Abstract
Background
Estimates of the prevalence of lifetime suicidal ideation and attempt, and risks for new-onset suicidality, among HIV-infected (HIV+) individuals are not widely available in the era of modern combined antiretroviral treatment (cART).
Method
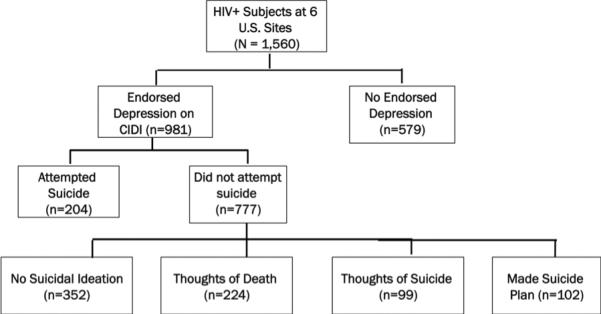
Participants (n=1560) were evaluated with a comprehensive battery of tests that included the depression and substance use modules of the Composite International Diagnostic Interview (CIDI) and the Beck Depression Inventory-II (BDI-II) as part of a large prospective cohort study at six U.S. academic medical centers. Participants with possible lifetime depression (n=981) were classified into five categories: 1) no thoughts of death or suicide (n=352); 2) thoughts of death (n=224); 3) thoughts of suicide (n=99); 4) made a suicide plan (n=102); and 5) attempted suicide (n=204).
Results
Twenty-six percent (405/1560) of participants reported lifetime suicidal ideation and 13% (204/1560) reported lifetime suicide attempt. Participants who reported suicidal thoughts or plans, or attempted suicide, reported higher scores on the BDI-II (p<0.0001), and higher rates of current major depressive disorder (p=0.01), than those who did not. Attempters reported higher rates of lifetime substance abuse (p=0.02) and current use of psychotropic medications (p=0.01) than non-attempters.
Limitations
Study assessments focused on lifetime, rather than current, suicide. Data was not collected on the timing of ideation or attempt, frequency, or nature of suicide attempt.
Conclusions
High rates of lifetime suicidal ideation and attempt, and the relationship of past report with current depressed mood, suggests that mood disruption is still prevalent in HIV. Findings emphasize the importance of properly diagnosing and treating psychiatric comorbidities among HIV persons in the cART era.
Keywords: HIV, depression, suicide
Introduction
Mood disturbance is common among HIV-infected (HIV+) persons (Atkinson et al., 1988, Atkinson et al., 2008, Judd et al., 2005, Rabkin, 2008). Within the context of depressed mood and clinical depression, suicide is of particular concern (Kessler et al., 1999). Previous studies have shown rates of suicidal ideation and behavior to be elevated among patients with chronic illness, including cancer and pain disorders when compared to the general population (Ilgen et al., 2010, Lofman et al., 2011, Robson et al., 2010). To date, investigations of suicidal ideation and suicidal behavior among HIV+ individuals have yielded inconsistent results. These inconsistencies have been attributed to issues with study design and methodology, including sampling and differing methods of assessing suicidal behavior (Komiti et al., 2001, Starace, 1995).
In the late 1980s and early 1990s, several registry-based studies reported extremely high rates of completed suicide among HIV+ individuals when compared to suicide rates in the general population (Cote et al., 1992, Marzuk et al., 1988). Although these studies found increased rates of suicide in men with HIV, they did not address any related covariates, such as disease stage or psychiatric diagnoses. Additionally, these studies were conducted before the advent of combination antiretroviral therapy (cART). During the pre-cART era, survival time for individuals diagnosed with HIV was much shorter, and was a likely factor contributing to the extremely high rates of suicide among HIV+ individuals when compared to the general population at that time. More recently, a Swiss study found significantly elevated rates of completed suicide in HIV+ individuals when compared to the general population (Keiser et al., 2010).
Several studies have compared the rates of suicidal ideation between HIV+ and HIV− individuals. Results from these studies have also been mixed, with some studies suggesting elevated rates of suicidal ideation among HIV+ persons and some suggesting comparable levels between the groups (Kelly et al., 1998, O'Dowd and McKegney, 1990, Rabkin et al., 1993, Schneider et al., 1991).
Multiple studies have explored the relationship between suicidal ideation and stage of HIV illness. Several research groups have found no significant difference in rates of suicidal ideation across different disease stages, (Chandra et al., 1998, Robertson et al., 2006) whereas others have found that suicidal ideation is less prevalent in individuals with AIDS than in individuals with less severe HIV disease (McKegney and O'Dowd, 1992, Sherr, 1995, Twiname, 1993). These data suggest that over the course of HIV illness, individuals may be able to adapt and find coping strategies that are more effective than suicidal thoughts, and that psychosocial variables may be more related to suicidal ideation than disease stage or severity (Cooperman and Simoni, 2005, Robertson et al., 2006).
