
- 44.Buchberger DJ. Use of active release techniques in the postoperative shoulder: A case report. J Sports Chiropr Rehabil. 1999;13:60–65. [Google Scholar]
- 45.Lorenz D. Eccentric exercise interventions for tendinopathies. J Strength Cond Res. 2010;32(2):90–98. [Google Scholar]
- 46.Khan KM, Scott A. Mechanotherapy: How physical therapists’ prescription of exercise promotes tissue repair. Br J Sports Med. 2009;43(4):247–52. doi: 10.1136/bjsm.2008.054239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kingma JJ, de Knikker R, Wittink HM, Takken T. Eccentric overload training in patients with chronic achilles tendinopathy: A systematic review. Br J Sports Med. 2007;41(6):e3. doi: 10.1136/bjsm.2006.030916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Alfredson H, Pietila T, Jonsson P, Lorentzon R. Heavy-load eccentric calf muscle training for the treatment of chronic achilles tendinosis. Am J Sports Med. 1998;26(3):360–6. doi: 10.1177/03635465980260030301. [DOI] [PubMed] [Google Scholar]
- 49.MacAuley D, Best TM. Evidence-based sports medicine. 2nd ed. Malden, Mass: Blackwell Pub; 2007. p. 615. [Google Scholar]
- 50.Zakas A. The effect of stretching duration on the lower-extremity flexibility of adolescent soccer players. J Bodywork Mov Ther. 2005;9:220–225. [Google Scholar]
- 51.Shrier I. Does stretching improve performance? A systematic and critical review of the literature. Clin J Sport Med. 2004;14(5):267–73. doi: 10.1097/00042752-200409000-00004. [DOI] [PubMed] [Google Scholar]
- 52.LaRoche DP, Connolly DA. Effects of stretching on passive muscle tension and response to eccentric exercise. Am J Sports Med. 2006;34(6):1000–7. doi: 10.1177/0363546505284238. [DOI] [PubMed] [Google Scholar]
- 53.Paavola M, Kannus P, Paakkala T, Pasanen M, Jarvinen M. Long-term prognosis of patients with achilles tendinopathy. an observational 8-year follow-up study. Am J Sports Med. 2000;28(5):634–42. doi: 10.1177/03635465000280050301. [DOI] [PubMed] [Google Scholar]