CASE PRESENTATION
A 24-year-old woman with no significant medical history presented to the hospital with complaints of nausea and vomiting for one day. The patient had experienced associated symptoms of abdominal distension, which worsened after meals, for the previous six months. The patient denied weight loss. The laboratory results were unremarkable. On physical examination, her abdomen was soft, with minimal tenderness in the epigastric area without guarding or rigidity. Bowel sounds were heard in all four quadrants, and there were no signs of organomegaly, ascites or asterixis.
DIAGNOSIS
Superior mesenteric artery syndrome
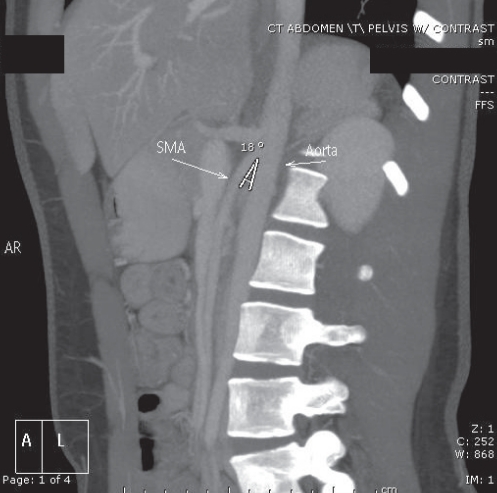
An abdominal computed tomography (CT) scan with contrast revealed the narrowing of the third portion of the duodenum compressed by the superior mesenteric artery (SMA), with dilation of the portion of the duodenum proximal to the compression. An abdominal CT scan and ultrasound with Doppler was used to measure the aortomesenteric (AO) angle and the AO distance. The normal AO angle is between 45° and 60° (1); the AO angle in this patient was 18° (Figure 1). The normal AO distance is between 10 mm and 20 mm (1); the AO distance in this patient was 5 mm to 6 mm (Figures 2 to 4); hence, the diagnosis was consistent with SMA syndrome.
Figure 1.
Longitudinal grey-scale ultrasound image demonstrating an aorta-superior mesenteric artery (SMA) angle of 18°
Figure 2.
Longitudinal grey-scale ultrasound image showing an aorta-superior mesenteric artery (SMA) distance of 6 mm measured at the level of the duodenum
Figure 4.
Axial contrast-enhanced computed tomography scan showing a narrow aorta-superior mesenteric artery (SMA) distance of 5 mm
DISCUSSION
SMA syndrome, also known as Wilkie’s syndrome (2), cast syndrome or AO syndrome, is described as the loss of the intervening mesenteric fat pad between the aorta and SMA, leading to narrowing of the angle between the two vessels, which in turn causes compression of the third portion of the duodenum. The most common cause of SMA syndrome is severe weight loss including trauma, burns, anorexia nervosa and/or after prolonged bed rest (3). Other rare causes of SMA syndrome are surgical correction of scoliosis (4) and a congenitally short ligament of Treitz. Patients with SMA syndrome present with bloating sensation, epigastric pain, abdominal distension, nausea and vomiting. Symptoms may be relieved when patients are in the left lateral decubitus, prone or knee-chest position (2). Diagnostic modalities include abdominal ultrasound with Doppler or abdominal CT (5) with contrast to measure the AO angle and AO distance. The treatment for this syndrome is correction of electrolyte imbalance, decompression of the obstruction via a nasogastric tube and nutritional support. Feeding in such patients is aided by a nasojejunal tube placed beyond the third portion of the duodenum. After initial weeks, and once the patient begins gaining weight, oral feeding should be encouraged. If the weight gain does not improve the symptoms, surgical mobilization of the duodenum after the ligament of Treitz is required. The duodenum is placed to the right of the SMA so it does not lie in the acute angle between the SMA and the aorta (6). A comprehensive history should be obtained, especially weight loss, in patients in whom the clinical suspicion of SMA syndrome is high.
Figure 3.
Sagittal maximum intensity projection image of aorta and superior mesenteric artery (SMA) showing a narrow aorta-SMA angle of 18°
The Canadian Journal of Gastroenterology is now considering a limited number of submissions for IMAGE OF THE MONTH. These will be based on endoscopic, histological, radiological and/or patient images, which must be anonymous with no identifying features visible. The patient must consent to publication, and the consent must be submitted with the manuscript. All manuscripts should be practical and relevant to clinical practice, and not simply a case report of an esoteric condition. The text should be brief, structured as CASE PRESENTATION and DISCUSSION, and not more than 700 words in length. A maximum of three to four images can be submitted, and the number of references should not exceed five. The submission may be edited by our editorial team.
REFERENCES
- 1.Gustafsson L, Falk A, Lukest PJ, Gamklou R. Diagnosis and treatment of superior mesenteric artery syndrome. Br J Surg. 1984;71:499–501. doi: 10.1002/bjs.1800710706. [DOI] [PubMed] [Google Scholar]
- 2.Gniftiths GJ, Whitehouse GH, Wilkie DP. Chronic duodenal ileus. Br J Surg. 1921;9:204. [Google Scholar]
- 3.Laffont I, Bensmail D, Rech C, Prigent G, Loubert G, Dizien O. Late superior mesenteric artery syndrome in paraplegia: Case report and review. Spinal Cord. 2002;40:88. doi: 10.1038/sj.sc.3101255. [DOI] [PubMed] [Google Scholar]
- 4.Crowther MA, Webb PJ, Eyre-Brook IA. Superior mesenteric artery syndrome following surgery for scoliosis. Spine. 2002;27:E528. doi: 10.1097/00007632-200212150-00023. [DOI] [PubMed] [Google Scholar]
- 5.Santer R, Young C, Rossi T, Riddlesberger MM. Computed tomography in superior mesenteric artery syndrome. Pediatr Radiol. 1991;21:154. doi: 10.1007/BF02015638. [DOI] [PubMed] [Google Scholar]
- 6.Wilson-Storey D, MacKinlay GA. The superior mesenteric artery syndrome. J R Coll Surg (Edin) 1986;31:175. [PubMed] [Google Scholar]