Significant predictors of high rates of suicidal ideation in HIV+ individuals have been identified. Psychosocial stressors, including perceived social isolation and lack of social support, have been consistently associated with suicidal ideation in HIV+ individuals. Comorbid psychiatric illnesses, especially major depressive disorder and substance use disorders, have also been found to be highly predictive of suicidal ideation in HIV+ individuals (Perry et al., 1990, Rundell et al., 1988, Starace and Sherr, 1998). Protective factors against suicidal ideation among HIV+ persons have also been found including being in a primary relationship and coping self-efficacy (Carrico et al., 2007, Kelly et al., 1998, O'Dowd and McKegney, 1990, Rabkin et al., 1993, Schneider et al., 1991).
Many studies have explored the prevalence and correlations of suicidal ideation in the context of HIV infection; they have employed different methodologies and have achieved mixed results. Nonetheless, these prior investigations have highlighted the importance of addressing mood disturbance and suicidal ideation in HIV+ individuals. The present study aimed to provide an estimate of the lifetime prevalence of suicidal ideation (e.g., thoughts and plans of suicide) and behavior (e.g., suicide attempts) in a large, diverse multi-site United States cohort in the post-cART era, and to evaluate the correlates of lifetime and incident suicidal ideation and behavior. We hypothesized that lifetime prevalence rates of suicidal ideation and behavior would be elevated as compared to the general population, but lower than rates observed in the pre-cART era. We also hypothesized that current indicators of depressed mood would be strongly associated with lifetime suicide risk suggesting the possibility of continued mood dysregulation in the post-cART era.
Methods
Participants
A cross-sectional study was conducted to evaluate the prevalence of suicidal ideation in a representative sample of HIV+ individuals enrolled in the CNS HIV Antiretroviral Therapy Effects Research (CHARTER) study between 2003 and 2007. The CHARTER study is a multi-site, prospective, observational study conducted at the following six North American academic medical centers: Johns Hopkins University, Baltimore, MD; The Mount Sinai School of Medicine, New York, NY; University of California, San Diego, San Diego, CA; University of Texas, Medical Branch, Galveston, TX; University of Washington, Seattle, WA; and Washington University, St. Louis, MO. Local institutional review boards approved research at each site and all participants provided written informed consent. Between 2003 and 2007, 1,560 HIV+ participants were recruited to be in the CHARTER cross-sectional cohort. Of these, 659 participants completed a 6-month follow-up visit.
Participants were eligible to participate in the CHARTER study if they were HIV+, able to provide informed consent, and able to complete baseline assessments. Minimal exclusion criteria were present and only those persons who were unable to complete assessments were excluded from study participation.
In addition to the assessments detailed below, participants received comprehensive neurobehavioral, neuromedical, and laboratory testing as described elsewhere (Heaton et al., 2010).
Materials and Methods
Suicidal ideation and attempt were measured by participant response to four questions concerning suicide in the depression module of the Composite International Diagnostic Interview (CIDI; Version 2.1, World Health Organization). The CIDI is a computerized psychodiagnostic instrument designed for administration by lay interviewers to assess diagnoses of a wide range of psychiatric disorders. All participants were administered the CIDI substance use and depression modules; according to the CIDI algorithm, participants who endorsed a two-week or longer period in their lifetime where they 1) felt sad, empty, or depressed and 2) loss interest in activities were asked additional questions regarding their depressive symptoms, including questions about suicidal ideation. Each of the CIDI suicide questions required a “yes” or “no” response. The text of the four CIDI questions is found in Table 1.
Table 1.
CIDI questions used to identify suicidality
| Q1 | During one of those periods, did you think a lot about death? |
| Q2 | Did you feel so low you thought a lot about committing suicide? |
| Q3 | Did you make a plan as to how you might do it? |
| Q4 | Did you attempt suicide? |
Suicidal ideation was defined as a participant endorsing any thoughts or plans about committing suicide in the absence of a suicide attempt. Suicide attempt was defined as a participant indicating any action taken by the participant with the intent of ending his or her own life. Lifetime suicidal ideation and behavior was assessed within the context of evaluation for the presence of a possible major depressive episode.
Of 1,560 participants who completed the baseline assessment for the CHARTER study, 981 (63%) endorsed CIDI depression screening module items significant enough to warrant additional questions about lifetime suicidal ideation. These participants were grouped into 5 categories based on the most severe suicidality behavior endorsed. From least severe to most severe in response to the CIDI questions, these categories are 1) had no thoughts of death or suicide (n=352); 2) had thoughts of death (n=224); 3) had thoughts of committing suicide (n=99); 4) made a plan to commit suicide (n=102); and 5) attempted suicide (n=204). In order to compare characteristics of attempters versus non-attempters, participants were also grouped into suicide attempters (n=204) and non-attempters (n=777) based on the CIDI suicide attempt question. A summary of all participant groupings by the various levels of suicidality can be found in Figure 1.
Figure 1.
Grouping of Study Participants
Data Analysis
Covariates considered to be potential correlates of suicidal ideation and attempt were also evaluated. Demographic variables included: sex, age, education, and ethnicity. Neuromedical variables included: CD4 cell count, lowest reported (nadir) CD4 cell count, plasma HIV RNA, current antiretroviral (ARV) status (on antiretroviral therapy, ART; prior but not current use of ARVs; or no prior use of ARVs, i.e., ARV naïve), and current psychotropic medication use (yes or no). Plasma HIV RNA (plasma viral load) was log transformed to improve its distribution. Neurobehavioral variables included: CIDI diagnosis of current major depression (yes or no), Beck Depression Inventory – II (BDI-II) total score, lifetime substance abuse or dependence (yes or no), and the MOS HIV Health Survey quality of life assessment (McHorney et al., 1992, Ware and Sherbourne, 1992). Current diagnosis of major depressive disorder and assessments of lifetime substance abuse or dependence were obtained from participant responses to the CIDI. BDI-II total score was calculated as the sum score of patient responses to 21 graded-response (0 to 3) questions, with a maximum score of 63. We also examined participant responses to Beck Depression Inventory-II Item 9 that asks about suicidal ideation, plan and attempt; however, distribution of the BDI-II item 9 was skewed and did not allow for detailed analyses (i.e., very few persons endorsed the more severe suicidal categorizations). As such, the present study focuses on the results from the CIDI.
Frequencies and descriptive statistics were computed for each independent variable. Chi-square tests were used to assess group differences for categorical covariates. Analysis of variance (ANOVA) was used to assess group differences for continuous covariates. Multivariate analyses were carried out using ordinal logistic regression, with the 6-category suicide variable as the outcome. Analyses were not adjusted for multiple comparisons. Covariates with significant group differences across the suicide categories or those found to be significant in univariate analyses were included in the ordinal logistic regression model. Changes in suicide category, BDI-II total score, and HIV disease characteristics were assessed between the baseline and 6-month follow-up visit. Data was analyzed using JMP version 8.0.
Results
Of 1,560 participants who completed baseline assessments, 981 (63%) endorsed lifetime depressive symptoms on the CIDI. Among these 981 individuals, suicidal ideation was common; 405 participants (26% overall) reported history of lifetime suicidal ideation, and 204 (13% overall) reported history of lifetime suicide attempt.
The sample was comprised of 735 males (74.9%) and 246 females (25.1%). The mean age for the sample was 43 years. Roughly equal proportions of study participants identified themselves as either Black or White (43.3% and 43.2% respectively). Complete demographic characteristics of the study population by suicide category are presented in Table 2.
Table 2.
Demographic Characteristics of CHARTER Cohort (n = 1560)
| Characteristic | A. No Endorsed Depression (n=579) | B.No Suicidal Ideation (n=352) | C. Thoughts of Death (n=224) | D.Thoughts of Suicide (n=99) | E. Made Suicide Plan (n=102) | F. Made Suicide Attempt (n=204) | Total (n=1560) | P-value | Pairwise Comparison |
|---|---|---|---|---|---|---|---|---|---|
| Sex1 | 0.01 | E >A,B,C,D,F | |||||||
| Male | 460 [79.5] | 253 [71.9] | 173 [77.2] | 71 [71.7] | 88 [86.3] | 150 [73.5] | 1195 [76.6] | ||
| Age (years)2 | 43.5 [8.3] | 43.1 [8.6] | 43.9 [8.5] | 43.0 [8.2] | 44.7 [8.9] | 40.9 [8.3] | 43.2 [8.5] | 0.001 | A,B,C,D,E > F |
| Education (years)2 | 12.5 [2.5] | 12.6 [2.5] | 12.6 [2.6] | 12.8 [2.6] | 13.0 [2.5] | 12.0 [2.5] | 12.5 [2.5] | 0.003 | E > A,B,C,D >F |
| Ethnicity1 | <0.0001 | ||||||||
| Black | 337 [58.2] | 166 [47.2] | 95 [42.4] | 47 [47.5] | 33 [32.4] | 84 [41.2] | 425[43.3] | A>B,C,D>E,F | |
| Hispanic | 39 [6.7] | 38 [10.7] | 25 [11.2] | 13 [13.1] | 8 [7.8] | 23 [11.3] | 107 [10.9] | A>E | |
| White | 189 [32.6] | 141 [40.1] | 98 [43.8] | 38 [38.4] | 56 [54.9] | 91 [44.6] | 424 [43.2] | E >B,C,D,F>A | |
| Other | 14 [2.4] | 7 [2.0] | 6 [2.7] | 1 [1.0] | 5 [4.9] | 6 [2.9] | 25 [2.5] | NS | |
Number(%)
Mean (Standard Deviation)
Note: Percentages may not add to 100 due to rounding.
In Table 3, clinical characteristics of the study population are displayed by suicide category. Several clinical variables presented significant group differences. Participants with thoughts of suicide, those who made a suicide plan, and those who attempted suicide had significantly higher BDI-II total scores and reported significantly lower overall health-related quality of life than those with less severe lifetime suicidality endorsements (i.e., participants without suicidal ideation and participants who only endorsed thoughts of death). Participants who did not endorse any lifetime depressive symptoms had significantly lower BDI-II total scores than participants who endorsed some suicidal ideation (p< 0.0001). Those who entered the additional depressive screening on the CIDI were significantly more likely to report current psychotropic medication use than those who did not report any depressive symptoms on the CIDI (p<0.0001).
Table 3.
Clinical Characteristics of CHARTER Cohort (n = 1560)
| Suicide Category [n(%)or mean(sd)] | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Characteristic | A. No Depression Endorsed (n=579) | B.No Suicidal Ideation (n=352) | C. Thoughts of Death (n=224) | D.Thoughts of Suicide (n=99) | E. Made Suicide Plan (n=102) | F. Made Suicide Attempt (n=204) | Total (n=1560) | P-value | Pairwise Comparison |
| BDI-II Total Score | 10.1 (9.3) | 13.8 (9.6) | 15.4 (10.5) | 20.0 (10.7) | 19.2 (12.5) | 18.3 (11.7) | 14.0 (10.8) | <0.0001 | A<B,C<D,E,F |
| ARV Status | 0.13 | ||||||||
| Naïve | 92 (15.9) | 59 (16.8) | 28 (12.5) | 15 (15.2) | 8 (7.8) | 35 (17.2) | 237 (15.1) | ||
| HAART | 414 (71.5) | 251 (71.3) | 161 (71.2) | 69 (69.7) | 82 (80.4) | 131 (64.2) | 1108 (71.1) | ||
| No ARVs | 73 (12.6) | 42 (11.9) | 35 (15.6) | 15 (15.2) | 12 (11.8) | 38 (18.6) | 215 (13.8) | ||
| Current EFV | 0.003 | F< A,B,C,D,E | |||||||
| Yes | 129 (31.2) | 66 (26.3) | 52 (32.3) | 16 (23.2) | 18 (22.0) | 20 (15.2) | 301 (27.2) | ||
| No | 285 (68.8) | 185 (73.7) | 109 (67.7) | 53 (76.8) | 64 (78.0) | 111 (84.7) | 807 (72.8) | ||
| Regimen Type | 0.1 | ||||||||
| NNRTI-Based | 141 (34.1) | 86 (34.3) | 64 (39.8) | 24 (34.8) | 21 (25.6) | 28 (21.4) | 364 (32.9) | ||
| Pi-Based | 230 (55.6) | 134 (53.4) | 81 (50.3) | 36 (52.2) | 45 (54.9) | 88 (67.2) | 614 (55.4) | ||
| Other | 44 (10.4) | 31 (12.4) | 16 (10.9) | 9 (13.0) | 16 (19.5) | 15 (11.4) | 130 (11.7) | ||
| Current Psychotropics | <0.0001 | ||||||||
| No | 313 (54.4) | 135 (38.5) | 86 (38.4) | 30 (30.3) | 27 (26.5) | 51 (25.1) | 642 (41.3) | A>B,C,D,E>F | |
| Yes | 262 (45.6) | 216 (61.5) | 138 (61.6) | 69 (69.7) | 75 (73.5) | 152 (74.9) | 912 (58.7) | ||
| Est. Dur. Infec.(mos) | 118 (76) | 118 (76) | 123 (75) | 117 (66) | 133 (82) | 120 (78) | 120 (76) | 0.57 | |
| Current CD4 Count | 455 (291) | 445 (278) | 465 (303) | 493 (325) | 489 (265) | 470 (265) | 461 (287) | 0.36 | |
| Nadir CD4 Count | 211 (221) | 209 (189) | 192 (174) | 224 (205) | 192 (166) | 214 (161) | 208 (196) | 0.54 | |
| Log10 Plasma Viral Load | 2.7 (1.2) | 3.0 (1.3) | 2.9 (1.4) | 2.9 (1.4) | 2.7 (1.3) | 3.1 (1.3) | 2.9 (1.3) | 0.01 | A,E < B,C,D,F |
| HCV Status | 0.27 | ||||||||
| Positive | 158 (28.1) | 93 (27.0) | 50 (22.5) | 21 (21.4) | 22 (21.8) | 61 (30.0) | 405 (26.5) | ||
| Negative | 404 (71.9) | 251 (73.0) | 172 (77.5) | 77 (78.6) | 79 (78.2) | 142 (70.0) | 1125 (73.5) | ||
| Current MDD | <0.0001 | ||||||||
| No | 537 (95.2) | 297 (84.9) | 180 (80.4) | 71 (71.7) | 79 (77.5) | 152(74.9) | 1316 (85.3) | ||
| Yes | 27 (4.8) | 53 (15.1) | 44 (19.6) | 28 (28.3) | 23 (22.6) | 51 (25.1) | 226 (14.7) | D,F>E,C>B>A | |
| Lifetime Substance Abuse or Dependence | <0.0001 | ||||||||
| No | 203 (35.1) | 88 (25.0) | 52 (23.2) | 25 (25.3) | 24 (23.5) | 27 (13.2) | 419 (26.9) | ||
| Yes | 376 (64.9) | 264 (75.0) | 172 (76.8) | 74 (76.5) | 78 (76.5) | 177 (86.8) | 1141 (73.1) | A<B,C,D,E<F | |
| Quality of Life | |||||||||
| Mental Health | 74.3 (19.3) | 67.0 (19.4) | 63.5 (21.6) | 52.8 (21.5) | 58.9 (26.7) | 58.0 (22.2) | 66.6 (21.6) | <0.0001 | A>B>C, E>D>F |
| Physical Health | 72.7 (27.2) | 68.2 (27.2) | 66.3 (26.9) | 62.7 (26.1) | 63.7 (28.4) | 65.9 (28.3) | 68.7 (27.5) | <0.0001 | A>B,C,D,E,F |
The mean CD4 count and plasma viral load for the entire sample was 461 cells/μl (SD 287) and 2.9 log10 copies/ml (SD 1.3) respectively. The mean nadir CD4 count was 208 cells/μl (SD 196). Approximately 70% of participants were on ART. Of the 1108 participants on ART, 301 (27%) reported taking efavirenz as a part of their current regimen. Participants who reported a lifetime suicide attempt were significantly less likely to be on an efavirenz-containing regimen. A majority (73%) of participants reported a history of substance use disorder (abuse or dependence). In response to Item 9 on the BDI-II, which assesses suicidal ideation and behavior over the past two weeks, 79% of all participants (n=1227) reported no suicidal ideation, 20% (n=308) reported suicidal ideation with no intent to act (i.e., participant endorsed suicidal thoughts without a suicide plan), and less than 2% (n=20) reported current suicidal intent (i.e., participant endorsed making a plan for suicide or participant endorsed intent to commit suicide). Clinical characteristics of the study population are presented in Table 3.
In a multivariate ordinal regression model, Black ethnicity (p = 0.0006), higher current BDI-II total score (p<0.0001), currently taking psychotropic medications (p<0.0001), and lower mental health-related quality of life scores (p < 0.0001) were associated with more severe lifetime suicide categories.
Of the 659 participants who completed a 6-month follow-up visit and completed the CIDI assessment, 35 (5%) reported incident suicidal ideation or behavior, or progression in severity of suicidal ideation or behavior from that reported at the baseline assessment. Incidence or progression of suicidal ideation was associated with higher BDI-II total scores (p < 0.0001).
Discussion
Among all 1560 participants, 405 (26%) reported history of lifetime suicidal ideation, plan or attempt. Among individuals who endorsed depressive symptoms on the CIDI, the rate of lifetime suicidal ideation, plan or attempt was 41.3%. Moreover, longitudinal analysis revealed that 5% of those with at least one follow-up visit reported incident or worsening of suicidal ideation or behavior, and that this incident worsening was associated with more depressive symptoms. These findings emphasize the importance of thorough suicide evaluations among HIV-infected cohorts.
Whereas some studies have shown the rate of ideation to be elevated in HIV+ cohorts in comparison to HIV− controls, consistent rates have not been established. The prevalence rate of suicidal ideation found in this study (26%) was higher than the rate reported by Carrico and colleagues (19.3%)(Carrico et al., 2007) and lower than that found in another study 31% (Sherr et al., 2008). Of note, however, is that both of these studies assessed the 1-week prevalence of suicidal ideation rather than the lifetime prevalence assessed in the current study. In a much smaller HIV+ cohort, Robertson and colleagues reported a lifetime suicidal ideation prevalence rate of 56% (Robertson et al., 2006).
The lifetime prevalence of suicide attempt in the CHARTER cohort was approximately 13%. This is lower than the approximate rate of 20% reported in previous studies of HIV+ individuals conducted in the United States during the pre-cART era (Kelly et al., 1998, Robertson et al., 2006). Additionally, a 2008 investigation conducted in France yielded a lifetime suicide attempt prevalence of 22% in a large HIV+ cohort (Preau et al., 2008).
This study confirmed previous studies indicating a lack of relationship between suicide attempt and estimated duration of HIV illness. This is consistent with previous research that has suggested that HIV+ individuals may develop healthy and effective coping strategies over the course of HIV illness (Cooperman and Simoni, 2005, Robertson et al., 2006). We also found that Black ethnicity was a significantly associated with more severe lifetime suicide behavior, a finding that is in agreement with results from previous studies (Sherr et al., 2008). This finding may indicate that the stigma and shame associated with HIV infection increases the risk for mood disturbances in this population. For instance, factors such as social support and effective coping strategies are likely more important to successfully avoiding suicidal thoughts and behavior than the duration of HIV infection.
Individuals with a history of suicidal ideation and suicide attempt reported significantly higher levels of current depressive symptoms and had a significantly higher prevalence of current (within the last 30 days) major depressive disorder, as well as higher levels of plasma HIV RNA. Higher levels of plasma HIV RNA may indicate decreased adherence to ARV medications in currently depressed individuals. Participants who attempted suicide were also significantly more likely to report a lifetime history of substance use disorder (abuse or dependence), and to be currently taking psychotropic medications. Although currently depressed participants may have been more likely to report past behaviors, it is unlikely that this accounted for the significant association that was observed. The fact that prior suicidal ideation and behavior is associated with current depression in this population indicates that these individuals may still be at risk for future suicidal ideation and behavior. Those who had attempted suicide were significantly less likely to be on an efavirenz-containing ARV regimen; this is likely a result of provider bias in not prescribing efavirenz to persons with significant psychiatric problems. Clinicians should be cognizant of past suicidal ideation or behavior in their patients, and monitor them carefully for current mood disturbances.
This study also had a number of important limitations. First, suicide and other psychological data were based on participant self-report. Because of possible stigma associated with report of psychological symptoms, some participants may not have admitted to suicidal ideation or attempt; inaccurate responses with regard to suicide questions would lead to misclassification of subjects into the wrong suicide category, possibly causing an underestimation of the prevalence of suicidal ideation and attempt in the CHARTER cohort. It should be noted, however, that self-report methodology is a limitation of most studies of this nature. The present study focused on lifetime rates of suicidal thoughts and behavior rather than current suicide reports. Because of the focus on past behavior, and the fact that the data were gathered in the context of a larger study on the neurocognitive consequences of HIV infection, data was not collected on the timing of ideation or attempt (e.g., before or after HIV diagnosis), frequency (e.g., frequency of ideation or number of attempts), or nature of suicide attempt (e.g., passive versus active attempt, in the context of a major depressive episode). Moreover, no measures of social support were available for consideration. Previous studies of suicide in the context of HIV infection have consistently shown social support and stability to be protective against suicidal ideation and attempt (Carrico et al., 2007, Sherr et al., 2008).
Although the suicidal ideation and attempt may or may not have occurred in the context of HIV illness, these individuals still bear a heavy psychological burden. Physicians treating HIV+ individuals should be aware of the higher prevalence of major depressive disorder, as well as the high likelihood that many of their patients may have struggled with suicidal ideation or attempt in the past. In recognizing the increased prevalence of psychological disturbance in this population, clinicians may be better able to address the enduring burden of past suicidal thoughts or behavior.
Although additional longitudinal studies are needed to confirm these findings, results from this study may assist in identifying individuals who may be at increased risk for psychological distress. In the future, longitudinal analysis of the correlates of incident suicidal ideation and suicide attempt in the context of progressing HIV illness are needed. Knowledge of when suicidal ideation and attempts occurred during the participants' lifetime would allow a more complete understanding of mood disturbance in the context of HIV infection. Additionally, future studies should take measures of social support into account in order to provide better understanding of suicidal ideation and behavior in this population.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- ATKINSON JH, HEATON RK, PATTERSON TL, WOLFSON T, DEUTSCH R, BROWN SJ, SUMMERS J, SCIOLLA A, GUTIERREZ R, ELLIS RJ, ABRAMSON I, HESSELINK JR, MCCUTCHAN JA, GRANT I. Two-year prospective study of major depressive disorder in HIV-infected men. J Affect Disord. 2008;108:225–34. doi: 10.1016/j.jad.2007.10.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- ATKINSON JH, JR., GRANT I, KENNEDY CJ, RICHMAN DD, SPECTOR SA, MCCUTCHAN JA. Prevalence of psychiatric disorders among men infected with human immunodeficiency virus. A controlled study. Arch Gen Psychiatry. 1988;45:859–64. doi: 10.1001/archpsyc.1988.01800330091011. [DOI] [PubMed] [Google Scholar]
- CARRICO AW, JOHNSON MO, MORIN SF, REMIEN RH, CHARLEBOIS ED, STEWARD WT, CHESNEY MA. Correlates of suicidal ideation among HIV-positive persons. Aids. 2007;21:1199–203. doi: 10.1097/QAD.0b013e3281532c96. [DOI] [PubMed] [Google Scholar]
- CHANDRA PS, RAVI V, DESAI A, SUBBAKRISHNA DK. Anxiety and depression among HIV-infected heterosexuals--a report from India. J Psychosom Res. 1998;45:401–9. doi: 10.1016/s0022-3999(98)00028-2. [DOI] [PubMed] [Google Scholar]
- COOPERMAN NA, SIMONI JM. Suicidal ideation and attempted suicide among women living with HIV/AIDS. J Behav Med. 2005;28:149–56. doi: 10.1007/s10865-005-3664-3. [DOI] [PubMed] [Google Scholar]
- COTE TR, BIGGAR RJ, DANNENBERG AL. Risk of suicide among persons with AIDS. A national assessment. Jama. 1992;268:2066–8. doi: 10.1001/jama.1992.03490150118035. [DOI] [PubMed] [Google Scholar]
- HEATON RK, CLIFFORD DB, FRANKLIN DR, JR., WOODS SP, AKE C, VAIDA F, ELLIS RJ, LETENDRE SL, MARCOTTE TD, ATKINSON JH, RIVERA-MINDT M, VIGIL OR, TAYLOR MJ, COLLIER AC, MARRA CM, GELMAN BB, MCARTHUR JC, MORGELLO S, SIMPSON DM, MCCUTCHAN JA, ABRAMSON I, GAMST A, FENNEMA-NOTESTINE C, JERNIGAN TL, WONG J, GRANT I. HIV-associated neurocognitive disorders persist in the era of potent antiretroviral therapy: CHARTER Study. Neurology. 2010;75:2087–96. doi: 10.1212/WNL.0b013e318200d727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- ILGEN MA, ZIVIN K, AUSTIN KL, BOHNERT AS, CZYZ EK, VALENSTEIN M, KILBOURNE AM. Severe pain predicts greater likelihood of subsequent suicide. Suicide Life Threat Behav. 2010;40:597–608. doi: 10.1521/suli.2010.40.6.597. [DOI] [PubMed] [Google Scholar]
- JUDD F, KOMITI A, CHUA P, MIJCH A, HOY J, GRECH P, STREET A, LLOYD J, WILLIAMS B. Nature of depression in patients with HIV/AIDS. Aust N Z J Psychiatry. 2005;39:826–32. doi: 10.1080/j.1440-1614.2005.01659.x. [DOI] [PubMed] [Google Scholar]
- KEISER O, SPOERRI A, BRINKHOF MW, HASSE B, GAYET-AGERON A, TISSOT F, CHRISTEN A, BATTEGAY M, SCHMID P, BERNASCONI E, EGGER M. Suicide in HIV-infected individuals and the general population in Switzerland, 1988–2008. Am J Psychiatry. 2010;167:143–50. doi: 10.1176/appi.ajp.2009.09050651. [DOI] [PubMed] [Google Scholar]
- KELLY B, RAPHAEL B, JUDD F, PERDICES M, KERNUTT G, BURNETT P, DUNNE M, BURROWS G. Suicidal ideation, suicide attempts, and HIV infection. Psychosomatics. 1998;39:405–15. doi: 10.1016/S0033-3182(98)71299-X. [DOI] [PubMed] [Google Scholar]
- KESSLER RC, BORGES G, WALTERS EE. Prevalence of and risk factors for lifetime suicide attempts in the National Comorbidity Survey. Arch Gen Psychiatry. 1999;56:617–26. doi: 10.1001/archpsyc.56.7.617. [DOI] [PubMed] [Google Scholar]
- KOMITI A, JUDD F, GRECH P, MIJCH A, HOY J, LLOYD JH, STREET A. Suicidal behaviour in people with HIV/AIDS: a review. Aust N Z J Psychiatry. 2001;35:747–57. doi: 10.1046/j.1440-1614.2001.00943.x. [DOI] [PubMed] [Google Scholar]
- LOFMAN S, RASANEN P, HAKKO H, MAINIO A. Suicide among persons with back pain: a population-based study of 2310 suicide victims in northern Finland. Spine (Phila Pa 1976) 2011;36:541–8. doi: 10.1097/BRS.0b013e3181f2f08a. [DOI] [PubMed] [Google Scholar]
- MARZUK PM, TIERNEY H, TARDIFF K, GROSS EM, MORGAN EB, HSU MA, MANN JJ. Increased risk of suicide in persons with AIDS. Jama. 1988;259:1333–7. [PubMed] [Google Scholar]
- MCHORNEY CA, WARE JE, JR., ROGERS W, RACZEK AE, LU JF. The validity and relative precision of MOS short- and long-form health status scales and Dartmouth COOP charts. Results from the Medical Outcomes Study. Med Care. 1992;30:MS253–65. doi: 10.1097/00005650-199205001-00025. [DOI] [PubMed] [Google Scholar]
- MCKEGNEY FP, O'DOWD MA. Suicidality and HIV status. Am J Psychiatry. 1992;149:396–8. doi: 10.1176/ajp.149.3.396. [DOI] [PubMed] [Google Scholar]
- O'DOWD MA, MCKEGNEY FP. AIDS patients compared with others seen in psychiatric consultation. Gen Hosp Psychiatry. 1990;12:50–5. doi: 10.1016/0163-8343(90)90038-e. [DOI] [PubMed] [Google Scholar]
- PERRY S, JACOBSBERG L, FISHMAN B. Suicidal ideation and HIV testing. Jama. 1990;263:679–82. [PubMed] [Google Scholar]
- PREAU M, BOUHNIK AD, PERETTI-WATEL P, OBADIA Y, SPIRE B. Suicide attempts among people living with HIV in France. AIDS Care. 2008;20:917–24. doi: 10.1080/09540120701777249. [DOI] [PubMed] [Google Scholar]
- RABKIN JG. HIV and depression: 2008 review and update. Curr HIV/AIDS Rep. 2008;5:163–71. doi: 10.1007/s11904-008-0025-1. [DOI] [PubMed] [Google Scholar]
- RABKIN JG, REMIEN R, KATOFF L, WILLIAMS JB. Suicidality in AIDS long-term survivors: what is the evidence? AIDS Care. 1993;5:401–11. doi: 10.1080/09540129308258010. [DOI] [PubMed] [Google Scholar]
- ROBERTSON K, PARSONS TD, VAN DER HORST C, HALL C. Thoughts of death and suicidal ideation in nonpsychiatric human immunodeficiency virus seropositive individuals. Death Stud. 2006;30:455–69. doi: 10.1080/07481180600614435. [DOI] [PubMed] [Google Scholar]
- ROBSON A, SCRUTTON F, WILKINSON L, MACLEOD F. The risk of suicide in cancer patients: a review of the literature. Psychooncology. 2010;19:1250–8. doi: 10.1002/pon.1717. [DOI] [PubMed] [Google Scholar]
- RUNDELL JR, PAOLUCCI SL, BEATTY DC, BOSWELL RN. Psychiatric illness at all stages of human immunodeficiency virus infection. Am J Psychiatry. 1988;145:652–3. doi: 10.1176/ajp.145.5.652b. [DOI] [PubMed] [Google Scholar]
- SCHNEIDER SG, TAYLOR SE, HAMMEN C, KEMENY ME, DUDLEY J. Factor influencing suicide intent in gay and bisexual suicide ideators: differing models for men with and without human immunodeficiency virus. J Pers Soc Psychol. 1991;61:776–88. doi: 10.1037//0022-3514.61.5.776. [DOI] [PubMed] [Google Scholar]
- SHERR L. Suicide and AIDS: lessons from a case note audit in London. AIDS Care. 1995;7(Suppl 2):S109–16. doi: 10.1080/09540129550126083. [DOI] [PubMed] [Google Scholar]
- SHERR L, LAMPE F, FISHER M, ARTHUR G, ANDERSON J, ZETLER S, JOHNSON M, EDWARDS S, HARDING R. Suicidal ideation in UK HIV clinic attenders. Aids. 2008;22:1651–8. doi: 10.1097/QAD.0b013e32830c4804. [DOI] [PubMed] [Google Scholar]
- STARACE F. Epidemiology of suicide among persons with AIDS. AIDS Care. 1995;7(Suppl 2):S123–8. doi: 10.1080/09540129550126100. [DOI] [PubMed] [Google Scholar]
- STARACE F, SHERR L. Suicidal behaviours, euthanasia and AIDS. Aids. 1998;12:339–47. doi: 10.1097/00002030-199804000-00001. [DOI] [PubMed] [Google Scholar]
- TWINAME BG. The relationship between HIV classification and depression and suicidal intent. J Assoc Nurses AIDS Care. 1993;4:28–35. [PubMed] [Google Scholar]
- WARE JE, JR., SHERBOURNE CD. The MOS 36-item short-form health survey (SF- 36). I. Conceptual framework and item selection. Med Care. 1992;30:473–83. [PubMed] [Google Scholar]